- Systematic Review
Medication Adherence Following Stroke and TIA: A Qualitative Synthesis of Patient, Caregiver and Clinician Perspectives
- Erin O’Kane,
- Rhiannon De Ivey and
- Eugene Yee Hing Tang
- + 6 authors
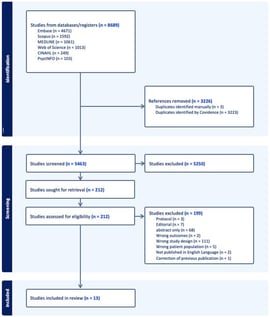
Background/Objectives: Stroke survivors require life-long secondary prevention to reduce recurrence, but they also often face long-term impairments that may limit medication adherence (MA) including cognitive, physical, and psychological effects. This updated qualitative meta-synthesis aims to descriptively explore and synthesise the experiences and perspectives of stroke/TIA survivors, informal and formal carers of stroke survivors, and healthcare professionals involved in post-stroke/TIA care, with a focus on factors influencing and hindering MA. Methods: A qualitative meta-synthesis was conducted in accordance with PRISMA guidance. Searches were undertaken across MEDLINE, CINAHL, Embase, PsycINFO, Scopus and Web of Science for studies published from 1 January 2018. Study quality was assessed using the Joanna Briggs Institute checklist and data synthesised using Thomas and Harden’s method. Results: Of 5463 titles and abstracts screened, 212 underwent full-text review with 13 papers meeting inclusion criteria from eight countries with a total of 435 participants. Seven key themes were identified: knowledge and understanding, beliefs and attitudes, practical barriers, social support, healthcare system, psychological factors and medication characteristics. Survivors showed a varied understanding of their condition and prescribed medicines, with unclear communication often contributing to confusion. Beliefs and attitudes shaped adherence, ranging from confidence in treatment to scepticism. Practical barriers included financial costs, physical impairments, and limited access to services. Social support from family, friends, and healthcare professionals was also important. Psychological wellbeing, coping strategies, and medication side effects further influenced adherence, highlighting the challenges faced by this patient group. Conclusions: Medication adherence post-stroke/TIA is shaped by multiple complex factors including knowledge, beliefs, attitudes, and lived experience. As a descriptive synthesis of qualitative evidence, these findings do not permit conclusions regarding causality or intervention effectiveness but provide insight into perceived barriers and facilitators that may inform future intervention development and clinical questioning.
11 February 2026