- Article
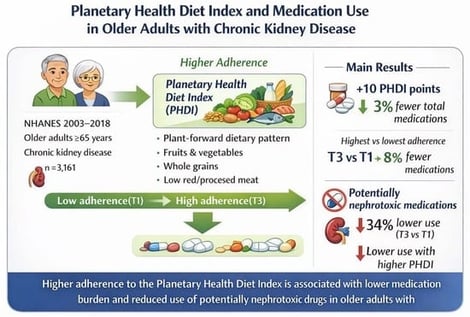
Planetary Health Diet Adherence and Medication Use in Older Adults with Chronic Kidney Disease: A Cross-Sectional Study
- Luca Soraci,
- Guido Gembillo and
- Andrea Corsonello
- + 7 authors
Background/Objectives: Chronic kidney disease (CKD) in older adults is frequently accompanied by substantial medication burden, increasing risks of adverse drug events and poor adherence. The Planetary Health Diet Index (PHDI), emphasizing plant-based foods and sustainable dietary patterns, may improve cardiometabolic health and reduce medication requirements. This study examined the association between PHD adherence as measured by the PHDI and medication burden among older adults with CKD. Methods: We analyzed cross-sectional data from the National Health and Nutrition Examination Survey (NHANES) 2003–2018 cycles. Older individuals aged ≥ 65 years with CKD (estimated glomerular filtration rate < 60 mL/min/1.73 m2 or albumin-to-creatinine ratio > 30 mg/g) at the baseline visit were included (n = 3161). PHDI scores (0–150) were calculated from two consecutive 24 h dietary recalls. Medication burden was assessed as the total prescription medication count and frequency of individual classes. Multivariable Poisson regression models evaluated associations between PHDI score and number of prescribed medications, adjusting for sociodemographic, lifestyle, and clinical covariates; logistic regression models were used to evaluate the association between PHDI score and specific medication classes. Results: Mean (SD) age was 75.0 (5.5) years; mean PHDI score was 62.4 (18.7). Participants in the highest PHDI tertile had significantly lower medication burden compared to the lowest tertile. In fully adjusted Poisson regression models, each 10-point increase in PHDI score was associated with 3% fewer medications (RR: 0.97, 95% CI: 0.96–0.99, p = 0.011). Participants in the highest PHDI tertile had 8% fewer medications compared to the lowest tertile (RR: 0.92, 95% CI: 0.87–0.98, p = 0.013). Higher PHDI scores were significantly associated with lower odds of proton pump inhibitor use (OR: 0.86, 95% CI: 0.79–0.94 per 10-point increase) and nonsteroidal anti-inflammatory drug prescription (OR: 0.86, 95% CI: 0.76–0.97 per 10-point increase). Participants in the highest PHDI tertile had 34% lower odds of PPI use (OR: 0.66, 95% CI: 0.49–0.89) and nonsignificant lower odds of NSAID use (OR: 0.67, 95% CI: 0.40–1.11) compared to those in the lowest tertile. Conclusions: Higher PHDI adherence was independently associated with lower medication burden in older adults with CKD. These findings suggest that plant-forward, sustainable dietary patterns may reduce pharmacological complexity in this vulnerable population. Prospective studies are needed to assess causality and clinical implementation strategies.
5 February 2026