- Case Report
Mucocutaneous Findings Highlighting Multisystem Inflammatory Syndrome in a Child Following SARS-CoV-2 Infection: A Case Report
- Ramosaj Morina Atifete,
- Beqiraj Qendresa and
- Baloku Zejnullahu Arbana
- + 2 authors
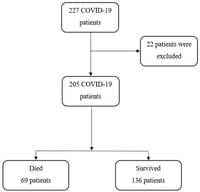
A rare but potentially fatal hyperinflammatory disease that develops following SARS-CoV-2 infection is called multisystem inflammatory syndrome in children (MIS-C). Mucocutaneous manifestations are common and frequently overlap with other pediatric inflammatory illnesses, including Kawasaki disease, and may serve as early diagnostic indicators. We describe a 6-year-old girl who was previously healthy but was hospitalized in the pediatric intensive care unit due to a high-grade fever, toxic appearance, and quickly progressing mucocutaneous symptoms, such as bilateral non-purulent conjunctivitis and broad maculopapular rash. Myocardial dysfunction, severe anemia and thrombocytopenia, respiratory failure necessitating mechanical ventilation, and hypotensive shock complicated the clinical course. Laboratory tests showed positive SARS-CoV-2 serology and significantly increased inflammatory markers. Several microbiological tests came up negative. Bacterial sepsis and Kawasaki diseases were not included. A diagnosis of MIS-C was made based on clinical, laboratory, and epidemiological data. In addition to supportive intensive care, the patient received systemic corticosteroids and intravenous immunoglobulin. After two weeks, she was released in a stable condition after gradually improving clinically and biochemically. This instance emphasizes how crucial it is to identify noticeable mucocutaneous manifestations as early warning signs of MIS-C. Immunomodulatory therapy must be started as soon as possible in order to minimize serious consequences and enhance the prognosis of afflicted infants.
18 February 2026