- Case Report
Fatal Postoperative Deterioration Consistent with Sepsis After Burr-Hole Drainage for Chronic Subdural Hematoma in a Frail Older Adult with Diabetes: Suspected Abdominal Source and a Failure-to-Rescue Case Highlighting Delayed Abdominal Assessment
- Yuta Arakaki,
- Takuto Nishihara and
- Nobuo Kutsuna
- + 2 authors
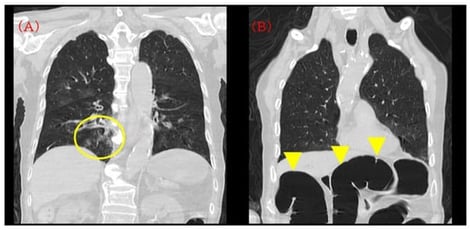
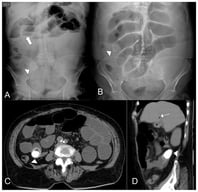
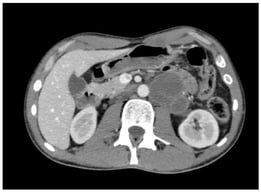
Chronic subdural hematoma (CSDH) in frail older adults is increasingly recognized as a sentinel event, with mortality often driven by medical complications rather than neurosurgical factors. We report a failure-to-rescue case in which rapid postoperative deterioration occurred after burr-hole drainage for bilateral CSDH in a frail older adult with diabetes. A clinical picture consistent with sepsis was suspected, and a gastrointestinal source was considered, but the infectious focus could not be confirmed due to limited diagnostic work-up. On admission, chest-computed tomography showed mild right lower-lobe pneumonia, and incidental transverse colonic dilatation was also visible. Burr-hole drainage was uneventful and oxygenation rapidly normalized on room air. On postoperative day (POD) 3, the patient developed a high fever (39 °C), rising C-reactive protein (CRP; 14 mg/dL), abrupt leukopenia (15,300 → 3300/µL), and, several hours later, profuse watery diarrhea. At that time, an evaluation for an infectious source and escalation of therapy (e.g., blood cultures, serum lactate, and abdominal imaging) were not performed. In the early hours of POD 4, he suffered sudden desaturation, shock, and cardiac arrest, and died despite resuscitation. A portable radiograph after intubation showed no new diffuse pulmonary infiltrates but marked colonic gas distension. This case highlights the need to reassess diagnostic framing when discordant postoperative “red flags” emerge and proposes practical triggers for early sepsis evaluation and escalation—prioritizing early recognition and timely rescue rather than a definitive determination of the cause of death—in high-risk CSDH patients.
2 February 2026