- Article
Parental Attitudes Towards Vaccination in Children with Inflammatory Bowel Disease: A Comparative Study
- Svetlana I. Erdes,
- Ivan S. Samolygo and
- Marina A. Manina
- + 8 authors
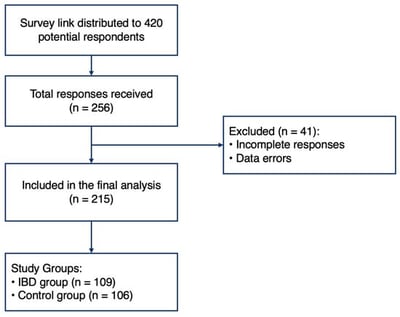
Objective: To evaluate parental attitudes towards vaccination in children with inflammatory bowel disease (IBD), assess the level of adherence to immunization schedules, and identify key barriers hindering vaccination. Materials and Methods: A comparative survey was conducted involving 215 respondents, divided into an IBD group (109 parents of children with IBD) and a control group (106 parents of healthy children). The majority of respondents were mothers (96%) with higher education (81% and 79%, respectively) residing in a major metropolitan area. We assessed demographic data, vaccination history of both children and parents, sources of medical information, and reasons for vaccine refusal. Results: Routine vaccination coverage in children under 6 years of age was high and comparable in both groups (>93%). The majority of parents in the IBD group (n = 68; 62%) expressed a positive attitude towards vaccination. However, following the onset of IBD, only 24 (22%) continued vaccination, while 85 (78%) reported a categorical refusal to continue immunization. It was found that parents tend to misinterpret normal post-vaccination reactions as vaccine complications. A significant factor contributing to refusal is the lack of information from attending physicians and reliance on the Internet as a primary information source. Additionally, low rates of adult revaccination were noted, with over 30% of parents in both groups not being vaccinated in adulthood. Conclusions: The low vaccination rate in children with IBD after disease onset is driven not by initial anti-vaccination sentiment, but by acquired fears and a lack of professional communication from primary care providers and specialists. Improving immunization coverage requires the active implementation of educational programs for parents regarding vaccine safety during immunosuppressive therapy, as well as the development of specific guidelines for attending physicians.
7 February 2026