Plasma Biomarkers for Hypertension-Mediated Organ Damage Detection: A Narrative Review
Abstract
1. Introduction
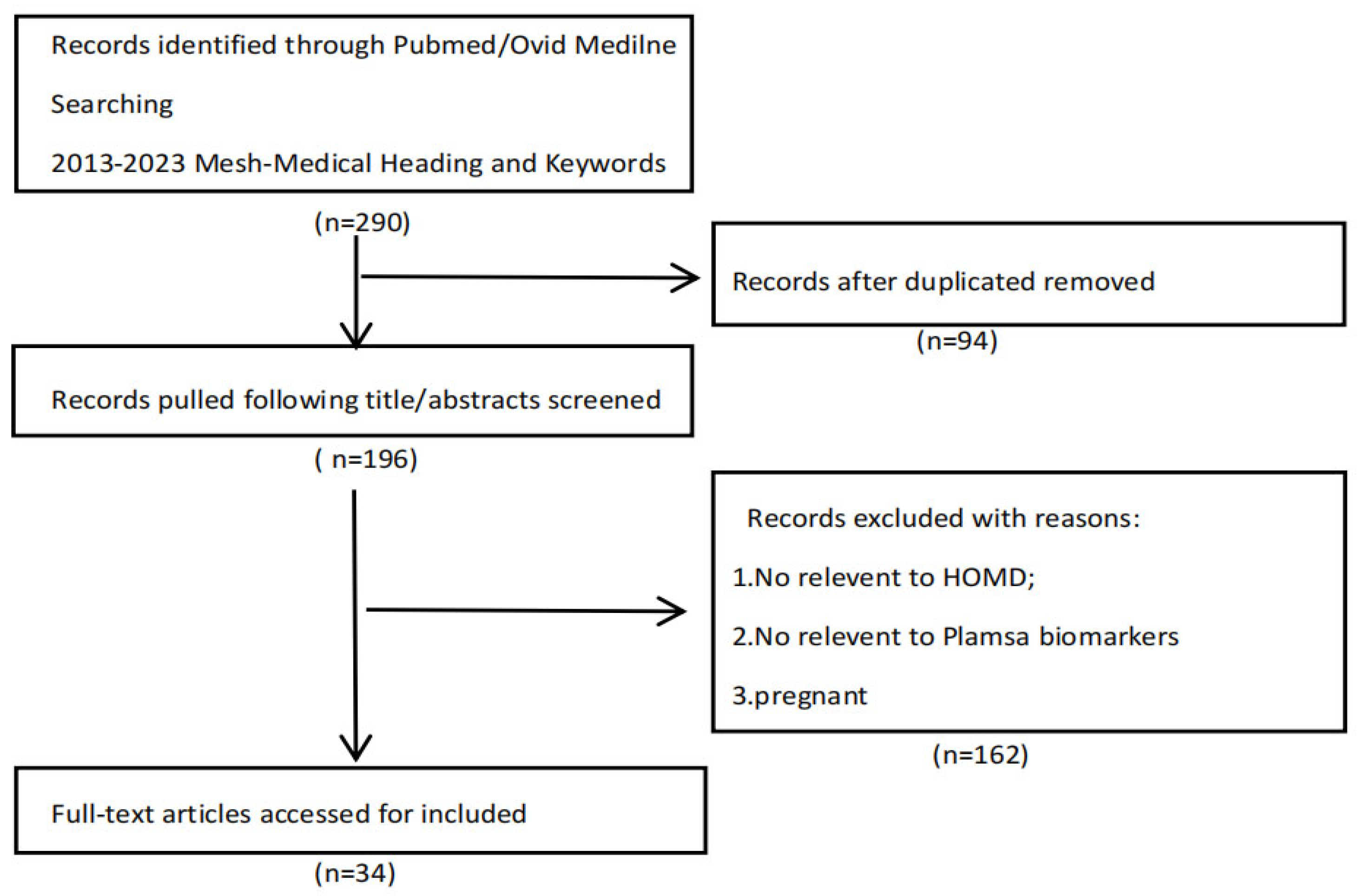
2. Methods
3. Biomarkers of Interest
3.1. Interleukins
3.1.1. IL-1β
3.1.2. IL-17A
3.1.3. IL-21
3.1.4. IL-22
3.2. C-Reactive Protein
3.3. Adiponectin
3.4. Complement
3.5. Natriuretic Peptides
3.6. Matrix Metalloproteinases (MMPs)
3.7. Cardiotrophin 1
3.8. Neutrophil Gelatinase-Associated Lipocalin
3.9. Circular Ribonucleic Acids
3.10. MicroRNAs
3.11. Other
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Meng, X.; Sun, H.; Tu, X.; Li, W. The Predictive Role of Hematological Parameters in Hypertension. Angiology 2023, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.M.; Wright, J.S. A National Commitment to Improve the Care of Patients with Hypertension in the US. JAMA 2020, 324, 1825–1826. [Google Scholar] [CrossRef] [PubMed]
- Hengel, F.E.; Sommer, C.; Wenzel, U. Arterielle Hypertonie—Eine Übersicht für den ärztlichen Alltag. Dtsch. Med. Wochenschr. 2022, 147, 414–428. [Google Scholar] [CrossRef] [PubMed]
- Shalaeva, E.V.; Messerli, F.H. What is resistant arterial hypertension? Blood Press. 2023, 32, 2185457. [Google Scholar] [CrossRef] [PubMed]
- Collaborators, G.B.D.N. Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 459–480. [Google Scholar] [CrossRef] [PubMed]
- Rizzoni, D.; Agabiti-Rosei, C.; De Ciuceis, C.; Boari, G.E.M. Subclinical Hypertension-Mediated Organ Damage (HMOD) in Hypertension: Atherosclerotic Cardiovascular Disease (ASCVD) and Calcium Score. High. Blood Press. Cardiovasc. Prev. 2023, 30, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G.; Kreutz, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J. Hypertens. 2023, 41, 1874–2071. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [CrossRef]
- Orejudo, M.; García-Redondo, A.B.; Rodrigues-Diez, R.R.; Rodrigues-Díez, R.; Santos-Sanchez, L.; Tejera-Muñoz, A.; Egido, J.; Selgas, R.; Salaices, M.; Briones, A.M.; et al. Interleukin-17A induces vascular remodeling of small arteries and blood pressure elevation. Clin. Sci. 2020, 134, 513–527. [Google Scholar] [CrossRef]
- Dale, B.L.; Pandey, A.K.; Chen, Y.; Smart, C.D.; Laroumanie, F.; Ao, M.; Xiao, L.; Dikalova, A.E.; Dikalov, S.I.; Elijovich, F.; et al. Critical role of Interleukin 21 and T follicular helper cells in hypertension and vascular dysfunction. JCI Insight 2019, 4, e129278. [Google Scholar] [CrossRef]
- Wang, W.; Lu, Y.; Hu, X.; Li, H.; Li, X.; Xiao, C.; Meng, T.; Peng, L.; Gan, L.; Zhou, Q.; et al. Interleukin-22 exacerbates angiotensin II-induced hypertensive renal injury. Int. Immunopharmacol. 2022, 109, 108840. [Google Scholar] [CrossRef]
- Chen, X.H.; Ruan, C.C.; Ge, Q.; Ma, Y.; Xu, J.Z.; Zhang, Z.B.; Lin, J.R.; Chen, D.R.; Zhu, D.L.; Gao, P.J. Deficiency of Complement C3a and C5a Receptors Prevents Angiotensin II-Induced Hypertension via Regulatory T Cells. Circ. Res. 2018, 122, 970–983. [Google Scholar] [CrossRef]
- Barbaro, N.R.; Fontana, V.; Modolo, R.; De Faria, A.P.; Sabbatini, A.R.; Fonseca, F.H.; Anhê, G.F.; Moreno, H. Increased arterial stiffness in resistant hypertension is associated with inflammatory biomarkers. Blood Press. 2015, 24, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, J.; Yang, P.; Song, X.; Li, Y. Elevated Th17 cell proportion, related cytokines and mRNA expression level in patients with hypertension-mediated organ damage: A case control study. BMC Cardiovasc. Disord. 2022, 22, 257. [Google Scholar] [CrossRef]
- Lu, Y.; Peng, L.; Li, X.; Li, H.; Zhou, Q.; Xiao, P.; Tang, R. Changes in serum IL-22 level in patients with hypertensive renal damage and its clinical significance. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2019, 44, 871–877. [Google Scholar] [CrossRef]
- He, L.; Fan, C.; Li, G. The relationship between serum C-reactive protein and senile hypertension. BMC Cardiovasc. Disord. 2022, 22, 500. [Google Scholar] [CrossRef] [PubMed]
- Armas-Padron, A.M.; Sicilia-Sosvilla, M.; Ruiz-Esteban, P.; Torres, A.; Hernandez, D. Association between Cardiovascular Health, C-Reactive Protein, and Comorbidities in Spanish Urban-Dwelling Overweight/Obese Hypertensive Patients. J. Cardiovasc. Dev. Dis. 2023, 10, 300. [Google Scholar] [CrossRef] [PubMed]
- Timmermans, S.; Abdul-Hamid, M.A.; Vanderlocht, J.; Damoiseaux, J.; Reutelingsperger, C.P.; van Paassen, P. Patients with hypertension-associated thrombotic microangiopathy may present with complement abnormalities. Kidney Int. 2017, 91, 1420–1425. [Google Scholar] [CrossRef]
- Sabbatini, A.R.; Faria, A.P.; Barbaro, N.R.; Gordo, W.M.; Modolo, R.G.; Pinho, C.; Fontana, V.; Moreno, H. Deregulation of adipokines related to target organ damage on resistant hypertension. J. Hum. Hypertens. 2014, 28, 388–392. [Google Scholar] [CrossRef]
- Çelik, M.; Nar, R.; Nar, G.; Sökmen, E.; Günver, G. Serum omentin-1 levels in hypertensive patients. J. Hum. Hypertens. 2021, 35, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Su, Z.; Tian, S.; Liang, W. Circulating CTRP1 Levels Are Increased and Associated with the STOD in Essential Hypertension in Chinese Patients. Cardiovasc. Ther. 2019, 2019, 4183781. [Google Scholar] [CrossRef] [PubMed]
- Satoh, M.; Hosaka, M.; Asayama, K.; Kikuya, M.; Inoue, R.; Metoki, H.; Tsubota-Utsugi, M.; Hara, A.; Hirose, T.; Obara, T.; et al. Association between N-terminal pro B-type natriuretic peptide and day-to-day blood pressure and heart rate variability in a general population: The Ohasama study. J. Hypertens. 2015, 33, 1536–1541. [Google Scholar] [CrossRef] [PubMed]
- Lyngbæk, S.; Winkel, P.; Gøtze, J.P.; Kastrup, J.; Gluud, C.; Kolmos, H.J.; Kjøller, E.; Jensen, G.B.; Hansen, J.F.; Hildebrandt, P.; et al. Risk stratification in stable coronary artery disease is possible at cardiac troponin levels below conventional detection and is improved by use of N-terminal pro-B-type natriuretic peptide. Eur. J. Prev. Cardiol. 2014, 21, 1275–1284. [Google Scholar] [CrossRef] [PubMed]
- Poortvliet, R.K.; van Peet, P.G.; de Craen, A.J.; Mertens, B.J.; Mooijaart, S.P.; Wijsman, L.W.; Drewes, Y.M.; Ford, I.; Sattar, N.; Jukema, J.W.; et al. Risk stratification and treatment effect of statins in secondary cardiovascular prevention in old age: Additive value of N-terminal pro-B-type natriuretic peptide. Eur. J. Prev. Cardiol. 2016, 23, 1104–1113. [Google Scholar] [CrossRef] [PubMed]
- Welsh, P.; Poulter, N.R.; Chang, C.L.; Sever, P.S.; Sattar, N. The value of N-terminal pro-B-type natriuretic peptide in determining antihypertensive benefit: Observations from the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT). Hypertension 2014, 63, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Courand, P.Y.; Harbaoui, B.; Bècle, C.; Mouly-Bertin, C.; Lantelme, P. Plasma NT-proBNP mirrors the deleterious cardiovascular and renal continuum in hypertension. Eur. J. Prev. Cardiol. 2017, 24, 452–459. [Google Scholar] [CrossRef]
- Valente, F.M.; de Andrade, D.O.; Cosenso-Martin, L.N.; Cesarino, C.B.; Guimarães, S.M.; Guimarães, V.B.; Lacchini, R.; Tanus-Santos, J.E.; Yugar-Toledo, J.C.; Vilela-Martin, J.F. Plasma levels of matrix metalloproteinase-9 are elevated in individuals with hypertensive crisis. BMC Cardiovasc. Disord. 2020, 20, 132. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sánchez, E.; Navarro-García, J.A.; Aceves-Ripoll, J.; Álvarez-Llamas, G.; Segura, J.; Barderas, M.G.; Ruilope, L.M.; Ruiz-Hurtado, G. Association between renal dysfunction and metalloproteinase (MMP)-9 activity in hypertensive patients. Nefrologia 2019, 39, 184–191. [Google Scholar] [CrossRef]
- Anderson, C.L.; Brown, C.J. Variability of X chromosome inactivation: Effect on levels of TIMP1 RNA and role of DNA methylation. Hum. Genet. 2002, 110, 271–278. [Google Scholar] [CrossRef]
- Zhang, X.M.; Zhong, X.G.; Gong, J.; Tian, J.; Zhang, Y.; Chen, Y.Z.; Cui, J.; Wang, Z.Z.; Ran, S.Q.; Xiang, T.Y.; et al. Screening biomarkers for hypertensive heart disease: Analysis based on data from 7 medical institutions. Zhongguo Ying Yong Sheng Li Xue Za Zhi 2021, 37, 142–146. [Google Scholar] [CrossRef]
- Gamella-Pozuelo, L.; Fuentes-Calvo, I.; Gómez-Marcos, M.A.; Recio-Rodriguez, J.I.; Agudo-Conde, C.; Fernández-Martín, J.L.; Cannata-Andía, J.B.; López-Novoa, J.M.; García-Ortiz, L.; Martínez-Salgado, C. Plasma Cardiotrophin-1 as a Marker of Hypertension and Diabetes-Induced Target Organ Damage and Cardiovascular Risk. Medicine 2015, 94, e1218. [Google Scholar] [CrossRef] [PubMed]
- Matokhniuk, M.O.; Limanskiy, O.V.; Maiko, O.V.; Zhebel, V.; Shevchuk, O.K.; Palii, I.K. Prognostic Significance of Blood Marker of Hypertrophy—Cardiotrophin-1 When Carrying Different Variants of Its Gene in Men with Essential Hypertension. Wiadomości Lek. 2021, 74, 273–277. [Google Scholar] [CrossRef]
- Miteva, K.; Baptista, D.; Montecucco, F.; Asrih, M.; Burger, F.; Roth, A.; Fraga-Silva, R.A.; Stergiopulos, N.; Mach, F.; Brandt, K.J. Cardiotrophin-1 Deficiency Abrogates Atherosclerosis Progression. Sci. Rep. 2020, 10, 5791. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Zhang, D.D.; Feng, Y.M.; Huang, Z.Q.; Xie, Y.B.; Zhou, J.; Li, J. Relationship between morning peak phenomenon and early renal injury NGAL in H-type hypertension. Blood Press. 2022, 31, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Nurkoç, S.G.; Ünlü, S.; Şen, B.; Tefon, A.B.; Hasanreisoglu, M.; Şahinarslan, A. Neutrophil Gelatinase-Associated Lipocalin Level Can Predict Early Organ Damage in Primary Hypertensive Patients: A Pilot Study. Anatol. J. Cardiol. 2023, 27, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Qian, H.; Zhang, Z.; Tao, Z.; Xie, Y.; Yin, Y.; He, W.; Zhang, L. Association of Circular RNAs levels in blood and Essential Hypertension with Carotid Plaque. Clin. Exp. Hypertens. 2023, 45, 2180020. [Google Scholar] [CrossRef]
- Huang, Y.; Chen, J.; Zhou, Y.; Tang, S.; Li, J.; Yu, X.; Mo, Y.; Wu, Y.; Zhang, Y.; Feng, Y. Circulating miR155 expression level is positive with blood pressure parameters: Potential markers of target-organ damage. Clin. Exp. Hypertens. 2016, 38, 331–336. [Google Scholar] [CrossRef]
- Berillo, O.; Huo, K.G.; Fraulob-Aquino, J.C.; Richer, C.; Briet, M.; Boutouyrie, P.; Lipman, M.L.; Sinnett, D.; Paradis, P.; Schiffrin, E.L. Circulating let-7g-5p and miR-191-5p Are Independent Predictors of Chronic Kidney Disease in Hypertensive Patients. Am. J. Hypertens. 2020, 33, 505–513. [Google Scholar] [CrossRef]
- Kaneto, C.M.; Nascimento, J.S.; Moreira, M.C.R.; Ludovico, N.D.; Santana, A.P.; Silva, R.A.A.; Silva-Jardim, I.; Santos, J.L.; Sousa, S.M.B.; Lima, P.S.P. MicroRNA profiling identifies miR-7-5p and miR-26b-5p as differentially expressed in hypertensive patients with left ventricular hypertrophy. Braz. J. Med. Biol. Res. 2017, 50, e6211. [Google Scholar] [CrossRef]
- Huang, Y.Q.; Huang, C.; Chen, J.Y.; Li, J.; Feng, Y.Q. Plasma expression level of miRNA let-7 is positively correlated with carotid intima-media thickness in patients with essential hypertension. J. Hum. Hypertens. 2017, 31, 843–847. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Tang, S.; Ji-Yan, C.; Huang, C.; Li, J.; Cai, A.P.; Feng, Y.Q. Circulating miR-92a expression level in patients with essential hypertension: A potential marker of atherosclerosis. J. Hum. Hypertens. 2017, 31, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Mattson, D.L. Immune mechanisms of salt-sensitive hypertension and renal end-organ damage. Nat. Rev. Nephrol. 2019, 15, 290–300. [Google Scholar] [CrossRef] [PubMed]
- Perez-Morales, R.E.; Del Pino, M.D.; Valdivielso, J.M.; Ortiz, A.; Mora-Fernandez, C.; Navarro-Gonzalez, J.F. Inflammation in Diabetic Kidney Disease. Nephron 2019, 143, 12–16. [Google Scholar] [CrossRef]
- Rothman, A.M.; MacFadyen, J.; Thuren, T.; Webb, A.; Harrison, D.G.; Guzik, T.J.; Libby, P.; Glynn, R.J.; Ridker, P.M. Effects of Interleukin-1beta Inhibition on Blood Pressure, Incident Hypertension, and Residual Inflammatory Risk: A Secondary Analysis of CANTOS. Hypertension 2020, 75, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Itani, H.A.; McMaster, W.G., Jr.; Saleh, M.A.; Nazarewicz, R.R.; Mikolajczyk, T.P.; Kaszuba, A.M.; Konior, A.; Prejbisz, A.; Januszewicz, A.; Norlander, A.E.; et al. Activation of Human T Cells in Hypertension: Studies of Humanized Mice and Hypertensive Humans. Hypertension 2016, 68, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Guzik, T.J.; Touyz, R.M. Oxidative Stress, Inflammation, and Vascular Aging in Hypertension. Hypertension 2017, 70, 660–667. [Google Scholar] [CrossRef]
- Rodrigues-Diez, R.R.; Tejera-Munoz, A.; Orejudo, M.; Marquez-Exposito, L.; Santos, L.; Rayego-Mateos, S.; Cantero-Navarro, E.; Tejedor-Santamaria, L.; Marchant, V.; Ortiz, A.; et al. Interleukin-17A: Possible mediator and therapeutic target in hypertension. Nefrologia 2021, 41, 244–257. [Google Scholar] [CrossRef]
- Prinsen, J.K.; Kannankeril, P.J.; Sidorova, T.N.; Yermalitskaya, L.V.; Boutaud, O.; Zagol-Ikapitte, I.; Barnett, J.V.; Murphy, M.B.; Subati, T.; Stark, J.M.; et al. Highly Reactive Isolevuglandins Promote Atrial Fibrillation Caused by Hypertension. JACC Basic. Transl. Sci. 2020, 5, 602–615. [Google Scholar] [CrossRef]
- Saleh, M.A.; McMaster, W.G.; Wu, J.; Norlander, A.E.; Funt, S.A.; Thabet, S.R.; Kirabo, A.; Xiao, L.; Chen, W.; Itani, H.A.; et al. Lymphocyte adaptor protein LNK deficiency exacerbates hypertension and end-organ inflammation. J. Clin. Investig. 2015, 125, 1189–1202. [Google Scholar] [CrossRef]
- Carbo, A.; Olivares-Villagomez, D.; Hontecillas, R.; Bassaganya-Riera, J.; Chaturvedi, R.; Piazuelo, M.B.; Delgado, A.; Washington, M.K.; Wilson, K.T.; Algood, H.M. Systems modeling of the role of interleukin-21 in the maintenance of effector CD4+ T cell responses during chronic Helicobacter pylori infection. mBio 2014, 5, e01243-14. [Google Scholar] [CrossRef] [PubMed]
- Drummond, G.R.; Vinh, A.; Guzik, T.J.; Sobey, C.G. Immune mechanisms of hypertension. Nat. Rev. Immunol. 2019, 19, 517–532. [Google Scholar] [CrossRef] [PubMed]
- Norlander, A.E.; Madhur, M.S.; Harrison, D.G. The immunology of hypertension. J. Exp. Med. 2018, 215, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Xue, Y.; Iqbal, N.; Chan, J.; Maisel, A. Biomarkers in hypertension and their relationship with myocardial target-organ damage. Curr. Hypertens. Rep. 2014, 16, 502. [Google Scholar] [CrossRef] [PubMed]
- Kuppa, A.; Tripathi, H.; Al-Darraji, A.; Tarhuni, W.M.; Abdel-Latif, A. C-Reactive Protein Levels and Risk of Cardiovascular Diseases: A Two-Sample Bidirectional Mendelian Randomization Study. Int. J. Mol. Sci. 2023, 24, 9129. [Google Scholar] [CrossRef] [PubMed]
- Ciobanu, D.M.; Mircea, P.A.; Bala, C.; Rusu, A.; Vesa, S.; Roman, G. Intercellular adhesion molecule-1 (ICAM-1) associates with 24-hour ambulatory blood pressure variability in type 2 diabetes and controls. Cytokine 2019, 116, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Sproston, N.R.; Ashworth, J.J. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front. Immunol. 2018, 9, 754. [Google Scholar] [CrossRef] [PubMed]
- Šilhavý, J.; Zídek, V.; Landa, V.; Šimáková, M.; Mlejnek, P.; Oliyarnyk, O.; Malínská, H.; Kazdová, L.; Mancini, M.; Pravenec, M. Rosuvastatin ameliorates inflammation, renal fat accumulation, and kidney injury in transgenic spontaneously hypertensive rats expressing human C-reactive protein. Physiol. Res. 2015, 64, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Martins, Â.M.; Silva Sarto, D.A.Q.; Caproni, K.P.; Silva, J.; Silva, J.; Souza, P.S.; Dos Santos, L.; Ureña, M.J.E.; Souza Carvalho, M.D.G.; Vilas Boas, B.M.; et al. Grape juice attenuates left ventricular hypertrophy in dyslipidemic mice. PLoS ONE 2020, 15, e0238163. [Google Scholar] [CrossRef]
- Hage, F.G. C-reactive protein and hypertension. J. Hum. Hypertens. 2014, 28, 410–415. [Google Scholar] [CrossRef]
- Parida, S.; Siddharth, S.; Sharma, D. Adiponectin, Obesity, and Cancer: Clash of the Bigwigs in Health and Disease. Int. J. Mol. Sci. 2019, 20, 2519. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Hou, P.; Wu, Z.; Nie, Y. Decreased levels of serum omentin-1 in patients with inflammatory bowel disease. Med. Sci. Monit. 2015, 21, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Watanabe-Kominato, K.; Takahashi, Y.; Kojima, M.; Watanabe, R. Adipose Tissue-Derived Omentin-1 Function and Regulation. Compr. Physiol. 2017, 7, 765–781. [Google Scholar] [CrossRef] [PubMed]
- Bai, B.; Ban, B.; Liu, Z.; Zhang, M.M.; Tan, B.K.; Chen, J. Circulating C1q complement/TNF-related protein (CTRP) 1, CTRP9, CTRP12 and CTRP13 concentrations in Type 2 diabetes mellitus: In vivo regulation by glucose. PLoS ONE 2017, 12, e0172271. [Google Scholar] [CrossRef] [PubMed]
- van Hinsbergh, V.W.; Eringa, E.C. C1q/TNF-related protein 1: A novel link between visceral fat and athero-inflammation. Eur. Heart J. 2016, 37, 1772–1774. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Park, J.S.; Lee, S.; Jeong, A.L.; Oh, K.S.; Ka, H.I.; Choi, H.J.; Son, W.C.; Lee, W.Y.; Oh, S.J.; et al. CTRP1 protects against diet-induced hyperglycemia by enhancing glycolysis and fatty acid oxidation. J. Nutr. Biochem. 2016, 27, 43–52. [Google Scholar] [CrossRef]
- Pouvreau, C.; Dayre, A.; Butkowski, E.G.; de Jong, B.; Jelinek, H.F. Inflammation and oxidative stress markers in diabetes and hypertension. J. Inflamm. Res. 2018, 11, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Jeong, A.L.; Lee, S.; Park, J.S.; Buyanravjikh, S.; Kang, W.; Choi, S.; Park, C.; Han, J.; Son, W.C.; et al. C1q/TNF-alpha-Related Protein 1 (CTRP1) Maintains Blood Pressure Under Dehydration Conditions. Circ. Res. 2018, 123, e5–e19. [Google Scholar] [CrossRef] [PubMed]
- Lillegard, K.E.; Loeks-Johnson, A.C.; Opacich, J.W.; Peterson, J.M.; Bauer, A.J.; Elmquist, B.J.; Regal, R.R.; Gilbert, J.S.; Regal, J.F. Differential effects of complement activation products c3a and c5a on cardiovascular function in hypertensive pregnant rats. J. Pharmacol. Exp. Ther. 2014, 351, 344–351. [Google Scholar] [CrossRef]
- McMaster, W.G.; Kirabo, A.; Madhur, M.S.; Harrison, D.G. Inflammation, immunity, and hypertensive end-organ damage. Circ. Res. 2015, 116, 1022–1033. [Google Scholar] [CrossRef]
- Zhang, Y.; Yan, X.; Zhao, T.; Xu, Q.; Peng, Q.; Hu, R.; Quan, S.; Zhou, Y.; Xing, G. Targeting C3a/C5a receptors inhibits human mesangial cell proliferation and alleviates immunoglobulin A nephropathy in mice. Clin. Exp. Immunol. 2017, 189, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Totina, A.; Iorember, F.; El-Dahr, S.S.; Yosypiv, I.V. Atypical hemolytic-uremic syndrome in a child presenting with malignant hypertension. Clin. Pediatr. 2013, 52, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Palma, L.M.P.; Sridharan, M.; Sethi, S. Complement in Secondary Thrombotic Microangiopathy. Kidney Int. Rep. 2021, 6, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Cannone, V.; Cabassi, A.; Volpi, R.; Burnett, J.C. Atrial Natriuretic Peptide: A Molecular Target of Novel Therapeutic Approaches to Cardio-Metabolic Disease. Int. J. Mol. Sci. 2019, 20, 3265. [Google Scholar] [CrossRef] [PubMed]
- Kuwahara, K. The natriuretic peptide system in heart failure: Diagnostic and therapeutic implications. Pharmacol. Ther. 2021, 227, 107863. [Google Scholar] [CrossRef] [PubMed]
- Oremus, M.; McKelvie, R.; Don-Wauchope, A.; Santaguida, P.L.; Ali, U.; Balion, C.; Hill, S.; Booth, R.; Brown, J.A.; Bustamam, A.; et al. A systematic review of BNP and NT-proBNP in the management of heart failure: Overview and methods. Heart Fail. Rev. 2014, 19, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Jia, X.; Al Rifai, M.; Hoogeveen, R.; Echouffo-Tcheugui, J.B.; Shah, A.M.; Ndumele, C.E.; Virani, S.S.; Bozkurt, B.; Selvin, E.; Ballantyne, C.M.; et al. Association of Long-term Change in N-Terminal Pro-B-Type Natriuretic Peptide with Incident Heart Failure and Death. JAMA Cardiol. 2023, 8, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Chia, Y.C.; Kario, K.; Tomitani, N.; Park, S.; Shin, J.; Turana, Y.; Tay, J.C.; Buranakitjaroen, P.; Chen, C.H.; Hoshide, S.; et al. Comparison of day-to-day blood pressure variability in hypertensive patients with type 2 diabetes mellitus to those without diabetes: Asia BP@Home Study. J. Clin. Hypertens. 2020, 22, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.I.; Lee, M.Y.; Oh, B.K.; Lee, S.J.; Kang, J.G.; Lee, S.H.; Lee, J.Y.; Kim, B.J.; Kim, B.S.; Kang, J.H.; et al. Effects of Age, Sex, and Obesity on N-Terminal Pro B-Type Natriuretic Peptide Concentrations in the General Population. Circ. J. 2021, 85, 647–654. [Google Scholar] [CrossRef]
- Rubattu, S.; Forte, M.; Marchitti, S.; Volpe, M. Molecular Implications of Natriuretic Peptides in the Protection from Hypertension and Target Organ Damage Development. Int. J. Mol. Sci. 2019, 20, 798. [Google Scholar] [CrossRef]
- Bisogni, V.; Cerasari, A.; Pucci, G.; Vaudo, G. Matrix Metalloproteinases and Hypertension-Mediated Organ Damage: Current Insights. Integr. Blood Press. Control 2020, 13, 157–169. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.Y.; Zhang, Y.; Li, Y.; Zhu, D.L.; Gao, P.J. The association of serum inflammatory biomarkers with chronic kidney disease in hypertensive patients. Ren. Fail. 2014, 36, 666–672. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, A.; Prado, A.F.; Antonio, R.C.; Issa, J.P.; Gerlach, R.F. Matrix metalloproteinases are involved in cardiovascular diseases. Basic. Clin. Pharmacol. Toxicol. 2014, 115, 301–314. [Google Scholar] [CrossRef] [PubMed]
- Hendry, R.G.; Bilawchuk, L.M.; Marchant, D.J. Targeting matrix metalloproteinase activity and expression for the treatment of viral myocarditis. J. Cardiovasc. Transl. Res. 2014, 7, 212–225. [Google Scholar] [CrossRef]
- Gonçalves, P.R.; Nascimento, L.D.; Gerlach, R.F.; Rodrigues, K.E.; Prado, A.F. Matrix Metalloproteinase 2 as a Pharmacological Target in Heart Failure. Pharmaceuticals 2022, 15, 920. [Google Scholar] [CrossRef] [PubMed]
- Niemirska, A.; Litwin, M.; Trojanek, J.; Gackowska, L.; Kubiszewska, I.; Wierzbicka, A.; Kulaga, Z.; Michalkiewicz, J. Altered matrix metalloproteinase 9 and tissue inhibitor of metalloproteinases 1 levels in children with primary hypertension. J. Hypertens. 2016, 34, 1815–1822. [Google Scholar] [CrossRef] [PubMed]
- Song, K.; Wang, S.; Huang, B.; Luciano, A.; Srivastava, R.; Mani, A. Plasma cardiotrophin-1 levels are associated with hypertensive heart disease: A meta-analysis. J. Clin. Hypertens. 2014, 16, 686–692. [Google Scholar] [CrossRef] [PubMed]
- Moreno, M.U.; San José, G.; Pejenaute, Á.; Landecho, M.F.; Díez, J.; Beloqui, Ó.; Fortuño, A.; Zalba, G. Association of phagocytic NADPH oxidase activity with hypertensive heart disease: A role for cardiotrophin-1? Hypertension 2014, 63, 468–474. [Google Scholar] [CrossRef]
- Vlahodimitris, I.; Karangelis, D.; Moschaki, M.; Moyssakis, I.; Christodoulou, K.C.; Perrea, D.N.; Mourouzis, I.; Papadogiannis, D. Cardiotrophin-1 in Asymptomatic Hypertensive Patients with Mild Diastolic Dysfunction: Potential Prognostic Value in Early Stages of Hypertensive Heart Disease. Cureus 2023, 15, e46516. [Google Scholar] [CrossRef]
- Gharishvandi, F.; Kazerouni, F.; Ghanei, E.; Rahimipour, A.; Nasiri, M. Comparative assessment of neutrophil gelatinase-associated lipocalin (NGAL) and cystatin C as early biomarkers for early detection of renal failure in patients with hypertension. Iran. Biomed. J. 2015, 19, 76–81. [Google Scholar] [CrossRef]
- Sancho-Martínez, S.M.; Blanco-Gozalo, V.; Quiros, Y.; Prieto-García, L.; Montero-Gómez, M.J.; Docherty, N.G.; Martínez-Salgado, C.; Morales, A.I.; López-Novoa, J.M.; López-Hernández, F.J. Impaired Tubular Reabsorption Is the Main Mechanism Explaining Increases in Urinary NGAL Excretion Following Acute Kidney Injury in Rats. Toxicol. Sci. 2020, 175, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Törnblom, S.; Nisula, S.; Petäjä, L.; Vaara, S.T.; Haapio, M.; Pesonen, E.; Pettilä, V. Urine NGAL as a biomarker for septic AKI: A critical appraisal of clinical utility-data from the observational FINNAKI study. Ann. Intensive Care 2020, 10, 51. [Google Scholar] [CrossRef]
- Hjortrup, P.B.; Haase, N.; Wetterslev, M.; Perner, A. Clinical review: Predictive value of neutrophil gelatinase-associated lipocalin for acute kidney injury in intensive care patients. Crit. Care 2013, 17, 211. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhang, T.; Qin, A.; Li, F.; Zheng, Z.; Zhou, H.; Tang, Y.; Qin, W. Association of morning blood pressure surge with chronic kidney disease progression in patients with chronic kidney disease and hypertension. J. Clin. Hypertens. 2021, 23, 1879–1886. [Google Scholar] [CrossRef]
- Chen, L.L. The expanding regulatory mechanisms and cellular functions of circular RNAs. Nat. Rev. Mol. Cell Biol. 2020, 21, 475–490. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Li, Z.; Lin, C.; Zhang, J.; Shen, Z. Translation role of circRNAs in cancers. J. Clin. Lab. Anal. 2021, 35, e23866. [Google Scholar] [CrossRef]
- Dergunova, L.V.; Vinogradina, M.A.; Filippenkov, I.B.; Limborska, S.A.; Dergunov, A.D. Circular RNAs Variously Participate in Coronary Atherogenesis. Curr. Issues Mol. Biol. 2023, 45, 6682–6700. [Google Scholar] [CrossRef]
- Ali, M.K.; Schimmel, K.; Zhao, L.; Chen, C.K.; Dua, K.; Nicolls, M.R.; Spiekerkoetter, E. The role of circular RNAs in pulmonary hypertension. Eur. Respir. J. 2022, 60, 2200012. [Google Scholar] [CrossRef]
- Unfried, J.P.; Marín-Baquero, M.; Rivera-Calzada, Á.; Razquin, N.; Martín-Cuevas, E.M.; de Bragança, S.; Aicart-Ramos, C.; McCoy, C.; Prats-Mari, L.; Arribas-Bosacoma, R.; et al. Long Noncoding RNA NIHCOLE Promotes Ligation Efficiency of DNA Double-Strand Breaks in Hepatocellular Carcinoma. Cancer Res. 2021, 81, 4910–4925. [Google Scholar] [CrossRef]
- Orenes-Piñero, E.; Montoro-García, S.; Patel, J.V.; Valdés, M.; Marín, F.; Lip, G.Y. Role of microRNAs in cardiac remodelling: New insights and future perspectives. Int. J. Cardiol. 2013, 167, 1651–1659. [Google Scholar] [CrossRef]
- Natarelli, L.; Schober, A. MicroRNAs and the response to injury in atherosclerosis. Hamostaseologie 2015, 35, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Loyer, X.; Potteaux, S.; Vion, A.C.; Guérin, C.L.; Boulkroun, S.; Rautou, P.E.; Ramkhelawon, B.; Esposito, B.; Dalloz, M.; Paul, J.L.; et al. Inhibition of microRNA-92a prevents endothelial dysfunction and atherosclerosis in mice. Circ. Res. 2014, 114, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.J.; Yun, C.J.; Liu, J.; Yao, S.Y.; Li, Y.; Wang, M.; Wang, C.; Bai, Y.Y.; Xue, H. MicroRNA-29a attenuates angiotensin-II induced-left ventricular remodeling by inhibiting collagen, TGF-β and SMAD2/3 expression. J. Geriatr. Cardiol. 2020, 17, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Wang, Q.; Xing, X.; Yang, L.; Xu, M.; Cao, C.; Wang, R.; Li, W.; Niu, X.; Gao, D. The antagonistic effects and mechanisms of microRNA-26a action in hypertensive vascular remodelling. Br. J. Pharmacol. 2021, 178, 1037–1054. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Cai, W.; Xi, W.; Sun, W.; Shen, W.; Wei, T.; Chen, X.; Sun, L.; Zhou, H.; Sun, Y.; et al. MicroRNA-31 Regulates Immunosuppression in Ang II (Angiotensin II)-induced Hypertension by Targeting Ppp6C (Protein Phosphatase 6c). Hypertension 2019, 73, e14–e24. [Google Scholar] [CrossRef] [PubMed]
- Romaine, S.P.; Charchar, F.J.; Samani, N.J.; Tomaszewski, M. Circulating microRNAs and hypertension--from new insights into blood pressure regulation to biomarkers of cardiovascular risk. Curr. Opin. Pharmacol. 2016, 27, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Wang, X.; Kong, W. Hyperhomocysteinaemia and vascular injury: Advances in mechanisms and drug targets. Br. J. Pharmacol. 2018, 175, 1173–1189. [Google Scholar] [CrossRef] [PubMed]
- Maloberti, A.; Meani, P.; Vallerio, P.; Varrenti, M.; Casadei, F.; Musca, F.; Facchetti, R.; Di Blasio, A.M.; Ravassa, S.; Mancia, G.; et al. Annexin A5 in treated hypertensive patients and its association with target organ damage. J. Hypertens. 2017, 35, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Barbaro, N.R.; de Araujo, T.M.; Tanus-Santos, J.E.; Anhe, G.F.; Fontana, V.; Moreno, H. Vascular Damage in Resistant Hypertension: TNF-Alpha Inhibition Effects on Endothelial Cells. Biomed. Res. Int. 2015, 2015, 631594. [Google Scholar] [CrossRef]
- Ritter, A.M.V.; Faria, A.P.C.; Sabbatini, A.; Correa, N.B.; Brunelli, V.; Modolo, R.; Moreno, H. MCP-1 Levels are Associated with Cardiac Remodeling but not with Resistant Hypertension. Arq. Bras. Cardiol. 2017, 108, 331–338. [Google Scholar] [CrossRef]
- Cortez, A.; Muxfeldt, E. Monocyte chemoattractant protein-1 and hypertension: An overview. Hipertens. Riesgo Vasc. 2022, 39, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Maresca, A.M.; Guasti, L.; Bozzini, S.; Mongiardi, C.; Tandurella, N.; Corso, R.; Zerba, F.G.; Squizzato, A.; Campiotti, L.; Dentali, F.; et al. sRAGE and early signs of cardiac target organ damage in mild hypertensives. Cardiovasc. Diabetol. 2019, 18, 17. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Guo, Y.; Dong, Y.; Li, X.; Liu, Q.; Liu, Q.; Wang, G.; Qin, M.; Zhang, Z.; Song, J.; et al. Association of plasma bone morphogenetic protein-4 levels with arterial stiffness in hypertensive patients. J. Clin. Lab. Anal. 2022, 36, e24746. [Google Scholar] [CrossRef] [PubMed]


| Biomarkers Tested | Author, Year (Ref) | Study Type | Animal Model | Mean Age/Number | Follow-Up (Months) | Major Findings |
|---|---|---|---|---|---|---|
| IL-17A | Orejudo, 2020 [10] | Retrospective study | A murine model of continuous systemic IL-17A administration (adult male C57BL/6 mice) | 9–12 weeks old/8 | NA | IL-17A levels induced vascular remodeling and stiffness. |
| IL-21 | Dale, 2019 [11] | Retrospective study | Ang II model or DOCA-salt (WT C57BL/6J mice, CD4-Cre transgenic mice (TgCD4cre), and Bcl6fl/fl mice) | 10–12 weeks old/13 | NA | Mice deficient in IL-21 exhibit blunted hypertension and vascular end-organ dysfunction. |
| IL-22 | Wang, 2022 [12] | Retrospective study | Ang II model (C57BL/6 mice) | 8–10 weeks old/24 | NA | IL-22 levels were elevated significantly in Ang II-induced mice. Infiltrated Th22 cells proportion in kidney and IL-22 were higher than control group. |
| C3aR C5aR | Chen, 2018 [13] | Retrospective study | Ang II model (WT, C3aR−/−, And C5aR−/− mice) | 10–11 weeks old/8 | NA | C3aR and C5aR DKO-mediated Treg function prevents Ang II-induced hypertension and target organ damage. |
| Biomarkers Tested | Author, Year (Ref) | Study Type | Population | Mean Age/Number | Follow-Up (Months) | Major Findings |
|---|---|---|---|---|---|---|
| IL-1β IL-10 | Barbaro, 2014 [14] | Retrospective cross-sectional study | 32 RHTN, 20 mild HT and 20 NT patients | RHTN (57.4 ± 12.9) HT (55.1 ± 12.0) NT (51.7 ± 5.0) /72 | NA | IL-1β levels were independently associated with arterial stiffness; RHTN patients had a higher frequency of subjects with increased levels of IL-10 and IL-β compared with mild HT and NT patients. |
| IL-17A IL-23 | Wang, 2022 [15] | Retrospective study (case–control study) | 179 with hypertension-mediated organ damage and 87 without hypertension-mediated organ damage and 63 healthy participants | Control (57.3 ± 10.2) Non-HMOD (59.5 ± 9.1) HMOD (60.1 ± 7.3) /249 | NA | IL-17 and IL-23 concentrations were significantly increased in both HMOD and non-HMOD group compared with control group; IL-17 and IL-23 level in HMOD group was also higher than that in non-HMOD group. |
| IL-22 | Lu, 2019 [16] | Retrospective study | 45 hypertension and 52 hypertensive Kidney damage, 40 healthy control | Control (50.8 ± 10.2) HT (52.9 ± 8.8) HRI (54.1 ± 11.31) /137 | NA | IL-22 level increased in renal damage, a positive correlation with renal damage. |
| IL-22 | Wang, 2022 [12] | Retrospective study | Human (21 normal control, 12 newly diagnosed HRI patients and 18 HT patients without renal injury | Control (53.3 ± 8.4) HT (50.7 ± 9.6) HRI (52.1 ± 12.5) /51 | NA | Compared with control and HT group, IL-22 level in patients with hypertensive renal injury. |
| CRP | He, 2022 [17] | Retrospective study (cross- sectional) | Hospitalized patients aged over 65 | Elevated CRP 72.5 (68.0, 78.0) Normal CRP 73.0 (68.3, 77.0) /196 | NA | An elevated CRP level in hypertensive patients. |
| Hs-CRP | Armas-Padrón, 2023 [18] | Prospective (longitudinal cohort study) | Hypertension | Overall (68.5 ± 13.0) Tertile 1 (69.5 ± 13.0) Tertile 2 (67.2 ± 13.3) Tertile 3 (39.2 ± 12.9) /243 | 24 | Hs-CRP levels correlated with the HMOD. |
| C5b-9 | Timmermans, 2016 [19] | Cohort study | Malignant hypertension | (27.9, 65.0) /9 | NA | C5b-9 levels increased in malignant hypertension |
| Biomarkers Tested | Author, Year (Ref) | Study Type | Population | Mean Age/Number | Follow-Up (Months) | Major Findings |
|---|---|---|---|---|---|---|
| Adiponectin | Sabbatini, 2014 [20] | Retrospective study (cross-sectional) | 51 CRHTN and 38 UCRHTN) | CRHTN (58.5 ± 10.5) UCRHTN (56.1 ± 11.3) /89 | 6 | Uncontrolled BP had higher arterial stiffness, MA, LVH as well as higher levels of adipokines, such as leptin and resistin, and lower levels of adiponectin; arterial stiffness correlated with adiponectin and leptin, and MA was associated with adiponectin. |
| Omentin-1 | Çelik, 2021 [21] | Retrospective study (single-center and cross-sectional) | 61 new EH and 60 healthy normotensive individuals | Control (46.52 ± 11.82) Stage 1 HT (51.47 ± 7.96) Stage 2 HT (53.77 ± 11.70) /121 | NA | Omentin 1 levels were decreased in renal vascular injury. |
| CTRP1 IL-6 | Su, 2019 [22] | Retrospective study | 360 patients with EH and 360 healthy subjects | Control (58.91 ± 13.16) HT (58.27 ± 15.08) /720 | NA | CTRP1, TNF-α, and IL-6 levels were found to increase in HMOD; IL-6 and the organ damage risk was only in LVH group; CTRP1 levels were elevated according to the severity of STOD. |
| Biomarkers Tested | Author, Year (Ref) | Study Type | Population | Mean Age/Number | Follow-Up (Months) | Major Findings |
|---|---|---|---|---|---|---|
| NT-proBNP | Satoh, 2015 [23] | Retrospective study (cross-sectional study) | Community- based cohort | NT-proBNP <125 pg/mL (60.4 ± 9.9) NT-proBNP ≥ 125 pg/mL (72.0 ± 8.3) /664 | NA | An elevated NT-proBNP level may be associated with target organ damage or complications and day-to-day variability in BP or heart rate. |
| NT-proBNP | Lyngbæk, 2014 [24] | Prospective | Hypertension | All (65.3 ± 10.3) /4197 | 30 | NT-proBNP levels are associated with increased cardiovascular risk. |
| NT-proBNP | Poortvliet, 2016 [25] | Prospective | Hypertension | All (73.3 ± 10.8) /5804 | 38 | NT-proBNP improves prediction of recurrent cardiovascular disease, cardiovascular mortality. |
| NT-proBNP | Welsh, 2014 [26] | Prospective | Hypertension | All (61.3 ± 10.8) Men (62.8 ± 20.3) Women (65.0 ± 18.3) 18.3)/1852 | 30 | NT-proBNP level independently predicted subsequent CVD risk. |
| NT-proBNP | Courand, 2017 [27] | Retrospective study (cross-sectional study) | Hypertension | All (50.3 ± 23.8) Men (50.6 ± 23.3) Women (50.0 ± 24.3) /837 | NA | NT-proBNP levels were independently correlated with PWV, LVH and eGFR; NT-proBNP levels increased gradually according to the number of target organs damaged; NT-proBNP levels were independently associated with sex; daytime NT-proBNP levels were slightly higher than nighttime NT-proBNP levels. |
| Biomarkers Tested | Author, Year (Ref) | Study Type | Population | Mean Age/Number | Follow-Up (Months) | Major Findings |
|---|---|---|---|---|---|---|
| MMP-9 | Valente, 2020 [28] | Retrospective study (cross-sectional study) | 40 normotensive and 58 controlled hypertensive subjects, 57 patients with hypertensive emergency and 43 in hypertensive urgency | NT (43.5 ± 10.2) CHyp (57.7 ± 7.4) HypUrg (59.4 ± 15.6) HypEmerg (62.4 ± 14.3) /198 | NA | MMP-9 concentrations are significantly higher in the hypertensive crisis groups (urgency and emergency) compared to the control groups. |
| MMP-9, MMP-1 | Niemirska,2016 [29] | Retrospective study (case–control study) | 109 children with untreated primary and 74 healthy children | HT (15.6 ± 1.5) Control (15.3 ± 1.6) HT girls (15.9 ± 1.4) HT boys (15.6 ± 1.6) Control girls (15.5 ± 1.3) Control boys (15.1 ± 1.6) /183 | NA | Hypertensive boys increased MMP-9 and TIMP-1 in comparison with age- and BMI-matched group of normotensive boys; TIMP-1 concentrations tended to be greater in children with metabolic syndrome and with MMP-9 correlated with HDL-C; TIMP-1 levels were increased within hypertensive children with arterial stiffness. |
| MMP-9, MMP-1 | Rodríguez-Sánchez, 2019 [30] | Descriptive study | Hypertension | eGFR > 90 mL/1/1.73 min/m2 (59.3 ± 9.2) eGFR 90–60 mL/1/1.73 min/m2 (62.7 ± 9.0) eGFR 60–30 mL/1/1.73 min/m2 (74.6 ± 4.9) /37 | NA | TIMP-1, active MMP-9, and MMP-9–TIMP-1 interaction correlate significantly with the decline in renal function. |
| Biomarkers Tested | Author, Year (Ref) | Study Type | Population | Mean Age/Number | Follow-Up (Months) | Major Findings |
|---|---|---|---|---|---|---|
| CT-1 | Vlahodimitris, 2023 [31] | Retrospective study | Hypertension | HT (56.0 ± 5.0) Control (52.0 ± 3.5)/60 | NA | Levels of CT-1 were not affected by left ventricular hypertrophy; elevated CT-1 levels were affected by mild diastolic dysfunction. |
| CT-1 | Gamella-Pozuelo, 2015 [32] | Retrospective study (cross-sectional study) | Hypertension and diabetes | Control (56.17 ± 9.79) HT (58.43 ± 10.56) DM (59.61 ± 9.58)/384 | NA | CT-1 levels are higher in the presence than in the absence of LVH; HT groups with renal damage have higher plasma CT-1 than without renal Damage; CT-1 levels indicative of vascular damage such as PWV. |
| CT-1 | Moreno, 2013 [33] | Retrospective study | Hypertension | NT(50.0 ± 2.0) HT with LVH (59.0 ± 1.0) HT without LVH (56.0 ± 1.0)/140 | NA | CT-1 levels were increased in hypertensive patients with LVH compared with normotensive subjects and hypertensive patients without LVH. |
| CT-1 | Matokhniuk, 2021 [34] | Retrospective study | Male hypertension | Control (48.81 ± 0.78) HT with LVH (50.65 ± 0.46) CHF (50.62 ± 0.73) /170 | NA | CT-1 levels ≥ 122,895 pg/mL can be used for early diagnosis of myocardial changes such as LVH; the cutoff level is ≥303.81 pg/mL for screening diagnosis of CHF. |
| Biomarkers Tested | Author, Year (Ref) | Study Type | Population | Mean Age/Number | Follow-Up (Months) | Major Findings |
|---|---|---|---|---|---|---|
| NGAL | Zhang, 2022 [35] | Retrospective study | Hypertension and hyperhomocystinemia | MBPS (64.69 ± 7.87) Non-MBPS (62.90 ± 8.48) /224 | NA | Systolic morning peak the most significant factor affecting NGAL levels; NGAL is reflected in early renal impairment. |
| NGAL | Nurkoç, 2023 [36] | Retrospective study (single-center and polit study) | Hypertension | Control (50.7 ± 8.9) HT (52.8 ± 7.2) /67 | NA | Global longitudinal strain and NGAL demonstrated a high correlation. |
| Biomarkers Tested | Author, Year (Ref) | Study Type | Population | Mean Age/Number | Follow-Up (Months) | Major Findings |
|---|---|---|---|---|---|---|
| CircRNAs | Qian, 2023 [37] | Retrospective (case–control study) | 64 healthy controls, 64 EH patients, and 64 EH patients with carotid plaque | Control (55.20 ± 9.54) HT (57.83 ± 10.82) HT with Carotid plaque (57.93 ± 10.66) /192 | NA | Three circRNAs (hsa_circ_0124782, hsa_circ_0131618 and hsa_circ_0127342) and HT with carotid plaque; Levels of hsa_circ_0124782 were upregulated, hsa_circ_0131618 and hsa_circ_0127342 were downregulated in HT patients with carotid plaque. |
| miRNAs | Berillo, 2020 [38] | Retrospective (case–control study) | 16 patients with EH, 15 with EH associated with other features of the MetS, and 16 With EH or CKD | NT (52.0 ± 11.0) HT (59.0 ± 10.0) MetS (62.0 ± 6.0) CKD (66.0 ± 7.0) /62 | NA | Decreased circulating let-7g-5p and miR-191-5p as independent biomarkers of CKD among patients with HT. |
| miR155 | Huang, 2016 [39] | Retrospective (case–control study) | 50 patients with essential hypertension and 30 healthy individuals | Control (53.20 ± 5.71) HT (55.28 ± 8.03) /80 | NA | MiR155 showed a positive association with 24 h mean SBP, 24 h mean DBP and 24 h mean PP the positive correlation between miR155 with LVH of all the participants. |
| miR-7–5p miR-26b-5p | Kaneto, 2017 [40] | Retrospective (matched case–control study) | 8 hypertensive patients with LVH, 28 hypertensive patients without LVH and 23 healthy Subjects control, 3 hypertensive patients with LVH, 4 hypertensive patients without LVH and 4 normal subjects | Control (46.8 ± 4.7) HT (52.8 ± 9.6) HT with LVH (57.6 ± 2.5) /69 | NA | Circulating levels of miR-7-5p and miR-26b-5p were elevated in LVH hypertensive patients. |
| Let-7 | Huang, 2017 [41] | Retrospective (cross-sectional study) | 240 participants including 60 healthy volunteers with nCIMT, 60 healthy volunteers with iCIMT, 60 hypertension patients with nCIMT and 60 hypertension patients with iCIMT | All (50.35 ± 5.58) Healthy with nCIMT (49.65 ± 5.79) Healty with iCIMT (50.65 ± 6.01) HT with nCIMT (50.00 ± 5.74) HT with iCIMT (51.08 ± 4.69) /240 | NA | Hypertensive and atherosclerosis subjects had significantly higher let-7 expression level than controls Correlation of let-7 expression in plasma with CIMT. |
| miR-92a | Huang, 2017 [42] | Retrospective (cross-sectional study) | 60 healthy volunteers with nCIMT, 60 healthy volunteers with iCIMT, 60 hypertensive patients with nCIMT and 60 hypertensive patients with iCIMT | Healthy with nCIMT (49.65 ± 5.79) Healty with iCIMT (50.65 ± 6.01) HT with nCIMT (50.00 ± 5.74) HT with iCIMT (51.08 ± 4.69) /240 | NA | Hypertensive and atherosclerosis subjects had significantly higher miR-92a expression level than controls; positive correlations between miR-92a expression and CIMT. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, X.; Yang, M.; Lip, G.Y.H.; McDowell, G. Plasma Biomarkers for Hypertension-Mediated Organ Damage Detection: A Narrative Review. Biomedicines 2024, 12, 1071. https://doi.org/10.3390/biomedicines12051071
Liu X, Yang M, Lip GYH, McDowell G. Plasma Biomarkers for Hypertension-Mediated Organ Damage Detection: A Narrative Review. Biomedicines. 2024; 12(5):1071. https://doi.org/10.3390/biomedicines12051071
Chicago/Turabian StyleLiu, Xinghui, Miao Yang, Gregory Y. H. Lip, and Garry McDowell. 2024. "Plasma Biomarkers for Hypertension-Mediated Organ Damage Detection: A Narrative Review" Biomedicines 12, no. 5: 1071. https://doi.org/10.3390/biomedicines12051071
APA StyleLiu, X., Yang, M., Lip, G. Y. H., & McDowell, G. (2024). Plasma Biomarkers for Hypertension-Mediated Organ Damage Detection: A Narrative Review. Biomedicines, 12(5), 1071. https://doi.org/10.3390/biomedicines12051071







