Value-Based Health Care for Prostate Cancer Centers by Implementing Specific Key Performance Indicators Using a Balanced Score Card
Abstract
1. Introduction
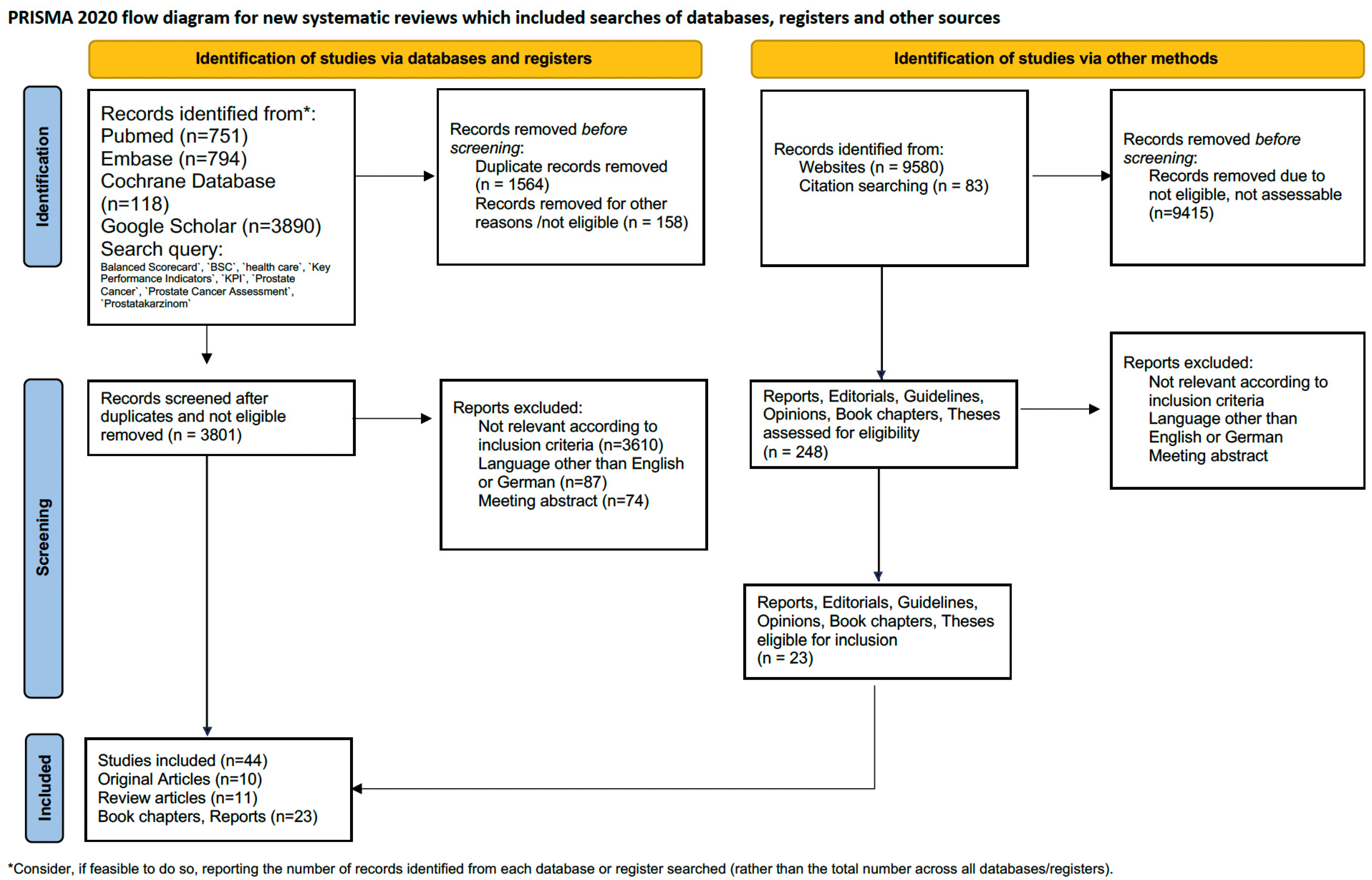
2. Material and Methods
3. Results
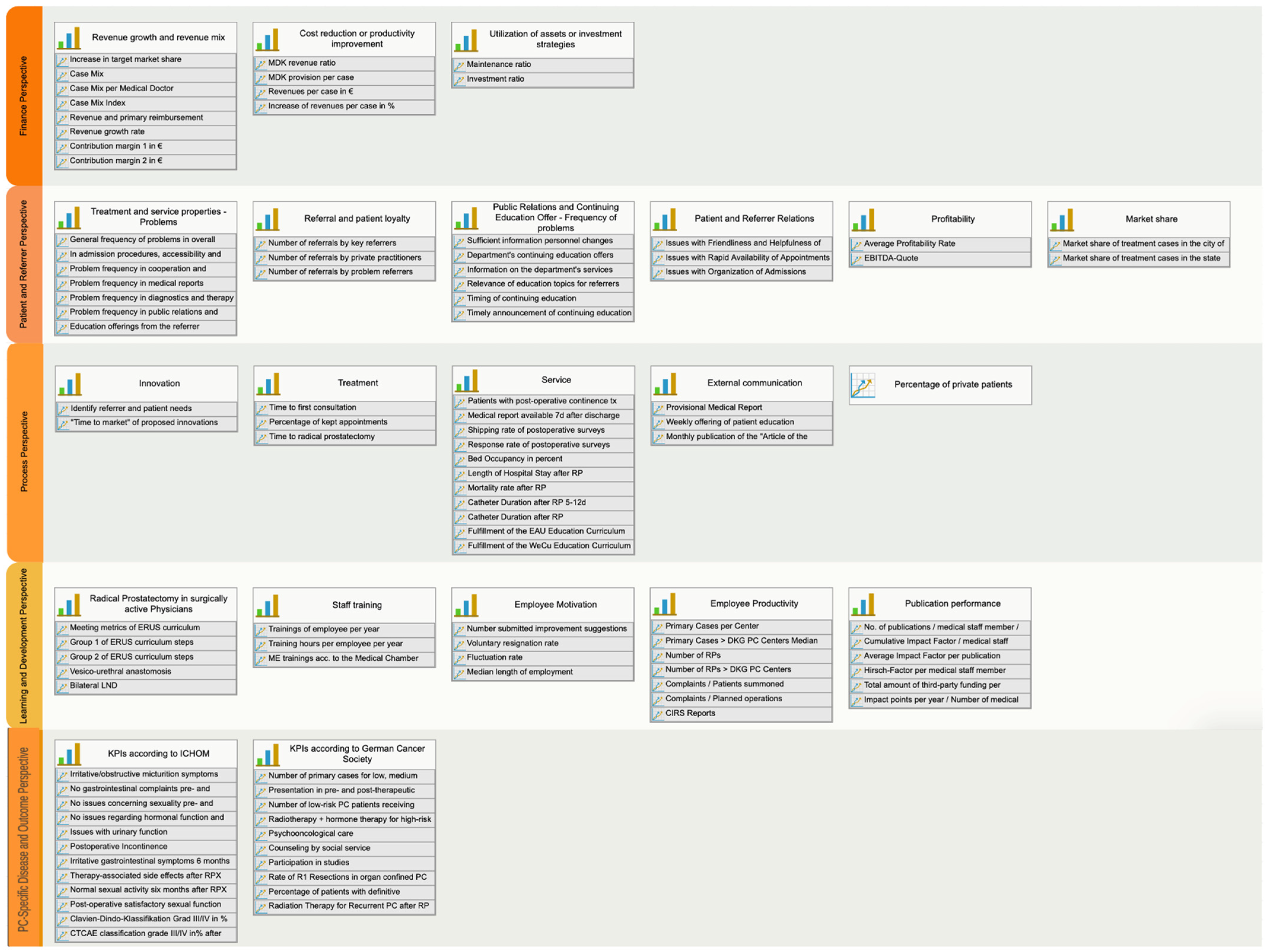
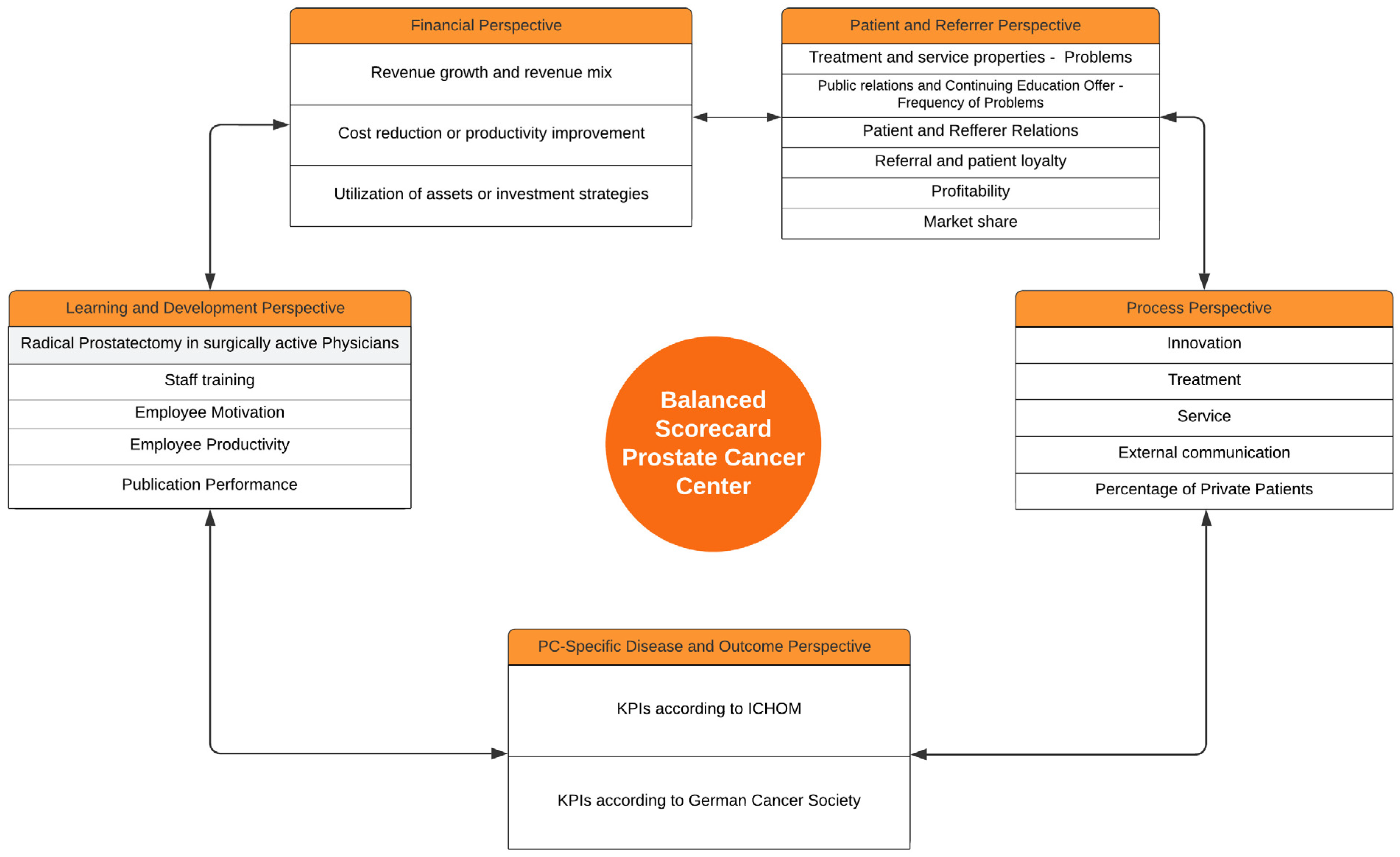
3.1. Financial Perspective
- Revenue growth and revenue mix;
- Cost reduction or productivity improvement;
- Utilization of assets or investment strategies.
| Key Performance Indicators of Financial Perspective | Benchmark | Aim | Reference |
|---|---|---|---|
| Revenue growth and revenue mix | |||
| Increase in target market share | 19% | 25% | [31,32] |
| Case Mix | 1440 | Increase | [32] |
| Case Mix per full-time physician | 116 | 142 | [33] |
| Case Mix Index | 1.72 | 2.27 | [33] |
| Revenue and primary reimbursement | 10,703,328.00 | Increase | [32] |
| Revenue growth rate | 13% | 5% per Year | [32] |
| Contribution margin 1 in EUR | 2,106,766.00 | [32] | |
| Contribution margin 2 in EUR | −869,441.00 | 0 | [32] |
| Cost reduction or productivity improvement | |||
| MDK revenue ratio | 2.10% | Increase | [31] |
| MDK provision per case | 94 | [31] | |
| Revenues per case in EUR | 4806 | Increase | [32] |
| Increase in revenues per case in % | 7% | 5% per Jahr | [32] |
| Assets or investment strategies | [32] | ||
| Maintenance ratio | 3.30% | −0.60% | [31] |
| Investment ratio | 13.20% | Increase | [31] |
3.2. Patient and Referrer Perspective (Table 2 and Figure 2)
| Key Performance Indicators of Patient and Referrer Perspective | Benchmark | Aim | Reference |
|---|---|---|---|
| Treatment and service properties | |||
| General frequency of problems in terms of overall quality | 32% | Reduction | [34] |
| Problem frequency in admission procedures, accessibility and organization | 26% | Reduction | [34] |
| Problem frequency in cooperation and information | 62% | Reduction | [34] |
| Problem frequency in medical reports | 24% | Reduction | [34] |
| Problem frequency in diagnostics and therapy | 40% | Reduction | [34] |
| Problem frequency in public relations and continuing | 57% | Reduction | [34] |
| Education offerings from the referrer perspective | |||
| Referral and patient loyalty | |||
| Number of referrals by key referrers | Referral of last year | Increase | [35] |
| Number of referrals by private practitioners with potential | Referral of last year | Increase | [35] |
| Number of referrals by problem referrers | Referral of last year | Reduction | [35] |
| Public Relations and Continuing Education Offer | |||
| Frequency of problems regarding sufficient information about personnel changes in the department | 86% | Reduction to 50% | [34] |
| Frequency of problems regarding the department’s continuing education offers | 71% | Reduction to 25% | [34] |
| Frequency of problems regarding information on the department’s services | 55% | Reduction to 25% | [34] |
| Frequency of problems regarding the relevance of continuing education topics for referrers | 42% | Reduction <10% | [34] |
| Frequency of problems regarding timing of continuing education | 58% | Reduction to 20% | [34] |
| Frequency of problems regarding timely announcement of continuing education | 23% | Reduction <10% | [34] |
| Patient and Referrer Relations | |||
| Frequency of Issues with Friendliness and Helpfulness of Personnel | 26% | Reduction to 20% | [34] |
| Issues with Rapid Availability of Appointments | 17% | Reduction | [34] |
| Frequency of Issues with Organization of Admissions Process | 33% | Reduction | [34] |
| Profitability | |||
| Average Profitability Rate | 0.40% | 0.40% | [31] |
| EBITDA-Quote | 3.60% | 3.60% | [31] |
| Market share | |||
| Market share of treatment cases in the city of the center | 19.00% | 25% | http://www.lzg.nrw.de (accessed on 21 December 2021) |
| Market share of treatment cases in the state of the center | 0.01% | Increase | http://www.lzg.nrw.de (accessed on 21 December 2021) |
3.3. Process Perspective
3.3.1. Innovation
3.3.2. Treatment
3.3.3. Service
3.3.4. Communication
3.3.5. Additional KPIs in the Process Perspective
| Key Performance Indicators of the Process Perspective | Benchmark | Aim | Reference |
|---|---|---|---|
| Innovation | |||
| Identify referrer and patient needs | 75% | 75% | [1] |
| “Time to market” of implementation of 75% of proposed innovations | [1] | ||
| Treatment | |||
| Time to first consultation | 14 days | 14 days | [30] |
| Percentage of kept appointments | >90% | >90% | [37] |
| Time to radical prostatectomy | 4–6 weeks | 4–6 weeks | [30] |
| Service | |||
| Patients with post-operative continence training | 100% | 100% | [30] |
| Time until dispatch of completed medical report to referrer after discharge | 7 days | 7 days | [30] |
| Shipping rate of postoperative surveys (Clavien-Dindo classification, EPIC-26 and EORTC-QLQ-25 6 months postoperatively to Patients) | 100% | 100% | [30] |
| Response rate of postoperative surveys (Clavien-Dindo classification, EPIC-26 and EORTC-QLQ-25 6 months postoperatively to Patients) | >75% | >75% | [30] |
| Bed Occupancy in percent | 85–90% | 85–90% | [44] |
| Length of Hospital Stay after Radical Prostatectomy | 5 days | 5 days | [30] |
| Mortality rate after Radical Prostatectomy | <1% | <1% | [44] |
| Catheter Duration after Radical Prostatectomy 5–12 days in % of patients | >95% | >95% | [46] |
| Readmission rate after Radical Prostatectomy | <8% | <8% | [45] |
| Fulfillment of the Continuing Education Curriculum of the EAU | 100% | 100% | [48] |
| Fulfillment of the Continuing Education Curriculum of the DGU (WeCu) | 100% | 100% | [47] |
| External communication | |||
| Provisional Medical Report upon discharge, as a percentage of all patients | 100% | 100% | [30] |
| Weekly offering of patient education during hospital stay, in % | 100% | 100% | [30] |
| Monthly publication of the “Article of the Month” | 100% | 100% | [30] |
| Percentage of private patients | 29% | >3.6% | [31] |
3.4. Learning and Development Perspective
| Key Performance Indicators of the Learning and Development Perspective | Benchmark | Aim | Reference |
|---|---|---|---|
| Radical Prostatectomy in surgically active Physicians | |||
| Meeting the 17 metrics of standardized training in robotic radical prostatectomy according to ERUS requirements per operator | 100% | 100% | [48] |
| Group 1 of the ERUS standardized radical prostatectomy with set-up, patient positioning, establishment of pneumoperitonium, adhesion lysis and docking | 100% | 100% | [48] |
| Group 2: Opening peritoneum, endopelvine fasci preparation, dorsal vein plexus suturing, anterior and posterior prostate and prostatic pillar dissection, nerve-vascular bundle preparation and apical dissection of the prostate | 100% | 100% | [48] |
| Vesico-urethral anastomosis and anterior reconstruction | 100% | 100% | [48] |
| Bilateral pelvic lymph node dissection and finalization of the operation | 100% | 100% | [48] |
| Staff training | |||
| Number of trainings per employee per year, including those specified by the DKG: Fire Protection, MANV, Data Protection, IT Security, Hygiene, Occupational Safety, Radiation Protection, 1 freely chosen training | 8 | ≥8 | [16,20] |
| Training hours per employee per year | 19.6 | ≥19.6 | [50] |
| ME trainings according to the Medical Chamber (200 h in 5 years for Medical Employees), compliance in % of the employees | 100 | 100 | Federal Medical Chamber |
| Employee Motivation | |||
| Number of submitted improvement suggestions/number of employees per month | Comparison pre-month | [52] | |
| Voluntary resignation rate | Comparison pre-year | Reduction | [52] |
| Fluctuation rate | Comparison pre-year | Reduction | [52] |
| Median length of employment of employees in years | Comparison pre-year | [52] | |
| Employee Productivity | |||
| Number of Primary Cases per Center | >100 | >100 | [16,20] |
| Number of Primary Cases > DKG Prostate Centers Median | >159 | >159 | [16,20] |
| Number of Radical Prostatectomies | >50 | >50 | [16,20] |
| Number of Radical Prostatectomies > DKG Prostate Centers | >79 | >79 | [16,20] |
| Number of Complaints/Number of Patients Summoned | <15% | <15% | [51] |
| Number of Complaints/Number of Planned Operations | Comparison pre-year | Reduction | [51] |
| Number of CIRS Reports | Comparison pre-year | Reduction | [51] |
| Publication performance | |||
| Number of publications per medical staff member per year | Comparison pre-year | Increase | [51] |
| Cumulative Impact Factor per medical staff member per year | Comparison pre-year | Increase | [51] |
| Average Impact Factor per publication | Comparison pre-year | Increase | [51] |
| Hirsch-Factor per medical staff member | Comparison pre-year | Increase | [51] |
| Total amount of third-party funding per medical staff member | Comparison pre-year | Increase | [51] |
| Impact points per year/Number of medical staff members | Comparison pre-year | Increase | [51] |
3.5. PC-Specific Disease and Outcome Perspective (Table 5 and Figure 2)
| Key Performance Indicators of the PC-Specific Disease and Outcome Perspective | Benchmark | Aim | Reference |
|---|---|---|---|
| No unwanted urine leakage pre- and post-therapy | 92–94%/63–77% | >63–77% | [19] |
| Irritative/obstructive micturition symptoms pre- and post-therapy | 80–87%/89–95% | ≤89–95% | [19] |
| No gastrointestinal complaints pre- and post-therapy | 92–95%/89–95% | ≥89–95% | [19] |
| No issues concerning sexuality pre- and post-therapy | 48–66%/14–30% | >14–30% | [19] |
| No issues regarding hormonal function and vitality (hot flashes, depression, fatigue) pre- and post-therapy | 81–90%/72–87% | >72–87% | [19] |
| Issues with urinary function | 15% | ≤15% | [16,19,20] |
| Postoperative Incontinence | 8% | ≤8% | [16,19,20] |
| Irritative gastrointestinal symptoms 6 months post-operatively | 5% | ≤5% | [16,19,20] |
| Therapy-associated side effects after RPX | 10–12% | ≤10–12% | [16,19,20] |
| Normal sexual activity six months after RPX | 35% | ≥35% | [19] |
| Post-operative satisfactory sexual function | 40% | ≥40% | [19] |
| Clavien-Dindo-Classification Grade III/IV in % after RPX | 6.50% | ≤6.50% | [16,19,20] |
| CTCAE classification grade III/IV in% after radiation therapy | 0% | 0% | [16,19,20] |
| Number of primary cases for low, medium and high risk PC, median per year | 29/51/42 | >Median | [16,20] |
| Presentation in pre- and post-therapeutic tumor conferences | 95%/100% | ≥95%/100% | [16,20] |
| Number of low-risk carcinoma patients receiving active surveillance, median | 21% | ≥21% | [16,20] |
| Radiotherapy + hormone therapy for high-risk PC | ≥75% | ≥75% | [16,20] |
| Psychooncological care, median | ≥20% | ≥20% | [16,20] |
| Counseling by social service, median | ≥50% | ≥50% | [16,20] |
| Participation in studies, in % of patients | ≥5% | ≥5% | [16,20] |
| Rate of R1 Resections in organ confined PC | <10% | <10% | [16,20] |
| Percentage of patients with definitive radiotherapy per center | ≥17% | ≥17% | [16,20] |
| Radiation Therapy for Recurrent PC after RP with PSA less than 0.5 ng/mL | 70% | ≥70% | [16,20] |
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BSC | Balanced Scorecard |
| CM | Case Mix |
| CME | Continuing Medical Education |
| CMI | Case Mix Index |
| DGU | Deutsche Gesellschaft für Urologie |
| DKG | German Cancer Society, Deutsche Krebsgesellschaft |
| DRG | Diagnosis related groups |
| EAU | European Association of Urology |
| EBIT | Earnings Before Interests and Taxes |
| EBITDA | Earnings Before Interests, Taxes, Depreciation and Amortisation |
| EORTC | European Organisation for Research and Treatment of Cancer |
| EPIC | Common Terminology Criteria of Adverse Events |
| G-BA | Gemeinsamer Bundesausschuss, |
| ICHOM | International Consortium for Health Outcome Measurement |
| IPP | Impact Factor per Publication |
| IPU | Integrated Practice Unit |
| KPI | Key Performance Indicator |
| MDK | Medical Service of Statutory Health Insurance Funds |
| PC | Prostate Cancer |
| PIT | Population-Index Test-Condition |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROM | Patient-related Outcome Measurement |
| PWC | PricewaterhouseCoopers International |
| QUADAS | Quality Assessment of Diagnostic Accuracy Studies |
| RP | Radical Prostatectomy |
| RT | Radiotherapy |
| WeCu | Weiterbildungscurriculum |
References
- Weimann, E.; Weimann, P. High Performance im Krankenhausmanagement; Springer: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Weimann, E.; Weimann, P. Die “Balanced Scorecard“ in Praxis und Krankenhaus. Pneumologe 2012, 9, 289–294. [Google Scholar] [CrossRef]
- Brinkmann, A.; Gebhard, F.; Isenmann, R.; Bothner, U.; Mohl, U.; Schwilk, B. Balanced Scorecard. Anaesthesist 2003, 52, 947–956. [Google Scholar] [CrossRef] [PubMed]
- Bade, M. Die Balanced Scorecard als strategisches Management-Instrument einer Medizinischen Fakultät. Medical. Doctoral Thesis, University Hospital Münster, Münster, Germany, 2007. [Google Scholar]
- Porter, M.E. A Strategy for Health Care Reform—Toward a Value-Based System. N. Engl. J. Med. 2009, 361, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Falter, E.B. Redefining Health Care. Nurs. Adm. Q. 2007, 31, 267–268. [Google Scholar] [CrossRef]
- Porter, M.E.; Larsson, S.; Lee, T.H. Standardizing Patient Outcomes Measurement. N. Engl. J. Med. 2016, 374, 504–506. [Google Scholar] [CrossRef]
- Porter, M.E.; Lee, T.H. The Strategy That Will Fix Health Care. Harv. Bus. Rev. 2013, 91, 50–70. [Google Scholar]
- van Harten, W.H. Turning teams and pathways into integrated practice units: Appearance characteristics and added value. Int. J. Care Coord. 2018, 21, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Wind, A.; Gonçalves, F.R.; Marosi, E.; Da Pieve, L.; Groza, M.; Asioli, M.; Albini, M.; Van Harten, W. Benchmarking cancer centers: From care pathways to integrated practice units. JNCCN J. Natl. Compr. Cancer Netw. 2018, 16, 1075–1083. [Google Scholar] [CrossRef]
- Saghatchian, M.; Thonon, F.; Boomsma, F.; Hummel, H.; Koot, B.; Harrison, C.; Rajan, A.; de Valeriola, D.; Otter, R.; Laranja Pontes, J.; et al. Pioneering Quality Assessment in European Cancer Centers: A Data Analysis of the Organization for European Cancer Institutes Accreditation and Designation Program. J. Oncol. Pract. 2014, 10, e342–e349. [Google Scholar] [CrossRef]
- Kaplan, R.S.; Norton, D.P. Balanced Scorecard. XXIV; Kaplan, R.S., Norton, D.P., Eds.; Schäffer-Poeschel: Stuttgart, Germany, 1997; Volume 1. [Google Scholar]
- Sant, M.; Capocaccia, R.; Verdecchia, A.; Estève, J.; Gatta, G.; Micheli, A.; Coleman, M.P.; Berrino, F.; EUROCARE Working Group. Survival of women with breast cancer in Europe: Variation with age, year of diagnosis and country. Int. J. Cancer 1998, 77, 679–683. [Google Scholar] [CrossRef]
- Kowalski, C.; Ferencz, J.; Albers, P.; Fichtner, J.; Wiegel, T.; Feick, G.; Wesselmann, S. Quality assessment in prostate cancer centers certified by the German Cancer Society. World J. Urol. 2016, 34, 665–672. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, C.; Ferencz, J.; Brucker, S.Y.; Kreienberg, R.; Wesselmann, S. Quality of care in breast cancer centers: Results of benchmarking by the German Cancer Society and German Society for Breast Diseases. Breast 2015, 24, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Burchhardt, M.; Fichtner, J. Catalogue of Requirements for Prostate Cancer Centers. 2020. Available online: https://www.krebsgesellschaft.de/zertdokumente.html?file=files/dkg/deutsche-krebsgesellschaft/content/pdf/Zertifizierung/Erhebungs-und-Kennzahlenboegen/eb_pz-K1_190910.docx&cid=16519 (accessed on 14 March 2024).
- Sikic, D.; Fiebig, C.; Wullich, B.; Wolff, I.; Hoschke, B.; Manseck, A.; Gillitzer, R.; Burger, M.; Steinestel, J.; Harke, N.; et al. Patient Benefits of Radical Prostatectomy in Certified Prostate Cancer Centers: Comparative Results from the Multicenter IMPROVE Study. Urol. Int. 2023, 107, 949–958. [Google Scholar] [CrossRef]
- James, N.D.; Tannock, I.; N’Dow, J.; Feng, F.; Gillessen, S.; Ali, S.A.; Trujillo, B.; Al-Lazikani, B.; Attard, G.; Bray, F.; et al. The Lancet Commission on prostate cancer: Planning for the surge in cases. Lancet 2024, 403, 1683–1722. [Google Scholar] [CrossRef]
- International Consortium for Health Outcomes Measurement (ICHOM). Localized Prostate Cancer Data Collection Reference Guide Version 2.0.5; ICHOM: Boston, MA, USA, 2017. [Google Scholar]
- Burchhardt, M.; Fichtner, J.; Wesselmann, S.; Rückher, J.; Utzig, M.; Jörg, V.; Dudu, F. Jahresbericht der zertifizierten Prostatakrebszentren—Auditjahr 2021/Kennzahlenjahr 2020; Deutsche Krebsgesellschaft e.V.: Berlin, Germany, 2023. [Google Scholar]
- Panzer, R.J.; Gitomer, R.S.; Greene, W.H.; Webster, P.R.; Landry, K.R.; Riccobono, C.A. Increasing demands for quality measurement. JAMA 2013, 310, 1971–1980. [Google Scholar] [CrossRef] [PubMed]
- Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft DKA). S3-Leitlinie Prostatakarzinom, Langversion 6.2; Leitlinienprogramm Onkologie: Berlin, Germany, 2021. [Google Scholar]
- Gori, D.; Dulal, R.; Blayney, D.W.; Brooks, J.D.; Fantini, M.P.; McDonald, K.M.; Hernandez-Boussard, T. Utilization of Prostate Cancer Quality Metrics for Research and Quality Improvement: A Structured Review. Jt. Comm. J. Qual. Patient Saf. 2019, 45, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Huland, H.; Graefen, M.; Deerberg-Wittram, J. Das Martini-Prinzip; Huland, H., Graefen, M., Deerberg-Wittram, J., Eds.; MWV Medizinisch Wissenschaftliche Verlagsgesellschaft: Berlin, Germany, 2018; Volume 1. [Google Scholar]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of Surgical Complications. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Sterne, J.A.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Porter, M.E.; Deerberg-Wittram, J.; Feeley, T.W. Martini Klinik: Prostate Cancer Care 2019. Harv. Bus. Sch. Case 2019, 1–23. [Google Scholar]
- Friedl, C. Krankenhäuser im Vergleich—Finanzkennzahlen 2019; PwC Deutschland: Berlin, Germany, 2019. [Google Scholar]
- University Hospital Essen. Contribution Margin Report; University Hospital Essen: Essen, Germany, 2019. [Google Scholar]
- Runkel, F.G. Die Martini-Klinik am UKE Hamburg. UroForum 2016, 3, 1–4. Available online: www.martini-klinik.de (accessed on 14 March 2024).
- PICKER Institut Deutschland gGmbh. Ergebnisse der Einweiserbefragung; PICKER Institut Deutschland gGmbh: Hamburg, Germany, 2019. [Google Scholar]
- Raab, A. Drissner Al Der strategische Planungsprozess: Wie entwickelt ein Krankenhaus eine Einweiserstrategie? In Einweiserbeziehungsmanagement Stuttgart; W. Kohlhammer GmbH: Stuttgart, Germany, 2011; pp. 32–85. [Google Scholar]
- Burghardt, K. Einweiser- und Patientenbeziehungsmanagement im Krankenhaus; Braun, G.E., Selbmann, H.K., Eds.; Springer-Gabler: Wiesbaden, Germany, 2016; pp. 245–257. [Google Scholar]
- Catuogno, S.; Arena, C.; Saggese, S.; Sarto, F. Balanced performance measurement in research hospitals: The participative case study of a haematology department. BMC Health Serv. Res. 2017, 17, 522. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.D.; Haeuser, L.; Paciotti, M.; Reitblat, C.; Cellini, J.; Lipsitz, S.R.; Kibel, A.S.; Choudhury, A.D.; Cone, E.B.; Trinh, Q.D. Systematic Review of Time to Definitive Treatment for Intermediate Risk and High Risk Prostate Cancer: Are Delays Associated with Worse Outcomes? J. Urol. 2021, 205, 1263–1274. [Google Scholar] [CrossRef] [PubMed]
- Milios, J.E.; Ackland, T.R.; Green, D.J. Pelvic floor muscle training in radical prostatectomy: A randomized controlled trial of the impacts on pelvic floor muscle function and urinary incontinence. BMC Urol. 2019, 19, 16. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.I.; Lam, V.; Patel, M.I. Preoperative Pelvic Floor Muscle Exercise and Postprostatectomy Incontinence: A Systematic Review and Meta-analysis. Eur. Urol. 2016, 69, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, C.; Carl, G.; Feick, G.; Wesselmann, S. The Prostate Cancer Outcomes (PCO) study in prostate cancer centres certified by the German Cancer Society. Strahlenther. Und Onkol. 2021, 197, 116–117. [Google Scholar] [CrossRef] [PubMed]
- Kuntz, L.; Mennicken, R.; Scholtes, S. Stress on the ward: Evidence of safety tipping points in hospitals. Manag. Sci. 2015, 61, 754–771. [Google Scholar] [CrossRef]
- Institut für das Entgeltsystem im Krankenhaus (InEK). Diagnosis-Related Groups Catalog; InEK: Siegburg, Germany, 2020. [Google Scholar]
- Touijer, K.A.; Karnes, R.J.; Passoni, N.; Sjoberg, D.D.; Assel, M.; Fossati, N.; Gandaglia, G.; Eastham, J.A.; Scardino, P.T.; Vickers, A.; et al. Survival Outcomes of Men with Lymph Node-positive Prostate Cancer After Radical Prostatectomy: A Comparative Analysis of Different Postoperative Management Strategies. Eur. Urol. 2018, 73, 890–896. [Google Scholar] [CrossRef] [PubMed]
- Yaxley, J.W.; Coughlin, G.D.; Chambers, S.K.; Occhipinti, S.; Samaratunga, H.; Zajdlewicz, L.; Dunglison, N.; Carter, R.; Williams, S.; Payton, D.J.; et al. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: Early outcomes from a randomised controlled phase 3 study. Lancet 2016, 388, 1057–1066. [Google Scholar] [CrossRef] [PubMed]
- Haese, A.; Knipper, S.; Isbarn, H.; Heinzer, H.; Tilki, D.; Salomon, G.; Michl, U.; Steuber, T.; Budäus, L.; Maurer, T.; et al. A comparative study of robot-assisted and open radical prostatectomy in 10 790 men treated by highly trained surgeons for both procedures. BJU Int. 2019, 123, 1031–1040. [Google Scholar] [CrossRef]
- Michel, M.S.; Himmler, M.; Necknig, U.; Kriegmair, M.; Speck, T.; Fichtner, J.; Steffens, J.; Borgmann, H.; Bolenz, C.; Tuellmann, M.; et al. Certified residency curriculum for the specialization training in urology from the German Society of Urology according to the 2018 Training Regulations (version of 20. September 2019). Urologe 2020, 59, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Lovegrove, C.; Novara, G.; Mottrie, A.; Guru, K.A.; Brown, M.; Challacombe, B.; Popert, R.; Raza, J.; Van der Poel, H.; Peabody, J.; et al. Structured and Modular Training Pathway for Robot-assisted Radical Prostatectomy (RARP): Validation of the RARP Assessment Score and Learning Curve Assessment. Eur. Urol. 2016, 69, 526–535. [Google Scholar] [CrossRef]
- Ryan, J.P.; Lynch, O.; Broe, M.P.; Swan, N.; Moran, D.; McGuire, B.; Mulvin, D. Robotic-assisted radical prostatectomy—Impact of a mentorship program on oncological outcomes during the learning curve. Ir. J. Med. Sci. 2022, 191, 479–484. [Google Scholar] [CrossRef]
- Seyda, S.; Placke, B. The 9th IW Survey of Further Training–The Costs and Benefits of Continuing Vocational Training in Enterprises. IW-Trends 2017, 4, 1–19. [Google Scholar]
- Donnelly, L.F.; Gessner, K.E.; Dickerson, J.M.; Koch, B.L.; Towbin, A.J.; Lehkamp, T.W.; Moskovitz, J.; Brody, A.S.; Dumoulin, C.L.; Jones, B.V. Quality initiatives department scorecard: A Tool to help drive imaging care delivery performance. Radiographics 2010, 30, 2029–2038. [Google Scholar] [CrossRef] [PubMed]
- Havighorst, F. Personalkennzahlen; Hans-Böckler-Stiftung: Düsseldorf, Germany, 2006. [Google Scholar]
- Salzburger Landeskliniken—Stabsstelle für Qualitätsmanagement und Riskmanagemt. Statusbericht 2010/2011 [Internet]. 2010. Available online: www.salk.at (accessed on 21 December 2021).
- Agarwal, A.; Durairajanayagam, D.; Tatagari, S.; Esteves, S.C.; Harlev, A.; Henkel, R.; Roychoudhury, S.; Homa, S.; Puchalt, N.G.; Ramasamy, R.; et al. Bibliometrics: Tracking research impact by selecting the appropriate metrics. Asian J. Androl. 2016, 18, 296–309. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, C.R.; Cone, D.C.; Sarli, C.C. Using publication metrics to highlight academic productivity and research impact. Acad. Emerg. Med. 2014, 21, 1160–1172. [Google Scholar] [CrossRef]
- Wolff, I.; Burchardt, M.; Peter, J.; Thomas, C.; Sikic, D.; Fiebig, C.; Promnitz, S.; Hoschke, B.; Burger, M.; Schnabel, M.J.; et al. Patient’s Desire and Real Availability Concerning Supportive Measures Accompanying Radical Prostatectomy: Differences between Certified Prostate Cancer Centers and Non-Certified Centers Based on Patient-Reported Outcomes within the Cross-Sectional Study Improve. Cancers 2023, 15, 2830. [Google Scholar] [CrossRef]
- Pompe, R.S.; Tian, Z.; Preisser, F.; Tennstedt, P.; Beyer, B.; Michl, U.; Graefen, M.; Huland, H.; Karakiewicz, P.I.; Tilki, D. Short- and Long-term Functional Outcomes and Quality of Life after Radical Prostatectomy: Patient-reported Outcomes from a Tertiary High-volume Center. Eur. Urol. Focus. 2017, 3, 615–620. [Google Scholar] [CrossRef] [PubMed]
- Irusen, H.; Fernandez, P.; Van der Merwe, A.; Suliman, S.; Esterhuizen, T.; Lazarus, J.; Parkes, J.; Seedat, S. Depression, Anxiety, and Their Association to Health-Related Quality of Life in Men Commencing Prostate Cancer Treatment at Tertiary Hospitals in Cape Town, South Africa. Cancer Control 2022, 29, 10732748221125561. [Google Scholar] [CrossRef] [PubMed]
- Sibert, N.T.; Breidenbach, C.; Dieng, S.; Oesterle, A.; Horvath, E.; Roth, R.; Feick, G.; Carl, G.; Burchardt, M.; Fichtner, J.; et al. Ergebnisbericht an die Studienzentren Dezember 2020 Prostate Cancer Outcomes (PCO) Studie; Deutsche Krebsgesellschaft: Berlin, Germany, 2020. [Google Scholar]
- Sibert, N.T.; Kurth, T.; Breidenbach, C.; Wesselmann, S.; Feick, G.; Carl, E.G.; Dieng, S.; Albarghouth, M.H.; Aziz, A.; Baltes, S.; et al. Prediction models of incontinence and sexual function one year after radical prostatectomy based on data from 20 164 prostate cancer patients. PLoS ONE 2023, 18, e0295179. [Google Scholar] [CrossRef] [PubMed]
- Donabedian, A. The Quality of Care—How Can It Be Assessed? JAMA 1988, 260, 1743–1748. [Google Scholar] [CrossRef]
- Berg, W.T.; Danzig, M.R.; Pak, J.S.; Korets, R.; RoyChoudhury, A.; Hruby, G.; Benson, M.C.; McKiernan, J.M.; Badani, K.K. Delay from biopsy to radical prostatectomy influences the rate of adverse pathologic outcomes. Prostate 2015, 75, 1085–1091. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radtke, J.P.; Albers, P.; Hadaschik, B.A.; Graefen, M.; Meyer, C.P.; Behr, B.; Nüesch, S. Value-Based Health Care for Prostate Cancer Centers by Implementing Specific Key Performance Indicators Using a Balanced Score Card. Healthcare 2024, 12, 991. https://doi.org/10.3390/healthcare12100991
Radtke JP, Albers P, Hadaschik BA, Graefen M, Meyer CP, Behr B, Nüesch S. Value-Based Health Care for Prostate Cancer Centers by Implementing Specific Key Performance Indicators Using a Balanced Score Card. Healthcare. 2024; 12(10):991. https://doi.org/10.3390/healthcare12100991
Chicago/Turabian StyleRadtke, Jan Philipp, Peter Albers, Boris A. Hadaschik, Markus Graefen, Christian P. Meyer, Björn Behr, and Stephan Nüesch. 2024. "Value-Based Health Care for Prostate Cancer Centers by Implementing Specific Key Performance Indicators Using a Balanced Score Card" Healthcare 12, no. 10: 991. https://doi.org/10.3390/healthcare12100991
APA StyleRadtke, J. P., Albers, P., Hadaschik, B. A., Graefen, M., Meyer, C. P., Behr, B., & Nüesch, S. (2024). Value-Based Health Care for Prostate Cancer Centers by Implementing Specific Key Performance Indicators Using a Balanced Score Card. Healthcare, 12(10), 991. https://doi.org/10.3390/healthcare12100991






