Production of PEGylated Vancomycin-Loaded Niosomes by a Continuous Supercritical CO2 Assisted Process
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. SuperSomes Process and Plant Description
2.3. Characterization Analyses
3. Results and Discussion
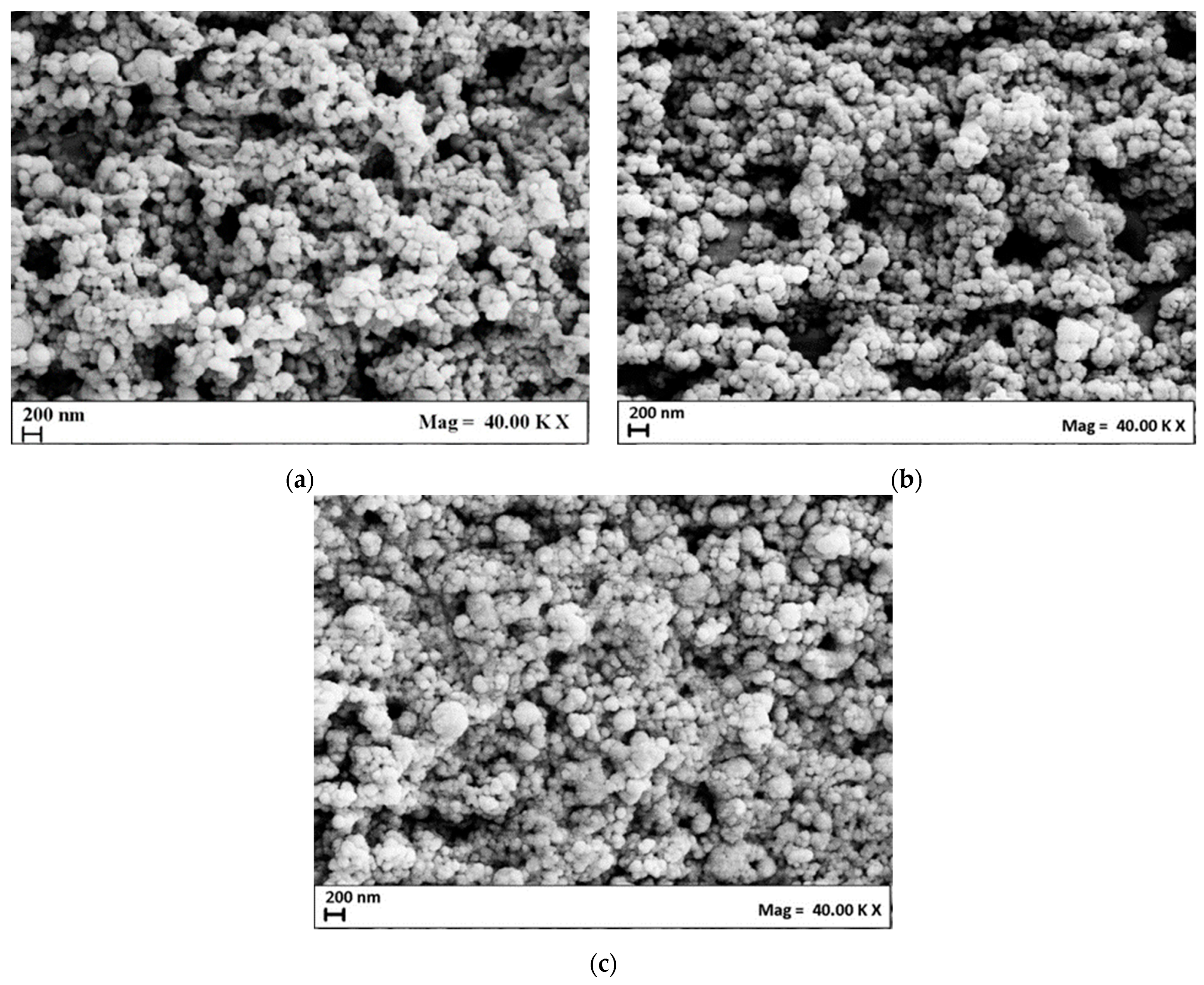
3.1. Production of Unloaded Niosomes
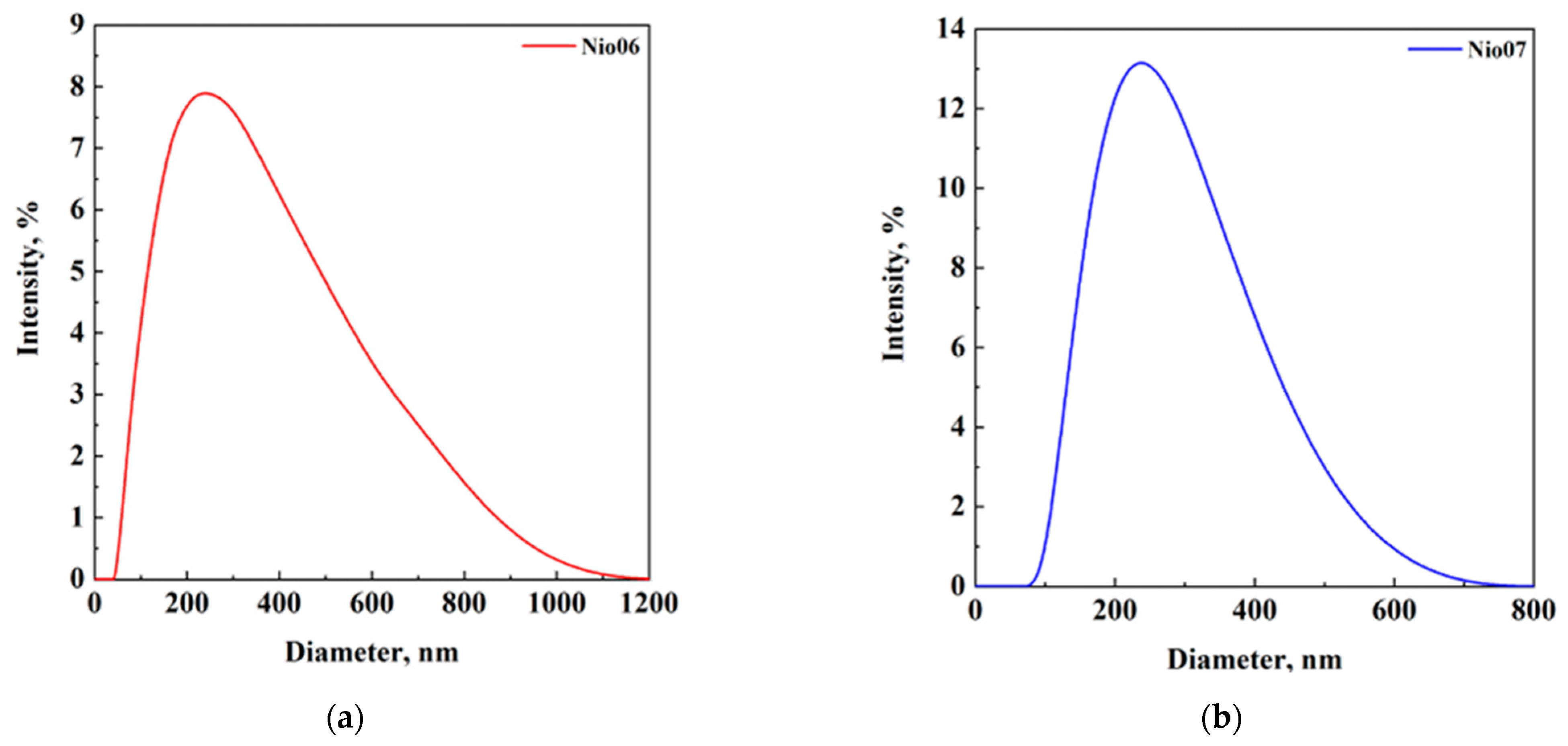
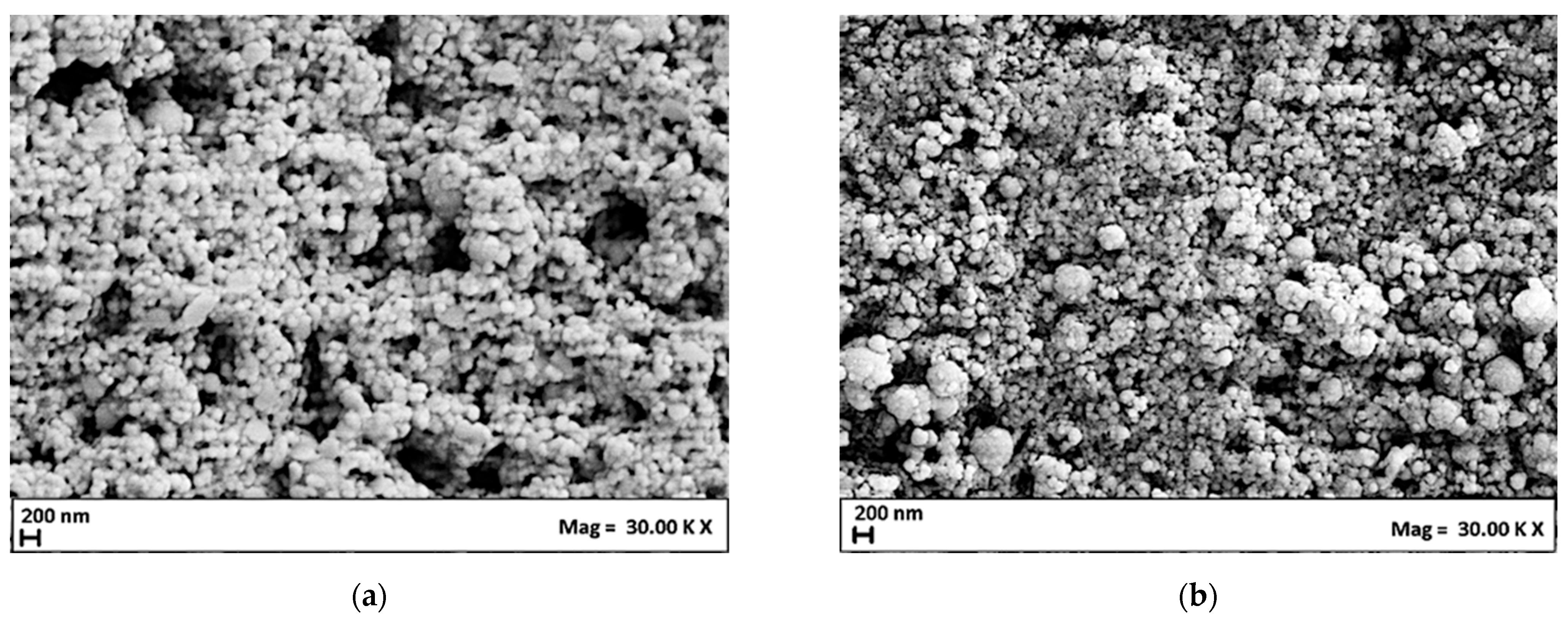
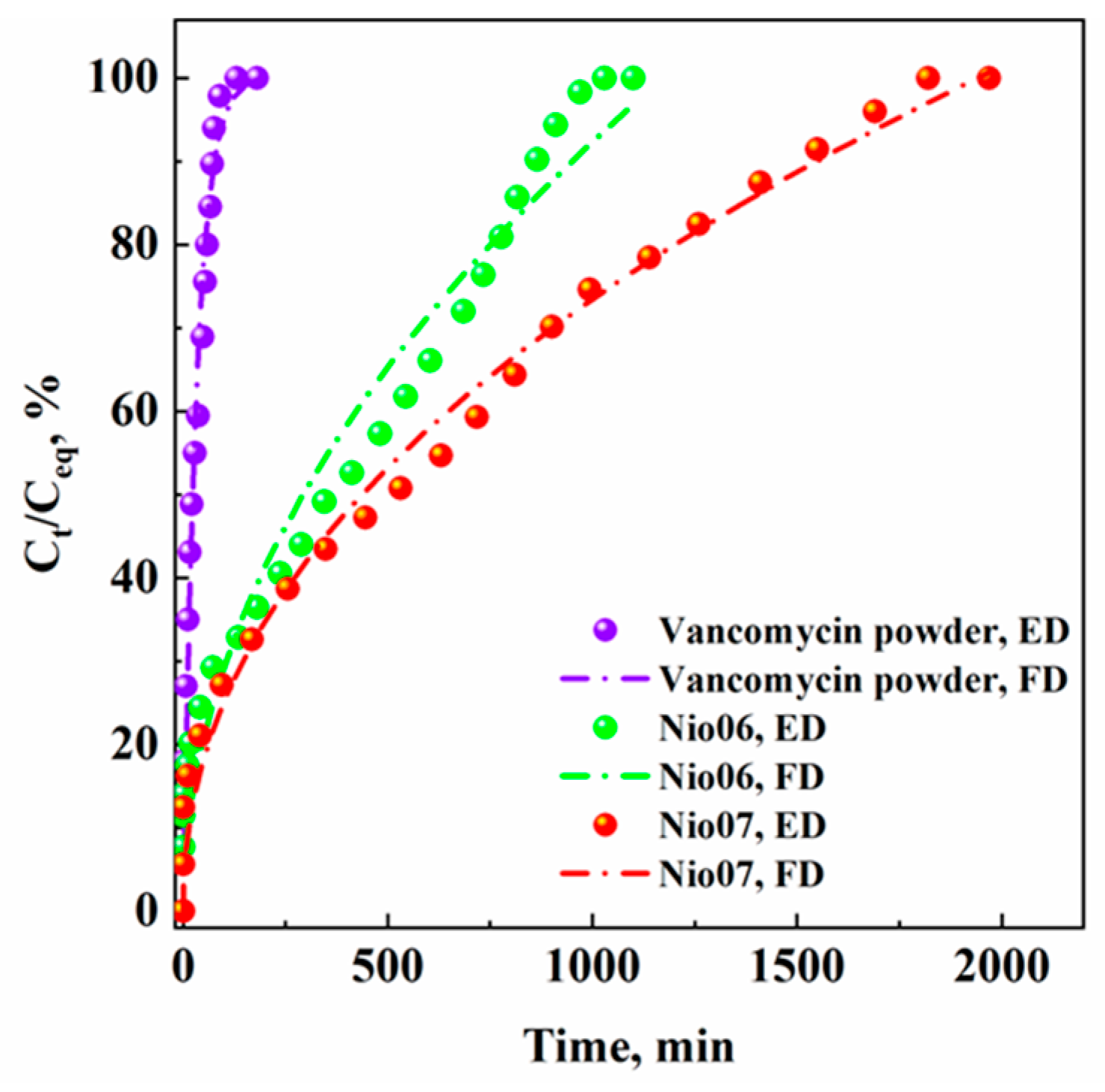
3.2. Production of Vancomycin-Loaded Niosomes
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sahu, T.; Ratre, Y.K.; Chauhan, S.; Bashkar, L.V.K.S.; Nair, P.; Verma, H.K. Nanotechnology based drug delivery system: Current strategies and emerging therapeutic potential for medical science. J. Drug Deliv Sci. Technol. 2021, 63, 102487. [Google Scholar] [CrossRef]
- Song, M.; Aipire, A.; Dilxat, E.; Li, J.; Xia, G.; Jiang, Z.; Fan, Z.; Li, J. Research progress of polysaccharide-gold nanocomplexes in drug delivery. Pharmaceutics 2024, 16, 88. [Google Scholar] [CrossRef] [PubMed]
- Riccardi, D.; Baldino, L.; Reverchon, E. Liposomes, transfersomes and niosomes: Production methods and their applications in the vaccinal field. J. Transl. Med. 2024, 22, 339. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.; Wang, Z.; Ju, X.; Deng, F.; Yang, F.; He, R. Co-Encapsulation of rutinoside and β-carotene in liposomes modified by rhamnolipid: Antioxidant activity, antibacterial activity, Storage stability, and in vitro gastrointestinal digestion. J. Food Sci. 2023, 88, 2064–2077. [Google Scholar] [CrossRef] [PubMed]
- Pasarin, D.; Ghizdareanu, A.I.; Enascuta, C.E.; Matei, C.B.; Bilbie, C.; Paraschiv-Palada, L.; Veres, P.A. Coating materials to increase the stability of liposomes. Polymers 2023, 15, 782. [Google Scholar] [CrossRef] [PubMed]
- Inglut, C.T.; Sorrin, A.J.; Kuruppu, T.; Vig, S.; Cicalo, J.; Ahmad, H.; Huang, H.-C. Immunological and toxicological considerations for the design of liposomes. Nanomaterials 2020, 10, 190. [Google Scholar] [CrossRef]
- Zhang, T.; Xu, X.; Pan, Y.; Yang, H.; Han, J.; Liu, J.; Liu, W. Specific surface modification of liposomes for gut targeting of food bioactive agents. Comp. Rev. Food Sci. Food Saf. 2023, 22, 3685–3706. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Hanning, S.; Falconer, J.; Locke, M.; Wen, J. Recent advances in non-ionic surfactant vesicles (niosomes): Fabrication, characterization, pharmaceutical and cosmetic applications. Eur. J. Pharm. Biopharm. 2019, 144, 18–39. [Google Scholar] [CrossRef]
- Moghassemi, S.; Hadjizadeh, A. Nano-niosomes as nanoscale drug delivery systems: An illustrated review. J. Control Release 2014, 185, 22–36. [Google Scholar] [CrossRef]
- Sharma, S.; Sharma, D.; Thakur, P.; Devi, P.; Sharma, M.D. A comprehensive review on niosomes; targeted drug delivery system. Ymer 2023, 22, 1969–1987. [Google Scholar]
- Du, X.; Huang, X.; Wang, L.; Mo, L.; Jing, H.; Bai, X.; Wang, H. Nanosized niosomes as effective delivery device to improve the stability and bioaccessibility of goat milk whey protein peptide. Food Res. Int. 2022, 161, 1117–1129. [Google Scholar] [CrossRef] [PubMed]
- Vyas, S.P.; Singh, R.P.; Jain, S.; Mishra, V.; Mahor, S.; Singh, P.; Gupta, P.N.; Rawat, A.; Dubey, P. Non-ionic surfactant based vesicles (niosomes) for non-invasive topical genetic immunization against hepatitis B. Int. J Pharm. 2005, 296, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Obeid, M.A.; Teeravatcharoenchai, T.; Connell, D.; Niwasabutra, K.; Hussain, M.; Carte, K.; Ferro, V.A. Examination of the effect of niosome preparation methods in encapsulating model antigens on the vesicle characteristics and their ability to induce immune responses. J. Liposome Res. 2021, 31, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Pamornpathomkul, B.; Niyomtham, N.; Yingyongnarongkul, B.-E.; Prasitpuriprecha, C.; Rojanarata, T.; Ngawhirunpat, T.; Opanasopit, P. Cationic niosomes for enhanced skin immunization of plasmid DNA-encoding ovalbumin via hollow microneedles. AAPS PharmSciTech 2018, 19, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Abruzzo, A.; Pucci, R.; Abruzzo, P.M.; Canaider, S.; Parolin, C.; Vitali, B.; Valle, F.; Brucale, M.; Cerchiara, T.; Luppi, B.; et al. Azithromycin-loaded liposomes and niosomes for the treatment of skin infections: Influence of excipients and preparative methods on the functional properties. Eur. J. Pharm. Biopharm. 2024, 197, 14233. [Google Scholar] [CrossRef] [PubMed]
- Al-Kofahi, T.; Altrad, B.; Amawi, H.; Aljabali, A.A.; Abul-Haija, Y.M.; Obeid, M.A. Paclitaxel-loaded niosomes in combination with metformin: Development, characterization and anticancer potentials. Ther. Deliv. 2024, 15, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Khambalkar, S.M.; Ghuge, A.D.; Deshmukh, S.P.; Jadhav, K.P.; Jaiswal, R.V.; Khune, A.A. Niosomes: A targeted drug delivery system. GCS Biol. Pharm. Sci. 2024, 26, 48–62. [Google Scholar] [CrossRef]
- Priyadarshini, K.; Gopinath, E.; Ganesh, N.S.; Vineeth, C. Niosomes as a potential approach for enhanching topical application. Int. J. Pharm. Sci. Invent. 2024, 2, 35–45. [Google Scholar] [CrossRef]
- Momekova, D.B.; Gugleva, V.E.; Petrov, P.D. Nanoarchitectonics of multifunctional niosomes for advanced drug delivery. ACS Omega 2021, 6, 33265–33273. [Google Scholar] [CrossRef]
- Hussain, Z.; Khan, S.; Imran, M.; Sohail, M.; Shah, S.W.A.; de Matas, M. PEGylation: A promising strategy to overcome challenges to cancer-targeted nanomedicines: A review of challenges to clinical transition and promising resolution. Drug. Deliv. Transl. Res. 2019, 9, 721–734. [Google Scholar] [CrossRef]
- Attia, M.F.; Anton, N.; Wallyn, J.; Omran, Z.; Vandamme, T.F. An overview of active and passive targeting strategies to improve the nanocarriers efficiency to tumour sites. J. Pharm. Pharmacol. 2019, 71, 1185–1198. [Google Scholar] [CrossRef]
- Maurer, V.; Altin, S.; Ag Seleci, D.; Zarinwall, A.; Temel, B.; Vogt, P.M.; Strauß, S.; Stahl, F.; Scheper, T.; Bucan, V.; et al. In-vitro application of magnetic hybrid niosomes: Targeted siRNA-delivery for enhanced breast cancer therapy. Pharmaceutics 2021, 13, 394. [Google Scholar] [CrossRef]
- Mohamed, A.M.; Hossam, S.E.-S.; Ahmed, M.R.; Fathy, I.A.; Sherif, K.A.E.; Ahmed, E.L.; Hatem, R.I.; Khalid, M.E. Effect of nanovesicular surface-functionalization via chitosan and/or PEGylation on cytotoxicity of tamoxifen in induced-breast cancer model. Life Sci. 2022, 307, 120908. [Google Scholar] [CrossRef] [PubMed]
- Suk, J.S.; Xu, Q.; Kim, N.; Hanes, J.; Ensign, L.M. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv. Drug Deliv. Rev. 2016, 99, 28–51. [Google Scholar] [CrossRef] [PubMed]
- Cosco, D.; Paolino, D.; Muzzalupo, R.; Celia, C.; Citrato, R.; Caponio, D.; Picci, N.; Fresta, M. Novel PEG-coated niosomes based on bola-surfactant as drug carriers for 5-fluorouracil. Biomed. Microdevices 2009, 11, 1115–1125. [Google Scholar] [CrossRef]
- Kopermsub, P.; Mayen, V.; Warin, C. Potential use of niosomes for encapsulation of nisin and EDTA and their antibacterial activity enhancement. Food Res. Int. 2011, 44, 605–612. [Google Scholar] [CrossRef]
- Baranei, M.; Taheri, R.A.; Tirgar, M.; Saeidi, A.; Oroojalian, F.; Uzun, L.; Asefnejad, A.; Wurm, F.R.; Goodarzi, V. Anticancer effect of green tea extract (GTE)-loaded pH-responsive niosome coated with PEG against different cell lines. Mater. Today Commun. 2021, 26, 101751. [Google Scholar] [CrossRef]
- Chaves, M.A.; Baldino, L.; Pinho, S.C.; Reverchon, E. Supercritical CO2 assisted process for the production of mixed phospholipid nanoliposomes: Unloaded and vitamin D3-loaded vesicles. J. Food Eng. 2022, 316, 110851. [Google Scholar] [CrossRef]
- Baldino, L.; Reverchon, E. Production of Nanoliposomes by a supercritical CO2 assisted process: Application to cosmetics. Chem. Eng. Trans. 2023, 101, 61–66. [Google Scholar] [CrossRef]
- Chaves, M.A.; Baldino, L.; Pinho, S.C.; Reverchon, E. Co-Encapsulation of curcumin and vitamin D3 in mixed phospholipid nanoliposomes using a continuous supercritical CO2 assisted process. J. Taiwan Inst. Chem. Eng. 2022, 132, 104120. [Google Scholar] [CrossRef]
- Squittieri, R.; Baldino, L.; Reverchon, E. Production of antioxidant transfersomes by a supercritical CO2 assisted process for transdermal delivery applications. Nanomater. 2023, 13, 1812. [Google Scholar] [CrossRef] [PubMed]
- Baldino, L.; Reverchon, E. Niosomes formation using a continuous supercritical CO2 assisted process. J. CO2 Util. 2021, 52, 101669. [Google Scholar] [CrossRef]
- Baldino, L.; Reverchon, E. Continuous supercritical CO2 assisted process for the production of nano-niosomes loaded with a second-generation antibiotic for ocular therapy. J. Supercrit. Fluids 2022, 188, 1056–1073. [Google Scholar] [CrossRef]
- Coleman, K.J.; Roos, K.L. Acute bacterial infections of the central nervous system. In Aminoff’s Neurology and General Medicine, 6th ed.; Academic Press: Cambridge, MA, USA, 2021; pp. 683–701. [Google Scholar] [CrossRef]
- Singh, V.; Kumar, V.; Kashyap, S.; Singh, A.V.; Kishore, V.; Sitti, M.; Saxena, P.S.; Srivastava, A. graphene oxide synergistically enhances antibiotic efficacy in vancomycin-resistant staphylococcus aureus. ACS App. Bio Mater. 2019, 2, 1148–1157. [Google Scholar] [CrossRef] [PubMed]
- Tavano, L.; Alfano, P.; Muzzalupo, R.; de Cindio, B. Niosomes vs microemulsions: New carriers for topical delivery of capsaicin. Colloids Surf. B Biointerfaces 2011, 87, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Malviya, K.; Soni, P.; Omray, L.K. Application of ethanol-injection technique for formulation of vitexin loaded noisomes and characterization of the vesicles. J. Popl. Ther. Clin. Pharmacol. 2023, 30, 2850–2858. [Google Scholar] [CrossRef]
- Tyagi, R.; Waheed, A.; Kumar, N.; Ahad, A.; Bin Jardan, Y.A.; Mujeeb, M.; Kumar, A.; Naved, T.; Madan, S. Formulation and Evaluation of plumbagin-loaded niosomes for an antidiabetic study: Optimization and in vitro evaluation. Pharmaceuticals 2023, 16, 1169. [Google Scholar] [CrossRef]
- Smith, M.C.; Crist, R.M.; Clogston, J.D.; McNeil, S.E. Zeta potential: A case study of cationic, anionic, and neutral liposomes. Anal. Bioanal. Chem. 2017, 409, 5779–5787. [Google Scholar] [CrossRef]
- Serrano-Lotina, A.; Portela, R.; Baeza, P.; Alcolea-Rodriguez, V.; Villarroel, M.; Avila, P. Zeta potential as a tool for functional materials development. Catal. Today 2022, 423, 113862. [Google Scholar] [CrossRef]
- Bhardwaj, P.; Tripathi, P.; Gupta, R.; Pandey, S. Niosomes: A review on niosomal research in the last decade. J. Drug Deliv. Sci. Technol. 2020, 56, 101581. [Google Scholar] [CrossRef]
- Nowroozi, F.; Almasi, A.; Javidi, J.; Haeri, A.; Dadashzadeh, S. Effect of surfactant type, cholesterol, and various downsizing methods on the particle size of niosomes. Iran. J. Pharm. Res. 2018, 17, 1–11. [Google Scholar] [PubMed]
- Javani, R.; Hashemi, F.S.; Ghanbarzadeh, B.; Hamishehkar, H. Quercetin-loaded niosomal nanoparticles prepared by the thin-layer hydration method: Formulation development, colloidal stability, and structural properties. LWT 2021, 141, 110865. [Google Scholar] [CrossRef]
- Huang, Y.; Chen, J.; Chen, X.; Gao, J.; Liang, W. PEGylated synthetic surfactant vesicles (niosomes): Novel carriers for oligonucleotides. J. Mater. Sci. Mater. Med. 2020, 19, 607–614. [Google Scholar] [CrossRef] [PubMed]
- García-Manrique, P.; Machado, N.D.; Fernández, M.A.; Blanco-López, M.C.; Matos, M.; Gutiérrez, G. Effect of drug molecular weight on niosomes size and encapsulation efficiency. Colloids Surf. B Biointerfaces 2020, 186, 110711. [Google Scholar] [CrossRef] [PubMed]
- Ren, H.; He, Y.; Liang, J.; Cheng, Z.; Zhang, M.; Zhu, Y.; Hong, C.; Qin, J.; Xu, X.; Wang, J. Role of liposome size, surface charge, and PEGylation on rheumatoid arthritis targeting therapy. ACS Appl. Mater. Interfaces 2019, 11, 20304–20315. [Google Scholar] [CrossRef]
- Wolfram, J.; Suri, K.; Yang, Y.; Shen, J.; Celia, C.; Fresta, M.; Zhao, Y.; Shen, H.; Ferrari, M. Shrinkage of pegylated and non-pegylated liposomes in serum. Colloids Surf. B Biointerfaces 2014, 114, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Haroun, M.; Elsewedy, H.S.; Shehata, T.M.; Tratrat, C.; Dhubiab, A.; Venugopala, K.N.; Almostafa, M.M.; Kochkar, H.; Elnahas, H.M. Significant of injectable brucine PEGylated niosomes in treatment of MDA cancer cells. J. Drug. Deliv. Sci. Technol. 2022, 71, 103322. [Google Scholar] [CrossRef]
- Asghari Lalami, Z.; Tafvizi, F.; Naseh, V.; Salehipour, M. Fabrication, optimization, and characterization of pH-responsive PEGylated nanoniosomes containing gingerol for enhanced treatment of breast cancer. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2023, 396, 3867–3886. [Google Scholar] [CrossRef] [PubMed]
- Mahsa, B.; Nazanin, K.; Noorbazargan, H.; Mohammad, T.Y.; Zahra, A.L.; Iman, A.; Faten, E.Y.; Aghigh, D.; Fatmeh, M.Y.; Yen, N.T. Evaluation of anti-cancer and anti-metastatic effects of folate-PEGylated niosomes for co-delivery of letrozole and ascorbic acid on breast cancer cells. Mol. Syst. Des. Eng. 2022, 7, 1102–1118. [Google Scholar] [CrossRef]
- Park, S.-J.; Choi, S.G.; Davaa, E.; Park, J.-S. Encapsulation enhancement and stabilization of insulin in cationic liposomes. Int. J. Pharm. 2011, 415, 267–272. [Google Scholar] [CrossRef]
- Saharkhiz, S.; Zarepour, A.; Zarrabi, A. Empowering cancer therapy: Comparing PEGylated and non-PEGylated niosomes loaded with curcumin and doxorubicin on MCF-7 cell Line. Bioengineering 2023, 10, 1159. [Google Scholar] [CrossRef]
- Alemi, A.; Zavar Reza, J.; Haghiralsadat, F.; Zarei Jaliani, H.; Haghi, K.M.; Hosseini, S.A.; Haghi, K.S. Paclitaxel and curcumin coadministration in novel cationic PEGylated niosomal formulations exhibit enhanced synergistic antitumor efficacy. J. Nanobiotechnol. 2018, 28, 16. [Google Scholar] [CrossRef] [PubMed]
- Wu, I.Y.; Bala, S.; Škalko-Basnet, N.; di Cagno, M.P. Interpreting non-linear drug diffusion data: Utilizing Korsmeyer-Peppas model to study drug release from liposomes. Eur. J. Pharm. Biopharm. 2019, 138, 105026. [Google Scholar] [CrossRef]
- Hussain, A.; Altamimi, M.A.; Alshehri, S.; Imam, S.S.; Singh, S.K. Vesicular elastic liposomes for transdermal delivery of rifampicin: In-vitro, in-vivo and in silico GastroPlusTM prediction studies. Eur. J. Pharm. Sci. 2020, 151, 105411. [Google Scholar] [CrossRef]
- Jain, A.; Jain, S.K. In vitro release kinetics model fitting of liposomes: An insight. Chem. Phys. Lipids 2016, 201, 28–40. [Google Scholar] [CrossRef]
- Ahmed, L.; Atif, R.; Eldeen, T.S.; Yahya, I.; Omara, A.; Eltayed, M. Study the using of nanoparticles as drug delivery system based on mathematical models for controlled release. Int. J. Latest Technol. Eng. Manag. Appl. Sci. 2019, 8, 52–56. [Google Scholar]

| Set of Experiments | Span 80/Tween 80 | HLB | Span 80, mg | Tween 80, mg | Surfactant/Cholesterol, mol/mol | PEG400, % w/v |
|---|---|---|---|---|---|---|
| Nio01 | 95:5 | 4.84 | 1900 | 100 | - | - |
| Nio02 | 90:10 | 5.37 | 1800 | 200 | - | - |
| Nio03 | 80:20 | 6.44 | 1600 | 400 | - | - |
| Nio04 | 80:20 | 6.44 | 1600 | 400 | 4 | - |
| Nio05 | 80:20 | 6.44 | 1600 | 400 | 4 | 1 |
| Sample | Stability, Days | MHD, nm | PDI | ζ-Potential, mV |
|---|---|---|---|---|
| Nio01 | 0 | 181 ± 55 | 0.365 | −16.2 ± 2.5 |
| 15 | 180 ± 49 | 0.297 | −16.1 ± 3.6 | |
| 30 | 181 ± 54 | 0.362 | −17.1 ± 2.7 | |
| 60 | 185 ± 51 | 0.301 | −15.0 ± 2.2 | |
| Nio02 | 0 | 191 ± 47 | 0.242 | −19.8 ± 2.5 |
| 15 | 190 ± 50 | 0.276 | −19.8 ± 3.1 | |
| 30 | 188 ± 52 | 0.302 | −17.4 ± 3.0 | |
| 60 | 189 ± 56 | 0.348 | −15.3 ± 2.0 | |
| Nio03 | 0 | 248 ± 52 | 0.182 | −23.1 ± 2.3 |
| 15 | 248 ± 58 | 0.222 | −21.0 ± 2.7 | |
| 30 | 247 ± 58 | 0.228 | −19.7 ± 2.4 | |
| 60 | 245 ± 56 | 0.210 | −18.5 ± 2.5 | |
| Nio04 | 0 | 118 ± 33 | 0.318 | −27.4 ± 3.0 |
| 15 | 118 ± 34 | 0.325 | −27.4 ± 3.0 | |
| 30 | 118 ± 35 | 0.357 | −25.7 ± 4.0 | |
| 60 | 119 ± 39 | 0.424 | −23.1 ± 3.1 | |
| Nio05 | 0 | 203 ± 62 | 0.372 | −30.6 ± 2.4 |
| 15 | 203 ± 62 | 0.372 | −30.6 ± 2.4 | |
| 30 | 204 ± 63 | 0.381 | −30.7 ± 2.4 | |
| 60 | 205 ± 67 | 0.430 | −30.8 ± 2.7 |
| Set of Experiments | Span 80/Tween 80 | Span 80, mg | Tween 80, mg | Surfactant/Cholesterol, mol/mol | PEG400, % w/v | Drug to Lipid Ratio, % w/w |
|---|---|---|---|---|---|---|
| Nio06 | 80:20 | 1600 | 400 | 4 | - | 5 |
| Nio07 | 80:20 | 1600 | 400 | 4 | 1 | 5 |
| Sample | Stability, Days | MHD, nm | PDI | ζ-Potential, mV |
|---|---|---|---|---|
| Nio06 | 0 | 214 ± 59 | 0.300 | −31.1 ± 2.5 |
| 15 | 214 ± 57 | 0.300 | −31.1 ± 2.5 | |
| 30 | 214 ± 65 | 0.372 | −31.1 ± 2.3 | |
| 60 | 214 ± 65 | 0.370 | −31.0 ± 2.0 | |
| Nio07 | 0 | 254 ± 73 | 0.330 | −27.7 ± 2.0 |
| 15 | 254 ± 73 | 0.330 | −27.7 ± 2.0 | |
| 30 | 250 ± 66 | 0.280 | −27.6 ± 2.4 | |
| 60 | 250 ± 65 | 0.270 | −27.3 ± 2.0 |
| Vancomycin Powder | Nio06 | Nio07 | ||
|---|---|---|---|---|
| First order | a | 100.18 | 118.3 | 103.42 |
| b | 0.0298 | 0.0016 | 0.0014 | |
| R2adj | 0.965 | 0.921 | 0.941 | |
| AIC | 70.05 | 118.83 | 98.71 | |
| Korsmeyer–Peppas | kKP | 15.78 | 2.40 | 2.95 |
| n | 0.38 | 0.53 | 0.47 | |
| R2adj | 0.950 | 0.960 | 0.985 | |
| AIC | 70.76 | 95.61 | 62.68 | |
| Higuchi | kH | 9.57 | 2.92 | 2.31 |
| R2adj | 0.899 | 0.961 | 0.983 | |
| AIC | 79.54 | 93.55 | 62.74 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baldino, L.; Riccardi, D.; Reverchon, E. Production of PEGylated Vancomycin-Loaded Niosomes by a Continuous Supercritical CO2 Assisted Process. Nanomaterials 2024, 14, 846. https://doi.org/10.3390/nano14100846
Baldino L, Riccardi D, Reverchon E. Production of PEGylated Vancomycin-Loaded Niosomes by a Continuous Supercritical CO2 Assisted Process. Nanomaterials. 2024; 14(10):846. https://doi.org/10.3390/nano14100846
Chicago/Turabian StyleBaldino, Lucia, Domenico Riccardi, and Ernesto Reverchon. 2024. "Production of PEGylated Vancomycin-Loaded Niosomes by a Continuous Supercritical CO2 Assisted Process" Nanomaterials 14, no. 10: 846. https://doi.org/10.3390/nano14100846







