The Impact of Open versus Closed Computer-Aided Design/Computer-Aided Manufacturing Systems on the Marginal Gap of Zirconia-Reinforced Lithium Silicate Single Crowns Evaluated by Scanning Electron Microscopy: A Comparative In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- In everyday dentistry, both closed systems and open systems can be used to achieve an acceptable marginal gap (<120 µm) for ZLS CELTRA® DUO single crowns.
- No significant difference was found regarding the marginal gap when comparing ZLS CELTRA® DUO single crowns produced by closed systems or open systems and cemented with Gcem One self-adhesive resin cement.
- There was a significant difference between cementation with Temp-bond and Gcem One self-adhesive resin cement regarding the marginal gap (p < 0.0005).
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Ting-Shu, S.; Jian, S. Intraoral Digital Impression Technique: A Review. J. Prosthodont. 2015, 24, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.; Ruse, D.; Wyatt, C. A comparison of the marginal fit of crowns fabricated with digital and conventional methods. J. Prosthetics Dent. 2014, 112, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Al Hamad, K.Q.; Al Rashdan, B.A.; Al Omari, W.M.; Baba, N.Z. Comparison of the Fit of Lithium Disilicate Crowns made from Conventional, Digital, or Conventional/Digital Techniques. J. Prosthodont. 2019, 28, e580–e586. [Google Scholar] [CrossRef]
- Gjelvold, B.; Chrcanovic, B.R.; Korduner, E.K.; Collin-Bagewitz, I.; Kisch, J. Intraoral Digital Impression Technique Compared to Conventional Impression Technique. A Randomized Clinical Trial. J. Prosthodont. 2016, 25, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Rödiger, M.; Heinitz, A.; Bürgers, R.; Rinke, S. Fitting accuracy of zirconia single crowns produced via digital and conventional impressions-a clinical comparative study. Clin. Oral. Investig. 2017, 21, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Ferrini, F.; Sannino, G.; Chiola, C.; Capparé, P.; Gastaldi, G.; Gherlone, E.F. Influence of Intra-Oral Scanner (I.O.S.) on The Marginal Accuracy of CAD/CAM Single Crowns. Int. J. Environ. Res. Public Health. 2019, 16, 544. [Google Scholar] [CrossRef] [PubMed]
- Diker, B.; Tak, Ö. Comparing the accuracy of six intraoral scanners on prepared teeth and effect of scanning sequence. J. Adv. Prosthodont. 2020, 12, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Nulty, A.B. A Comparison of Full Arch Trueness and Precision of Nine Intra-Oral Digital Scanners and Four Lab Digital Scanners. Dent. J. 2021, 9, 75. [Google Scholar] [CrossRef] [PubMed]
- Jivănescu, A.; Bara, A.; Faur, A.-B.; Rotar, R.N. Is There a Significant Difference in Accuracy of Four Intraoral Scanners for Short-Span Fixed Dental Prosthesis? A Comparative In Vitro Study. Appl. Sci. 2021, 11, 8280. [Google Scholar] [CrossRef]
- Vaz, I.M.; Carracho, J.F. Marginal fit of zirconia copings fabricated after conventional impression making and digital scanning: An in vitro study. J. Prosthet. Dent. 2020, 124, 223.e1–223.e6. [Google Scholar] [CrossRef]
- Amos, W.B.; White, J.G. How the confocal laser scanning microscope entered biological research. Biol. Cell. 2003, 95, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Logozzo, S.; Zanetti, E.M.; Franceschini, G.; Kilpelä, A.; Mäkynen, A. Recent advances in dental optics–Part I: 3D intraoral scanners for restorative dentistry. Opt. Lasers Eng. 2014, 54, 203–221. [Google Scholar] [CrossRef]
- Sheppard, C.J.; Gu, M.; Roy, M. Signal-to-noise ratio in confocal microscope systems. J. Microsc. 1992, 168, 209–218. [Google Scholar] [CrossRef]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef] [PubMed]
- McLean, J.W.; von Fraunhofer, J.A. The estimation of cement film thickness by an in vivo technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Tsirogiannis, P.; Reissmann, D.R.; Heydecke, G. Evaluation of the marginal fit of single-unit, complete-coverage ceramic restorations fabricated after digital and conventional impressions: A systematic review and meta-analysis. J. Prosthet. Dent. 2016, 116, 328–335.e2. [Google Scholar] [CrossRef]
- Sadeqi, H.A.; Baig, M.R.; Al-Shammari, M. Evaluation of Marginal/Internal Fit and Fracture Load of Monolithic Zirconia and Zirconia Lithium Silicate (ZLS) CAD/CAM Crown Systems. Materials 2021, 14, 6346. [Google Scholar] [CrossRef]
- Suárez, M.J.; González de Villaumbrosia, P.; Pradíes, G.; Lozano, J.F.L. Comparison of the Marginal Fit of Procera AllCeram Crowns with Two Finish Lines. Int. J. Prosthodont. 2003, 16, 229–232. [Google Scholar]
- Coli, P.; Karlsson, S. Fit of a New Pressure-Sintered Zirconium Dioxide Coping. Int. J. Prosthodont. 2004, 17, 59–64. [Google Scholar]
- Neves, F.D.; Prado, C.J.; Prudente, M.S.; Carneiro, T.A.P.N.; Zancopé, K.; Davi, L.R.; Mendonça, G.; Cooper, L.F.; Soares, C.J. MicroComputed Tomography Evaluation of Marginal Fit of Lithium Disilicate Crowns Fabricated by Using Chairside CAD/CAM Systems or the Heat-Pressing Technique. J. Prosthet. Dent. 2014, 112, 1134–1140. [Google Scholar] [CrossRef]
- Freire, Y.; Gonzalo, E.; Lopez-Suarez, C.; Suarez, M.J. The marginal fit of CAD/CAM monolithic ceramic and metal-ceramic crowns. J. Prosthodont. 2019, 28, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Boitelle, P.; Mawussi, B.; Tapie, L.; Fromentin, O. A systematic review of CAD/CAM fit restoration evaluations. J. Oral. Rehabil. 2014, 41, 853–874. [Google Scholar] [CrossRef] [PubMed]
- Totiam, P.; Gonzalez-Cabezas, C.; Fontana, M.R.; Zero, D.T. A new in vitro model to study the relationship of gap size and secondary caries. Caries Res. 2007, 4, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Kosyfaki, P.; del Pilar Pinilla Martín, M.; Strub, J.R. Relationship between crowns and the periodontium: A literature update. Quintessence Int. 2010, 41, 109–126. [Google Scholar] [PubMed]
- Lawson, N.C.; Bansal, R.; Burgess, J.O. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent. Mater. 2016, 32, e275–e283. [Google Scholar] [CrossRef] [PubMed]
- Traini, T.; Sinjari, B.; Pascetta, R.; Serafini, N.; Perfetti, G.; Trisi, P.; Caputi, S. The zirconia-reinforced lithium silicate ceramic: Lights and shadows of a new material. Dent. Mater. J. 2016, 35, 748–755. [Google Scholar] [CrossRef] [PubMed]
- Zarone, F.; Ruggiero, G.; Leone, R.; Breschi, L.; Leuci, S.; Sorrentino, R. Zirconia-reinforced lithium silicate (ZLS) mechanical and biological properties: A literature review. J. Dent. 2021, 109, 103661. [Google Scholar] [CrossRef]
- Ben-Izhack, G.; Shely, A.; Naishlos, S.; Glikman, A.; Frishman, L.; Meirowitz, A.; Dolev, E. The Influence of Three Different Digital Cement Spacers on the Marginal Gap Adaptation of Zirconia-Reinforced Lithium Silicate Crowns Fabricated by CAD-CAM System. Appl. Sci. 2021, 11, 10709. [Google Scholar] [CrossRef]
- Naves, L.Z.; Gerdolle, D.A.; de Andrade, O.S.; Markus Maria Gresnigt, M. Seeing is believing? When scanning electron microscopy (SEM) meets clinical dentistry: The replica technique. Microsc. Res. Tech. 2020, 83, 1118–1123. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.-R.; Essig, M.E. Panorama of dental CAD/CAM restorative systems. Compend. Contin. Educ. Dent. 2008, 29, 482–484. [Google Scholar]
- Tariq, F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthet. Dent. 2016, 60, 72–84. [Google Scholar]
- Kricheldorf, F.; Bueno, C.R.S.; Amaral, W.D.S.; Junior, J.F.S.; Filho, H.N. Analysis of vertical marginal discrepancy in feldspathic porcelain crowns manufactured with different CAD/CAM systems: Closed and open. Eur. J. Dent. 2018, 12, 123–128. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ben-Izhack, G.; Shely, A.; Koton, O.; Meirowitz, A.; Levartovsky, S.; Dolev, E. (In-Vitro Comparison between Closed Versus Open CAD/CAM Systems) Comparison between Closed and Open CAD/CAM Systems by Evaluating the Marginal Fit of Zirconia-Reinforced Lithium Silicate Ceramic Crowns. Appl. Sci. 2021, 11, 4534. [Google Scholar] [CrossRef]
- Akat, B.; Şentürk, A.; Ocak, M.; Kiliçarslan, M.A.; Özcan, M. Does cad software affect the marginal and internal fit of milled full ceramic crowns? Braz. Oral. Res. 2022, 36, e042. [Google Scholar] [CrossRef] [PubMed]
- Pilo, R.; Folkman, M.; Arieli, A.; Levartovsky, S. Marginal Fit and Retention Strength of Zirconia Crowns Cemented by Self-adhesive Resin Cements. Oper. Dent. 2018, 43, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Dapieve, K.S.; Pilecco, R.O.; Temp, R.W.; Villetti, M.A.; Pereira, G.K.R.; Valandro, L.F. Adhesion to lithium disilicate glass-ceramics after aging: Resin viscosity and ceramic surface treatment effects. J. Mech. Behav. Biomed. Mater. 2023, 142, 105819. [Google Scholar] [CrossRef] [PubMed]
- El-Ashkar, A.; Taymour, M.; El-Tannir, A. Evaluation of the marginal and internal gaps of partially crystallized versus fully crystallized zirconia-reinforced lithium silicate CAD-CAM crowns: An in vitro comparison of the silicone replica technique, direct view, and 3-dimensional superimposition analysis. J. Prosthet. Dent. 2023, 129, 769–776. [Google Scholar] [CrossRef]
- Di Fiore, A.; Zuccon, A.; Carraro, F.; Basilicata, M.; Bollero, P.; Bruno, G.; Stellini, E. Assessment Methods for Marginal and Internal Fit of Partial Crown Restorations: A Systematic Review. J. Clin. Med. 2023, 12, 5048. [Google Scholar] [CrossRef]





| Total Mean Marginal Gap Temp-Bond (μm) | Mean ±SD | CI—Upper/ Lower Limit | Min Max |
|---|---|---|---|
| PrimeScan | 28.09 ±3.06 | 29.52 26.65 | 20.75 32.88 |
| Trios | 28.94 ±3.30 | 30.49 27.39 | 24.54 34.79 |
| Buccal Surface | Mesial Surface | Palatal Surface | Distal Surface | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean Marginal Gap Temp-Bond (μm) | Mean ±SD | CI—Upper/ Lower Limit | Min Max | Mean ±SD | CI—Upper/ Lower Limit | Min Max | Mean ±SD | CI—Upper/ Lower Limit | Min Max | Mean ±SD | CI—Upper/ Lower Limit | Min Max |
| Primescan | 26.79 ±4.35 | 28.83 24.76 | 21.20 34.84 | 27.05 ±6.32 | 30.01 24.09 | 18.39 39.39 | 29.80 ±4.84 | 32.07 27.53 | 21.27 38.31 | 28.70 ±5.08 | 31.08 26.33 | 18.17 35.42 |
| Trios | 31.27 ±3.66 | 32.99 29.56 | 24.10 37.73 | 26.40 ±4.77 | 28.63 24.16 | 19.16 36.93 | 29.94 ±7.15 | 33.29 26.59 | 17.97 46.05 | 28.16 ±5.22 | 30.61 25.71 | 19.08 42.05 |
| Total Mean Marginal Gap Gcem ONE (μm) | Mean ±SD | CI—Upper/ Lower Limit | Min Max |
|---|---|---|---|
| PrimeScan | 46.70 ±3.80 | 48.48 44.92 | 38.42 52.47 |
| Trios | 47.79 ±2.59 | 49.00 46.57 | 42.67 52.72 |
| Buccal Surface | Mesial Surface | Palatal Surface | Distal Surface | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean Marginal Gap Gcem ONE (μm) | Mean ±SD | CI—Upper/ Lower Limit | Min Max | Mean ±SD | CI—Upper/ Lower Limit | Min Max | Mean ±SD | CI—Upper/ Lower Limit | Min Max | Mean ±SD | CI—Upper/ Lower Limit | Min Max |
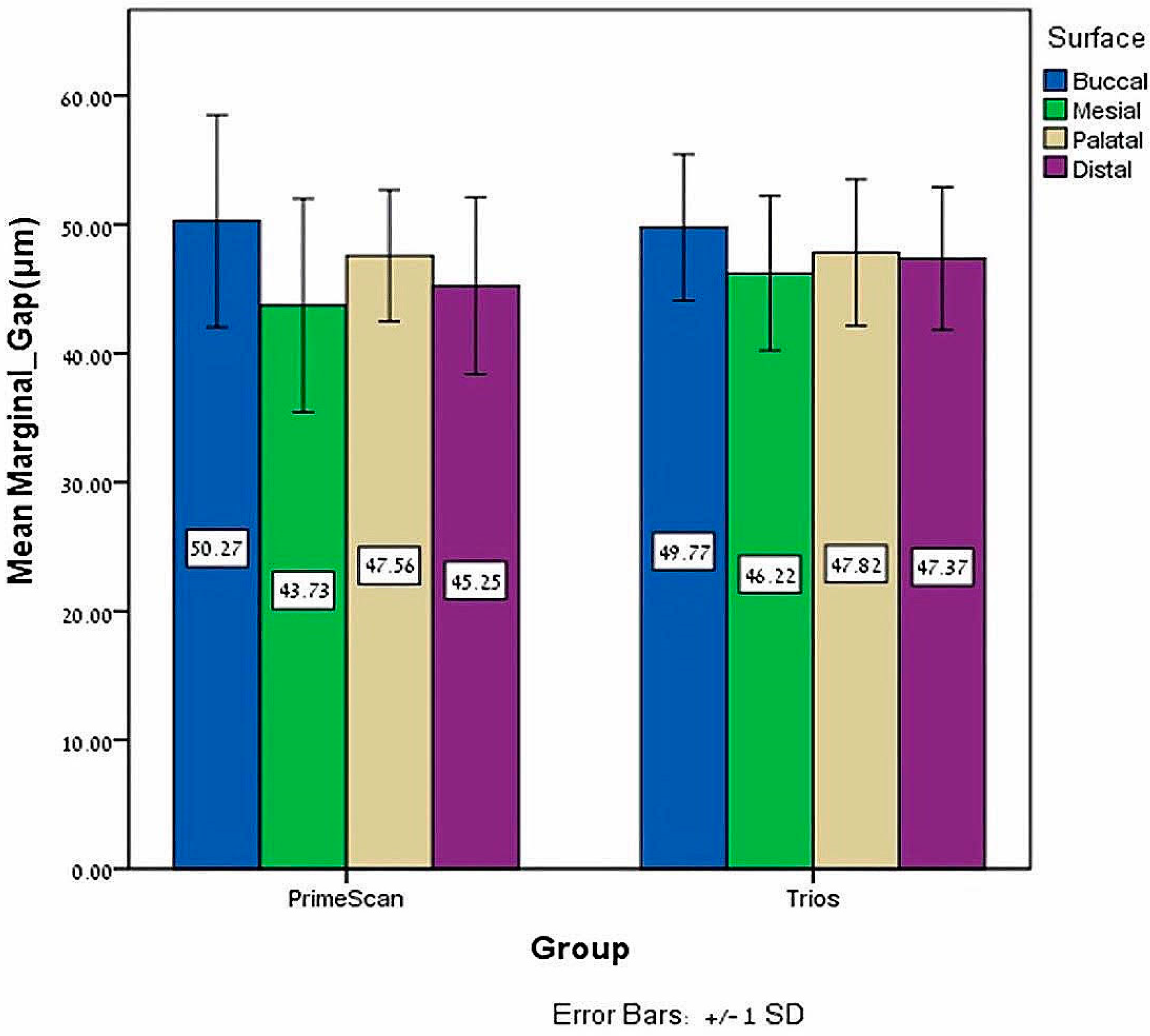
| Primescan | 50.26 ±8.22 | 54.11 46.41 | 33.07 62.67 | 43.72 ±8.27 | 47.59 39.85 | 27.72 57.44 | 47.56 ±5.09 | 49.94 45.17 | 35.90 59.00 | 45.24 ±6.86 | 48.45 42.03 | 35.54 59.16 |
| Trios | 49.76 ±5.67 | 52.42 47.11 | 32.28 57.50 | 46.21 ±5.97 | 49.01 43.42 | 34.49 56.14 | 47.82 ±5.66 | 50.47 45.16 | 34.65 56.60 | 47.36 ±5.52 | 49.94 44.78 | 36.35 54.95 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shely, A.; Nissan, J.; Rosner, O.; Zenziper, E.; Lugassy, D.; Abidulkrem, K.; Ben-Izhack, G. The Impact of Open versus Closed Computer-Aided Design/Computer-Aided Manufacturing Systems on the Marginal Gap of Zirconia-Reinforced Lithium Silicate Single Crowns Evaluated by Scanning Electron Microscopy: A Comparative In Vitro Study. J. Funct. Biomater. 2024, 15, 130. https://doi.org/10.3390/jfb15050130
Shely A, Nissan J, Rosner O, Zenziper E, Lugassy D, Abidulkrem K, Ben-Izhack G. The Impact of Open versus Closed Computer-Aided Design/Computer-Aided Manufacturing Systems on the Marginal Gap of Zirconia-Reinforced Lithium Silicate Single Crowns Evaluated by Scanning Electron Microscopy: A Comparative In Vitro Study. Journal of Functional Biomaterials. 2024; 15(5):130. https://doi.org/10.3390/jfb15050130
Chicago/Turabian StyleShely, Asaf, Joseph Nissan, Ofir Rosner, Eran Zenziper, Diva Lugassy, Khadija Abidulkrem, and Gil Ben-Izhack. 2024. "The Impact of Open versus Closed Computer-Aided Design/Computer-Aided Manufacturing Systems on the Marginal Gap of Zirconia-Reinforced Lithium Silicate Single Crowns Evaluated by Scanning Electron Microscopy: A Comparative In Vitro Study" Journal of Functional Biomaterials 15, no. 5: 130. https://doi.org/10.3390/jfb15050130
APA StyleShely, A., Nissan, J., Rosner, O., Zenziper, E., Lugassy, D., Abidulkrem, K., & Ben-Izhack, G. (2024). The Impact of Open versus Closed Computer-Aided Design/Computer-Aided Manufacturing Systems on the Marginal Gap of Zirconia-Reinforced Lithium Silicate Single Crowns Evaluated by Scanning Electron Microscopy: A Comparative In Vitro Study. Journal of Functional Biomaterials, 15(5), 130. https://doi.org/10.3390/jfb15050130







