Evaluation of the Effect of Primary and Secondary Closure on the Use of Leukocyte and Platelet-Rich Fibrin in Impacted Lower Third Molar Surgery
Abstract
1. Introduction
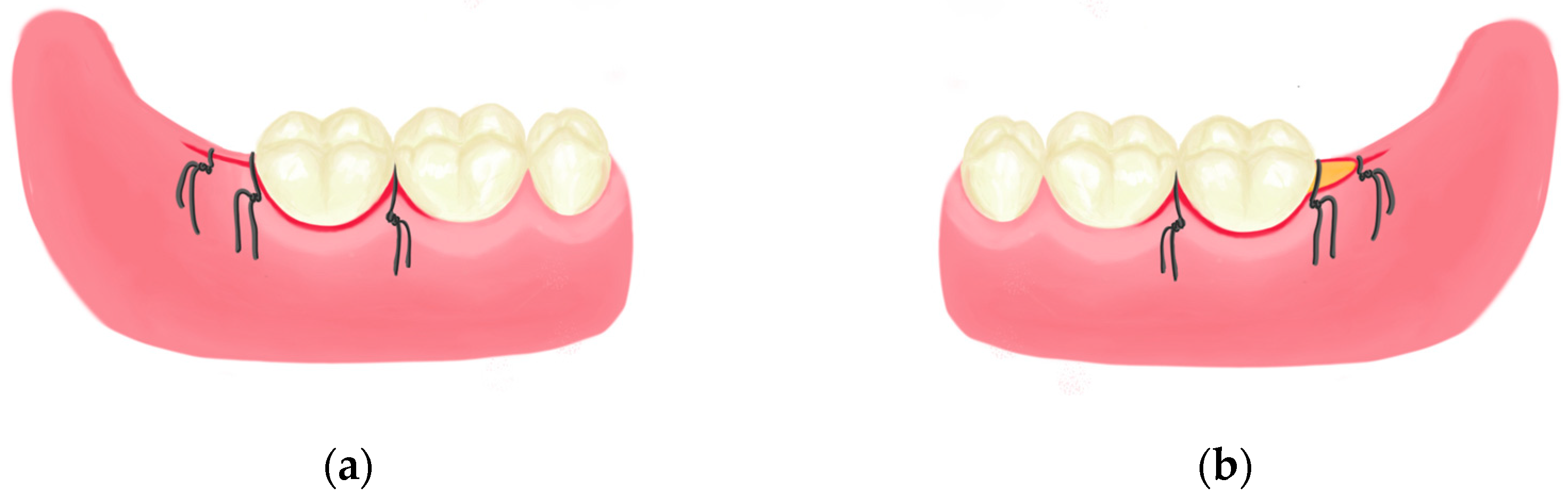
2. Materials and Methods
2.1. Study Groups
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Duarte-Rodrigues, L.; Miranda, E.F.P.; Souza, T.O.; de Paiva, H.N.; Falci, S.G.M.; Galvão, E.L. Third molar removal and its impact on quality of life: Systematic review and meta-analysis. Qual. Life Res. 2018, 27, 2477–2489. [Google Scholar] [CrossRef] [PubMed]
- Sifuentes-Cervantes, J.S.; Carrillo-Morales, F.; Castro-Núñez, J.; Cunningham, L.L.; Van Sickels, J.E. Third molar surgery: Past, present, and the future. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 132, 523–531. [Google Scholar] [CrossRef]
- Kasapoglu, M.B.; Cebi, A.T. Randomized split-mouth study for evaluating the efficacy of nimesulide and nimesulide + Thiocolchicoside combination following impacted mandibular third molar surgery. Niger. J. Clin. Pract. 2022, 25, 641–646. [Google Scholar] [CrossRef]
- Bailey, E.; Kashbour, W.; Shah, N.; Worthington, H.V.; Renton, T.F.; Coulthard, P. Surgical techniques for the removal of mandibular wisdom teeth. Cochrane Database Syst. Rev. 2020, 7, CD004345. [Google Scholar] [CrossRef]
- Bello, S.A.; Olaitan, A.A.; Ladeinde, A.L. A randomized comparison of the effect of partial and total wound closure techniques on postoperative morbidity after mandibular third molar surgery. J. Oral Maxillofac. Surg. 2011, 69, e24–e30. [Google Scholar] [CrossRef]
- Maria, A.; Malik, M.; Virang, P. Comparison of primary and secondary closure of the surgical wound after removal of impacted mandibular third molars. J. Maxillofac. Oral Surg. 2012, 11, 276–283. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Danda, A.K.; Krishna Tatiparthi, M.; Narayanan, V.; Siddareddi, A. Influence of primary and secondary closure of surgical wound after impacted mandibular third molar removal on postoperative pain and swelling--a comparative and split mouth study. J. Oral Maxillofac. Surg. 2010, 68, 309–312. [Google Scholar] [CrossRef] [PubMed]
- Pasqualini, D.; Cocero, N.; Castella, A.; Mela, L.; Bracco, P. Primary and secondary closure of the surgical wound after removal of impacted mandibular third molars: A comparative study. Int. J. Oral Maxillofac. Surg. 2005, 34, 52–57. [Google Scholar] [CrossRef]
- de Santana, I.H.; Viana, M.R.; Galiza, L.S.; Pereira, K.C.; de Medeiros Paiva, L.M.; de Medeiros Lira, A.C.; Nascimento, J.V.; da Silva Araújo, U.; Bezerra, R.V.; Moreira, J.B.; et al. Applications of platelet-and leukocyte-rich fibrin (L-PRF) in Oral and Maxillofacial Surgery. Braz. J. Implantol. Health Sci. 2023, 5, 4703–4718. [Google Scholar] [CrossRef]
- Zwittnig, K.; Mukaddam, K.; Vegh, D.; Herber, V.; Jakse, N.; Schlenke, P.; Zrnc, T.A.; Payer, M. Platelet-rich fibrin in oral surgery and implantology: A narrative review. Transfus. Med. Hemotherapy 2023, 50, 348–359. [Google Scholar] [CrossRef]
- Barhate, U.H.; Mangaraj, M.; Jena, A.; Sharan, J. Applications of Platelet Rich Fibrin in Dental Surgery: A Comprehensive Literature Review. Trends Biomater. Artif. Organs 2021, 35, 203–213. [Google Scholar]
- Özalp, Ö.; Yıldırımyan, N.; Öztürk, C.; Kocabalkan, B.; Şimşek Kaya, G.; Sindel, A.; Altay, M.A. Promising results of surgical management of advanced medication related osteonecrosis of the jaws using adjunctive leukocyte and platelet rich fibrin. BMC Oral Health 2021, 21, 613. [Google Scholar] [CrossRef] [PubMed]
- da Silva, M.T.; de Almeida Barros Mourão, C.F.; Mello-Machado, R.C.; Montemezzi, P.; de Lima Barbosa, R.; Sartoretto, S.C.; Leite, P.E.C.; Javid, K.; Kawase, T.; Alves, G.G.; et al. Effects of Leukocyte-Platelet-Rich Fibrin (L–PRF) on Pain, Soft Tissue Healing, Growth Factors, and Cytokines after Third Molar Extraction: A Randomized, Split-Mouth, Double-Blinded Clinical Trial. Appl. Sci. 2021, 11, 1666. [Google Scholar] [CrossRef]
- Naeimi Darestani, M.; Asl Roosta, H.; Mosaddad, S.A.; Yaghoubee, S. The effect of leukocyte-and platelet-rich fibrin on the bone loss and primary stability of implants placed in posterior maxilla: A randomized clinical trial. Int. J. Implant. Dent. 2023, 9, 23. [Google Scholar] [CrossRef] [PubMed]
- Aravena, P.C.; Sandoval, S.P.; Pizarro, F.E.; Simpson, M.I.; Castro-Adams, N.; Serandour, G.; Rosas, C. Leukocyte and platelet-rich fibrin have same effect as blood clot in the 3-dimensional alveolar ridge preservation. A split-mouth randomized clinical trial. J. Oral Maxillofac. Surg. 2021, 79, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Daugela, P.; Grimuta, V.; Sakavicius, D.; Jonaitis, J.; Juodzbalys, G. Influence of leukocyte- and platelet-rich fibrin (L-PRF) on the outcomes of impacted mandibular third molar removal surgery: A split-mouth randomized clinical trial. Quintessence Int. 2018, 49, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.T.; Zhang, S.; Leung, Y.Y.; Li, S.K.; Tsang, C.C.; Chu, C.H. Patients’ satisfaction and prevalence of complications on surgical extraction of third molar. Patient Prefer. Adherence 2015, 9, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Dohan, D.M.; Choukroun, J.; Diss, A.; Dohan, S.L.; Dohan, A.J.; Mouhyi, J.; Gogly, B. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. J. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, e45–e50. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.-S.; Feng, Z.-H.; Wu, G.-F.; Bai, S.-Z.; Dong, Y.; Chen, F.-M.; Zhao, Y.-M. The use of platelet-rich fibrin combined with periodontal ligament and jaw bone mesenchymal stem cell sheets for periodontal tissue engineering. Sci. Rep. 2016, 6, 28126. [Google Scholar] [CrossRef]
- Gassling, V.; Douglas, T.; Warnke, P.H.; Açil, Y.; Wiltfang, J.; Becker, S.T. Platelet-rich fibrin membranes as scaffolds for periosteal tissue engineering. Clin. Oral Implant. Res. 2010, 21, 543–549. [Google Scholar] [CrossRef]
- Dubois, D.D.; Pizer, M.E.; Chinnis, R.J. Comparison of primary and secondary closure techniques after removal of impacted mandibular third molars. J. Oral Maxillofac. Surg. 1982, 40, 631–634. [Google Scholar] [CrossRef]
- Carrasco-Labra, A.; Brignardello-Petersen, R.; Yanine, N.; Araya, I.; Guyatt, G. Secondary versus primary closure techniques for the prevention of postoperative complications following removal of impacted mandibular third molars: A systematic review and meta-analysis of randomized controlled trials. J. Oral Maxillofac. Surg. 2012, 70, e441–e457. [Google Scholar] [CrossRef]
- Chaudhary, M.; Singh, M.; Singh, S.; Singh, S.P.; Kaur, G. Primary and secondary closure technique following removal of impacted mandibular third molars: A comparative study. Natl. J. Maxillofac. Surg. 2012, 3, 10–14. [Google Scholar]
- Aggarwal, V.; Umarani, M.; Baliga, S.D.; Issrani, R.; Prabhu, N. Comparison between primary and secondary method of closing surgical wound after tooth extraction: A split-mouth study. Pesqui. Bras. Odontopediatria Clín Integr. 2021, 21, e0227. [Google Scholar] [CrossRef]
- Varghese, M.P.; Manuel, S.; Surej Kumar, L.K. Potential for Osseous Regeneration of Platelet Rich Fibrin—A Comparative Study in Mandibular Third Molar Impaction Sockets. J. Oral Maxillofac. Surg. 2017, 75, 1322–1329. [Google Scholar] [CrossRef]
- Baqain, Z.H.; Al-Shafii, A.; Hamdan, A.A.; Sawair, F.A. Flap design and mandibular third molar surgery: A split mouth randomized clinical study. Int. J. Oral Maxillofac. Surg. 2012, 41, 1020–1024. [Google Scholar] [CrossRef]
- Mobilio, N.; Gremigni, P.; Pramstraller, M.; Vecchiatini, R.; Calura, G.; Catapano, S. Explaining pain after lower third molar extraction by preoperative pain assessment. J. Oral Maxillofac. Surg. 2011, 69, 2731–2738. [Google Scholar] [CrossRef]
- Loh, S.Y.; Mcleod, R.W.J.; Elhassan, H.A. Trismus following different treatment modalities for head and neck cancer: A systematic review of subjective measures. Eur. Arch. Otorhinolaryngol. 2017, 274, 2695–2707. [Google Scholar] [CrossRef]
- Kaplan, V.; Ciğerim, L.; Çınarsoy Ciğerim, S.; Bazyel, Z.D.; Dinç, G. Comparison of Various Measurement Methods in the Evaluation of Swelling after Third Molar Surgery. Van. Tıp Derg. 2021, 28, 412–420. [Google Scholar] [CrossRef]
- Antonelli, A.; Barone, S.; Bennardo, F.; Giudice, A. Three-dimensional facial swelling evaluation of pre-operative single-dose of prednisone in third molar surgery: A split-mouth randomized controlled trial. BMC Oral Health 2023, 23, 614. [Google Scholar] [CrossRef] [PubMed]
- Dar, M.; Hakim, T.; Shah, A.; Najar, L.; Yaqoob, G.; Lanker, F. Use of autologous platelet-rich fibrin in osseous regeneration after cystic enucleation: A clinical study. J. Oral Biol. Craniofac Res. 2016, 6 (Suppl. S1), S29–S32. [Google Scholar] [CrossRef]
- Tadic, A.; Bajkin, B.; Mijatov, I.; Mirnic, J.; Vukoje, K.; Sokac, M.; Vukelic, D. Influence of L-PRF Topical Application on Bone Tissue Healing after Surgical Extraction of Impacted Mandibular Third Molars: Randomized Split-Mouth Clinical Study. Appl. Sci. 2023, 13, 4823. [Google Scholar] [CrossRef]
- Caymaz, M.G.; Uyanik, L.O. Comparison of the effect of advanced platelet-rich fibrin and leukocyte-and platelet-rich fibrin on outcomes after removal of impacted mandibular third molar: A randomized split-mouth study. Niger. J. Clin. Pract. 2019, 22, 546–552. [Google Scholar] [CrossRef]
- Ritto, F.G.; Pimentel, T.; Canellas, J.V.S.; Junger, B.; Cruz, M.; Medeiros, P.J. Randomized double-blind clinical trial evaluation of bone healing after third molar surgery with the use of leukocyte- and platelet-rich fibrin. Int. J. Oral Maxillofac. Surg. 2019, 48, 1088–1093. [Google Scholar] [CrossRef]
- de Almeida Barros Mourão, C.F.; de Mello-Machado, R.C.; Javid, K.; Moraschini, V. The use of leukocyte- and platelet-rich fibrin in the management of soft tissue healing and pain in post-extraction sockets: A randomized clinical trial. J. Craniomaxillofac Surg. 2020, 48, 452–457. [Google Scholar] [CrossRef]
- Afat, I.M.; Akdoğan, E.T.; Gönül, O. Effects of leukocyte- and platelet-rich fibrin alone and combined with hyaluronic acid on early soft tissue healing after surgical extraction of impacted mandibular third molars: A prospective clinical study. J. Craniomaxillofac Surg. 2019, 47, 280–286. [Google Scholar] [CrossRef]
| Age | Min–Max: (18–39) | Mean: 22.42 ± 3.36 | |
|---|---|---|---|
| n | % | ||
| Gender | Female | 23 | 63.9 |
| Male | 13 | 36.1 |
| Groups | p2 | ||||
|---|---|---|---|---|---|
| Primary Closure | Secondary Closure | ||||
| Mean | Sd | Mean | Sd | ||
| Preoperative mouth opening | 45.56 | 6.51 | 44.23 | 6.37 | 0.547 |
| 2nd-postoperative-day mouth opening | 26.47 | 8.26 | 25.56 | 6.93 | 0.612 |
| 7th-postoperative-day mouth opening | 38.61 | 8.00 | 36.39 | 6.20 | 0.192 |
| p1 = 0.528 | |||||
| Preoperative face measurements | 109.67 | 7.73 | 110.21 | 7.47 | 0.179 |
| 2nd-postoperative-day face measurements | 114.72 | 8.10 | 111.78 | 7.51 | 0.114 |
| 7th-postoperative-day face measurements | 111.00 | 8.65 | 109.22 | 6.89 | 0.338 |
| p1 = 0.157 | |||||
| 6th-hour VAS | 5.83 | 2.48 | 4.50 | 2.72 | 0.033 * |
| 12th-hour VAS | 4.56 | 3.09 | 3.64 | 2.89 | 0.198 |
| 18th-hour VAS | 4.50 | 2.91 | 3.53 | 2.61 | 0.141 |
| 24th-hour VAS | 3.83 | 2.26 | 2.94 | 2.35 | 0.107 |
| 2nd-day VAS | 3.14 | 2.11 | 3.50 | 2.78 | 0.537 |
| 3rd-day VAS | 1.86 | 1.62 | 2.61 | 2.51 | 0.138 |
| 4th-day VAS | 1.31 | 1.53 | 2.06 | 2.12 | 0.090 |
| 5th-day VAS | 0.86 | 1.31 | 1.56 | 2.09 | 0.096 |
| 6th-day VAS | 0.81 | 1.51 | 1.17 | 1.54 | 0.318 |
| 7th-day VAS | 0.61 | 1.23 | 1.06 | 1.58 | 0.187 |
| p1 = 0.000 * | |||||
| Rescue analgesic number | 8.81 | 5.59 | 7.39 | 4.92 | 0.257 |
| Gender | p | ||||
|---|---|---|---|---|---|
| Female | Male | ||||
| Mean | Sd | Mean | Sd | ||
| Preoperative mouth opening | 44.48 | 6.70 | 47.46 | 5.94 | 0.191 |
| 2nd-postoperative-day mouth opening | 24.96 | 6.69 | 29.15 | 10.24 | 0.146 |
| 7th-postoperative-day mouth opening | 36.96 | 6.95 | 41.54 | 9.15 | 0.100 |
| Preoperative face measurements | 106.74 | 6.68 | 114.85 | 6.85 | 0.001 * |
| 2nd-postoperative-day face measurements | 111.74 | 6.33 | 120.00 | 8.42 | 0.002 * |
| 7th-postoperative-day face measurements | 108.48 | 8.04 | 115.46 | 8.13 | 0.018 * |
| 6th-hour VAS | 5.83 | 2.64 | 5.85 | 2.27 | 0.982 |
| 12th-hour VAS | 4.09 | 2.73 | 5.38 | 3.62 | 0.232 |
| 18th-hour VAS | 4.22 | 2.81 | 5.00 | 3.14 | 0.447 |
| 24th-hour VAS | 3.65 | 2.25 | 4.15 | 2.34 | 0.530 |
| 2nd-day VAS | 3.13 | 1.71 | 3.15 | 2.76 | 0.975 |
| 3rd-day VAS | 1.61 | 1.53 | 2.31 | 1.75 | 0.220 |
| 4th-day VAS | 0.87 | 1.14 | 2.08 | 1.85 | 0.020 * |
| 5th-day VAS | 0.61 | 0.94 | 1.31 | 1.75 | 0.201 |
| 6th-day VAS | 0.48 | 0.85 | 1.38 | 2.18 | 0.172 |
| 7th-day VAS | 0.35 | 0.78 | 1.08 | 1.71 | 0.166 |
| Rescue analgesic number | 8.17 | 5.20 | 9.92 | 6.28 | 0.375 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orhan, Z.D.; Ciğerim, L.; Güzel, M.; Doğru, İ.; Alsmadi, M.; Kahraman, N.H.; Hussein, A.; Tatar, K. Evaluation of the Effect of Primary and Secondary Closure on the Use of Leukocyte and Platelet-Rich Fibrin in Impacted Lower Third Molar Surgery. Appl. Sci. 2024, 14, 4228. https://doi.org/10.3390/app14104228
Orhan ZD, Ciğerim L, Güzel M, Doğru İ, Alsmadi M, Kahraman NH, Hussein A, Tatar K. Evaluation of the Effect of Primary and Secondary Closure on the Use of Leukocyte and Platelet-Rich Fibrin in Impacted Lower Third Molar Surgery. Applied Sciences. 2024; 14(10):4228. https://doi.org/10.3390/app14104228
Chicago/Turabian StyleOrhan, Zeynep Dilan, Levent Ciğerim, Mehmet Güzel, İbrahim Doğru, Mohammad Alsmadi, Nazlı Hilal Kahraman, Abdalrahim Hussein, and Kader Tatar. 2024. "Evaluation of the Effect of Primary and Secondary Closure on the Use of Leukocyte and Platelet-Rich Fibrin in Impacted Lower Third Molar Surgery" Applied Sciences 14, no. 10: 4228. https://doi.org/10.3390/app14104228
APA StyleOrhan, Z. D., Ciğerim, L., Güzel, M., Doğru, İ., Alsmadi, M., Kahraman, N. H., Hussein, A., & Tatar, K. (2024). Evaluation of the Effect of Primary and Secondary Closure on the Use of Leukocyte and Platelet-Rich Fibrin in Impacted Lower Third Molar Surgery. Applied Sciences, 14(10), 4228. https://doi.org/10.3390/app14104228






