Effects of Functional Strength Training Combined with Aerobic Training on Body Composition, Physical Fitness, and Movement Quality in Obese Adolescents
Abstract
1. Introduction
2. Materials and Methods
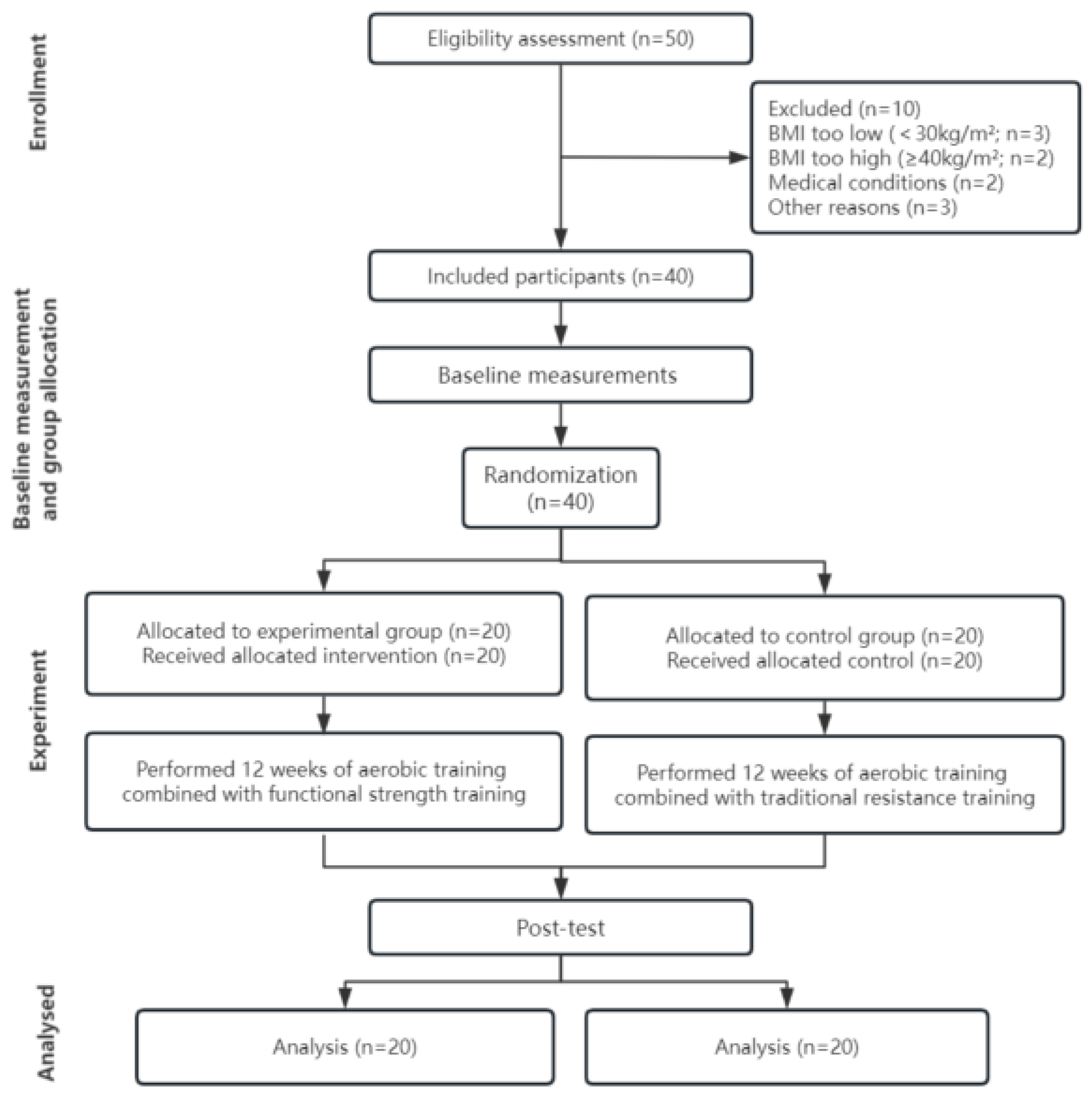
2.1. Participants
2.2. Study Design
2.3. Training Protocols
2.4. Aerobic Training
2.5. TST Program
2.6. FST Program
2.7. Diet Program
2.8. Anthropometric and Body Composition Assessments
2.9. Physical Fitness Assessments
2.10. Movement Quality Assessments
2.11. Statistical Analysis
3. Results
3.1. Anthropometric and Body Composition Results
3.2. Physical Fitness
3.3. Movement Quality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef] [PubMed]
- Kelly, T.; Yang, W.; Chen, C.S.; Reynolds, K.; He, J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. 2008, 32, 1431–1437. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Cong, D.; Wang, G.; Sun, J.; Ji, Y.; Zhong, Z.; Liu, T.; Liu, J.; Chu, Y.; Wu, X. Tuina combined with diet and exercise for simple obesity: A protocol for systematic review. Medicine 2022, 101, e28833. [Google Scholar] [CrossRef] [PubMed]
- Halfon, N.; Larson, K.; Slusser, W. Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of US children aged 10 to 17. Acad. Pediatr. 2013, 13, 6–13. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee; World Health Organization Technical Report Series; World Health Organization: Geneva, Switzerland, 1995; Volume 854, pp. 1–452. [Google Scholar]
- Chen, G.; Chen, J.; Liu, J.; Hu, Y.; Liu, Y. Relationship between body mass index and physical fitness of children and adolescents in Xinjiang, China: A cross-sectional study. BMC Public Health 2022, 22, 1680. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, D.J.; Erskine, R.M.; Morse, C.I.; Winwood, K.; Onambélé-Pearson, G. The impact of obesity on skeletal muscle strength and structure through adolescence to old age. Biogerontology 2016, 17, 467–483. [Google Scholar] [CrossRef]
- King, A.C.; Challis, J.H.; Bartok, C.; Costigan, F.A.; Newell, K.M. Obesity, mechanical and strength relationships to postural control in adolescence. Gait Posture 2012, 35, 261–265. [Google Scholar] [CrossRef]
- Molina-Garcia, P.; Migueles, J.H.; Cadenas-Sanchez, C.; Esteban-Cornejo, I.; Mora-Gonzalez, J.; Rodriguez-Ayllon, M.; Plaza-Florido, A.; Molina-Molina, A.; Garcia-Delgado, G.; D’hondt, E.; et al. Fatness and fitness in relation to functional movement quality in overweight and obese children. J. Sports Sci. 2019, 37, 878–885. [Google Scholar] [CrossRef] [PubMed]
- Hills, A.P.; Hennig, E.M.; Byrne, N.M.; Steele, J.R. The biomechanics of adiposity--structural and functional limitations of obesity and implications for movement. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2002, 3, 35–43. [Google Scholar] [CrossRef]
- Jinning, Z.; Hongjuan, L. Correlation analysis of relation between adolescent sports injuries and fitness. J. Wuhan Sports Univ. 2017, 51, 96–100. [Google Scholar] [CrossRef]
- Molina-Garcia, P.; Plaza-Florido, A.; Mora-Gonzalez, J.; Torres-Lopez, L.V.; Vanrenterghem, J.; Ortega, F.B. Role of physical fitness and functional movement in the body posture of children with overweight/obesity. Gait Posture 2020, 80, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Duncan, M.J.; Stanley, M.; Liddington Wright, S. The association between functional movement and overweight and obesity in British primary school children. BMC Sports Sci. Med. Rehabil. 2013, 5, 11. [Google Scholar] [CrossRef]
- Alberga, A.S.; Sigal, R.J.; Goldfield, G.; Prudhomme, D.; Kenny, G.P. Overweight and obese teenagers: Why is adolescence a critical period? Pediatr. Obes. 2012, 7, 261–273. [Google Scholar] [CrossRef] [PubMed]
- Alberga, A.S.; Prudhomme, D.; Sigal, R.J.; Goldfield, G.S.; Hadjiyianakies, S.; Phillips, P.; Malcolm, J.; Ma, J.; Doucette, S.; Gougeon, R.; et al. Effects of aerobic training, resistance training, or both on cardiorespiratory and musculoskeletal fitness in adolescents with obesity: The HEARTY trial. Appl. Physiol. Nutr. Metab. 2016, 41, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Lee, K.J.; Jeon, Y.J.; Ahn, M.B.; Jung, I.A.; Kim, S.H.; Cho, W.K.; Cho, K.S.; Park, S.H.; Jung, M.H.; et al. Relationships of physical fitness and obesity with metabolic risk factors in children and adolescents: Chungju city cohort study. Ann. Pediatr. Endocrinol. Metab. 2016, 21, 31–38. [Google Scholar] [CrossRef]
- Ho, H.C.H.; Maddaloni, E.; Buzzetti, R. Risk factors and predictive biomarkers of early cardiovascular disease in obese youth. Diabetes/Metab. Res. Rev. 2019, 35, e3134. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P.; American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Sigal, R.J.; Alberga, A.S.; Goldfield, G.S.; Prudhomme, D.; Hadjiyianakies, S.; Gougeon, R.; Phillips, P.; Tulloch, H.; Malcolm, J.; Doucette, S.; et al. Effects of aerobic training, resistance training, or both on percentage body fat and cardiometabolic risk markers in obese adolescents: The healthy eating aerobic and resistance training in youth randomized clinical trial. JAMA Pediatr. 2014, 168, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Schranz, N.; Tomkinson, G.; Olds, T. What is the effect of resistance training on the strength, body composition and psychosocial status of overweight and obese children and adolescents? A Systematic review and meta-analysis. Sports Med. 2013, 43, 893–907. [Google Scholar] [CrossRef]
- Lee, J. Influences of exercise interventions on overweight and obesity in children and adolescents. Public Health Nurs. 2021, 38, 502–516. [Google Scholar] [CrossRef]
- Jakicic, J.M.; Clark, K.; Coleman, E.; Donnelly, J.E.; Foreyt, J.; Melanson, E.; Volek, J.; Volpe, S.L.; American College of Sports Medicine. Appropriate Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults. Med. Sci. Sports Exerc. 2001, 33, 2145–2156. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.S.; Dhaliwal, S.S.; Hills, A.P.; Pal, S. The effect of 12 weeks of aerobic, resistance or combination exercise training on cardiovascular risk factors in the overweight and obese in a randomized trial. BMC Public Health 2012, 12, 704. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Ramírez-Vélez, R.; Ramírez-Campillo, R.; Peterson, M.D.; Martínez-Vizcaíno, V. Concurrent aerobic plus resistance exercise versus aerobic exercise alone to improve health outcomes in pediatric obesity: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Lopez, P.; Taaffe, D.R.; Galvão, D.A.; Newton, R.U.; Nonemacher, E.R.; Wendt, V.M.; Bassanesi, R.N.; Turella, D.J.P.; Rech, A. Resistance training effectiveness on body composition and body weight outcomes in individuals with overweight and obesity across the lifespan: A systematic review and meta-analysis. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2022, 23, e13428. [Google Scholar] [CrossRef] [PubMed]
- Liao, T.; Duhig, S.J.; Du, G.; Luo, B.; Wang, Y.T. The Effect of a Functional Strength Training Intervention on Movement Quality and Physical Fitness in Adolescents. Percept. Mot. Ski. 2022, 129, 176–194. [Google Scholar] [CrossRef]
- Liao, T.; Li, L.; Wang, Y.T. Effects of Functional Strength Training Program on Movement Quality and Fitness Performance Among Girls Aged 12–13 Years. J. Strength Cond. Res. 2019, 33, 1534–1541. [Google Scholar] [CrossRef] [PubMed]
- Mile, M.; Balogh, L.; Papp, G.; Pucsok, J.M.; Szabó, K.; Barna, L.; Csiki, Z.; Lekli, I. Effects of Functional Training on Sarcopenia in Elderly Women in the Presence or Absence of ACE Inhibitors. Int. J. Environ. Res. Public Health 2021, 18, 6594. [Google Scholar] [CrossRef]
- Guler, O.; Tuncel, O.; Bianco, A.J.S. Effects of functional strength training on functional movement and balance in middle-aged adults. Sustainability 2021, 13, 1074. [Google Scholar] [CrossRef]
- de Resende-Neto, A.G.; Oliveira Andrade, B.C.; Cyrino, E.S.; Behm, D.G.; De-Santana, J.M.; Da Silva-Grigoletto, M.E. Effects of functional and traditional training in body composition and muscle strength components in older women: A randomized controlled trial. Arch. Gerontol. Geriatr. 2019, 84, 103902. [Google Scholar] [CrossRef]
- Ting, L.; Weitao, Z.; Danyang, L. Correlation between core stability, functional movements and adolescents’ physical quality performance. J. Chengdu Sport Univ. 2014, 40, 37–43. [Google Scholar] [CrossRef]
- Lloyd, R.S.; Oliver, J.L.; Radnor, J.M.; Rhodes, B.C.; Faigenbaum, A.D.; Myer, G.D. Relationships between functional movement screen scores, maturation and physical performance in young soccer players. J. Sports Sci. 2015, 33, 11–19. [Google Scholar] [CrossRef]
- Bennett, H.; Arnold, J.; Martin, M.; Norton, K.; Davison, K. A randomized controlled trial of movement quality-focused exercise versus traditional resistance exercise for improving movement quality and physical performance in trained adults. J. Sports Sci. 2019, 37, 2806–2817. [Google Scholar] [CrossRef] [PubMed]
- Neves, L.M.; Fortaleza, A.C.; Rossi, F.E.; Diniz, T.A.; Codogno, J.S.; Gobbo, L.A.; Gobbi, S.; Freitas, I.F., Jr. Functional training reduces body fat and improves functional fitness and cholesterol levels in postmenopausal women: A randomized clinical trial. J. Sports Med. Phys. Fit. 2017, 57, 448–456. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.J.; Hung, W.C.; Sharpe, P.A.; Wai, J.P. Neighborhood environment and physical activity among urban and rural schoolchildren in Taiwan. Health Place 2010, 16, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Alberga, A.S.; Goldfield, G.S.; Kenny, G.P.; Hadjiyianakies, S.; Phillips, P.; Prudhomme, D.; Tulloch, H.; Gougeon, R.; Wells, G.A.; Sigal, R.J. Healthy Eating, Aerobic and Resistance Training in Youth (HEARTY): Study rationale, design and methods. Contemp. Clin. Trials 2012, 33, 839–847. [Google Scholar] [CrossRef] [PubMed]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Weiss, T.; Kreitinger, J.; Wilde, H.; Wiora, C.; Steege, M.; Dalleck, L.; Janot, J. Effect of functional resistance training on muscular fitness outcomes in young adults. J. Exerc. Sci. Fit. 2010, 8, 113–122. [Google Scholar] [CrossRef]
- Mifflin, M.D.; St Jeor, S.T.; Hill, L.A.; Scott, B.J.; Daugherty, S.A.; Koh, Y.O. A new predictive equation for resting energy expenditure in healthy individuals. Am. J. Clin. Nutr. 1990, 51, 241–247. [Google Scholar] [CrossRef]
- Yuexin, Y. China Food Composition; Peking University Press: Beijing, China, 2002. [Google Scholar]
- Meyers, L.D.; Hellwig, J.P.; Otten, J.J. Dietary reference intakes: The essential guide to nutrient requirements. Am. J. Clin. Nutr. 2006, 85, 924. [Google Scholar] [CrossRef]
- Cook, G.; Burton, L.; Hoogenboom, B. Pre-participation screening: The use of fundamental movements as an assessment of function—Part 1. N. Am. J. Sports Phys. Ther. NAJSPT 2006, 1, 62–72. [Google Scholar] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavior Science: Lawrance Eribaum Association; Academic Press Books-Elsevier: Cambridge, MA, USA, 1988. [Google Scholar]
- Matłosz, P.; Michałowska, J.; Sarnik, G.; Herbert, J.; Przednowek, K.; Grzywacz, R.; Polak, E. Analysis of the correlation between body composition, construction and aerobic capacity in teenage team sport training. Eur. J. Clin. Exp. Med. 2018, 16, 109–116. [Google Scholar] [CrossRef]
- Lamberth, J.; Hale, B.; Knight, A.; Boyd, J.; Luczak, T. Effectiveness of a Six-Week Strength and Functional Training Program on Golf Performance. Int. J. Golf. Sci. 2013, 2, 33–42. [Google Scholar] [CrossRef]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional movement screening: The use of fundamental movements as an assessment of function—Part 1. Int. J. Sports Phys. Ther. 2014, 9, 396–409. [Google Scholar] [PubMed]
- Parchmann, C.J.; McBride, J.M. Relationship between functional movement screen and athletic performance. J. Strength Cond. Res. 2011, 25, 3378–3384. [Google Scholar] [CrossRef] [PubMed]
- Arriscado, D.; Muros, J.J.; Zabala, M.; Dalmau, J.M. Relationship between physical fitness and body composition in primary school children in northern Spain (Logroño). Nutr. Hosp. 2014, 30, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Nóbrega, A.C.; Paula, K.C.; Carvalho, A.C. Interaction between resistance training and flexibility training in healthy young adults. J. Strength Cond. Res. 2005, 19, 842–846. [Google Scholar] [CrossRef]
- Dumith, S.C.; Ramires, V.V.; Souza, M.A.; Moraes, D.S.; Petry, F.G.; Oliveira, E.S.; Ramires, S.V.; Hallal, P.C. Overweight/obesity and physical fitness among children and adolescents. J. Phys. Act. Health 2010, 7, 641–648. [Google Scholar] [CrossRef]
- Lockie, R.G.; Murphy, A.J.; Knight, T.J.; Janse de Jonge, X.A. Factors that differentiate acceleration ability in field sport athletes. J. Strength Cond. Res. 2011, 25, 2704–2714. [Google Scholar] [CrossRef]
- Morin, J.B.; Edouard, P.; Samozino, P. Technical ability of force application as a determinant factor of sprint performance. Med. Sci. Sports Exerc. 2011, 43, 1680–1688. [Google Scholar] [CrossRef]
- Duncan, M.J.; Stanley, M. Functional movement is negatively associated with weight status and positively associated with physical activity in British primary school children. J. Obes. 2012, 2012, 697563. [Google Scholar] [CrossRef]





| TG (n = 20) | CG (n = 20) | |||
|---|---|---|---|---|
| Females (n = 8) | Males (n = 12) | Females (n = 8) | Males (n = 12) | |
| Age (years) | 12.9 ± 2.0 | 13.6 ± 0.9 | 12.9 ± 2.0 | 13.6 ± 1.2 |
| Height (m) | 1.61 ± 0.08 | 1.61 ± 0.09 | 1.60 ± 0.07 | 1.63 ± 0.09 |
| Body mass (kg) | 76.5 ± 14.9 | 83.1 ± 19.9 | 76.1 ± 14.9 | 83.7 ± 17.3 |
| BMI (kg/m2) | 29.2 ± 3.7 | 31.5 ± 4.9 | 29.5 ± 3.4 | 31.0 ± 3.5 |
| A | B | C | D | E |
|---|---|---|---|---|
| Bench press | Incline bench press | Chest fly | Decline barbell bench press | Bench press |
| Seated row | Lateral pulldown | Seated row | Seated row | Hyperextension |
| Lateral raise | Shoulder press | Front raise | Shoulder press | Lateral raise |
| Alternate dumbbell curl | Preacher curl | Dumbbell triceps Extension | Concentration curls | Alternate dumbbell curls |
| Tricep press | Assisted tricep dips | Squat | Leg press | Seated leg press |
| Squat | Straight leg raises | Seated leg press | Leg extension | Seated leg curl |
| Standing calf raise | Seated leg press | Standing calf raise | Lying leg curl | Barbell calf raise |
| Sit-up | Broomstick twist | Sit-ups | Broomstick twist | Sit-ups |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Z.; Ma, H.; Zhang, W.; Zhang, Y.; Youssef, L.; Carneiro, M.A.S.; Chen, C.; Wang, D.; Wang, D. Effects of Functional Strength Training Combined with Aerobic Training on Body Composition, Physical Fitness, and Movement Quality in Obese Adolescents. Nutrients 2024, 16, 1434. https://doi.org/10.3390/nu16101434
Wang Z, Ma H, Zhang W, Zhang Y, Youssef L, Carneiro MAS, Chen C, Wang D, Wang D. Effects of Functional Strength Training Combined with Aerobic Training on Body Composition, Physical Fitness, and Movement Quality in Obese Adolescents. Nutrients. 2024; 16(10):1434. https://doi.org/10.3390/nu16101434
Chicago/Turabian StyleWang, Zhihai, Huihui Ma, Weiwei Zhang, Yufeng Zhang, Layale Youssef, Marcelo A. S. Carneiro, Chao Chen, Dan Wang, and Dexin Wang. 2024. "Effects of Functional Strength Training Combined with Aerobic Training on Body Composition, Physical Fitness, and Movement Quality in Obese Adolescents" Nutrients 16, no. 10: 1434. https://doi.org/10.3390/nu16101434
APA StyleWang, Z., Ma, H., Zhang, W., Zhang, Y., Youssef, L., Carneiro, M. A. S., Chen, C., Wang, D., & Wang, D. (2024). Effects of Functional Strength Training Combined with Aerobic Training on Body Composition, Physical Fitness, and Movement Quality in Obese Adolescents. Nutrients, 16(10), 1434. https://doi.org/10.3390/nu16101434





