Effect of Luting Materials on the Accuracy of Fit of Zirconia Copings: A Non-Destructive Digital Analysis Method
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- -
- The digital non-destructive method was able to detect the influence of the luting material on the fit of a zirconia single-tooth restoration before and after cementation;
- -
- The zinc phosphate cement led to increased vertical marginal discrepancies;
- -
- Only the self-adhesive luting resin did not influence the fit of the restoration after cementation, and can be clinically recommended.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAD | Computer-Aided Design |
| CAM | Computer-Aided Manufacturing |
| 3D | Three-dimensional |
| 2D | Two-dimensional |
| STL | Standard Transformation Language |
| Mean | Mean distance |
| SD | Standard deviation |
| Min | Minimum distance |
| Max | Maximum distance |
References
- Pak, H.S.; Han, J.S.; Lee, J.B.; Kim, S.H.; Yang, J.H. Influence of porcelain veneering on the marginal fit of Digident and Lava CAD/CAM zirconia ceramic crowns. J. Adv. Prosthodont. 2010, 2, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Takeichi, T.; Katsoulis, J.; Blatz, M.B. Clinical outcome of single porcelain-fused-to-zirconium dioxide crowns: A systematic review. J. Prosthet. Dent. 2013, 110, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.H.D.; Lima, E.; Miranda, R.B.P.; Favero, S.S.; Lohbauer, U.; Cesar, P.F. Dental ceramics: A review of new materials and processing methods. Braz. Oral Res. 2017, 31, e58. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Lawn, B.R. Novel Zirconia Materials in Dentistry. J. Dent. Res. 2018, 97, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Duret, F.; Blouin, J.L.; Duret, B. CAD-CAM in dentistry. J. Am. Dent. Assoc. 1988, 117, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Methani, M.M.; Revilla-León, M.; Zandinejad, A. The potential of additive manufacturing technologies and their processing parameters for the fabrication of all-ceramic crowns: A review. J. Esthet. Restor. Dent. 2020, 32, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, T.; Hotta, Y.; Kunii, J.; Kuriyama, S.; Tamaki, Y. A review of dental CAD/CAM: Current status and future perspectives from 20 years of experience. Dent. Mater. J. 2009, 28, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Javaid, M.; Haleem, A. Current status and applications of additive manufacturing in dentistry: A literature-based review. J. Oral Biol. Craniofacial Res. 2019, 9, 179–185. [Google Scholar] [CrossRef]
- Cesar, P.F.; Miranda, R.B.P.; Santos, K.F.; Scherrer, S.S.; Zhang, Y. Recent advances in dental zirconia: 15 years of material and processing evolution. Dent. Mater. 2024, in press. [Google Scholar] [CrossRef]
- Belli, R.; Hurle, K.; Schürrlein, J.; Petschelt, A.; Werbach, K.; Peterlik, H.; Rabe, T.; Mieller, B.; Lohbauer, U. Relationships between fracture toughness, Y2O3 fraction and phases content in modern dental Yttria-doped zirconias. J. Eur. Ceram. Soc. 2021, 41, 7771–7782. [Google Scholar] [CrossRef]
- Jurado, C.A.; Villalobos-Tinoco, J.; Watanabe, H.; Sanchez-Hernandez, R.; Tsujimoto, A. Novel translucent monolithic zirconia fixed restorations in the esthetic zone. Clin. Case Rep. 2022, 10, e05499. [Google Scholar] [CrossRef] [PubMed]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Abbate, M.F.; Tjan, A.H.; Fox, W.M. Comparison of the marginal fit of various ceramic crown systems. J. Prosthet. Dent. 1989, 61, 527–531. [Google Scholar] [CrossRef]
- Vasiliu, R.D.; Porojan, S.D.; Porojan, L. In Vitro Study of Comparative Evaluation of Marginal and Internal Fit between Heat-Pressed and CAD-CAM Monolithic Glass-Ceramic Restorations after Thermal Aging. Materials 2020, 13, 4239. [Google Scholar] [CrossRef]
- Padrós, R.; Giner, L.; Herrero-Climent, M.; Falcao-Costa, C.; Ríos-Santos, J.V.; Gil, F.J. Influence of the CAD-CAM Systems on the Marginal Accuracy and Mechanical Properties of Dental Restorations. Int. J. Environ. Res. Public Health 2020, 17, 4276. [Google Scholar] [CrossRef] [PubMed]
- Demir, N.; Ozturk, A.N.; Malkoc, M.A. Evaluation of the marginal fit of full ceramic crowns by the microcomputed tomography (micro-CT) technique. Eur. J. Dent. 2014, 8, 437–444. [Google Scholar] [CrossRef]
- Felton, D.A.; Kanoy, B.E.; Bayne, S.C.; Wirthman, G.P. Effect of in vivo crown margin discrepancies on periodontal health. J. Prosthet. Dent. 1991, 65, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, M.S.; Windeler, A.S. An investigation of dental luting cement solubility as a function of the marginal gap. J. Prosthet. Dent. 1991, 65, 436–442. [Google Scholar] [CrossRef]
- Tan, P.L.; Gratton, D.G.; Diaz-Arnold, A.M.; Holmes, D.C. An in vitro comparison of vertical marginal gaps of CAD/CAM titanium and conventional cast restorations. J. Prosthodont. 2008, 17, 378–383. [Google Scholar] [CrossRef]
- Balkaya, M.C.; Cinar, A.; Pamuk, S. Influence of firing cycles on the margin distortion of 3 all-ceramic crown systems. J. Prosthet. Dent. 2005, 93, 346–355. [Google Scholar] [CrossRef] [PubMed]
- McLean, J.W.; von Fraunhofer, J.A. The estimation of cement film thickness by an in vivo technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Christensen, G.J. Marginal fit of gold inlay castings. J. Prosthet. Dent. 1966, 16, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Gavelis, J.R.; Morency, J.D.; Riley, E.D.; Sozio, R.B. The effect of various finish line preparations on the marginal seal and occlusal seat of full crown preparations. J. Prosthet. Dent. 1981, 45, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.H.; Kern, M. Marginal discrepancies and leakage of all-ceramic crowns: Influence of luting agents and aging conditions. Int. J. Prosthodont. 2003, 16, 109–116. [Google Scholar] [PubMed]
- Kokubo, Y.; Ohkubo, C.; Tsumita, M.; Miyashita, A.; Vult von Steyern, P.; Fukushima, S. Clinical marginal and internal gaps of Procera AllCeram crowns. J. Oral Rehabil. 2005, 32, 526–530. [Google Scholar] [CrossRef] [PubMed]
- Donovan, T.E.; Cho, G.C. Contemporary evaluation of dental cements. Compend. Contin. Educ. Dent. 1999, 20, 197–199. [Google Scholar]
- Goodacre, C.J.; Campagni, W.V.; Aquilino, S.A. Tooth preparations for complete crowns: An art form based on scientific principles. J. Prosthet. Dent. 2001, 85, 363–376. [Google Scholar] [CrossRef]
- Hill, E.E. Dental cements for definitive luting: A review and practical clinical considerations. Dent. Clin. North. Am. 2007, 51, 643–658. [Google Scholar] [CrossRef]
- Lad, P.P.; Kamath, M.; Tarale, K.; Kusugal, P.B. Practical clinical considerations of luting cements: A review. J. Int. Oral Health 2014, 6, 116–120. [Google Scholar]
- Attin, T.; Vataschki, M.; Hellwig, E. Properties of resin-modified glass-ionomer restorative materials and two polyacid-modified resin composite materials. Quintessence Int. 1996, 27, 203–209. [Google Scholar] [PubMed]
- Berzins, D.W.; Abey, S.; Costache, M.C.; Wilkie, C.A.; Roberts, H.W. Resin-modified glass-ionomer setting reaction competition. J. Dent. Res. 2010, 89, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, E.; Yoshida, Y.; Inoue, S.; Fukuda, R.; Snauwaert, J.; Nakayama, Y.; De Munck, J.; Lambrechts, P.; Suzuki, K.; Van Meerbeek, B. Gel phase formation at resin-modified glass-ionomer/tooth interfaces. J. Dent. Res. 2007, 86, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Leyhausen, G.; Abtahi, M.; Karbakhsch, M.; Sapotnick, A.; Geurtsen, W. Biocompatibility of various light-curing and one conventional glass-ionomer cement. Biomaterials 1998, 19, 559–564. [Google Scholar] [CrossRef] [PubMed]
- Nagaraja Upadhya, P.; Kishore, G. Glass ionomer cement: The different generations. Trends Biomater. Artif. Organs 2005, 18, 158–165. [Google Scholar]
- Ferracane, J.L.; Stansbury, J.W.; Burke, F.J. Self-adhesive resin cements—Chemistry, properties and clinical considerations. J. Oral Rehabil. 2011, 38, 295–314. [Google Scholar] [CrossRef]
- Goulart, M.; Borges Veleda, B.; Damin, D.; Bovi Ambrosano, G.M.; Coelho de Souza, F.H.; Erhardt, M.C.G. Preheated composite resin used as a luting agent for indirect restorations: Effects on bond strength and resin-dentin interfaces. Int. J. Esthet. Dent. 2018, 13, 86–97. [Google Scholar]
- Gupta, A.A.; Mulay, S.; Mahajan, P.; Raj, A.T. Assessing the effect of ceramic additives on the physical, rheological and mechanical properties of conventional glass ionomer luting cement—An in-vitro study. Heliyon 2019, 5, e02094. [Google Scholar] [CrossRef]
- Sita Ramaraju, D.; Alla, R.K.; Alluri, V.R.; Raju, M. A review of conventional and contemporary luting agents used in dentistry. Am. J. Mater. Sci. Eng. 2014, 2, 28–35. [Google Scholar]
- White, S.N.; Yu, Z. Film thickness of new adhesive luting agents. J. Prosthet. Dent. 1992, 67, 782–785. [Google Scholar] [CrossRef]
- International Organization for Standardization. Water-Based Cements—Part 1: Powder/Liquid Acid-Base Cements. 2016. Available online: https://www.iso.org/standard/45818.html (accessed on 30 April 2024).
- International Organization for Standardization. Water-Based Cements—Part 2: Resin-Modified Cements. 2017. Available online: https://www.iso.org/standard/69901.html (accessed on 30 April 2024).
- International Organization for Standardization. Polymer-Based Luting Materials Containing Adhesive Components. 2021. Available online: https://www.iso.org/standard/56898.html (accessed on 30 April 2024).
- Zorzin, J.; Petschelt, A.; Ebert, J.; Lohbauer, U. pH neutralization and influence on mechanical strength in self-adhesive resin luting agents. Dent. Mater. 2012, 28, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Kious, A.R.; Roberts, H.W.; Brackett, W.W. Film thicknesses of recently introduced luting cements. J. Prosthet. Dent. 2009, 101, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Holst, S.; Karl, M.; Wichmann, M.; Matta, R.E. A new triple-scan protocol for 3D fit assessment of dental restorations. Quintessence Int. 2011, 42, 651–657. [Google Scholar] [PubMed]
- Matta, R.E.; Schmitt, J.; Wichmann, M.; Holst, S. Circumferential fit assessment of CAD/CAM single crowns—A pilot investigation on a new virtual analytical protocol. Quintessence Int. 2012, 43, 801–809. [Google Scholar] [PubMed]
- Sakrana, A.A.; Al-Zordk, W.; El-Sebaey, H.; Elsherbini, A.; Özcan, M. Does Preheating Resin Cements Affect Fracture Resistance of Lithium Disilicate and Zirconia Restorations? Materials 2021, 14, 5603. [Google Scholar] [CrossRef] [PubMed]
- Tyor, S.; Al-Zordk, W.; Sakrana, A.A. Fracture resistance of monolithic translucent zirconia crown bonded with different self-adhesive resin cement: Influence of MDP-containing zirconia primer after aging. BMC Oral Health 2023, 23, 636. [Google Scholar] [CrossRef] [PubMed]
- The R Project for Statistical Computing. A Language and Environment for Statistical Computing. 2017. Available online: https://www.r-project.org/ (accessed on 20 January 2023).
- Jørgensen, K.D. Factors affecting the film thickness of zinc phosphate cements. Acta Odontol. Scand. 1960, 18, 479–490. [Google Scholar] [CrossRef]
- Fleming, G.J.; Marquis, P.M.; Shortall, A.C. The influence of clinically induced variability on the distribution of compressive fracture strengths of a hand-mixed zinc phosphate dental cement. Dent. Mater. 1999, 15, 87–97. [Google Scholar] [CrossRef]
- McKenna, J.E.; Ray, N.J.; McKenna, G.; Burke, F.M. The effect of variability in the powder/liquid ratio on the strength of zinc phosphate cement. Int. J. Dent. 2011, 2011, 679315. [Google Scholar] [CrossRef]
- Walton, T.R. The flow properties of zinc phosphate cement: An argument for changing the standard. Aust. Dent. J. 1980, 25, 215–218. [Google Scholar] [CrossRef]
- Kogawa, E.M.; Calderon, P.D.; Lauris, J.R.; Pegoraro, L.F.; Conti, P.C. Evaluation of minimum interdental threshold ability in dentate female temporomandibular disorder patients. J. Oral Rehabil. 2010, 37, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Kern, M.; Schaller, H.G.; Strub, J.R. Marginal fit of restorations before and after cementation in vivo. Int. J. Prosthodont. 1993, 6, 585–591. [Google Scholar] [PubMed]
- Zeller, D.K.; Fischer, J.; Rohr, N. Viscous behavior of resin composite cements. Dent. Mater. J. 2021, 40, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Giannini, M.; Takagaki, T.; Bacelar-Sá, R.; Vermelho, P.M.; Ambrosano, G.M.; Sadr, A.; Nikaido, T.; Tagami, J. Influence of resin coating on bond strength of self-adhesive resin cements to dentin. Dent. Mater. J. 2015, 34, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Lubauer, J.; Belli, R.; Lorey, T.; Max, S.; Lohbauer, U.; Zorzin, J.I. A split-Chevron-Notched-Beam sandwich specimen for fracture toughness testing of bonded interfaces. J. Mech. Behav. Biomed. Mater. 2022, 131, 105236. [Google Scholar] [CrossRef] [PubMed]
- Zorzin, J.; Belli, R.; Wagner, A.; Petschelt, A.; Lohbauer, U. Self-adhesive resin cements: Adhesive performance to indirect restorative ceramics. J. Adhes. Dent. 2014, 16, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Attin, T.; Buchalla, W.; Kielbassa, A.M.; Helwig, E. Curing shrinkage and volumetric changes of resin-modified glass ionomer restorative materials. Dent. Mater. 1995, 11, 359–362. [Google Scholar] [CrossRef]
- Feilzer, A.J.; Kakaboura, A.I.; de Gee, A.J.; Davidson, C.L. The influence of water sorption on the development of setting shrinkage stress in traditional and resin-modified glass ionomer cements. Dent. Mater. 1995, 11, 186–190. [Google Scholar] [CrossRef]


| Luting Material | HOFFMANN’S READY2MIX NORMAL | Ketac Cem Aplicap | RelyX Unicem 2 Automix | GC Fuji-Cem 2 |
|---|---|---|---|---|
| Material type | Zinc phosphate | Glass- ionomer | Self-adhesive resin | Resin-modified glass–ionomer |
| Manufacturer | Hoffmann Dental Manufaktur GmbH, Berlin, Germany | 3M, St. Paul, MN, USA | 3M, St. Paul, MN, USA | GC, Tokyo, Japan |
| Shade | Yellow | Yellow | A2 | Light Yellow |
| Lot number | N.A. | 529059 | 574731 | 141211A |
| Composition | Powder: Zinc oxide, magnesium oxide Liquid: Ortho-phosphoric acid | Powder: Glass powder, pigments Liquid: Water, Acrylic acid/Maleic acid copolymer, tartaric acid, preservative | Base paste: Phosphorylated methacrylate monomers, methacrylate monomers, silanized fillers, initiators, stabilizers, rheology additive Catalyst paste: Methacrylate monomers, basic and silanized fillers, initiators, stabilizers, pigments, rheology additive | Paste A: Fluoroalumino- silicate glass, initiator, UDMA, dimethacrylate, pigments, silicon dioxide, inhibitor Paste B: Silicon dioxide, UDMA, dimethacrylate, initiator, inhibitor |
| Filler particle size | N.A. | ≤12 µm | <9.5 µm | N.A. |
| Film thickness | N.A. | 16 ± 1 µm | 13 µm | N.A. |
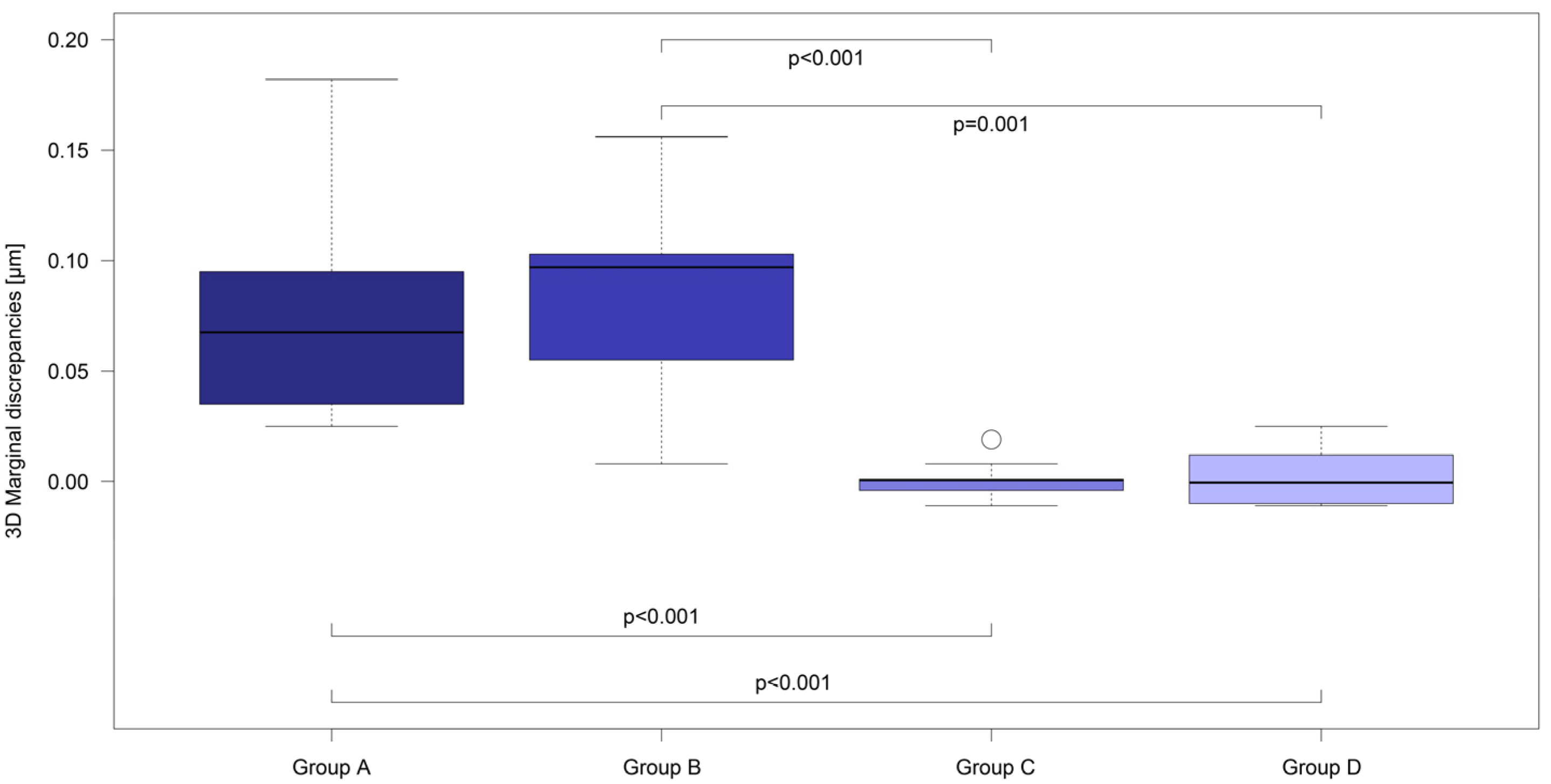
| 3D Analysis of the Marginal Fit (µm) before and after Cementation | ||||||
|---|---|---|---|---|---|---|
| Group | Mean | SD | Min | Max | p-Value | |
| Group A | before cem | 0.033 | 0.004 | 0.028 | 0.038 | 0.002 |
| after cem | 0.110 | 0.049 | 0.059 | 0.210 | ||
| Group B | before cem | 0.035 | 0.005 | 0.031 | 0.043 | 0.002 |
| after cem | 0.118 | 0.048 | 0.039 | 0.188 | ||
| Group C | before cem | 0.042 | 0.005 | 0.035 | 0.053 | 1.0 |
| after cem | 0.042 | 0.007 | 0.033 | 0.058 | ||
| Group D | before cem | 0.038 | 0.003 | 0.035 | 0.042 | 0.722 |
| after cem | 0.040 | 0.012 | 0.027 | 0.067 | ||
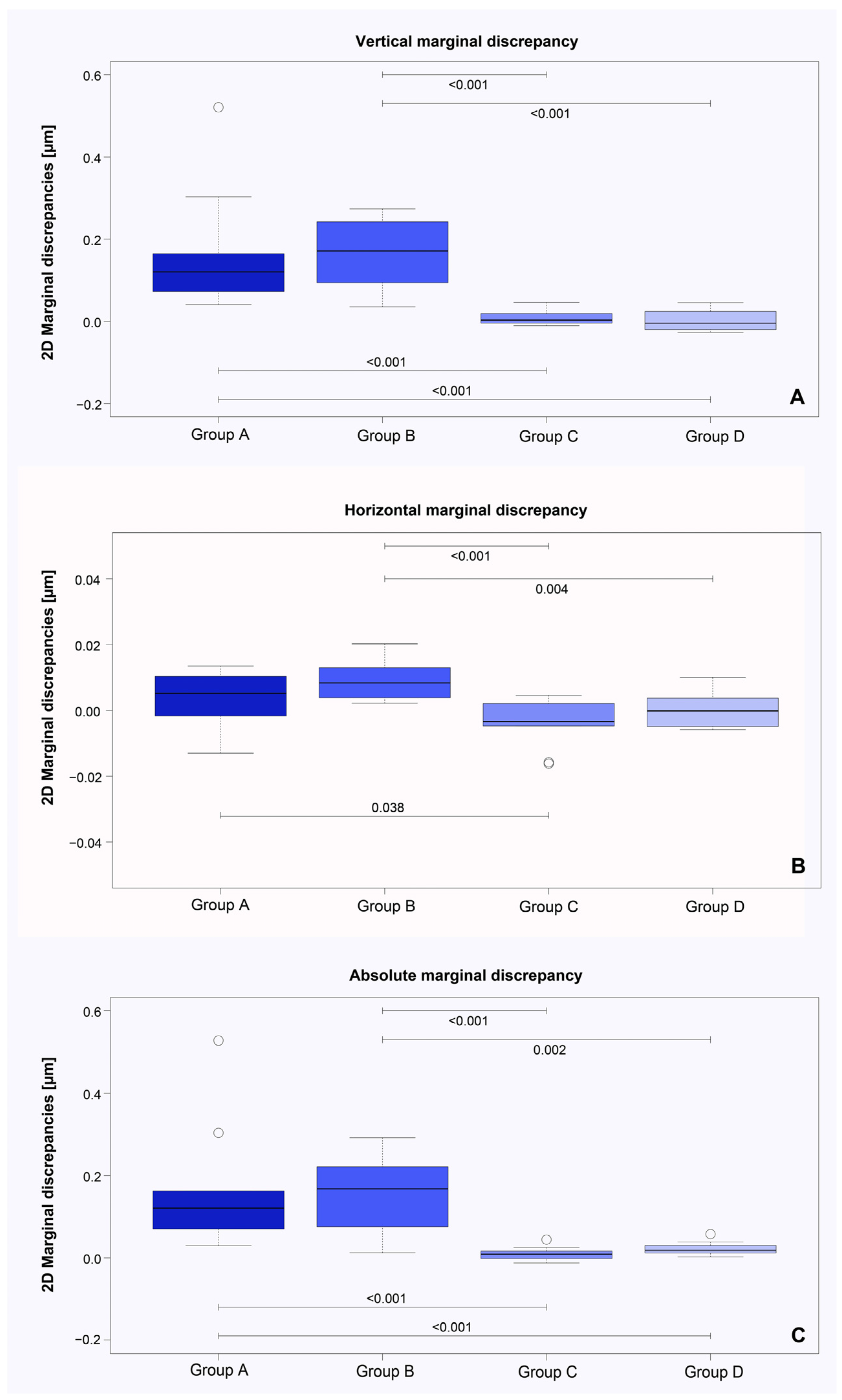
| 2D Analysis of the Marginal Fit (µm) before and after Cementation | |||||||
|---|---|---|---|---|---|---|---|
| Parameter | Group | Mean | SD | Min | Max | p-Value | |
| Vertical marginal discrepancy | A | before cem | 0.030 | 0.015 | −0.002 | 0.052 | 0.002 |
| after cem | 0.193 | 0.146 | 0.051 | 0.551 | |||
| B | before cem | −0.004 | 0.015 | −0.025 | 0.017 | 0.002 | |
| after cem | 0.164 | 0.092 | 0.011 | 0.291 | |||
| C | before cem | 0.018 | 0.007 | 0.008 | 0.031 | 0.322 | |
| after cem | 0.026 | 0.020 | −0.003 | 0.064 | |||
| D | before cem | 0.011 | 0.002 | 0.007 | 0.014 | 0.846 | |
| after cem | 0.013 | 0.025 | −0.014 | 0.057 | |||
| Horizontal marginal discrepancy | A | before cem | −0.021 | 0.014 | −0.049 | 0.002 | 0.232 |
| after cem | −0.017 | 0.019 | −0.046 | 0.015 | |||
| B | before cem | 0.010 | 0.006 | 0.003 | 0.024 | 0.002 | |
| after cem | 0.020 | 0.009 | 0.006 | 0.038 | |||
| C | before cem | 0.018 | 0.005 | 0.009 | 0.026 | 0.126 | |
| after cem | 0.014 | 0.006 | 0.008 | 0.026 | |||
| D | before cem | 0.012 | 0.003 | 0.009 | 0.017 | 0.922 | |
| after cem | 0.013 | 0.006 | 0.006 | 0.023 | |||
| Absolute marginal discrepancy | A | before cem | 0.045 | 0.014 | 0.031 | 0.076 | 0.002 |
| after cem | 0.207 | 0.148 | 0.076 | 0.570 | |||
| B | before cem | 0.031 | 0.005 | 0.026 | 0.042 | 0.002 | |
| after cem | 0.187 | 0.094 | 0.048 | 0.319 | |||
| C | before cem | 0.028 | 0.009 | 0.014 | 0.041 | 0.131 | |
| after cem | 0.037 | 0.016 | 0.021 | 0.070 | |||
| D | before cem | 0.017 | 0.003 | 0.012 | 0.023 | 0.002 | |
| after cem | 0.038 | 0.016 | 0.021 | 0.075 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berger, L.; Matta, R.-E.; Weiß, C.M.; Adler, W.; Wichmann, M.; Zorzin, J.I. Effect of Luting Materials on the Accuracy of Fit of Zirconia Copings: A Non-Destructive Digital Analysis Method. Materials 2024, 17, 2130. https://doi.org/10.3390/ma17092130
Berger L, Matta R-E, Weiß CM, Adler W, Wichmann M, Zorzin JI. Effect of Luting Materials on the Accuracy of Fit of Zirconia Copings: A Non-Destructive Digital Analysis Method. Materials. 2024; 17(9):2130. https://doi.org/10.3390/ma17092130
Chicago/Turabian StyleBerger, Lara, Ragai-Edward Matta, Christian Markus Weiß, Werner Adler, Manfred Wichmann, and José Ignacio Zorzin. 2024. "Effect of Luting Materials on the Accuracy of Fit of Zirconia Copings: A Non-Destructive Digital Analysis Method" Materials 17, no. 9: 2130. https://doi.org/10.3390/ma17092130





