COVID-19: Look to the Future, Learn from the Past
Abstract
:1. Introduction
2. Comparison to SARS-CoV and MERS-CoV
3. Prevention and Control
3.1. A New Perspective
- The total number of patients was small. Therefore, the administration was able to find and quarantine the close contacts of each patient;
- Once becomes onset, the symptoms were obvious, critical and typical. Patients were quickly identified and treated;
- There was no transmission capability during incubation period.
3.2. Vaccines
3.3. Hierarchical Management
3.4. A Long Winter
4. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Cheng, Z.J.; Shan, J. 2019 Novel Coronavirus: Where We are and What We Know. Infection 2020, 48, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
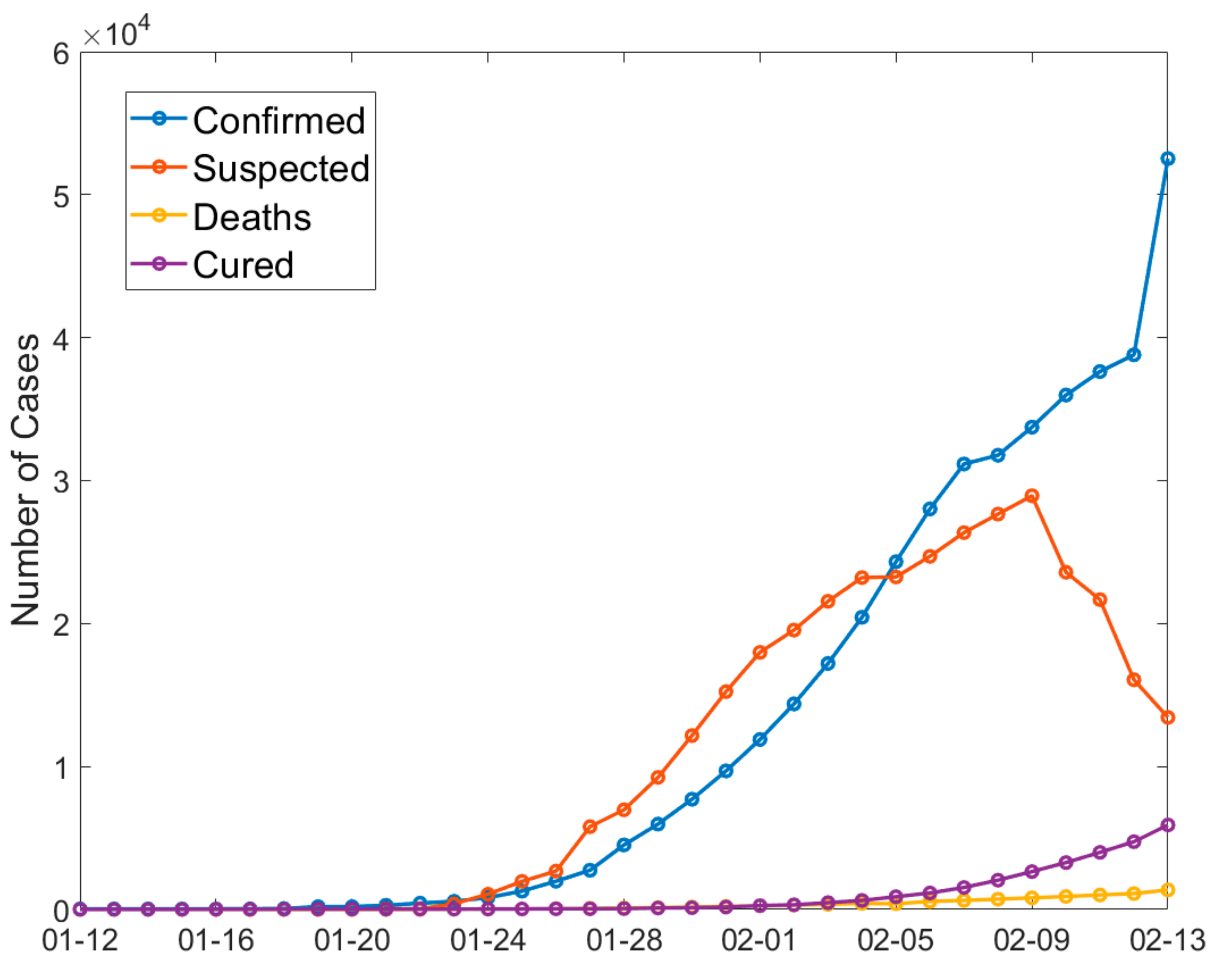
- NHC. Outbreak Notification. 2020. Available online: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml (accessed on 13 February 2020).
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72,314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Su, S.; Wong, G.; Shi, W.; Liu, J.; Lai, A.C.K.; Zhou, J.; Liu, W.; Bi, Y.; Gao, G.F. Epidemiology, Genetic Recombination, and Pathogenesis of Coronaviruses. Trends Microbiol. 2016, 24, 490–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhong, N.S.; Zheng, B.J.; Li, Y.M.; Poon, L.L.M.; Xie, Z.H.; Chan, K.H.; Li, P.H.; Tan, S.Y.; Chang, Q.; Xie, J.P.; et al. Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, People’s Republic of China, in February, 2003. Lancet 2003, 362, 1353–1358. [Google Scholar] [CrossRef] [Green Version]
- Peiris, J.S.; Guan, Y.; Yuen, K.Y. Severe acute respiratory syndrome. Nat. Med. 2004, 10 (Suppl. 12), S88–S97. [Google Scholar] [CrossRef] [PubMed]
- Zaki, A.M.; van Boheemen, S.; Bestebroer, T.M.; Osterhaus, A.D.; Fouchier, R.A. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N. Engl. J. Med. 2012, 367, 1814–1820. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Chowell, G.; Jung, E. A dynamic compartmental model for the Middle East respiratory syndrome outbreak in the Republic of Korea: A retrospective analysis on control interventions and superspreading events. J. Theor. Biol. 2016, 408, 118–126. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.Y.; Kim, Y.J.; Chung, E.H.; Kim, D.W.; Jeong, I.; Kim, Y.; Yun, M.R.; Kim, S.S.; Kim, G.; Joh, J.S. The clinical and virological features of the first imported case causing MERS-CoV outbreak in South Korea, 2015. BMC Infect Dis. 2017, 17, 498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, V.C.C.; Wong, S.C.; To, K.K.W.; Ho, P.L.; Yuen, K.Y. Preparedness and proactive infection control measures against the emerging Wuhan coronavirus pneumonia in China. J. Hosp. Infect. 2020, 104, 254–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- WHO. Summary of Probable SARS Cases with Onset of Illness from 1 November 2002 to 31 July 2003. 2003. Available online: http://www.who.int/csr/sars/country/table2004_04_21/en/index.html (accessed on 7 February 2020).
- WHO. MERS Monthly Report November 2019; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Biscayart, C.; Angeleri, P.; Lloveras, S.; Chaves, T.D.; Schlagenhauf, P.; Rodríguez-Morales, A.J. The next big threat to global health? 2019 novel coronavirus (2019-nCoV): What advice can we give to travellers?—Interim recommendations January 2020, from the Latin-American society for Travel Medicine (SLAMVI). Travel Med. Infect. Dis. 2020, 33, 101567. [Google Scholar] [CrossRef] [PubMed]
- Xinhua. China’s CDC Detects a Large Number of New Coronaviruses in the South China Seafood Market in Wuhan. 2020. Available online: http://www.xinhuanet.com/2020-01/27/c_1125504355.htm (accessed on 7 February 2020).
- Cohen, J. Wuhan seafood market may not be source of novel virus spreading globally. Science 2020. [Google Scholar] [CrossRef]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. Discovery of a novel coronavirus associated with the recent pneumonia outbreak in humans and its potential bat origin. bioRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Guo, Q.; Li, M.; Wang, C.; Wang, P.; Fang, Z.; Tan, J.; Wu, S.; Xiao, Y. Host and infectivity prediction of Wuhan 2019 novel coronavirus using deep learning algorithm. bioRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Kan, B.; Wang, M.; Jing, H.; Xu, H.; Jiang, X.; Yan, M.; Liang, W.; Zheng, H.; Wan, K.; Liu, Q.; et al. Molecular evolution analysis and geographic investigation of severe acute respiratory syndrome coronavirus-like virus in palm civets at an animal market and on farms. J. Virol. 2005, 79, 11892–11900. [Google Scholar] [CrossRef] [Green Version]
- Sabir, J.S.; Lam, T.T.; Ahmed, M.M.; Li, L.; Shen, Y.; Abo-Aba, S.E.; Qureshi, M.I.; Abu-Zeid, M.; Zhang, Y.; Khiyami, M.A.; et al. Co-circulation of three camel coronavirus species and recombination of MERS-CoVs in Saudi Arabia. Science 2016, 351, 81–84. [Google Scholar] [CrossRef] [Green Version]
- Cyranoski, D. Mystery deepens over animal source of coronavirus. Nature 2020, 579, 18–19. [Google Scholar] [CrossRef] [Green Version]
- Lam, T.T.; Jia, N.; Zhang, Y.W.; Shum, M.H.; Jiang, J.F.; Zhu, H.C.; Tong, Y.G.; Shi, Y.X.; Ni, X.B.; Liao, Y.S.; et al. Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature 2020, 583, 282–285. [Google Scholar] [CrossRef] [Green Version]
- Ji, W.; Wang, W.; Zhao, X.; Zai, J.; Li, X. Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross-species transmission from snake to human. J. Med. Virol. 2020, 92, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Frutos, R.; Serra-Cobo, J.; Chen, T.; Devaux, C.A. COVID-19: Time to exonerate the pangolin from the transmission of SARS-CoV-2 to humans. Infect. Genet. Evol. 2020, 84, 104493. [Google Scholar] [CrossRef]
- Perlman, S. Another Decade, Another Coronavirus. N. Engl. J. Med. 2020, 382, 760–762. [Google Scholar] [CrossRef]
- WHO. Novel Coronavirus (2019-nCoV) Situation Report; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Wu, J.T.; Leung, K.; Leung, G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling study. Lancet 2020, 395, 689–697. [Google Scholar] [CrossRef] [Green Version]
- WHO. Consensus Document on the Epidemiology of Severe Acute Respiratory Syndrome (SARS); WHO: Geneva, Switzerland, 2003. [Google Scholar]
- WHO. WHO MERS Global Summary and Assessment of Risk; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Liu, Y.; Qu, H.-Q.; Qu, J.; Tian, L.; Hakonarson, H. Expression Pattern of the SARS-CoV-2 Entry Genes ACE2 and TMPRSS2 in the Respiratory Tract. Viruses 2020, 12, 1174. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.-Q.; Sun, B.-Q.; Fang, Z.-F.; Zhao, J.-C.; Liu, X.-Y.; Li, Y.-M.; Sun, X.-Z.; Liang, H.-F.; Zhong, B.; Huang, Z.-F.; et al. Distinct features of SARS-CoV-2-specific IgA response in COVID-19 patients. Eur. Respir. J. 2020. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Yao, L.; Wei, T.; Tian, F.; Jin, D.-Y.; Chen, L.; Wang, M. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020, 323, 1406–1407. [Google Scholar] [CrossRef] [Green Version]
- Mizumoto, K.; Kagaya, K.; Zarebski, A.; Chowell, G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Eurosurveillance 2020, 25, 2000180. [Google Scholar] [CrossRef] [Green Version]
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 7798. [Google Scholar] [CrossRef] [Green Version]
- Qin, J.; You, C.; Lin, Q.; Hu, T.; Yu, S.; Zhou, X.-H. Estimation of incubation period distribution of COVID-19 using disease onset forward time: A novel cross-sectional and forward follow-up study. medRxiv 2020. [Google Scholar] [CrossRef]
- Rothe, C.; Schunk, M.; Sothmann, P.; Bretzel, G.; Froeschl, G.; Wallrauch, C.; Zimmer, T.; Thiel, V.; Janke, C.; Guggemos, W.; et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N. Engl. J. Med. 2020, 382, 970–971. [Google Scholar] [CrossRef] [Green Version]
- Kupferschmidt, K. Study claiming new coronavirus can be transmitted by people without symptoms was flawed. Science 2020. [Google Scholar] [CrossRef]
- About the Present Situation of New Type Coronavirus Infectious Disease and Correspondence of Ministry of Health, Labor and Welfare (February 7 Version). Ministry of Health, Labor and Welfare, 2020. Available online: https://www.mhlw.go.jp/stf/newpage_09396.html (accessed on 7 February 2020).
- The Second Batch of Wuhan Evacuees All Tested Negative and One Was Confirmed Infected in the First Batch. KBS, 2020. Available online: http://world.kbs.co.kr/service/news_view.htm?lang=c&Seq_Code=66621 (accessed on 7 February 2020).
- Routine New Headquarters of the Central Accident Management Division of New Coronavirus Infection 2020-02-01. Ministry of Health and Welfare, 2020. Available online: https://www.mohw.go.kr/eng/nw/nw0101vw.jsp?PAR_MENU_ID=1007&MENU_ID=100701&page=1&CONT_SEQ=352718 (accessed on 7 February 2020).
- New Outbreaks of Corona Virus in Korea. Ministry of Health and Welfare, 2020. Available online: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=3&CONT_SEQ=352645 (accessed on 7 February 2020).
- Waldrop, T.; Yan, H. The 1st Group of Americans Evacuated from Wuhan and Quarantined over Coronavirus just Got Released. CNN, 2020. Available online: https://edition.cnn.com/2020/02/10/us/coronavirus-american-evacuees-release/index.html (accessed on 7 February 2020).
- Coronavirus: German Evacuation Flight from China Carried Two Infected People. DW. 2020. Available online: https://www.dw.com/en/coronavirus-german-evacuation-flight-from-china-carried-two-infected-people/a-52229955 (accessed on 7 February 2020).
- AFP. Coronavirus: Countries Evacuate Citizens from China. New Straits Times, 2020. Available online: https://www.nst.com.my/world/world/2020/01/561086/coronavirus-countries-evacuate-citizens-china (accessed on 7 February 2020).
- Wei, T.T. Some Singaporeans with Symptoms of Virus Staying behind in Wuhan even as 92 Are Evacuated. The Straits Times. 2020. Available online: https://www.straitstimes.com/singapore/some-singaporeans-with-symptoms-of-virus-staying-behind-in-wuhan-even-as-92-are-evacuated (accessed on 7 February 2020).
- Yong, C. Coronavirus: 2 New Cases in S’pore, Including Certis Officer Who Had Served Quarantine Orders on 2 Who Tested Positive. The Straits Times. 2020. Available online: https://www.straitstimes.com/singapore/coronavirus-2-new-cases-in-singapore-including-certis-cisco-staff-who-had-served (accessed on 7 February 2020).
- Seckin, B. Italy Reports Third Confirmed Case of Coronavirus. AA. 2020. Available online: https://www.aa.com.tr/en/europe/italy-reports-third-confirmed-case-of-coronavirus/1726934 (accessed on 7 February 2020).
- Network, C.N. Health Committee Responds to 5 Million People Leaving Wuhan: Our Common Enemy Is Disease, not Wuhan. Sina News. 2020. Available online: https://news.sina.com.cn/c/2020-01-29/doc-iihnzhha5261128.shtml (accessed on 7 February 2020).
- Farzanegan, M.R.; Feizi, M.; Gholipour, H.F. Globalization and Outbreak of COVID-19: An Empirical Analysis; Philipps-Universität Marburg, Faculty of Business Administration and Economics in Germany: Marburg, Germany, 2020. [Google Scholar]
- Chan, J.F.; Yuan, S.; Kok, K.H.; To, K.K.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.; Poon, R.W.; et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef] [Green Version]
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- Taubenberger, J.K.; Morens, D.M. 1918 Influenza: The mother of all pandemics. Emerg. Infect. Dis. 2006, 12, 15–22. [Google Scholar] [CrossRef]
- Biggerstaff, M.; Cauchemez, S.; Reed, C.; Gambhir, M.; Finelli, L. Estimates of the reproduction number for seasonal, pandemic, and zoonotic influenza: A systematic review of the literature. BMC Infect. Dis. 2014, 14, 480. [Google Scholar] [CrossRef] [Green Version]
- Harper, S.A.; Fukuda, K.; Uyeki, T.M.; Cox, N.J.; Bridges, C.B. Prevention and Control of Influenza Recommendations of the Advisory Committee on Immunization Practices (ACIP). Morb. Mortal. Wkly. Rep. Recomm. Rep. 2005, 54, 1–41. [Google Scholar]
- Pan, H.; Peto, R.; Abdool Karim, Q.; Alejandria, M.; Henao Restrepo, A.M.; Hernandez Garcia, C.; Kieny, M.P.; Malekzadeh, R.; Murthy, S.; Preziosi, M.-P.; et al. Repurposed antiviral drugs for COVID-19; interim WHO SOLIDARITY trial results. medRxiv 2020. [Google Scholar] [CrossRef]
- Litvinova, M.; Liu, Q.H.; Kulikov, E.S.; Ajelli, M. Reactive school closure weakens the network of social interactions and reduces the spread of influenza. Proc. Natl. Acad. Sci. USA 2019, 116, 13174–13181. [Google Scholar] [CrossRef] [Green Version]
- Moghadas, S.M.; Haworth-Brockman, M.; Isfeld-Kiely, H.; Kettner, J. Improving public health policy through infection transmission modelling: Guidelines for creating a Community of Practice. Can. J. Infect. Dis. Med. Microbiol. 2015, 26, 191–195. [Google Scholar] [CrossRef]
- Bootsma, M.C.; Ferguson, N.M. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc. Natl. Acad. Sci. USA 2007, 104, 7588–7593. [Google Scholar] [CrossRef] [Green Version]
- Gunaratnam, P.J.; Tobin, S.; Seale, H.; Marich, A.; McAnulty, J. Airport arrivals screening during pandemic (H1N1) 2009 influenza in New South Wales, Australia. Med. J. Aust. 2014, 200, 290–292. [Google Scholar] [CrossRef] [Green Version]
- Nishiura, H.; Kamiya, K. Fever screening during the influenza (H1N1-2009) pandemic at Narita International Airport, Japan. BMC Infect. Dis. 2011, 11, 111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC. CDC Seasonal Flu Vaccine Effectiveness Studies; CDC: Atlanta, GA, USA, 2019. [Google Scholar]
- Plotkin, S.; Robinson, J.M.; Cunningham, G.; Iqbal, R.; Larsen, S. The complexity and cost of vaccine manufacturing—An overview. Vaccine 2017, 35, 4064–4071. [Google Scholar] [CrossRef]
- Pong, W. A Dozen Vaccine Programs under Way as WHO Declares Coronavirus Public Health Emergency. Biocentry, 2020. Available online: https://www.biocentury.com/article/304328/a-dozen-vaccine-programs-under-way-as-who-declares-coronavirus-public-health-emergency (accessed on 7 February 2020).
- Corum, J.; Wee, S.; Zimmer, C. Coronavirus Vaccine Tracker. 2020. Available online: https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html (accessed on 16 October 2020).
- Dong, Y.; Dai, T.; Wei, Y.; Zhang, L.; Zheng, M.; Zhou, F. A systematic review of SARS-CoV-2 vaccine candidates. Signal Transduct. Target Ther. 2020, 5, 237. [Google Scholar] [CrossRef]
- Feng, E.; Cheng, A. In Quarantined Wuhan, Hospital Beds For Coronavirus Patients Are Scarce. NPR 2020. [Google Scholar]
- Pickrell, R. Wuhan is scrambling to fill 11 sports centres, exhibition halls, and other local venues with over 10,000 beds to create makeshift coronavirus hospitals. Bus. Insider 2020. [Google Scholar]
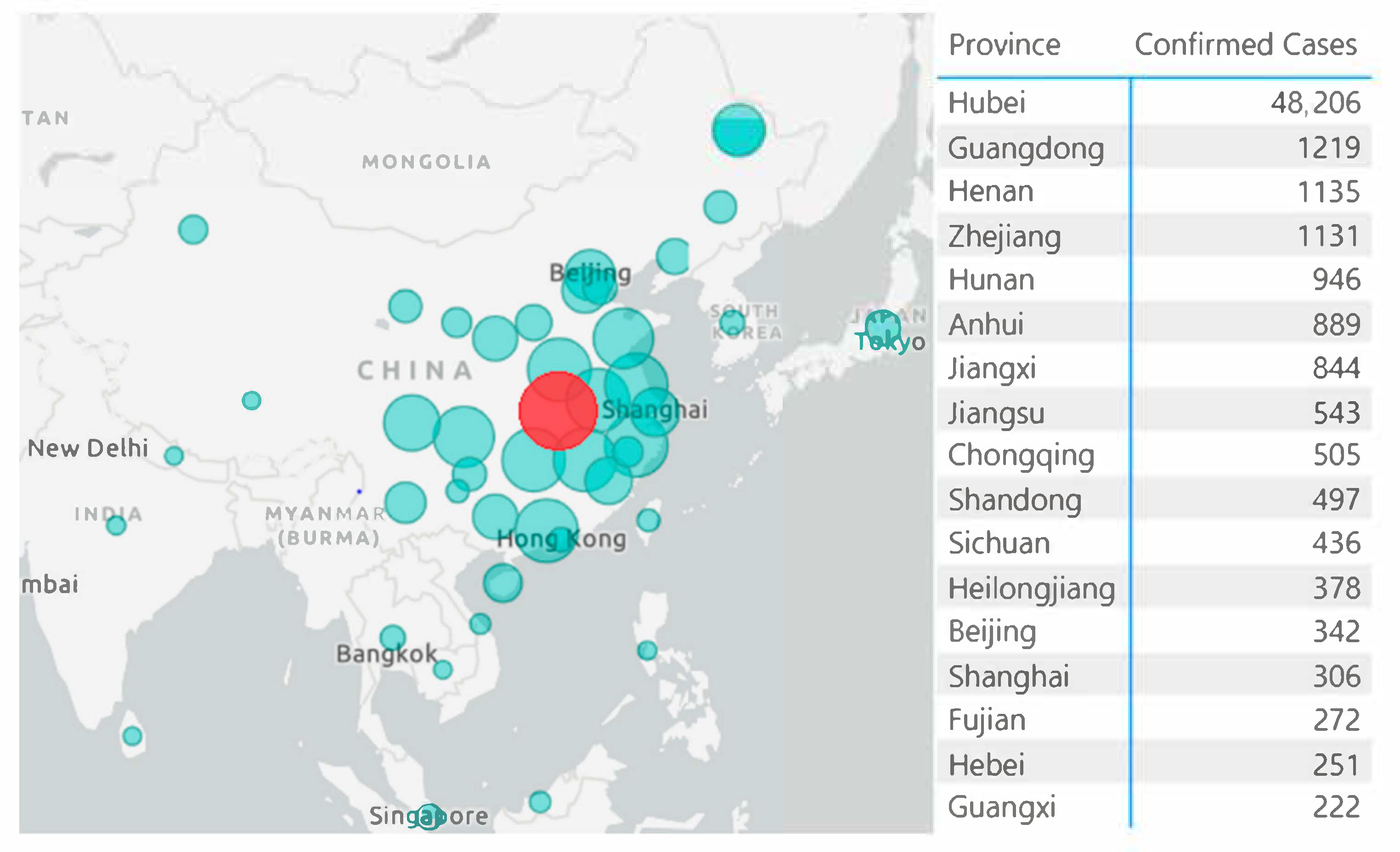
- DXY. Epidemic Map. 2020. Available online: https://3g.dxy.cn/newh5/view/pneumonia?from=timeline&isappinstalled=0 (accessed on 13 February 2020).
- Kwok, K.O.; Lai, F.; Wei, W.I.; Wong, S.Y.S.; Tang, J.W. Herd immunity–estimating the level required to halt the COVID-19 epidemics in affected countries. J. Infect. 2020, 80, e32–e33. [Google Scholar] [CrossRef]
- Korber, B.; Fischer, W.; Gnanakaran, S.; Yoon, H.; Theiler, J.; Abfalterer, W.; Foley, B.; Giorgi, E.; Bhattacharya, T.; Parker, M.; et al. Spike mutation pipeline reveals the emergence of a more transmissible form of SARS-CoV-2. bioRxiv 2020. [Google Scholar] [CrossRef]
- Vergano, D. Don’t Worry About The Coronavirus. Worry About The Flu. Buzzfeed News. 2020. Available online: https://www.buzzfeednews.com/article/danvergano/coronavirus-cases-deaths-flu?bftwnews&utm_term=4ldqpgc#4ldqpgc (accessed on 7 February 2020).
- The Lancet. Emerging understandings of 2019-nCoV. Lancet 2020, 395, 311. [Google Scholar] [CrossRef] [Green Version]
- Ioannidis, J. The infection fatality rate of COVID-19 inferred from seroprevalence data. medRxiv 2020. [Google Scholar] [CrossRef]
| Country | Evacuated | Confirmed Cases | Prevalence | Converted to Infected Population in Wuhan | Source |
|---|---|---|---|---|---|
| Japan | 566 | 9 | 1.4% | 156,000 | [40] |
| South Korea | 368 | 1 | 0.3% | 30,000 | [41,42,43] |
| US | 195 | 0 | 0 | 0 | [44] |
| Germany | 124 | 2 | 1.6% | 177,000 | [45] |
| Singapore | 92 | 1 | 1.1% | 119,000 | [46,47,48] |
| Italy | 56 | 1 | 1.8% | 196,000 | [49] |
| Total | 1401 | 14 | 1.0% | 110,000 | NA |
| Characteristics | SARS-CoV-2 | SARS-CoV | MERS-CoV | Influenza |
|---|---|---|---|---|
| R0 | 2.68 | 3 | <1 | 1.3 |
| Virulence | Low | High | High | Low |
| Case Fatality Rate | 2% | 10% | 37% | 0.1% |
| Natural Hosts | Bat | Bat | Bat | Animals, humans |
| Intermediate Hosts | Unknown | Civets | Camels | NA |
| Origin of Outbreak | Wuhan, China | Guangzhou, China | Saudi Arabia | NA |
| Incubation Period | 2–16 days | 2–7 days | 4–8 days | 1–4 days |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, Z.J.; Qu, H.-Q.; Tian, L.; Duan, Z.; Hakonarson, H. COVID-19: Look to the Future, Learn from the Past. Viruses 2020, 12, 1226. https://doi.org/10.3390/v12111226
Cheng ZJ, Qu H-Q, Tian L, Duan Z, Hakonarson H. COVID-19: Look to the Future, Learn from the Past. Viruses. 2020; 12(11):1226. https://doi.org/10.3390/v12111226
Chicago/Turabian StyleCheng, Zhangkai J., Hui-Qi Qu, Lifeng Tian, Zhifeng Duan, and Hakon Hakonarson. 2020. "COVID-19: Look to the Future, Learn from the Past" Viruses 12, no. 11: 1226. https://doi.org/10.3390/v12111226






