Dietary Behavior and Risk of Orthorexia in Women with Celiac Disease
Abstract
:1. Introduction
2. Materials and Methods
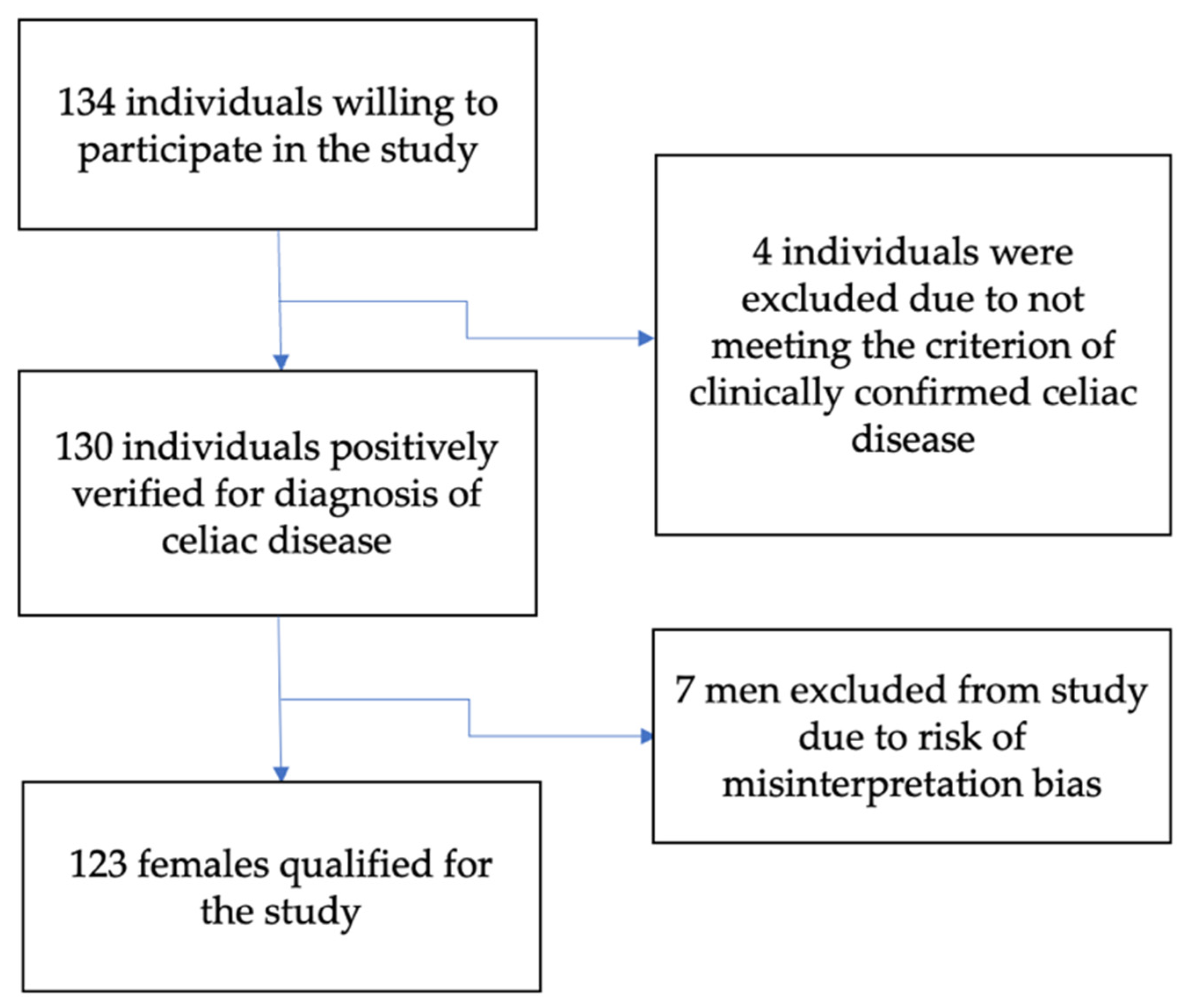
2.1. Study Group
2.2. Eating Habits and Physical Activity
2.3. Questionnaire ORTO-15
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Study Participants
3.2. Reliability Assessment of the ORTO-15 Questionnaire
3.3. Prevalence of Orthorexia in Celiac Participants
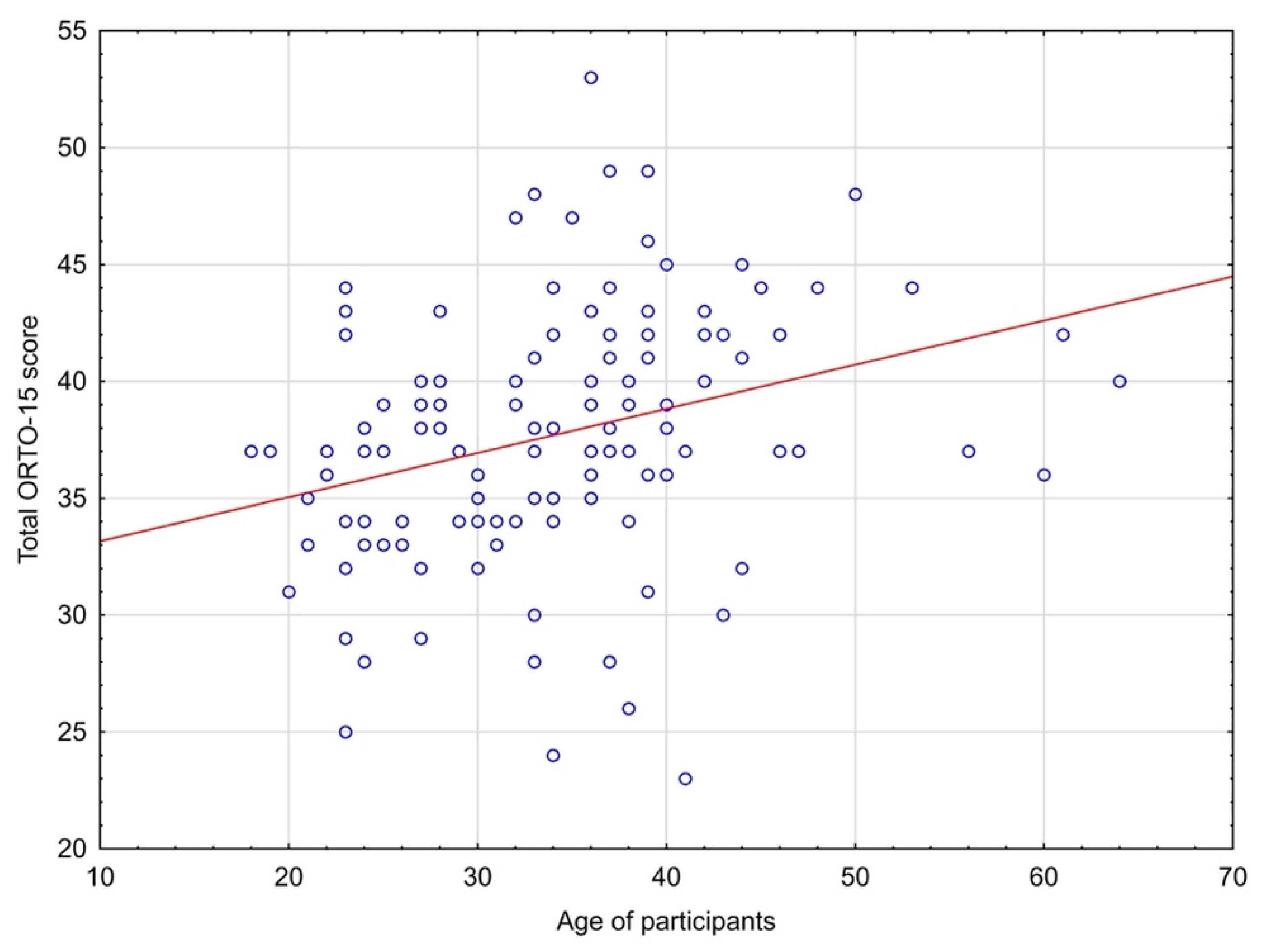
3.4. The Relationship between the Age of Study Participants and the ORTO-15 Questionnaire Total Score
3.5. Eating Habits and Behaviors and the Incidence of Orthorexia Risk
3.6. Differences between the Risk Group of Orthorexia and Non-Risk Participants in ORTO-15 Questionnaire
3.7. Self-Assessed Impact of Celiac Disease on Diet
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Husby, S.; Koletzko, S.; Korponay-Szabo, R.; Mearin, M.L.; Phillips, A.; Shamir, R.; Troncone, R.; Giersiepen, K.; Branski, D.; Catassi, C.; et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition Guidelines for the Diagnosis of Coeliac Disease. J. Pediatric Gastroenterol. Nutr. 2012, 54, 136–160. [Google Scholar] [CrossRef] [PubMed]
- Greetje, J.T.; Wieke, H.M.; Verbeek Marco, W.J.; Schreurs and Chris, J.J.M. The Spectrum of Celiac Disease: Epidemiology, Clinical Aspects and Treatment. Nat. Rev. Gastroenterol. Hepatol. 2010, 7, 204–213. [Google Scholar] [CrossRef]
- Pinkhasov, R.M.; Wong, J.; Kashanian, J.; Lee, M.; Samadi, D.B.; Pinkhasov, M.M.; Shabsigh, R. Are men shortchanged on health? Perspective on health care utilization and health risk behavior in men and women in the United States. Int. J. Clin. Pract. 2010, 64, 475–487. [Google Scholar] [CrossRef] [PubMed]
- Schappert, S.M.; Burt, C.W. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001–2002. Vital Health Stat. 2006, 13, 1–66. [Google Scholar]
- Zingone, F.; Swift, G.L.; Card, T.R.; Sanders, D.S.; Ludvigsson, J.F.; Bai, J.C. Psychological morbidity of celiac disease: A review of the literature. United Eur. Gastroenterol. J. 2015, 3, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Itzlinger, A.; Federica, B.; Luca, E.; Michael, S. Gluten-Free Diet in Celiac Disease—Forever and for All? Nutrients 2018, 10, 1796. [Google Scholar] [CrossRef] [Green Version]
- Carley, N.F.; Stephan, P.M.; Simon, R.K. Understanding disease-specific and non-specific factors predicting disordered eating in adults with coeliac disease. Appetite 2022, 168, 105744. [Google Scholar] [CrossRef]
- Saddichha, S.; Babu, G.N.; Chandra, P. Orthorexia nervosa presenting as prodrome of schizophrenia. Schizophr. Res. 2012, 134, 110. [Google Scholar] [CrossRef]
- Varga, M.; Dukay-Szabó, S.; Túry, F.; van Furth, E.F. Evidence and gaps in the literature on orthorexia nervosa. Eat. Weight Disord. 2013, 18, 103–111. [Google Scholar] [CrossRef]
- Niedzielski, A.; Kazmierczak-Wojta’s, N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools—A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 5488. [Google Scholar] [CrossRef]
- Strahler, J. Sex differences in orthorexic eating behaviors: A systematic review and meta-analytical integration. Nutrition 2019, 67–68, 110534. [Google Scholar] [CrossRef] [PubMed]
- Ramacciotti, C.E.; Perrone, E.; Coli, E.; Burgalassi, A.; Conversano, C.; Massimetti, G.; Dell’Osso, L. Orthorexia nervosa in the general population: A preliminary screening using a self-administered questionnaire (ORTO-15). Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2011, 16, 127–130. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- Brytek-Matera, A.; Onieva-Zafra, M.D.; Parra-Fernández, M.L.; Staniszewska, A.; Modrzejewska, J.; Fernández-Martínez, E. Evaluation of Orthorexia Nervosa and Symptomatology Associated with Eating Disorders among European University Students: A Multicentre Cross-Sectional Study. Nutrients 2020, 12, 3716. [Google Scholar] [CrossRef] [PubMed]
- Dunn, T.M.; Bratman, S. On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eat. Behav. 2016, 21, 11–17. [Google Scholar] [CrossRef]
- Moroze, R.M.; Dunn, T.M.; Holland, C.J.; Yager, J.; Weintraub, P. Microthinking about micronutrients: A case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics 2015, 56, 397–403. [Google Scholar] [CrossRef]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Canella, C. Orthorexia nervosa: Validation of a diagnosis questionnaire. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2005, 10, 28–32. [Google Scholar] [CrossRef]
- Brytek-Matera, A. Orthorexia nervosa—An eating disorder, obsessive-compulsive disorder or disturbed eating habit? Arch. Psychiatry Psychother. 2012, 14, 55–60. [Google Scholar]
- Kiss-Leizer, M.; Tóth-Király, I.; Rigó, A. How the obsession to eat healthy food meets with the willingness to do sports: The motivational background of orthorexia nervosa. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2019, 24, 465–472. [Google Scholar] [CrossRef] [Green Version]
- Segura-Garcia, C.; Ramacciotti, C.; Rania, M.; Aloi, M.; Caroleo, M.; Bruni, A.; Gazzarrini, D.; Sinopoli, F.; De Fazio, P. The prevalence of orthorexia nervosa among eating disorder patients after treatment. Eat. Weight Disorder. 2015, 20, 161–166. [Google Scholar] [CrossRef]
- Whitaker, J.K.H.; West, J.; Holmes, G.K.T.; Logan, R.F.A. Patient perceptions of the burden of coeliac disease and its treatment in the UK. Aliment. Pharmacol. Ther. 2009, 29, 1131–1136. [Google Scholar] [CrossRef]
- Toni, G.; Berioli, M.G.; Cerquiglini, L.; Ceccarini, G.; Grohmann, U.; Principi, N.; Esposito, S. Eating Disorders and Disordered Eating Symptoms in Adolescents with Type 1 Diabetes. Nutrients 2017, 9, 906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grammatikopoulou, M.G.; Gkiouras, K.; Polychronidou, G.; Kaparounaki, C.; Gkouskou, K.K.; Magkos, F.; Donini, L.M.; Eliopoulos, A.G.; Goulis, D.G. Obsessed with Healthy Eating: A Systematic Review of Observational Studies Assessing Orthorexia Nervosa in Patients with Diabetes Mellitus. Nutrients 2021, 13, 3823. [Google Scholar] [CrossRef] [PubMed]
- Passananti, V.; Siniscalchi, M.; Zingone, F.; Bucci, C.; Tortora, R.; Iovino, P.; Ciacci, C. Prevalence of eating disorders in adults with celiac disease. Gastroenterol. Res. Pract. 2013, 491657. [Google Scholar] [CrossRef] [Green Version]
- Barthels, F.; Barrada, J.R.; Roncero, M. Orthorexia nervosa and healthy orthorexia as new eating styles. PLoS ONE 2019, 14, e0219609. [Google Scholar] [CrossRef] [Green Version]
- Cartwright, M.M. Eating disorder emergencies: Understanding the medical complexities of the hospitalized eating disordered patient. Crit. Care Nurs. Clin. N. Am. 2004, 16, 515–530. [Google Scholar] [CrossRef]
- Lebwohl, B.; Sanders, D.S.; Green, P.H.R. Coeliac disease. Lancet 2018, 391, 70–81. [Google Scholar] [CrossRef]
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Aguilar-Salinas, C.A. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- Stochel, M.; Janas-Kozik, M.; Zejda, J.E.; Hyrnik, J.; Jelonek, I.; Siwiec, A. Validation of ORTO-15 Questionnaire in the group of urban youth aged 15–21. Psychiatr. Pol. 2015, 49, 119–134. [Google Scholar] [CrossRef]
- Brytek-Matera, A.; Krupa, M.; Poggiogalle, E.; Donini, L.M. Adaptation of the ORTHO-15 test to Polish women and men. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2014, 19, 69–76. [Google Scholar] [CrossRef]
- Nunnaly, J.C.; Bernstein, I.H. Psychometric Theory; Mc-Graw-Hill: New York, NY, USA, 1994; Volume 19, Chapter 3; pp. 303–305. [Google Scholar] [CrossRef]
- Bowling, A. Research Methods in Health: Investigating Health and Health Services; McGraw-Hill: New York, NY, USA, 2014; pp. 50–200. Available online: https://edisciplinas.usp.br/pluginfile.php/4374657/mod_resource/content/1/Research%20Methods%20in%20Health.pdf (accessed on 18 November 2021).
- Mitrofanova, E.; Pummell, E.; Martinelli, L.; Petróczi, A. Does ORTO-15 produce valid data for ‘Orthorexia Nervosa’? A mixed-method examination of participants’ interpretations of the fifteen test items. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2021, 26, 897–909. [Google Scholar] [CrossRef]
- Hallit, S.; Brytek-Matera, A.; Obeid, S. Orthorexia nervosa and disordered eating attitudes among Lebanese adults: Assessing psychometric proprieties of the ORTO-R in a population-based sample. PLoS ONE 2021, 16, e0254948. [Google Scholar] [CrossRef]
- Satherley, R.M.; Howard, R.; Higgs, S. The prevalence and predictors of disordered eating in women with coeliac disease. Appetite 2016, 107, 260–267. [Google Scholar] [CrossRef]
- Brytek-Matera, A. The Polish version of the Düsseldorf Orthorexia Scale (PL-DOS) and its comparison with the English version of the DOS (E-DOS). Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2021, 26, 1223–1232. [Google Scholar] [CrossRef] [PubMed]
- Brytek-Matera, A.; Sacre, H.; Staniszewska, A.; Hallit, S. The Prevalence of Orthorexia Nervosa in Polish and Lebanese Adults and Its Relationship with Sociodemographic Variables and BMI Ranges: A Cross-Cultural Perspective. Nutrients 2020, 12, 3865. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, M.A.; Al Hourani, H.M.; Alkhatib, B. Prevalence of orthorexia nervosa among nutrition students and nutritionists: Pilot study. Clin. Nutr. ESPEN 2020, 40, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Dunn, T.M.; Gibbs, J.; Whitney, N.; Starosta, A. Prevalence of orthorexia nervosa is less than 1 %: Data from a US sample. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2017, 22, 85–192. [Google Scholar] [CrossRef]
- Fidan, T.; Ertekin, V.; Isikay, S.; Kirpinar, I. Prevalence of orthorexia among medical students in Erzurum, Turkey. Compr. Psychiatry 2010, 51, 49–54. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Abelli, M.; Carpita, B.; Massimetti, G.; Pini, S.; Rivetti, L.; Gorassi, F.; Tognetti, R.; Ricca, V.; Carmassi, C. Orthorexia nervosa in a sample of Italian university population. Riv. Psichiatr. 2016, 51, 190–196. [Google Scholar] [CrossRef]
- Bongiovanni, T.R.; Ann, L.C.; Elizabeth, A.G.; Janet, M.W.; Melvin, B.H. Impact of gluten-free camp quality of life of children and adolescents with celiac disease. Pediatrics 2010, 125, 525–529. [Google Scholar] [CrossRef] [Green Version]
- West, J.; Fleming, K.M.; Tata, L.J.; Thimothy, R.C.; Colin, J.C. Incidence and prevalence of celiac disease and dermatitis herpetiformis in the UK over two decades: Population-based study. Am. J. Gastroenterol. 2014, 109, 757–768. [Google Scholar] [CrossRef] [Green Version]
- Zickgraf, H.F.; Barrada, J.R. Orthorexia nervosa vs. healthy orthorexia: Relationships with disordered eating, eating behavior, and healthy lifestyle choices [published online ahead of print, 2021 Jul 17]. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2021, 7, 1–13. [Google Scholar] [CrossRef]
- Al Sarkhy, A. Social media usage pattern and its influencing factors among celiac patients and their families. Saudi J. Gastroenterol. 2020, 26, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Sharp, P.; Bottorff, J.L.; Hunt, K.; Oliffe, J.L.; Johnson, S.T.; Dudley, L.; Caperchione, C.M. Men’s Perspectives of a Gender-Sensitized Health Promotion Program Targeting Healthy Eating, Active Living, and Social Connectedness. Am. J. Men’s Health 2018, 2157–2166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galdas, P.M.; Cheater, F.; Marshall, P. Men and health help-seeking behaviour: Literature review. J. Adv. Nurs. 2005, 49, 616–623. [Google Scholar] [CrossRef]
- Ciacci, C.; Cirillo, M.; Sollazzo, R.; Savino, G.; Sabbatini, F.; Mazzacca, G. Gender and clinical presentation in adult celiac disease. Scand J. Gastroenterol. 1995, 30, 1077–1081. [Google Scholar] [CrossRef]
- Lima, R.F.; Maria da Silva Kotze, L.; Kotze, L.R.; Chrisostomo, K.R.; Nisihara, R. Gender-Related Differences in Celiac Patients at Diagnosis. Arch. Med. Res. 2019, 50, 437–441. [Google Scholar] [CrossRef]
- Comino, I.; Fernández-Bañares, F.; Esteve, M.; Ortigosa, L.; Castillejo, G.; Fambuena, B.; Ribes-Koninckx, C.; Sierra, C.; Rodríguez-Herrera, A.; Salazar, J.C.; et al. Fecal Gluten Peptides Reveal Limitations of Serological Tests and Food Questionnaires for Monitoring Gluten-Free Diet in Celiac Disease Patients. Am. J. Gastroenterol. 2016, 111, 1456–1465, Erratum in Am. J. Gastroenterol. 2017, 112, 1208. [Google Scholar] [CrossRef] [Green Version]
- Black, J.L.; Orfila, C. Impact of coeliac disease on dietary habits and quality of life. J. Hum. Nutr. Diet. 2011, 24, 582–587. [Google Scholar] [CrossRef]
- Satherley, R.M.; Higgs, S.; Howard, R. Disordered eating patterns in coeliac disease: A framework analysis. J. Hum. Nutr. Diet. 2017, 30, 724–736. [Google Scholar] [CrossRef]
- Zysk, W.; Głąbska, D.; Guzek, D. Food Neophobia in Celiac Disease and Other Gluten-Free Diet Individuals. Nutrients 2019, 11, 1762. [Google Scholar] [CrossRef] [Green Version]
- Satherley, R.M.; Howard, R.; Higgs, S. Development and Validation of the Coeliac Disease Food Attitudes and Behaviours Scale. Gastroenterol. Res. Pract. 2018, 19, 6930269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cadenhead, J.W.; Wolf, R.L.; Lebwohl, B.; Lee, A.R.; Zybert, P.; Reilly, N.R.; Schebendach, J.; Satherley, R.; Green, P.H.R. Diminished quality of life among adolescents with coeliac disease using maladaptive eating behaviours to manage a gluten-free diet: A cross-sectional, mixed-methods study. J. Hum. Nutr. Diet. 2019, 32, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Casellas, F.; Rodrigo, L.; Lucendo, A.J.; Fernández-Bañares, F.; Molina-Infante, J.; Vivas, S.; Mercé Rosinach, D.C.; López-Vivancos, J. Benefit on health-related quality of life of adherence to gluten-free diet in adult patients with celiac disease. Rev. Esp. Enferm. Digestivas. 2015, 107, 196–201. [Google Scholar]
- Wolf, R.L.; Lebwohl, B.; Lee, A.R.; Zybert, P.; Reilly, N.R.; Cadenhead, J.; Amengual, C.; Green, P.H.R. Hypervigilance to a Gluten-Free Diet and Decreased Quality of Life in Teenagers and Adults with Celiac Disease. Dig. Dis. Sci. 2018, 63, 1438–1448. [Google Scholar] [CrossRef] [PubMed]
- Tremelling, K.; Sandon, L.; Vega, G.L.; McAdams, C.J. Orthorexia Nervosa and Eating Disorder Symptoms in Registered Dietitian Nutritionists in the United States. J. Acad. Nutr. Diet. 2017, 117, 1612–1617. [Google Scholar] [CrossRef] [PubMed]
- Al-Kattan, M. The Prevalence of Orthorexia Nervosa in Lebanese University Students and the Relationship between Orthorexia Nervosa and Body Image, BodyWeight and Physical Activity. Master’s Thesis, University of Chester, Chester, UK, 2016. [Google Scholar]
- Almeida, C.; Vieira Borba, V.; Santos, L. Orthorexia nervosa in a sample of Portuguese fitness participants. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2018, 23, 443–451. [Google Scholar] [CrossRef]
- Clifford, T.; Blyth, C. A pilot study comparing the prevalence of orthorexia nervosa in regular students and those in University sports teams. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2019, 24, 473–480. [Google Scholar] [CrossRef] [Green Version]
- Rudolph, S. The connection between exercise addiction and orthorexia nervosa in German fitness sports. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2018, 23, 581–586. [Google Scholar] [CrossRef]
- Malmborg, J.; Bremander, A.; Olsson, M.C.; Bergman, S. Health status, physical activity, and orthorexia nervosa: A comparison between exercise science students and business students. Appetite 2017, 109, 137–143. [Google Scholar] [CrossRef]
- Passananti, V.; Santonicola, A.; Bucci, C.; Andreozzi, P.; Ranaudo, A.; Di Giacomo, D.V.; Ciacci, C. Bone mass in women with celiac disease: Role of exercise and gluten-free diet. Dig Liver Dis. 2012, 44, 379–383. [Google Scholar] [CrossRef]
- Hagströmer, M.; Oja, P.; Sjöström, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Watson, K.B.; Carlson, S.A.; Gunn, J.P.; Galuska, D.A.; O’Connor, A.; Greenlund, K.J.; Fulton, J.E. Physical inactivity among adults aged 50 years and older—United States, 2014. Cent. Dis. Control Prev. 2016, 65, 954–958. [Google Scholar] [CrossRef] [PubMed]
- White, M.C.; Shoemaker, M.L.; Park, S.; Neff, L.J.; Carlson, S.A.; Brown, D.R.; Kanny, D. Prevalence of modifiable cancer risk factors among U.S. adults aged 18–44 years. Am. J. Prev. Med. 2017, 53, S14–S20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sampson, H.A. Food Allergy. J. Allergy Clin. Immunol. 2003, 111, S540–S547. [Google Scholar] [CrossRef]
- Dowd, A.J.; Kronlund, L.; Parmar, C.; Daun, J.T.; Wytsma-Fisher, K.; Reimer, R.A.; Millet, G.Y.; Culos-Reed, S.N. A 12-Week Pilot Exercise Program for Inactive Adults with Celiac Disease: Study Protocol. Glob. Adv. Health Med. 2019, 8, 2164956119853777. [Google Scholar] [CrossRef]
- Dowd, A.J.; Kronlund, L.; Warbeck, C.; Parmar, C.; Daun, J.T.; Wytsma-Fisher, K.; Reimer, R.A.; Millet, G.; Fung, T.; Culos-Reed, S.N. Effects of a 12-week HIIT + group mediated cognitive behavioural intervention on quality of life among inactive adults with coeliac disease: Findings from the pilot MOVE-C study. Psychol. Health 2021, 26, 1–17. [Google Scholar] [CrossRef]
- Missbach, B.; Hinterbuchinger, B.; Dreiseitl, V.; Zellhofer, S.; Kurz, C.; König, J. When Eating Right, Is Measured Wrong! A Validation and Critical Examination of the ORTO-15 Questionnaire in German. PLoS ONE 2015, 10, e0135772. [Google Scholar] [CrossRef]
- Barrada, J.R.; Roncero, M. Bidimensional Structure of the Orthorexia: Development and Initial Validation of a New Instrument. Ann. Psicol. 2018, 34, 283–291. [Google Scholar] [CrossRef]
- Brytek-Matera, A.; Plasonja, N.; Décamps, G. Assessing Orthorexia Nervosa: Validation of the Polish Version of the Eating Habits Questionnaire in a General Population Sample. Nutrients 2020, 12, 3820. [Google Scholar] [CrossRef]


| Parameter | Value |
|---|---|
| Age (year) | |
| (Median/Q1–Q3) | 34 (28–39) |
| (Average/age range/min-max) | 34 ± 8.7/18–64 |
| BMI (kg/m2) | |
| (Average/range) | 21.51 (14.1–29.75) |
| (Median/Q1–Q3) | 21.25 (19.1–23.6) |
| Education (%) | |
| Tertiary | 80.5 |
| Secondary | 15.4 |
| Middle | 3.2 |
| Primary | 0.8 |
| Occupation (%) | |
| Pension/retirement | 1.6% |
| Odd job | 1.6% |
| Unemployed | 5.7% |
| Parental leave | 8.1% |
| Students | 8.1% |
| Permanent employment | 74.8% |
| Weight Status (%) | |
| Underweight (moderate thinness) (16.0–16.99) | 6% |
| Underweight (mild thinness) (17.0–18.49) | 11% |
| Normal body weight (18.5–24.99) | 73% |
| Overweight (25.0–29.99) | 10% |
| Duration of celiac disease (n/%) | |
| Newly diagnosed (1–3 years) | 29 (24%) |
| Patients with the celiac disease for at least 3 years | 94 (76%) |
| Comorbidities (%) | |
| Lactose intolerance | 23% |
| Hashimoto’s disease | 22% |
| Hypothyroidism | 17% |
| Food allergy | 14% |
| Duhring’s disease | 6.5% |
| The most common symptoms reported before treatment of celiac patients | |
| Bloating | 53% |
| Chronic diarrhea | 49% |
| Anemia | 41% |
| Low body weight | 24% |
| Adherence to gluten-free diet (%) | |
| Full | 100% |
| Health self-assessment on a gluten-free diet (%) | |
| Better | 87% |
| No change | 10% |
| Worse | 3% |
| Questions from ORTO-15 Test | Score * (Mean ± SD) | Spearman’s Rho | Cronbach’s Alpha Coefficient ** | Mean ± SD of Total Points *** |
|---|---|---|---|---|
| 1. When eating, do you pay attention to the calories of the food? | 2.91 ± 0.90 | 0.33 | 0.66 | 34.82 ± 5.07 |
| 2. When you go in a food shop do you feel confused? | 3.34 ± 0.89 | 0.31 | 0.66 | 34.39 ± 5.08 |
| 3. In the last 3 months, did the thought of food worry you? | 2.57 ± 1.00 | 0.53 | 0.63 | 35.16 ± 4.83 |
| 4. Are your eating choices conditioned by your worry about your health status? | 1.66 ± 0.61 | 0.15 | 0.68 | 36.07 ± 5.30 |
| 5. Is taste of food more important than the quality when you evaluate food? | 2.53 ± 0.77 | 0.12 | 0.68 | 35.20 ± 5.29 |
| 6. Are you willing to spend more money to have healthier food? | 2.01 ± 0.66 | 0.11 | 0.68 | 35.72 ± 5.32 |
| 7. Does the thought about food worry you for more than three hours a day? | 3.34 ± 0.87 | 0.55 | 0.63 | 34.38 ± 4.90 |
| 8. Do you allow yourself any eating transgressions? | 3.00 ± 0.82 | −0.03 | 0.70 | 34.73 ± 5.39 |
| 9. Do you think your mood affects your eating behavior? | 2.33 ± 0.79 | 0.58 | 0.63 | 35.43 ± 4.93 |
| 10. Do you think that the conviction to eat only healthy food increases self-esteem? | 2.96 ± 0.93 | 0.51 | 0.63 | 34.77 ± 4.90 |
| 11. Do you think that eating healthy food changes your life-style (frequency of eating out, friends…)? | 2.38 ± 0.92 | 0.34 | 0.66 | 35.35 ± 5.05 |
| 12. Do you think that consuming healthy food may improve your appearance? | 2.07 ± 0.82 | 0.38 | 0.65 | 35.67 ± 5.06 |
| 13. Do you feel guilty when transgressing? | 2.52 ± 1.11 | 0.26 | 0.67 | 35.21 ± 5.03 |
| 14. Do you think that on the market there is also unhealthy food? | 1.43 ± 0.68 | 0.02 | 0.69 | 36.30 ± 5.35 |
| 15. At present, are you alone when having meals? | 2.72 ± 0.83 | 0.09 | 0.69 | 35.02 ± 5.29 |
| Reliability Analysis | Mean ± SD * | Min-Max * | Cronbach’s Raw α Coefficient | Standardized Cronbach’s α Coefficient | Average Spearman’s Rho between Questions |
|---|---|---|---|---|---|
| ORTO-15 questionnaire (15 scale items) | 37.73 ± 5.45 | 23–53 | 0.67 | 0.66 | 0.11 |
| ORTO-15 questionnaire (excluding question 8) | 34.73 ± 5.41 | 20–50 | 0.70 | 0.68 | 0.13 |
| Risk of Orthorexia | ORTHO-15 * | |
|---|---|---|
| n * | % | |
| The entire study group | 123 | 100 |
| Participants at risk of orthorexia ** | 87 | 71 |
| Participants at risk of orthorexia *** | 39 | 32 |
| Eating Habits and Behaviors * | Risk of Orthorexia | χ² Test p | ||
|---|---|---|---|---|
| Yes (n = 87) | No (n = 36) | |||
| Frequency of meals per day | 3 times a day | 36%(n = 31) | 19% (n = 7) | p = 0.014 |
| 4 times a day | 38% (n = 33) | 67% (n = 24) | ||
| 5 times a day | 26% (n = 23) | 14% (n = 5) | ||
| Independent preparation of gluten-free meals | 94% (n = 82) | 78% (n = 28) | p = 0.006 | |
| Difficulty eating out | 78% (n = 68) | 92%% (n = 33) | p = 0.075 | |
| Paying attention to the caloric content of gluten-free meals | 54% (n = 47) | 53% (n = 19) | p = 0.899 | |
| Paying attention to the composition of gluten-free products | 87% (n = 76) | 92% (n = 33) | p = 0.493 | |
| Physical activity * | ||||
| Total number of active people | 70% (n = 61) | 81% (n = 29) | p = 0.234 | |
| Aerobic (fitness) | 13% (n = 13) | 31% (n = 11) | p = 0.046 | |
| Swimming | 9% (n = 8) | 6% (n = 2) | p = 0.050 | |
| Strength training gym | 9% (n = 8) | 22% (n = 8) | p = 0.050 | |
| Running | 5% (n = 4) | 17% (n = 6) | p = 0.025 | |
| Walking | 46% (n = 40) | 53% (n = 19) | p = 0.492 | |
| Yoga | 5% (n = 4) | 0% | p = 0.190 | |
| Cycling | 30% (n = 26) | 42% (n = 15) | p = 0.207 | |
| Frequency of physical activity | 71% (n = 87) | 29% (n = 36) | p = 0.599 | |
| 1 time per week | 16% (n = 14) | 11% (n = 4) | ||
| 2–3 times a week | 37% (n = 32) | 44% (n = 16) | ||
| 4 and more per week | 14% (n = 12) | 17% (n = 6) | ||
| Daily | 9% (n = 8) | 14% (n = 5) | ||
| No physical activity | 24% (n = 21) | 14% (n = 5) | ||
| Risk of Orthorexia | χ² Test | ||
|---|---|---|---|
| ORTO-15 Questions | Yes (n = 87) | No (n = 36) | p |
| 1. When eating, do you pay attention to the calories of the food? | p = 0.001 | ||
| Always/Often % | 46%** | 69% | |
| 2. When you go in a food shop do you feel confused? | p = 0.003 | ||
| Always/Often % | 73% | 94% | |
| 3. In the last 3 months, did the thought of food worry you? | p = 0.001 | ||
| Always/Often % | 64% | 8% | |
| 4. Are your eating choices conditioned by your worry about your health status? | p = 0.086 | ||
| Always/Often % | 92% | 95% | |
| 5. Is taste of food more important than the quality when you evaluate food? | p = 0.043 | ||
| Always/Often % | 49% | 72% | |
| 6. Are you willing to spend more money to have healthier food? | p = 0.071 | ||
| Always/Often % | 85% | 67% | |
| 7. Does the thought about food worry you for more than three hours a day? | p = 0.001 | ||
| Always/Often % | 22% | 0% | |
| 8. Do you allow yourself any eating transgressions? | p = 0.437 | ||
| Always/Often % | 73% | 87% | |
| 9. Do you think your mood affects your eating behavior? | p = 0.001 | ||
| Always/Often % | 20% | 80% | |
| 10. Do you think that the conviction to eat only healthy food increases self-esteem? | p = 0.001 | ||
| Always/Often % | 43% | 6% | |
| 11. Do you think that eating healthy food changes your life-style (frequency of eating out, friends…)? | p = 0.001 | ||
| Always/Often % | 68% | 31% | |
| 12. Do you think that consuming healthy food may improve your appearance? | p = 0.001 | ||
| Always/Often % | 83% | 59% | |
| 13. Do you feel guilty when transgressing? | p = 0.001 | ||
| Always/Often % | 42% | 39% | |
| 14. Do you think that on the market there is also unhealthy food? | |||
| Always/Often % | 95% | 94% | p = 0.012 |
| 15. At present, are you alone when having meals? | |||
| Always/Often % | 41% | 42% | p = 0.819 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kujawowicz, K.; Mirończuk-Chodakowska, I.; Witkowska, A.M. Dietary Behavior and Risk of Orthorexia in Women with Celiac Disease. Nutrients 2022, 14, 904. https://doi.org/10.3390/nu14040904
Kujawowicz K, Mirończuk-Chodakowska I, Witkowska AM. Dietary Behavior and Risk of Orthorexia in Women with Celiac Disease. Nutrients. 2022; 14(4):904. https://doi.org/10.3390/nu14040904
Chicago/Turabian StyleKujawowicz, Karolina, Iwona Mirończuk-Chodakowska, and Anna Maria Witkowska. 2022. "Dietary Behavior and Risk of Orthorexia in Women with Celiac Disease" Nutrients 14, no. 4: 904. https://doi.org/10.3390/nu14040904






