Abdominal Computed Tomography Imaging Findings in Hospitalized COVID-19 Patients: A Year-Long Experience and Associations Revealed by Explainable Artificial Intelligence
Abstract
:1. Introduction
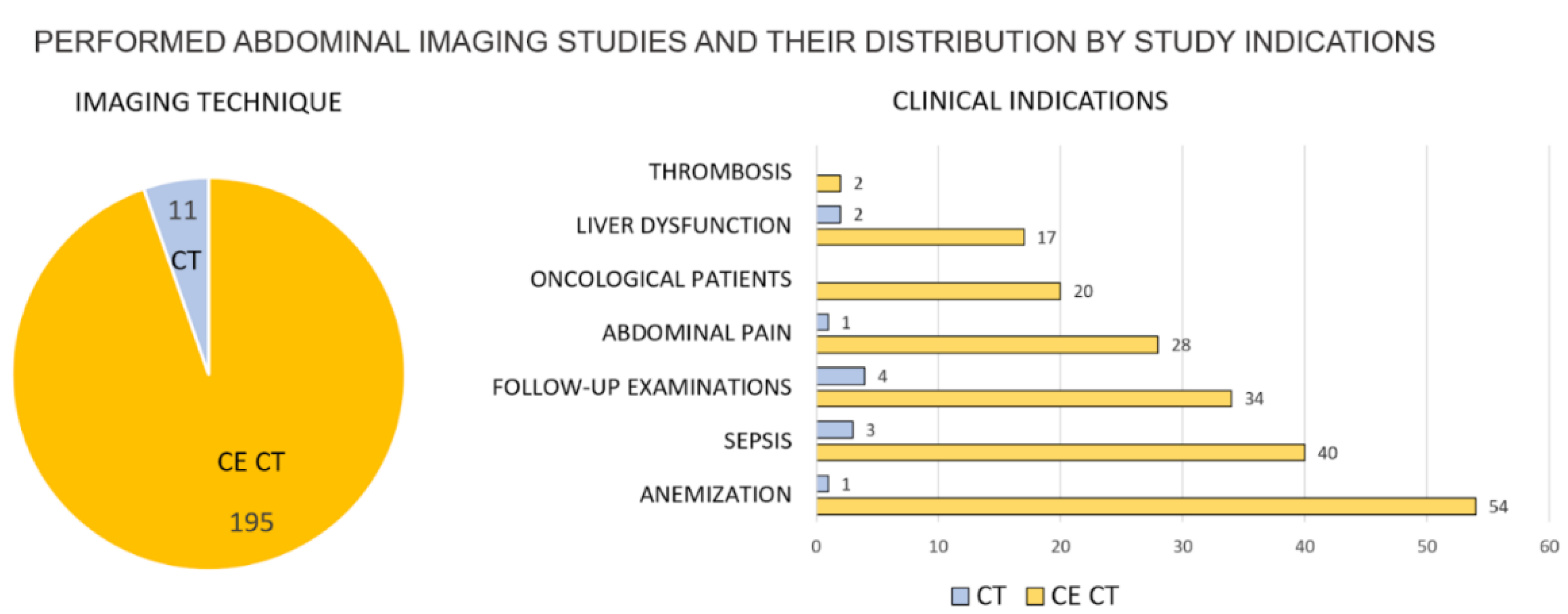
2. Materials and Methods
2.1. Patients Population
2.2. Image Acquisition
2.3. Image Analysis
2.4. Explainable AI for Causal Inference
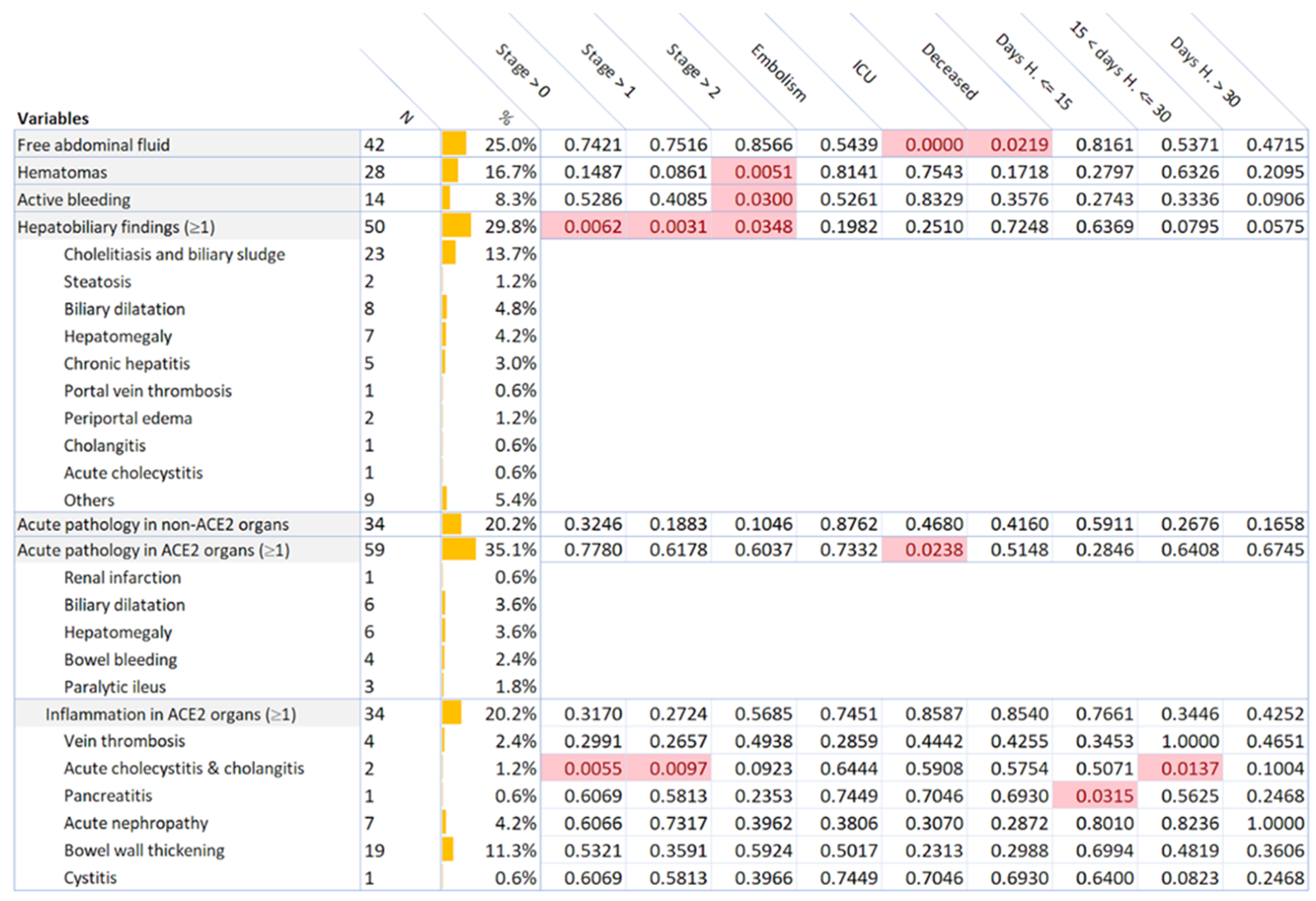
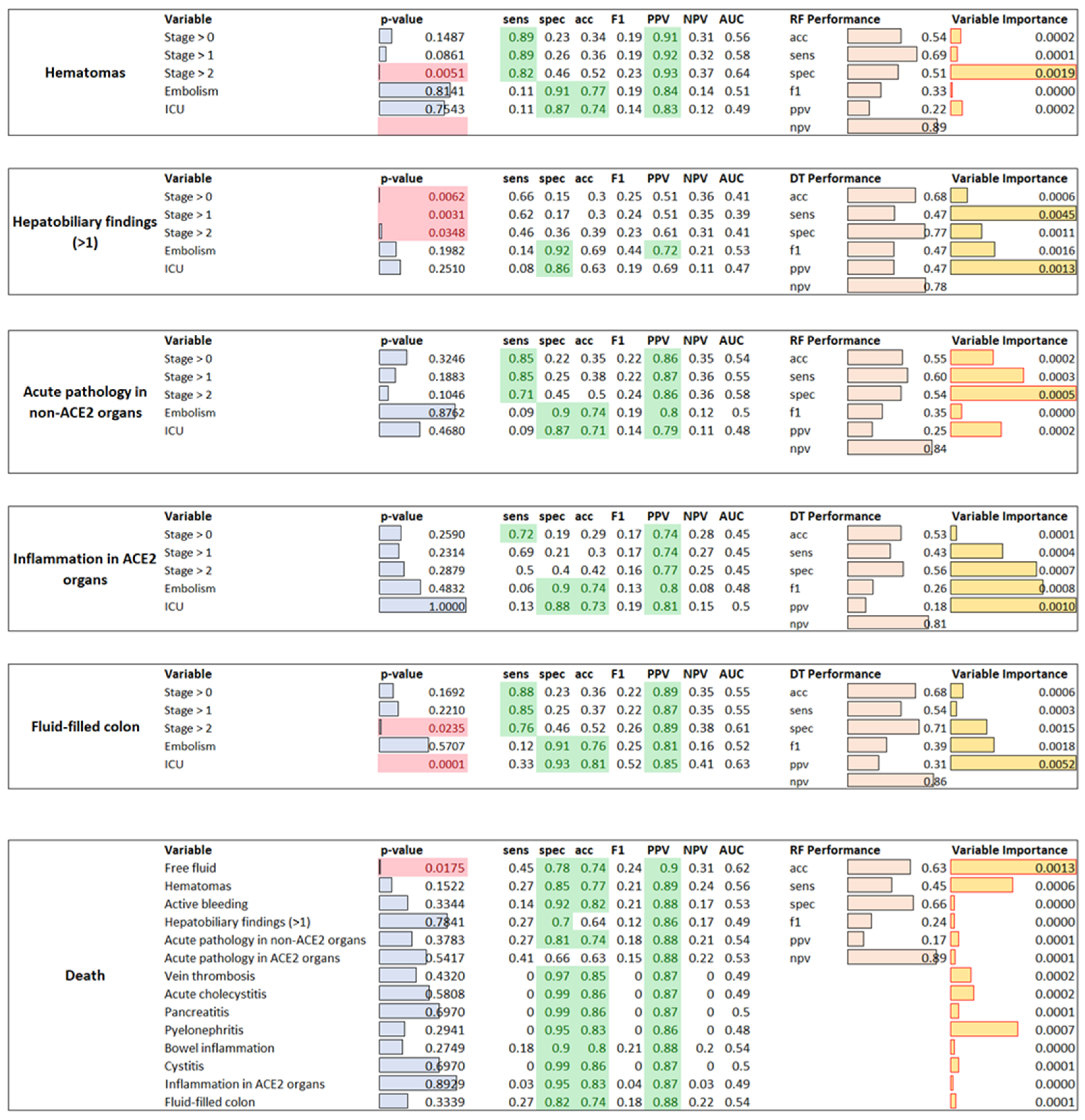
3. Results
4. Discussion
5. Conclusions
Abdominal Abnormalities Were Common Findings in COVID-19 Patients
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- WHO. Coronavirus Disease (COVID-19) Dashboard; World Health Organization: Geneva, Switzerland, 2020; Available online: https://covid19.who.int/ (accessed on 2 May 2021).
- Matricardi, P.; Dal Negro, R. The first, holistic immunological model of COVID-19: Implications for prevention, diagnosis, and public health measures. Paediatr. Allergy Immunol. 2020, 31, 454–470. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef]
- Qi, F.; Qian, S.; Zhang, S. Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses. Biochem. Biophys. Res. Commun. 2020, 526, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Pan, L.; Mu, M.; Yang, P. Clinical Characteristics of COVID-19 Patients with Digestive Symptoms in Hubei, China: A Descriptive, Cross-sectional, Multicenter Study. Am. J. Gastroenterol. 2020, 115, 766–773. [Google Scholar] [CrossRef]
- Cheung, K.S.; Hung, I.F.N.; Chan, P.P.Y.; Lung, K.C.; Tso, E.; Liu, R.; Ng, Y.Y.; Chu, M.Y.; Chung, T.W.H.; Tam, A.R.; et al. Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples from a Hong Kong Cohort: Systematic Review and Meta-analysis. Gastroenterology 2020, 159, 81–95. [Google Scholar] [CrossRef]
- Parasa, S.; Desai, M. Prevalence of Gastrointestinal Symptoms and Fecal Viral Shedding in Patients with Coronavirus Disease 2019: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e2011335. [Google Scholar] [CrossRef]
- Tirumani, S.H.; Rahnemai-Azar, A.A. Are asymptomatic gastrointestinal findings on imaging more common in COVID-19 infection? Study to determine frequency of abdominal findings of COVID-19 infection in patients with and without abdominal symptoms and in patients with chest-only CT scans. Abdom. Radiol. 2021, 46, 2407–2414. [Google Scholar] [CrossRef]
- Shiralkar, K.; Chinapuvvula, N. Cross-Sectional Abdominal Imaging Findings in Patients with COVID-19. Cureus 2020, 12, e9538. [Google Scholar] [CrossRef] [PubMed]
- Bhayana, R.; Som, A. Abdominal Imaging Findings in COVID-19: Preliminary Observations. Radiology 2020, 297, E207–E215. [Google Scholar] [CrossRef]
- Pan, F.; Ye, T. Time Course of Lung Changes on Chest CT During Recovery From 2019 Novel Coronavirus (COVID-19) Pneumonia. Radiology 2020, 295, 715–721. [Google Scholar] [CrossRef] [Green Version]
- Yueying, P.; Hanxiong, G. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): A study of 63 patients in Wuhan, China. Eur. Radiol. 2020, 30, 3306–3309. [Google Scholar]
- Stekhoven, D.J.; Bühlmann, P. MissForest—Non-parametric missing value imputation for mixed-type data. Bioinformatics 2012, 28, 112–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kleinbaum, D.G.; Klein, M. Logistic Regression; Springer: New York, NY, USA, 2002. [Google Scholar]
- Nelder, J.A.; Wedderburn, R.W.M. Generalized linear models. J. R. Stat. Soc. Ser. A Gen. 1972, 135, 370–384. [Google Scholar] [CrossRef]
- Safavian, S.R.; Landgrebe, D. A survey of decision tree classifier methodology. IEEE Trans. Syst. Man Cybern. 1991, 21, 660–674. [Google Scholar] [CrossRef] [Green Version]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef] [Green Version]
- Horton, P.; Nakai, K. Better Prediction of Protein Cellular Localization Sites with the it k Nearest Neighbors Classifier. Proc. Int. Conf. Intell. Syst. Mol. Biol. 1997, 5, 147–152. [Google Scholar] [PubMed]
- Snoek, J.; Larochelle, H.; Adams, R.P. Practical bayesian optimization of machine learning algorithms. arXiv 2012, arXiv:1206.2944. [Google Scholar]
- Molenat, F.; Boussuges, A. Gallbladder abnormalities in medical ICU patients: An ultrasonographic study. Intensive Care Med. 1996, 22, 356–358. [Google Scholar] [CrossRef]
- Nardo, A.D.; Schneeweiss-Gleixner, M. Pathophysiological mechanisms of liver injury in COVID-19. Liver Int. 2021, 41, 20–32. [Google Scholar] [CrossRef]
- Chai, X.; Hu, L. Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. bioRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Banales, J.M.; Huebert, R.C. Cholangiocyte pathobiology. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 269–281. [Google Scholar] [CrossRef] [PubMed]
- El Moheb, M.; Naar, L. Gastrointestinal Complications in Critically Ill Patients with and without COVID-19. JAMA 2020, 324, 1899–1901. [Google Scholar] [CrossRef]
- Funt, S.A.; Cohen, S.L. Abdominal pelvic CT findings compared between COVID-19 positive and COVID-19 negative patients in the emergency department setting. Abdom. Radiol. 2021, 46, 1498–1505. [Google Scholar] [CrossRef]
- Behzad, S.; Aghaghazvini, L. Extrapulmonary manifestations of COVID-19: Radiologic and clinical overview. Clin. Imaging 2020, 66, 35–41. [Google Scholar] [CrossRef]
- Zaim, S.; Chong, J.H. COVID-19 and multiorgan response. Curr. Probl. Cardiol. 2020, 45, 100618. [Google Scholar] [CrossRef]
- Rodríguez, C.; Luque, N. Pulmonary Endothelial Dysfunction and Thrombotic Complications in Patients with COVID-19. Am. J. Respir. Cell Mol. Biol. 2021, 64, 407–415. [Google Scholar] [CrossRef] [PubMed]
- MSD Manuals Msdmanuals. Available online: https://www.msdmanuals.com/professional/hepatic-and-biliary-disorders/gallbladder-and-bile-duct-disorders/acute-cholecystitis (accessed on 9 November 2021).
- Hilton, R. Defining acute renal failure. CMAJ 2011, 183, 1167–1169. [Google Scholar] [CrossRef] [Green Version]
- Summary of Recommendation Statements. Kidney Int. Suppl. 2013, 3, 5–14. [CrossRef] [Green Version]
- Stanford Childrens. Available online: https://www.stanfordchildrens.org/en/topic/default?id=biliary-dilatation-22-biliarydilatation (accessed on 9 November 2021).
- National Center of Biotechnology Information (NCBI). Available online: https://www.ncbi.nlm.nih.gov/books/NBK568709/ (accessed on 9 November 2021).
- Macari, M.; Balthazar, E.J. CT of bowel wall thickening: Significance and pitfalls of interpretation. AJR Am. J. Roentgenol. 2001, 176, 1105–1116. [Google Scholar] [CrossRef] [PubMed]
- National Center for Biotechnology Information (NCBI). Available online: https://www.ncbi.nlm.nih.gov/books/NBK558946/ (accessed on 9 November 2021).
- MSD Manuals Msdmanuals. Available online: https://www.msdmanuals.com/professional/hepatic-and-biliary-disorders/gallbladder-and-bile-duct-disorders/cholelithiasis (accessed on 9 November 2021).
- MSD Manuals Msdmanuals. Available online: https://www.msdmanuals.com/professional/hepatic-and-biliary-disorders/hepatitis/overview-of-chronic-hepatitis (accessed on 9 November 2021).
- National Cancer Institute: Comprehensive Cancer Information. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cystitis (accessed on 9 November 2021).
- National Cancer Institute: Comprehensive Cancer Information. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/hematoma (accessed on 9 November 2021).
- UpToDate. Available online: https://www.uptodate.com/contents/overview-of-the-evaluation-of-hepatomegaly-in-adults-search=Hepatomegaly (accessed on 9 November 2021).
- National Center for Biotechnology Information (NCBI). Available online: https://www.ncbi.nlm.nih.gov/books/NBK538337/ (accessed on 9 November 2021).
- National Center for Biotechnology Information (NCBI). Available online: https://www.ncbi.nlm.nih.gov/books/NBK560669/ (accessed on 9 November 2021).
- UpToDate. Available online: https://www.uptodate.com/contents/congestivehepatopathy-search=periportal-edema (accessed on 9 November 2021).
- UpToDate. Available online: https://www.uptodate.com/contents/acute-portal-vein-thrombosis-in-adults-clinical-manifestations-diagnosis-and-management (accessed on 9 November 2021).
- UpToDate. Available online: https://www.uptodate.com/contents/renal-infarction?search=renal-infarction (accessed on 8 November 2021).
- Simón, J.; Casado-Andrés, M. Nutraceutical Properties of Polyphenols against Liver Diseases. Nutrients 2020, 12, 3517. [Google Scholar] [CrossRef] [PubMed]
- National Center for Biotechnology Information (NCBI). Available online: https://www.ncbi.nlm.nih.gov/books/NBK507708/ (accessed on 9 November 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarabelli, A.; Zilocchi, M.; Casiraghi, E.; Fasani, P.; Plensich, G.G.; Esposito, A.A.; Stellato, E.; Petrini, A.; Reese, J.; Robinson, P.; et al. Abdominal Computed Tomography Imaging Findings in Hospitalized COVID-19 Patients: A Year-Long Experience and Associations Revealed by Explainable Artificial Intelligence. J. Imaging 2021, 7, 258. https://doi.org/10.3390/jimaging7120258
Scarabelli A, Zilocchi M, Casiraghi E, Fasani P, Plensich GG, Esposito AA, Stellato E, Petrini A, Reese J, Robinson P, et al. Abdominal Computed Tomography Imaging Findings in Hospitalized COVID-19 Patients: A Year-Long Experience and Associations Revealed by Explainable Artificial Intelligence. Journal of Imaging. 2021; 7(12):258. https://doi.org/10.3390/jimaging7120258
Chicago/Turabian StyleScarabelli, Alice, Massimo Zilocchi, Elena Casiraghi, Pierangelo Fasani, Guido Giovanni Plensich, Andrea Alessandro Esposito, Elvira Stellato, Alessandro Petrini, Justin Reese, Peter Robinson, and et al. 2021. "Abdominal Computed Tomography Imaging Findings in Hospitalized COVID-19 Patients: A Year-Long Experience and Associations Revealed by Explainable Artificial Intelligence" Journal of Imaging 7, no. 12: 258. https://doi.org/10.3390/jimaging7120258





