Abstract
Background: Poor medication adherence results in negative health outcomes and increased healthcare costs. Several healthcare professionals provide interventions to improve medication adherence, with the effectiveness of nurse-led interventions in people with chronic diseases remaining unclear. Objective: This study sought to evaluate the effectiveness of nurse-led interventions for improving medication adherence in adults with chronic conditions. Methods: Five databases (MEDLINE, CINAHL, EMBASE, Cochrane Library, SCOPUS) were searched without applying a temporal limit. Studies evaluating the effects of nurse-led interventions on medication adherence in adults with one or multiple chronic conditions were included. Interventions only targeting a single acute disease were excluded. Results: A total of twenty-two studies with 5975 participants were included. Statistically significant improvements in adherence were reported in five out of seven studies involving face-to-face visits to patients with heart failure (n = 2), chronic myeloid leukemia (n = 1), hypertension (n = 1) and multimorbidity (n = 1) and in four out of nine studies adopting a mixed method involving face-to-face visits and telephone follow-up for patients with heart failure (n = 1), hypertension (n = 1), coronary disease (n = 1) and multimorbidity (n = 1). Remote interventions were effective in improving medication adherence in one out of six studies. No statistically significant differences were found between tablet computer-based patient education and nurse-led educational sessions. The motivational approach was found to be one of the most common strategies used to promote patient medication adherence. Conclusions: Nurse-led face-to-face visits may be effective in improving medication adherence in people with chronic diseases. However, further research is needed because current methods for measuring medication adherence may not accurately capture patient behaviour and medication consumption patterns.
1. Introduction
The World Health Organization (WHO) defined medication adherence as “the extent to which a person takes medication, corresponds to agreed recommendations from a health care provider” [1]. Medication adherence is crucial for the success of treatment plans and improving patient outcomes, yet adherence to long-term therapy for chronic illnesses is estimated at only around 50% and is a common problem that occurs in various contexts, regardless of the disease being treated, its severity, or access to healthcare resources [1,2].
Many patients do not completely comply with their prescribed medications and often discontinue or do not take them as prescribed after the first month [3]. Poor medication adherence therefore represents a major obstacle to realizing the benefits of drugs that have proven to be more beneficial than harmful in clinical trials [3].
Improving medication adherence can reduce morbidity, mortality, and inpatient hospital stays and improve overall health condition [4,5,6]. Conversely, poor medication adherence results in negative health outcomes and increased healthcare costs [4]. Numerous factors are known to be associated with poor adherence, including patient demographics, psychosocial and socioeconomic factors, disease-related issues, and the patient–provider relationship [7,8].
Psychosocial and cultural beliefs can influence a patient’s medication behaviour, for example, a sense of mistrust or negative beliefs about medication, which may lead to thinking that the medication is ineffective or not really needed when symptoms resolve or when a potential side effect is experienced [8]. Such beliefs could be changed through education and support provided by healthcare professionals [8].
Non-adherence to medication has been defined as both “taking less than 80% of the prescribed doses” or equally taking higher doses [3]. Risk factors for non-adherence include polypharmacy, complex treatment plans, cognitive decline, and lack of support from health professionals and family members [6,8]. Polypharmacy is particularly problematic in older adults who often have multiple chronic conditions [6,9].
Although no optimal strategies for enhancing medication adherence have been recognized, building a strong alliance, educating patients, involving caregivers, and monitoring tolerability and side effects could improve patients’ medication adherence [10]. Consequently, all the patient’s disease-related and socioeconomic factors should be explored within the context of their lived experience. Notable too is that patients demonstrate better adherence when receiving care from the same provider over time, with attention paid to tailoring the communication of their needs [1].
Intervention to improve medication adherence can be provided by various healthcare professionals such as physicians, nurses, and pharmacists, as highlighted in previous systematic reviews [5,6,7,11]. A previous Cochrane systematic review [3] examined a variety of interventions provided by different health professionals aimed at improving medication adherence and concluded that there is insufficient evidence to suggest that medication adherence can be effectively enhanced with the current resources available in clinical settings. A proposed solution to the problem involves expanding the nursing role by allocating specific time for medication education and management to promote adherence in a sustainable and feasible manner within clinical settings [3]. Even if nurses are the most numerous healthcare professionals and closest to the patient in terms of knowledge and daily interaction, there is limited evidence regarding the impact of nursing interventions, either alone or in conjunction with other healthcare professionals, on improving medication adherence among adults with chronic conditions.
As frontline healthcare providers, nurses are uniquely positioned to understand patients’ needs and challenges daily, making them valuable contributors to policymaking and decision-making processes [12,13]. By actively participating in developing and implementing health policies, nurses can advocate for improvements in patient care, access to healthcare services, and overall health outcomes [14]. Exploring the impact of nursing intervention is fundamental as they already deal with medication administration and education in the healthcare environment daily [15].
The only available evidence supporting the effectiveness of nurse-led intervention in improving medication adherence is inconsistent, focused on specific diseases and generally in combination with psychological interventions [5,7,11]. In fact, two systematic reviews reported that nurse-led motivational interviewing and counselling enhanced medication adherence only in individuals with heart disease, older adults discharged from hospitals, and those with HIV [5,7,11].
To our knowledge, no previous systematic reviews have analyzed the effectiveness of nurse-led interventions alone in improving medication adherence in people with one or multiple chronic diseases.
Considering the impact of poor or non-adherence to medications on health outcomes in people with chronic conditions and on health services, this systematic review aimed to synthesize evidence on the effectiveness of nurse-led interventions in improving medication adherence in adults with chronic conditions. In addition, evidence-based strategies to enhance medication adherence and health outcomes in people with chronic diseases have been highlighted.
2. Methods
2.1. Design
We conducted a systematic review and a meta-analysis according to the updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [16]. The review protocol was registered in the PROSPERO register of systematic reviews on 10 March 2023 (registration number CRD42023403467), available at https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=403467 (accessed on 10 October 2024). We made no amendments to the original protocol.
2.2. Search Strategy
To create a comprehensive search strategy and identify keywords, we searched five databases (MEDLINE via Pubmed, CINAHL, EMBASE, Cochrane Library, and SCOPUS) initially from their inception to 1 March 2023, with the search re-run on 17 May 2024. One investigator (DB) with experience searching the literature under a health librarian’s (BM) supervision conducted this search. A combination of free text and MeSH terms were used, and no temporal restrictions were applied. An example search strategy is shown in Table 1. The full search strategy is presented as a Supplementary File. In addition, the PROSPERO register of systematic reviews was searched for ongoing, recently completed reviews and clinical trial registers (WHO International Clinical Trial Register Platform and Clinicaltrial.gov).

Table 1.
PUBMED search strategy.
2.3. Eligibility Criteria
We included clinical trials, controlled clinical trials, and randomized controlled trials published in peer-reviewed journals that assessed the efficacy of interventions performed by nurses on patients with one or more chronic condition. To be eligible, studies had to provide nurse-led or nurse-collaborative interventions to adults (≥18 years) and measure medication adherence as a primary or secondary outcome. Interventions were defined as such if they were based on a theory, a theoretical framework, a model, or an explicit method. We included nurse-collaborative interventions only where data related to the nurse’s role were described. Interventions were defined as nurse-collaborative where their involvement was part of an interdisciplinary team. Nurse-led or nurse-collaborative interventions were compared to usual care or any other control interventions. Interventions only targeting an acute single disease were excluded. Studies that focused on addiction diseases, where adherence problems are typically of a different nature and much more severe, as well as studies reporting patients’ lived experience during nurse-led interventions and follow-up were excluded. In addition, conference proceedings, theses, letters to the editor, and other grey literature were excluded.
2.4. Article Screening and Study Selection
Two reviewers (DB, AC) independently screened the titles and abstracts of all records to remove duplicates and identify relevant publications. Rayyan software (https://www.rayyan.ai/) was used for the title/abstract screening process. We retrieved the full-text versions of all potentially relevant records. In case of disagreements, a third reviewer (SC) was involved.
2.5. Assessment of Risk of Bias
The risk of bias was independently assessed by two reviewers (DB, AH) using the Revised Cochrane risk-of-bias tool for randomized trials (RoB2) [17]. Any disagreement was solved through discussion with a third investigator (AC). RoB 2 is the recommended tool to assess the risk of bias in randomized trials. RoB 2 is structured into a fixed set of 5 bias domains, focusing on different aspects of trial design, conduct, and reporting. Each domain provides a series of questions that aim to elicit information about features of the trial that are relevant to the risk of bias, with five response options (yes, probably yes, probably no, no, and no information). A judgement about the risk of bias arising from each domain is proposed by an algorithm based on given answers, but this needs to be confirmed by the investigator. The final judgement can be “Low” or “High” risk of bias, or it can express “Some concerns”. The overall risk of bias was rated as “low” if the risk of bias was low in all key domains. The study is judged to raise “some concerns” if it is in at least one domain for this result, but not to be at high risk of bias for any domain. The study is judged to be at high risk of bias in at least one domain for this result, or the study is judged to have some concerns for multiple domains in a way that substantially influences the result. The suggested Excel tool was used to collect risk-of-bias assessment data and generate visual “traffic light” plots of each domain-level judgement and overall judgement (available at riskofbias.info).
2.6. Data Extraction
Data were extracted by two independent reviewers (D.B. and A.C.). Data on study characteristics (author, country, year, study design, setting, study sample, description of the intervention, assessment tools or instruments, primary outcome investigated and timing of outcome measurements and follow-up), participants (sample size, chronic conditions), narrative summary of findings, and quantitative results (means and standard deviations or frequencies and percentages) were entered into a data collection form (Excel spreadsheet).
Discrepancies were resolved through discussion and involving a third reviewer (S.C.) when necessary. Efforts were made to contact authors to obtain missing information. The data collection form was piloted in five studies, and appropriate improvements were made.
2.7. Primary Outcome
Our primary outcome was patient medication adherence measured directly or indirectly. Direct methods included patient observation, taking the medication, or measuring medication levels in plasma or urine. Indirect methods encompassed pill count, use of pharmacological databases, a medication event-monitoring system (MEMS), questionnaires, scales, or self-reporting by patients or health professionals [18].
2.8. Secondary Outcomes
Our secondary outcomes were mortality, hospital readmission, need of urgent care and potentially relevant clinical outcomes.
2.9. Data Synthesis
Studies were grouped according to the mode of delivery and the characteristics of the intervention. Based on the Cochrane paradigm of Richards et al. [19], interventions were classified into two main categories of delivery: face-to-face or remote. Face-to-face interventions are characterized by the interaction between the implementer and the participant, which takes place in person. Instead, remote modalities included web-based, telephone-based, and telemonitoring interventions [20].
3. Results
3.1. Articles Included in Systematic Review and Meta-Analysis/Search Results
The search strategy generated 6137 articles, of which 1217 were duplicates which were removed. Screening of the titles and abstracts led to the exclusion of 4480 articles. A total of 40 articles were taken forward for full-text review. Eighteen were excluded as they did not meet the inclusion criteria, as stated in Figure 1. After re-running the search strategy, no additional articles were found. Twenty-two articles are included in this review. Among those included, additional data were requested from seven authors for data conversion for meta-analysis [21,22,23,24,25,26,27]. Only two authors answered, providing the requested information [22,24].
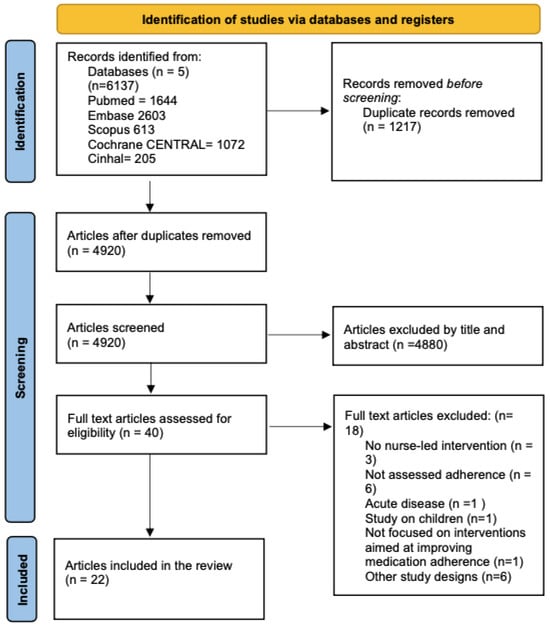
Figure 1.
Flow diagram of the study selection.
3.2. Characteristics of Studies Included in the Systematic Review
All studies were randomized control trials [21,22,23,24,25,26,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. Specifically, one was a cluster [37] and one was a pragmatic randomized control trial [31]. Blinding of the participants was not possible due to the nature of the interventions. Table 2 lists the characteristics of the included studies. These studies were published from 2006 to 2022 and performed in China [27,29,30,32,33,39,40,41,42], in the USA [22,23,24,34,37], in Europe [21,25,26,31,38], and in South America [28,35,36]. In sixteen studies, medication adherence was the primary outcome [21,22,23,24,25,27,28,29,32,34,36,38,39,40,41,42]. Other included outcomes were clinical endpoints, clinical outcomes, and patient-reported outcomes. Clinical endpoints were mortality [21,30,33,40,42], hospital readmission [21,30,32,33,39,40,42], and need of urgent care [21,22,33,39,41]. Clinical outcomes included blood pressure [27,29,35,36,37], BMI [35], immunosuppression level [26], glycated hemoglobin [31,36] and cholesterol level [31]. Patient-reported outcomes were self-care [28,40], self-management [27,30,35,37,41], self-monitoring [34,39], illness perception [22], coping strategies [32], knowledge of drug indications [37,41], treatment burden [41], QOL [27,27,31,32,35,37,39,40,42], healthy lifestyle behaviours [29,31], psychosocial outcomes [31], and satisfaction with care [22,39,41].

Table 2.
Summary of selected studies listed by date of publication.
3.3. Participants and Settings
The study sample size was variable, ranging from 33 [38] to 2665 [31], with a total of 5975 participants included in this review. The mean age of the individuals in the included studies was 59 years and ranged from 38 [38] to 82 [21]. Five studies targeted participants with multimorbidity, namely diabetes, depression and coronary disease [34]; hypertension and type 2 diabetes [36]; diabetes, hypertension, coronary heart disease, heart failure, depression and schizophrenia [31]; and hypertension, coronary heart disease, stroke and cerebrovascular disease [41]. One study did not state patients’ type of chronic disease [33]. The remaining studies were conducted among participants with a single chronic disease, such as heart failure [23,28,30,40,42], hypertension [27,29,35,37], coronary disease [21,22], atrial fibrillation [32], chronic myeloid leukemia [25], kidney disease [39], schizophrenia [38], HIV [24], and lung transplantation [26]. The studies were undertaken in a variety of different settings, such as hospital [21,22,23,25,26,27,29,30,33,39,40,42], health centres [32,36,37,41], clinics [24,28,34,35] and in ambulatory care [38]. For one study, data were retrieved from an insurance registry [31].
3.4. Characteristics of the Nurse-Led Intervention
Interventions were nurse-led in twenty studies and nurse-collaborative in two [34,37]. The detailed characteristics of the nurse-led interventions were extracted and are summarized in Table 3. In seven studies, nurse-led interventions were delivered through face-to-face visits [23,25,26,27,28,36,40]; in six studies, they were delivered through remote modalities (i.e., telephone follow-up or telemonitoring) [22,31,32,38,39,42]; and in nine studies, the two delivery methods were combined [21,24,29,30,33,34,35,37,41]. Among interventions carried out face-to-face, fourteen were structured educational interventions [21,23,24,25,27,28,29,30,34,35,36,37,40,41]. The frequency of these interventions varied from one meeting or encounter [21,25] to a maximum of eight [28], with their duration ranging from a five-minute telephone call [35] to a one-hour face-to-face visit [35]. Follow-up periods ranged from 24 h after the discharge of the patient [22] to 36 months [31] after the intervention.

Table 3.
Characteristics of the nurse-led face-to-face and remote interventions.
Twenty studies compared nurse-led interventions with usual care [21,22,23,24,25,27,28,29,30,31,33,34,35,36,37,38,39,40,41,42], whereas two studies compared nurse-led intervention with a web-based integrated management programme using tablet- and computer-based patient education [26,32].
3.5. Medication Adherence Measurements
Measurements of medication adherence varied widely (Table 2). All studies used indirect detection methods of medication adherence except for one, which additionally used a direct measure [26]. Multiple indirect methods were used to measure medication adherence: self-report scales [21,22,23,24,25,26,27,28,30,31,32,33,35,36,39,40,41], pill count [21,23,24,37], pharmacy refill records [24,34,42], and MEMS [24,38]. Among the thirteen different self-report scales used in the included studies, the Morisky Medication Adherence Scale (MMAS) [21,22,23,24,25,26,27,40] and the Medication Adherence Report Scale (MARS-5) [31,41] were the most frequently used (Table 2). Three studies adopted a mix of self-report and pill count [21,23] or self-report, pill count and pharmacy refill data [24].
3.6. Effects on Medication Adherence
Only four studies [21,30,35,41] highlighted a statistically significant increase in medication adherence using face-to-face visits plus telephone follow-up (Table 2). However, five studies found that face-to-face visits alone were statistically significant [23,25,27,36,40]. Among the face-to-face interventions, a statistically significant improvement in medication adherence was found in three studies, including patients with heart failure [23,30,40], two with multimorbidity [36,41], two with hypertension [27,35], one with coronary disease [21], and one with chronic myeloid leukemia [25].
Of the six studies offering a remote delivery intervention [22,31,32,38,39,42], only the study by Hsieh et al. [32] found a statistically significant improvement in medication adherence. In one study, no statistically significant differences were found between tablet computer-based patient education and one nurse educational session [26].
3.7. Effect of Nurse-Led Interventions on Other Outcomes
The nurse-led intervention also impacted other outcomes, such as mortality (OR 0.37, 95% CI = 0.154–0.892, p = 0.027) [33], hospital readmission (I = 10.4% C = 27.1% p 0.036; I = 6.38% C = 23.91% p = 0.038; 8.0% vs. 5.2% per person-week; OR 0.406; 95% CI 0.178–0.926; p = 0.03) [30,32,40,42], urgent care (OR = 0.388, 95% CI = 0.183–0.822, p = 0.013) [33], and systolic blood pressure, with a reduction ranging from 3 mmHg to 19 mmHg [27,29,35,36,37].
3.8. The Methodological Quality of the Included Studies
The quality of the studies was suboptimal: out of 22 studies, 1 was at low risk, 15 showed some concerns, and 6 were at high risk of bias (Figure 2). Although all studies were randomized controlled trials, only nine detailed the allocation concealment process [21,26,28,29,32,35,36,37,41]. Bias due to missing outcome data was of concern in ten studies [21,22,24,28,31,33,37,38,39,41]. Sixteen studies showed some concern or a high risk of bias in the measurement of the outcome [22,23,24,25,27,29,30,31,32,33,34,35,37,40,41,42]. This was due to a lack of validated measurement methods for the outcome and a lack of blindness that may have caused a recall or a social desirability bias and a self-report bias.

Figure 2.
Bias assessment of the selected studies. Symbols and colours represent the risk-of-bias assessment for individual studies: “+” (green) indicates low risk of bias, “!” (yellow) indicates unclear risk of bias, and “-“ (red) indicates high risk of bias.
4. Discussion
This systematic review aimed to synthesize the evidence on the effectiveness of nurse-led interventions that set out to improve medication adherence in adults with chronic conditions. The evidence of effectiveness presented in this systematic review was mixed and inconsistent, probably due to the different chronic conditions and medication adherence measurement methods, making comparing results challenging. Similarly, significant variability in data presentation was found in a previous systematic review conducted on nurse-led interventions [5]. Due to this heterogeneity, it was not possible to perform a meta-analysis.
Substantial differences in intervention conditions (such as type, frequency, duration, medication, adherence measures, and outcome composition) contributed to high heterogeneity. Other systematic reviews of adherence interventions have also noted this limitation [3,5,6,11]. Adherence is prevalently measured with indirect methods. This, in combination with the use of thirteen different questionnaires to detect medication adherence, makes comparability between studies challenging. The use of self-report questionnaires could also overestimate the impact of interventions [3]. While patient perspectives are important for enhancing patient empowerment in managing drug therapy and maintaining adherence, combining subjective data with objective measures using alternative methods of measuring medication adherence would be appropriate [43].
In our review, three studies used a combination of self-report questionnaires with objective measures such as pill counts, MEMS, and pharmacy refill data [21,24,37]. Employing a combined objective and subjective approach to measuring adherence could strengthen results, but methods like pill counts and MEMS have limitations. Pill counts require patients to return containers with unused medication and can be easily manipulated by patients overestimating their drug intake [5]. Additionally, pill counts only provide an estimate of adherence and do not offer insight into patients’ drug-taking behaviours [18]. Many studies used electronic monitoring with MEMS cups to generate objective data on the timing of medication intake by recording bottle cap openings, but this method does not confirm whether the patient actually took the medication [3]. Automated pharmacy refill data constitute another objective measure that ensures patient and provider blinding but does not provide information on patient behaviours [3]. The wide range of methods used to measure medication adherence is a well-known issue, as there is still no consensus on the best approach [3].
Our results are coherent with other systematic reviews conducted on people with multimorbidity, highlighting the potential role of nurse-led intervention in improving medication adherence [5,44]. Among all the considered interventions, slight medication adherence improvements were observed in face-to-face nurse-led visits [23,35,36,41]. The structure of nurse-led face-to-face interventions is complex and multi-component. In fact, different resources for educational sessions of the included studies were involved (i.e., verbal education, written material, technological support), increasing the knowledge and awareness of patients on the importance of medication adherence. During these educational sessions, nurses adopted motivational techniques to assist patients in changing negative behaviours and beliefs regarding medications and addressing patient doubts and concerns [36,41].
Patient motivation is a key factor in medication adherence, reflecting the patient’s willingness to modify behaviours and thoughts. Motivational interviewing involves a collaborative effort between the healthcare professional and the patient to identify goals that will be pursued and guide future sessions [45]. Implementing an individualized plan tailored to the patient’s specific needs [23,35,36,41] was frequently adopted to set specific goals with patients, focusing on lifestyle modifications and the effectiveness of treatments and their side effects. A systematic review focusing on cardiovascular patients indicates that motivational interviewing is a promising intervention for nurses to enhance medication adherence by improving patient capabilities, confidence, and motivation to achieve mutually agreed-upon goals [7]. A meta-analysis examining the effectiveness of motivational interviewing interventions on medication adherence in adults with chronic diseases found a positive effect, albeit small [46].
Furthermore, the motivational approach is one of the most common strategies used to promote patient self-management for people with chronic diseases in primary care [47]. The few nurse-led face-to-face educational interventions were designed to enhance understanding of the disease, provide self-care management measures and promote lifestyle modification strategy [23,41]. Self-management education and support (SMES) programmes are recommended to enhance the quality of life of individuals with chronic conditions and guide their health-related decisions and activities [47]. Nurses were the main healthcare professionals involved in the SMES programmes, playing a key role in promoting self-management [47].
Since medication adherence is a life-long phenomenon in people with chronic diseases, one might assume that nurse-led interventions aimed at improving medication adherence should be of a long duration; otherwise, their efficacy could be lost. In our review, medication adherence tends to be higher at the conclusion of the intervention and declines once the intervention is terminated [36,41], highlighting the benefits of maintaining constant follow-up over time [48]. However, the optimal duration, frequency and follow-up of nurse-led interventions still remain unclear. In our systematic review, a few studies had short follow-up periods, and their long-term efficacy should be further explored [32,41]. As adherence is an ongoing process for individuals with chronic conditions, this would suggest that medication adherence requires consistent monitoring and evaluation over time. However, a recent and unrelated study assessed the maintenance of effectiveness of a lifestyle counselling intervention over five years aimed at reducing blood pressure. While the intervention was effective at year one, its effectiveness waned after the educational intervention was discontinued following the final follow-up at the end of this year [49]. Evidence suggests that involving patients and making them partners in care has the potential to improve health outcomes and enhance healthy behaviours [50].
In our systematic review, an important factor found to influence medication adherence was the support of family members and caregivers in managing therapy and in recognizing and managing signs and symptoms [23,35]. In accordance with this, a meta-analysis revealed that social support from families, friends, and healthcare professionals was significantly linked to medication adherence [51]. Exploring the family context and living arrangements might therefore enhance medication adherence and identify other factors that may impact it or other healthcare needs. Socioeconomic conditions may also play a role in medication adherence, but neither our studies nor previous reviews have considered them as influencing factors [8].
Besides the support of family members, one study showed the effectiveness of nurse-led group educational interventions with patients with the same disease [35]. Currently, there is insufficient evidence to determine whether combining group and individual educational interventions is more effective [52]. Nevertheless, this creates an opportunity to consider educating more patients simultaneously and encourage relational exchange and sharing of self-management strategies.
Our results showed that most interventions improving medication adherence occurred in primary care settings [35,36,41], whereas only one intervention started at the patient’s discharge [23]. Interventions initiated at the hospital community level may be most likely to influence medication adherence [4]. Establishing a link between the hospital and primary care would be beneficial for maintaining continuity of care for patients. The primary care outpatient clinic, which deals with patients who are not hospitalized and, therefore, more clinically stable, should also provide more dedicated time to conduct a thorough care assessment of patients [53]. Involving nurses in advanced roles is a recognized way to optimize healthcare resources and increase quality of care. It is believed that the inclusion of nurses in a pivotal role can ensure that the demand for healthcare services that meet the needs of patients is adequately met [54]. Organizations such as the World Health Organization (WHO) have made several recommendations on how to strengthen the role of nurses (WHO 2012), and policy makers believe that in order to meet the challenges of hospitals and primary care, a more structured workforce in healthcare is required [55]. Nurse-led interventions lead to better health outcomes for a wide range of patient conditions, and the empowerment of the nursing role is vital and essential in the management of chronic diseases. With regard to the effects on clinical practice, despite the large heterogeneity of inventions, this study provides a wide view of nurse-led educational interventions that nurses could carry out both in community and hospital care. Practical implications for health systems and policy makers could be the integration of nurses-led clinics for the management of chronic diseases. The burden of complex and chronic diseases is increasing and requires expert nurses and financial resources to manage chronic and multimorbid patients properly. Nurse-led clinics could ensure the management of people with chronic diseases and help identify patients with unmet needs or complications early, giving appropriate care for patients and reducing pressure on the health system. Nurse-led clinics could represent a bridge between the hospital and the community and ensure continuity of care after discharge.
The benefits of nurse-led face-to-face intervention could be enhanced by using instant messaging services or web support to improve medication adherence. Despite advancements in technology, these benefits remain unclear due to limited evidence, with only two studies showing efficacy available in our review [32,35]. Instant messaging services could be used to communicate with health professionals at an early stage. However, they should be followed by a telephone call or, ideally, an in-person meeting to address any issues. A Cochrane review found insufficient evidence regarding the effectiveness of mobile text messaging and internet-based interventions in promoting medication adherence [3].
Almost half of the studies observed a statistically significant improvement in medication adherence. However, it is still unclear whether variations in adherence scores in the scales used correspond to a real change in patient medication adherence [23,32,35,36,41]. In fact, although statistically significant, the differences in the adherence scores are minimal and do not meet the thresholds set by each scale for enhancing medication adherence. We observed, respectively, an increase of 5 points on a scale of 60 to 110 [35], 3 points on a scale of 5 to 25 [41], 1 point on a scale of 0 to 13 [36], and 1 point on a scale of 0 to 10 [32]. One study observed an improvement in adherence levels from low to medium, specifically focusing on patients who were considered poorly adherent [23]. The variation in adherence cut-offs and the lack of baseline measurements across studies do not allow a clear understanding of the effects of nurse-led intervention on medication adherence [21,27,30,40]. Additionally, in four studies, medication adherence increased in both the intervention and control groups, further complicating the attribution of the effectiveness to the interventions proposed [23,32,36,41].
Beyond the scale scores, it is important to consider adherence in conjunction with other clinical outcomes to maximize the clinical benefits of interventions. Studies that solely focus on adherence may not provide conclusive evidence of patient improvement. Indeed, changes in medication adherence alone may not necessarily reflect changes in other clinical outcomes, such as blood pressure, which could be influenced by various factors, including lifestyle changes. Similarly, studies that solely focus on clinical outcomes may not accurately assess the importance of adherence in achieving these outcomes [3]. According to Cochrane researchers, studies evaluating medication adherence should also assess the intervention’s impact on clinical outcomes to determine its true effectiveness [3].
In our review, while changes in adherence scores do not evidently support an improvement in medication adherence [23,32,35,36,41], the nurse-led intervention had a positive impact on blood pressure values [35,36]. However, these improvements only result in clinically relevant reductions in cardiovascular risk, defined as a reduction of 10 mmHg and 5 mmHg in systolic and diastolic blood pressure [56], respectively. In our systematic review, only one study achieved this goal, even if it had a small sample size [35].
4.1. Limitations
This review has several limitations. Firstly, we only included articles written in English. Secondly, the quality of reporting in some studies is poor, complicating the quality assessment. Thirdly, the sample size of studies included in the review varies greatly. Most of the included studies were relatively small, with the exception of two studies involving a larger number of participants [31,37]. Relatively small studies are more susceptible to bias. Fourthly, the description of the control groups was often inadequate. Many studies reported that the control group received standard care without providing detailed descriptions of the interventions, making it difficult to evaluate effectiveness. Additionally, in cases where standard care was already of good quality, improvements in medication adherence might not be observed. Many studies also lack sufficient details of the intervention, making it challenging to understand its effectiveness, application, and usefulness in other contexts. A further limitation of this review is the evaluation of the short-term effect of the nurse-led intervention, with only three studies having a 12-month follow-up period [23,35,36]. The heterogeneity in nurse-led interventions and outcome measurement meant that undertaking a meta-analysis was not possible; this could be considered a further limitation. Finally, the most widely used instrument for measuring adherence was the MMAS, in both older and updated versions. However, the validity of this scale has recently been questioned, discouraging its future use [57].
4.2. Risk-of-Bias Assessment and Interpretation
The evidence presented in this review should be interpreted with caution. The overall quality of the studies included is suboptimal, encouraging higher-quality research with a high methodological rigour that could identify the real effect of nurse-led interventions on clinically relevant outcomes. The efficacy of face-to-face interventions should be carefully appraised. In fact, excluding studies with a high risk of bias, only a minority of studies [23,26,35,41] with low risk of bias or some concern suggest that nurse-led face-to-face intervention could slightly improve medication adherence in chronic conditions, limited to cardiovascular and metabolic diseases. For these reasons, larger studies with long-term follow-up are needed. Considering the times of staff shortages, maximizing resources becomes even more important for health organizations.
We would expect that nurse-led interventions need to be maintained for as long as the treatment is needed, integrating these in healthcare systems in a feasible and sustainable way. Investments in face-to-face interventions should be considered against the dedicated time required and the presence of highly competent nurses.
In regarding the quality of evidence carefully, RoB2’s most problematic domains were the first, the third, and the fourth. Specifically, thirteen studies did not provide full detail on the randomization process and the concealment of the sequence generation (domain 1). This may be due to limited word counts in journals and a lack of description of methods of randomization and allocation concealment, not necessarily meaning an inappropriate method. We carefully followed the RoB2 guidance and considered the presence of a central randomization as the minimum criterion for a judgement of adequate concealment of the allocation sequence. For future studies, a detailed description of the sequence generation is recommended to confirm the presence of a random component. The main reason for the negative impact on domain 3 assessment was the high percentage of studies with a consistent loss to follow-up of patients. According to the Rob2 guidance, we considered a proportion of less than 5% of the missing result data as “small”, which is considered small enough to exclude bias, and more than 20% as “large”. However, in all studies included in this systematic review, the author performed the recommended intention-to-treat analysis (ITT) to minimize this risk of bias. In addition, future studies could include sensitivity analyses to assess the potential impact of missing data. For domain 4, our assessment of the high risk of bias or some concern is due to the use of different questionnaires that have been not validated, and for this reason, they have a high probability of poor validity in detecting the outcome of interest. For future research, the use of validated questionnaires, possibly specific to the disease, must be encouraged to reduce this bias.
4.3. Implications for Research and Nursing Practice
Research on medication adherence is a critical component of healthcare that requires improvement in various areas. Current methods of measuring medication adherence may not accurately capture patient behaviour and medication consumption patterns. Consequently, this represents a research area that could be enhanced. New methods for detecting medication adherence need to be implemented, focusing on assessing patients’ cognitive, emotional, and socioeconomic perspectives. Investigating the psychological mechanisms underlying poor adherence and its maintenance is important. Measurement of medication adherence is a challenge due to its complexity and the multiple factors that could affect it. A common method of measuring medication adherence is through patient self-report questionnaires. While these measures are widely applicable and easy to implement, the use of available validated questionnaires, possibly disease-specific, must be encouraged. Questionnaires used to assess adherence are often tailored to a single disease or provide general questions that may not capture the concerns in patients with multimorbidity. Assessment tools should also consider patients’ priorities, such as factors hindering their medication adherence. Future research on medication adherence should incorporate the patient’s perspective through qualitative studies to better understand common problems and difficulties experienced. Studies should also consider patients’ baseline levels of adherence and identify those who could benefit most from nursing interventions. Additionally, despite the increasing prevalence and complexity of these cases, there is a lack of research on interventions to improve medication adherence in patients with multiple chronic conditions. While interprofessional collaboration is valuable, the role of nurses should not be underestimated. Nurses have a unique level of closeness with and understanding of their patients that can foster trust in and adherence to treatment plans. In a future perspective, nurses can influence the allocation of resources to support the healthcare system and reach better patient health outcomes by increasing their policy power through their clinical knowledge and closeness to patients [58].
5. Conclusions
Our findings highlight the necessity of a targeted, durable and based-on-trust interaction between people with one or more chronic diseases and nurses to support and improve medication adherence. Building a trusting patient–provider relationship is an opportunity to discuss patient beliefs and concerns about the efficacy and safety of medications prescribed. In order to reach shared decisions, it is therefore necessary to explore not only the medication knowledge but also the psychosocial dimension of the patient. Nurses play a fundamental role in screening, assessing and supporting medication adherence and could coordinate the treatment initiation and future management.
The patient’s education is part of the nursing scope of practice that can be carried out through various techniques, including motivational interviewing, structured interviews, and assessment of care needs. Finally, technology provides valuable support for human actions but cannot be a substitute for them. Relationships and human interaction are still the main vehicles for educating and supporting people. A key element of improving health services is increasing nurses’ opportunities and capacities to participate in policymaking activities and subsequently manage chronic diseases.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/healthcare12232337/s1, File S1. Original and Updated Search Strategies.
Author Contributions
Conceptualization, D.B., A.C. and S.C.; methodology, D.B., A.C. and S.C.; software, D.B. and A.C.; validation, S.C. and V.D.; formal analysis, D.B., A.C., E.C. and A.H.; investigation, D.B., A.C. and S.C.; resources, B.M.; data curation, D.B., A.C. and E.C.; writing—original draft preparation, D.B., A.C., E.C. and S.C.; writing—review and editing, S.C and V.D.; visualization, V.D.; supervision, S.C. and V.D.; project administration, D.B., S.C. and V.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We wish to thank Allison Finch for her valuable assistance with the English review and proofreading of this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- PAHO/WHO. Adherence to Long-Term Therapies: Evidence for Action. 2003. Available online: https://www.paho.org/en/documents/who-adherence-long-term-therapies-evidence-action-2003 (accessed on 10 October 2023).
- NICE. Overview. Medicines Adherence: Involving Patients in Decisions about Prescribed Medicines and Supporting Adherence. Guidance. Available online: https://www.nice.org.uk/guidance/cg76 (accessed on 16 May 2024).
- Nieuwlaat, R.; Wilczynski, N.; Navarro, T.; Hobson, N.; Jeffery, R.; Keepanasseril, A.; Agoritsas, T.; Mistry, N.; Iorio, A.; Jack, S.; et al. Interventions for Enhancing Medication Adherence. Cochrane Database Syst. Rev. 2014, 2014, CD000011. [Google Scholar] [CrossRef] [PubMed]
- Cross, A.J.; Elliott, R.A.; Petrie, K.; Kuruvilla, L.; George, J. Interventions for Improving Medication-Taking Ability and Adherence in Older Adults Prescribed Multiple Medications. Cochrane Database Syst. Rev. 2020, 5, CD012419. [Google Scholar] [CrossRef]
- Van Camp, Y.P.; Van Rompaey, B.; Elseviers, M.M. Nurse-Led Interventions to Enhance Adherence to Chronic Medication: Systematic Review and Meta-Analysis of Randomised Controlled Trials. Eur. J. Clin. Pharmacol. 2013, 69, 761–770. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Zhu, S.; Lee, D.T.F.; Chair, S.Y. Interventions for Improving Medication Adherence in Community-Dwelling Older People with Multimorbidity: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2022, 126, 104154. [Google Scholar] [CrossRef] [PubMed]
- Al-Ganmi, A.H.; Perry, L.; Gholizadeh, L.; Alotaibi, A.M. Cardiovascular Medication Adherence among Patients with Cardiac Disease: A Systematic Review. J. Adv. Nurs. 2016, 72, 3001–3014. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, K.J.; Roberts, M.E.; Neiheisel, M.B. Medication Adherence Part Two: Predictors of Nonadherence and Adherence. J. Am. Assoc. Nurse Pract. 2014, 26, 225–232. [Google Scholar] [CrossRef]
- Cole, J.A.; Gonçalves-Bradley, D.C.; Alqahtani, M.; Barry, H.E.; Cadogan, C.; Rankin, A.; Patterson, S.M.; Kerse, N.; Cardwell, C.R.; Ryan, C.; et al. Interventions to Improve the Appropriate Use of Polypharmacy for Older People. Cochrane Database Syst. Rev. 2023, 10, CD008165. [Google Scholar] [CrossRef]
- Balikai, S.I.; Rentala, S.; Mudakavi, I.B.; Nayak, R.B. Impact of Nurse-Led Medication Adherence Therapy on Bipolar Affective Disorder: A Randomized Controlled Trial. Perspect. Psychiatr. Care 2022, 58, 2676–2686. [Google Scholar] [CrossRef]
- Verloo, H.; Chiolero, A.; Kiszio, B.; Kampel, T.; Santschi, V. Nurse Interventions to Improve Medication Adherence among Discharged Older Adults: A Systematic Review. Age Ageing 2017, 46, 747–754. [Google Scholar] [CrossRef]
- WHO. Global Strategic Directions for Nursing and Midwifery 2021–2025, 1st ed.; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-003386-3. [Google Scholar]
- Scott, S.M.; Scott, P.A. Nursing, Advocacy and Public Policy. Nurs. Ethics 2021, 28, 723–733. [Google Scholar] [CrossRef]
- Inayat, S.; Younas, A.; Andleeb, S.; Rasheed, S.P.; Ali, P. Enhancing Nurses’ Involvement in Policy Making: A Qualitative Study of Nurse Leaders. Int. Nurs. Rev. 2023, 70, 297–306. [Google Scholar] [CrossRef]
- Celio, J.; Ninane, F.; Bugnon, O.; Schneider, M.P. Pharmacist-Nurse Collaborations in Medication Adherence-Enhancing Interventions: A Review. Patient Educ. Couns. 2018, 101, 1175–1192. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Neiheisel, M.B.; Wheeler, K.J.; Roberts, M.E. Medication Adherence Part One: Understanding and Assessing the Problem. J. Am. Assoc. Nurse Pract. 2014, 26, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Richards, J.; Hillsdon, M.; Thorogood, M.; Foster, C. Face-to-Face Interventions for Promoting Physical Activity. Cochrane Database Syst. Rev. 2013, 2013, CD010392. [Google Scholar] [CrossRef]
- Gordon, M.; Sinopoulou, V.; Lakunina, S.; Gjuladin-Hellon, T.; Bracewell, K.; Akobeng, A.K. Remote Care through Telehealth for People with Inflammatory Bowel Disease. Cochrane Database Syst. Rev. 2023, 5, CD014821. [Google Scholar] [CrossRef]
- Calvo, E.; Izquierdo, S.; Castillo, R.; César, E.; Domene, G.; Gómez, A.B.; Guerrero, C.; Andreu-Periz, L.; Gómez-Hospital, J.A.; Ariza-Solé, A. Can an Individualized Adherence Education Program Delivered by Nurses Improve Therapeutic Adherence in Elderly People with Acute Myocardial Infarction?: A Randomized Controlled Study. Int. J. Nurs. Stud. 2021, 120, 103975. [Google Scholar] [CrossRef]
- Gould, K.A. A Randomized Controlled Trial of a Discharge Nursing Intervention to Promote Self-Regulation of Care for Early Discharge Interventional Cardiology Patients. Dimens. Crit. Care Nurs. 2011, 30, 117–125. [Google Scholar] [CrossRef]
- Granger, B.B.; Ekman, I.; Hernandez, A.F.; Sawyer, T.; Bowers, M.T.; DeWald, T.A.; Zhao, Y.; Levy, J.; Bosworth, H.B. Results of the Chronic Heart Failure Intervention to Improve MEdication Adherence Study: A Randomized Intervention in High-Risk Patients. Am. Heart J. 2015, 169, 539–548. [Google Scholar] [CrossRef]
- Holzemer, W.L.; Bakken, S.; Portillo, C.J.; Grimes, R.; Welch, J.; Wantland, D.; Mullan, J.T. Testing a Nurse-Tailored HIV Medication Adherence Intervention. Nurs. Res. 2006, 55, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Kekäle, M.; Söderlund, T.; Koskenvesa, P.; Talvensaari, K.; Airaksinen, M. Impact of Tailored Patient Education on Adherence of Patients with Chronic Myeloid Leukaemia to Tyrosine Kinase Inhibitors: A Randomized Multicentre Intervention Study. J. Adv. Nurs. 2016, 72, 2196–2206. [Google Scholar] [CrossRef] [PubMed]
- Suhling, H.; Rademacher, J.; Zinowsky, I.; Fuge, J.; Greer, M.; Warnecke, G.; Smits, J.M.; Bertram, A.; Haverich, A.; Welte, T.; et al. Conventional vs. Tablet Computer-Based Patient Education Following Lung Transplantation—A Randomized Controlled Trial. PLoS ONE 2014, 9, e90828. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Guo, L.; Mao, J.; Qi, X.; Chen, L.; Huang, H.; Sun, Y.; Yang, X. The Effects of Nursing of Roy Adaptation Model on the Elderly Hypertensive: A Randomised Control Study. Ann. Palliat. Med. 2021, 10, 12149–12158. [Google Scholar] [CrossRef] [PubMed]
- Arruda, C.S.; de Melo Vellozo Pereira, J.; da Silva Figueiredo, L.; Scofano, B.D.S.; Flores, P.V.P.; Cavalcanti, A.C.D. Effect of an Orientation Group for Patients with Chronic Heart Failure: Randomized Controlled Trial. Rev. Lat. Am. Enfermagem 2018, 25, e2982. [Google Scholar] [CrossRef][Green Version]
- Chiu, C.W.; Wong, F.K.Y. Effects of 8 Weeks Sustained Follow-up after a Nurse Consultation on Hypertension: A Randomised Trial. Int. J. Nurs. Stud. 2010, 47, 1374–1382. [Google Scholar] [CrossRef]
- Cui, X.; Zhou, X.; Ma, L.; Sun, T.-W.; Bishop, L.; Gardiner, F.W.; Wang, L. A Nurse-Led Structured Education Program Improves Self-Management Skills and Reduces Hospital Readmissions in Patients with Chronic Heart Failure: A Randomized and Controlled Trial in China. Rural Remote Health 2019, 19, 5270. [Google Scholar] [CrossRef]
- Dwinger, S.; Rezvani, F.; Kriston, L.; Herbarth, L.; Härter, M.; Dirmaier, J. Effects of Telephone-Based Health Coaching on Patient-Reported Outcomes and Health Behavior Change: A Randomized Controlled Trial. PLoS ONE 2020, 15, e0236861. [Google Scholar] [CrossRef]
- Hsieh, H.-L.; Kao, C.-W.; Cheng, S.-M.; Chang, Y.-C. A Web-Based Integrated Management Program for Improving Medication Adherence and Quality of Life, and Reducing Readmission in Patients With Atrial Fibrillation: Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e30107. [Google Scholar] [CrossRef]
- Liang, H.Y.; Hann Lin, L.; Yu Chang, C.; Mei Wu, F.; Yu, S. Effectiveness of a Nurse-Led Tele-Homecare Program for Patients With Multiple Chronic Illnesses and a High Risk for Readmission: A Randomized Controlled Trial. J. Nurs. Scholarsh. 2021, 53, 161–170. [Google Scholar] [CrossRef]
- Lin, E.H.B.; Von Korff, M.; Ciechanowski, P.; Peterson, D.; Ludman, E.J.; Rutter, C.M.; Oliver, M.; Young, B.A.; Gensichen, J.; McGregor, M.; et al. Treatment Adjustment and Medication Adherence for Complex Patients with Diabetes, Heart Disease, and Depression: A Randomized Controlled Trial. Ann. Fam. Med. 2012, 10, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Mattei da Silva, Â.T.; de Fátima Mantovani, M.; Castanho Moreira, R.; Perez Arthur, J.; Molina de Souza, R. Nursing Case Management for People with Hypertension in Primary Health Care: A Randomized Controlled Trial. Res. Nurs. Health 2020, 43, 68–78. [Google Scholar] [CrossRef]
- Parra, D.I.; Guevara, S.L.R.; Rojas, L.Z. “Teaching: Individual” to Improve Adherence in Hypertension and Type 2 Diabetes. Br. J. Community Nurs. 2021, 26, 84–91. [Google Scholar] [CrossRef]
- Persell, S.D.; Karmali, K.N.; Lazar, D.; Friesema, E.M.; Lee, J.Y.; Rademaker, A.; Kaiser, D.; Eder, M.; French, D.D.; Brown, T.; et al. Effect of Electronic Health Record-Based Medication Support and Nurse-Led Medication Therapy Management on Hypertension and Medication Self-Management: A Randomized Clinical Trial. JAMA Intern. Med. 2018, 178, 1069–1077. [Google Scholar] [CrossRef]
- Tessier, A.; Dupuy, M.; Baylé, F.J.; Herse, C.; Lange, A.-C.; Vrijens, B.; Schweitzer, P.; Swendsen, J.; Misdrahi, D. Brief Interventions for Improving Adherence in Schizophrenia: A Pilot Study Using Electronic Medication Event Monitoring. Psychiatry Res. 2020, 285, 112780. [Google Scholar] [CrossRef]
- Wong, F.K.Y.; Chow, S.K.Y.; Chan, T.M.F. Evaluation of a Nurse-Led Disease Management Programme for Chronic Kidney Disease: A Randomized Controlled Trial. Int. J. Nurs. Stud. 2010, 47, 268–278. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Yu, Y.; Xu, H. Influence of Targeted Motivational Interviewing on Self-Care Level and Prognosis during Nursing Care of Chronic Heart Failure. Am. J. Transl. Res. 2021, 13, 6576–6583. [Google Scholar] [PubMed]
- Yang, C.; Lee, D.T.F.; Wang, X.; Chair, S.Y. Effects of a Nurse-Led Medication Self-Management Intervention on Medication Adherence and Health Outcomes in Older People with Multimorbidity: A Randomised Controlled Trial. Int. J. Nurs. Stud. 2022, 134, 104314. [Google Scholar] [CrossRef] [PubMed]
- You, J.; Wang, S.; Li, J.; Luo, Y. Usefulness of a Nurse-Led Program of Care for Management of Patients with Chronic Heart Failure. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020, 26, e920469. [Google Scholar] [CrossRef]
- Jácome, C.; Pereira, A.M.; Almeida, R.; Ferreira-Magalhaes, M.; Couto, M.; Araujo, L.; Pereira, M.; Correia, M.A.; Loureiro, C.C.; Catarata, M.J.; et al. Patient-Physician Discordance in Assessment of Adherence to Inhaled Controller Medication: A Cross-Sectional Analysis of Two Cohorts. BMJ Open 2019, 9, e031732. [Google Scholar] [CrossRef]
- McParland, C.; Johnston, B.; Cooper, M. A Mixed-Methods Systematic Review of Nurse-Led Interventions for People with Multimorbidity. J. Adv. Nurs. 2022, 78, 3930–3951. [Google Scholar] [CrossRef] [PubMed]
- Temedda, M.N.; Haesebaert, J.; Viprey, M.; Schott, A.M.; Dima, A.L.; Papus, M.; Schneider, M.P.; Novais, T. Motivational Interviewing to Support Medication Adherence in Older Patients: Barriers and Facilitators for Implementing in Hospital Setting According to Healthcare Professionals. Patient Educ. Couns. 2024, 124, 108253. [Google Scholar] [CrossRef] [PubMed]
- Zomahoun, H.T.V.; Guénette, L.; Grégoire, J.-P.; Lauzier, S.; Lawani, A.M.; Ferdynus, C.; Huiart, L.; Moisan, J. Effectiveness of Motivational Interviewing Interventions on Medication Adherence in Adults with Chronic Diseases: A Systematic Review and Meta-Analysis. Int. J. Epidemiol. 2017, 46, 589–602. [Google Scholar] [CrossRef]
- Allory, E.; Scheer, J.; De Andrade, V.; Garlantézec, R.; Gagnayre, R. Characteristics of Self-Management Education and Support Programmes for People with Chronic Diseases Delivered by Primary Care Teams: A Rapid Review. BMC Prim. Care 2024, 25, 46. [Google Scholar] [CrossRef]
- Chang, L.L.; Xu, H.; DeVore, A.D.; Matsouaka, R.A.; Yancy, C.W.; Fonarow, G.C.; Allen, L.A.; Hernandez, A.F. Timing of Postdischarge Follow-Up and Medication Adherence Among Patients With Heart Failure. J. Am. Heart Assoc. 2018, 7, e007998. [Google Scholar] [CrossRef]
- Thapa, R.; Zengin, A.; Neupane, D.; Mishra, S.R.; Koirala, S.; Kallestrup, P.; Thrift, A.G. Sustainability of a 12-Month Lifestyle Intervention Delivered by Community Health Workers in Reducing Blood Pressure in Nepal: 5-Year Follow-up of the COBIN Open-Label, Cluster Randomised Trial. Lancet Glob. Health 2023, 11, e1086–e1095. [Google Scholar] [CrossRef]
- Menichetti, J.; Graffigna, G. “PHE in Action”: Development and Modeling of an Intervention to Improve Patient Engagement among Older Adults. Front. Psychol. 2016, 7, 1405. [Google Scholar] [CrossRef]
- Magrin, M.E.; D’Addario, M.; Greco, A.; Miglioretti, M.; Sarini, M.; Scrignaro, M.; Steca, P.; Vecchio, L.; Crocetti, E. Social Support and Adherence to Treatment in Hypertensive Patients: A Meta-Analysis. Ann. Behav. Med. Publ. Soc. Behav. Med. 2015, 49, 307–318. [Google Scholar] [CrossRef] [PubMed]
- Nikolaus, S.; Schreiber, S.; Siegmund, B.; Bokemeyer, B.; Bästlein, E.; Bachmann, O.; Görlich, D.; Hofmann, U.; Schwab, M.; Kruis, W. Patient Education in a 14-Month Randomised Trial Fails to Improve Adherence in Ulcerative Colitis: Influence of Demographic and Clinical Parameters on Non-Adherence. J. Crohns Colitis 2017, 11, 1052–1062. [Google Scholar] [CrossRef]
- Baecker, A.; Meyers, M.; Koyama, S.; Taitano, M.; Watson, H.; Machado, M.; Nguyen, H.Q. Evaluation of a Transitional Care Program After Hospitalization for Heart Failure in an Integrated Health Care System. JAMA Netw. Open 2020, 3, e2027410. [Google Scholar] [CrossRef]
- Laurant, M.; van der Biezen, M.; Wijers, N.; Watananirun, K.; Kontopantelis, E.; van Vught, A.J. Nurses as substitutes for doctors in primary care. Cochrane Database Syst. Rev. 2018, 7, CD001271. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Recommendations: Optimizing Health Worker Roles to Improve Access to Key Maternal and Newborn Health Interventions Through Task Shifting—OPTIMIZEMNH; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Law, M.R.; Morris, J.K.; Wald, N.J. Use of Blood Pressure Lowering Drugs in the Prevention of Cardiovascular Disease: Meta-Analysis of 147 Randomised Trials in the Context of Expectations from Prospective Epidemiological Studies. BMJ 2009, 338, b1665. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.J.; Lee, W.Y.; Hwang, J.S.; Hong, Y.P.; Morisky, D.E. Accuracy of a screening tool for medication adherence: A systematic review and meta-analysis of the Morisky Medication Adherence Scale-8. PLoS ONE 2017, 12, e0187139. [Google Scholar] [CrossRef]
- Rasheed, S.P.; Younas, A.; Mehdi, F. Challenges, Extent of Involvement, and the Impact of Nurses’ Involvement in Politics and Policy Making in in Last Two Decades: An Integrative Review. J. Nurs. Scholarsh. 2020, 52, 446–455. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).