Cannabinoids in the Older Person: A Literature Review
Abstract
:1. Introduction
2. Background
3. Aims
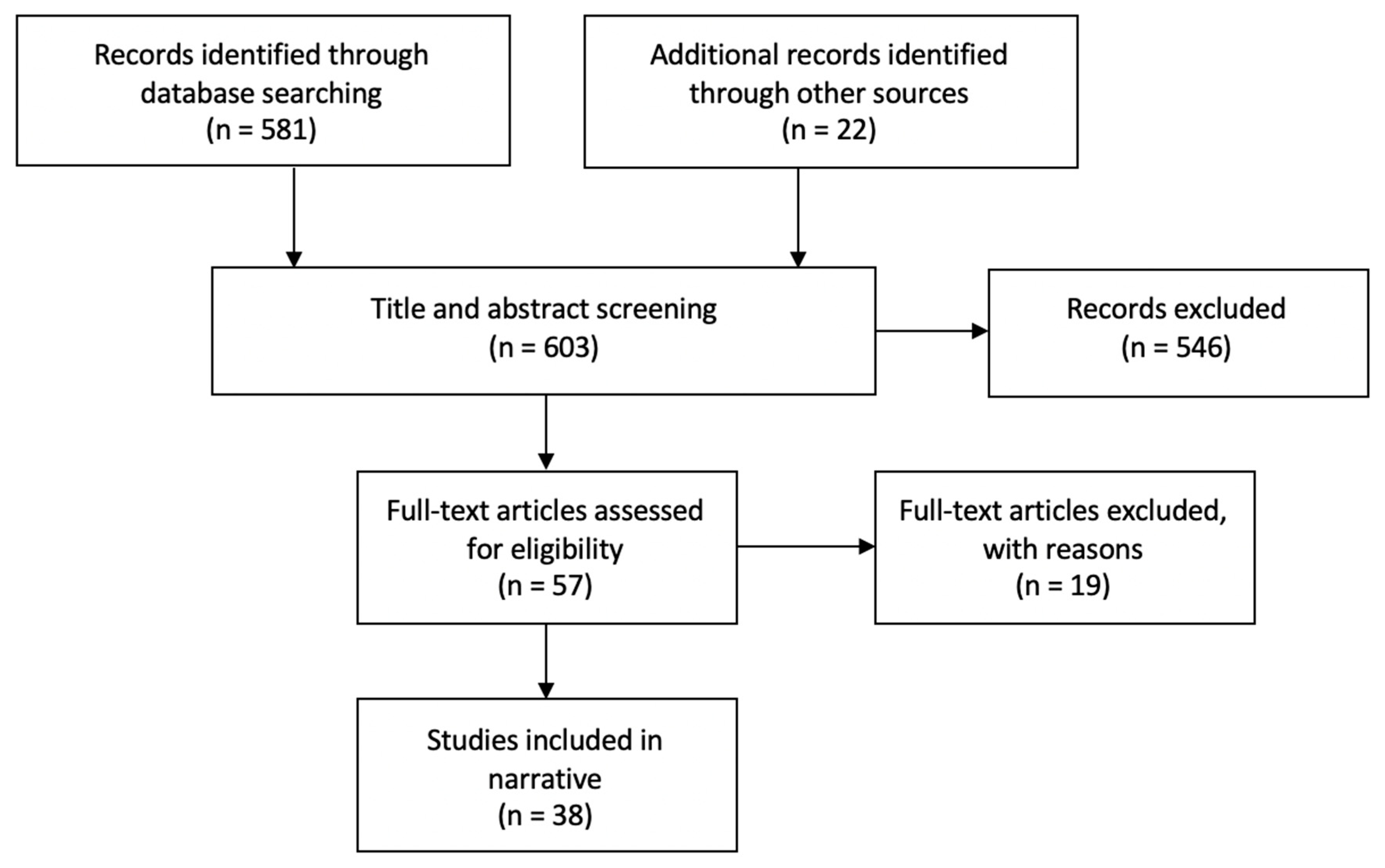
4. Methods
5. Results
6. Potential Indications for Medicinal Cannabinoids in the Older Person
7. Pain
7.1. Smoked Cannabis
7.2. Nabilone
7.3. Dronabinol
7.4. Nabiximols
8. Chemotherapy Related Nausea
9. Spasticity
10. Appetite Stimulation
11. Behavioral Problems in Dementia
12. Anxiety
13. Movement Disorders
14. Potential Hazards of Medical Cannabinoids in Older Adults
14.1. Smoked Cannabis
14.2. Nabilone
14.3. Dronabinol
14.4. Nabiximols
15. Safety and Adverse Effects
16. Medication Interaction
17. Long Term Safety
18. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Department of Health. An Introduction to the Biochemistry & Pharmacology of Medical Cannabis; District of Columbia, Government of District of Columbia Department of Health: Washington, DC, USA, 2019. Available online: https://doh.dc.gov/sites/default/files/dc/sites/doh/publication/attachments/Medical%20Cannabis%20An%20Introduction%20to%20the%20Biochemistry%20and%20Pharmacology.pdf (accessed on 6 June 2019).
- Burstein, S. Cannabidiol (CBD) and its analogues: A review of their effects on inflammation. Bioorg. Med. Chem. 2015, 23, 1377–1385. Available online: https://www.researchgate.net/publication/272373349_Cannabidiol_CBD_and_its_analogs_A_review_of_their_effects_on_inflammation (accessed on 9 May 2019). [CrossRef] [PubMed]
- Hillig, K.; Mahlberg, P. A chemotaxonomic analysis of cannabinoid variation in Cannabis (Cannabaceae). Am. J. Bot. 2004, 91, 966–975. Available online: https://bsapubs.onlinelibrary.wiley.com/doi/full/10.3732/ajb.91.6.966 (accessed on 6 June 2019). [CrossRef] [PubMed] [Green Version]
- Rom, S.; Persidsky, Y. Cannabinoid Receptor 2: Potential Role in Immunomodulation and Neuroinflammation. J. Neuroimmune Pharmacol. 2013, 8, 608–620. Available online: https://link.springer.com/article/10.1007%2Fs11481-013-9445-9 (accessed on 6 May 2019). [CrossRef] [PubMed] [Green Version]
- Van der Stelt, M.; Di Marzo, V. Cannabinoid Receptors and Their Role in Neuroprotection. Neuromol. Med. 2005, 7, 37–50. Available online: https://link.springer.com/article/10.1385%2FNMM%3A7%3A1-2%3A037 (accessed on 4 May 2019). [CrossRef]
- High-Strength Skunk ‘Now Dominates’ UK Cannabis Market [Internet]. NHS, 2018. Available online: https://www.nhs.uk/news/mental-health/high-strength-skunk-now-dominates-uk-cannabis-market/ (accessed on 11 May 2019).
- Minerbi, A.; Häuser, W.; Fitzcharles, M. Medical Cannabis for Older Patients. Drugs Aging 2019, 36, 39–51. [Google Scholar] [CrossRef] [PubMed]
- Adili, A.; Busse, J.; Ashoorion, V. Cannabinoids vs. Placebo on Persistent Post-surgical Pain Following TKA: A Pilot RCT. 2019. Available online: https://clinicaltrials.gov/ct2/show/NCT03825965 (accessed on 2 January 2020).
- Van Den Elsen, G.; Ahmed, A.; Verkes, R.; Kramers, C.; Feuth, T.; Rosenberg, P.; Van Der Marck, M.A.; Rikkert, M.G.M. OldeTetrahydrocannabinol for neuropsychiatric symptoms in dementia: A randomised controlled trial. Neurology 2019, 84, 2338–2346. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4464746/ (accessed on 4 May 2019). [CrossRef] [Green Version]
- Beauchet, O. Medical cannabis use in older patients: Update on medical knowledge. Maturitas 2018, 118, 56–59. [Google Scholar] [CrossRef]
- Abuhasira, R.; Schleider, L.; Mechoulam, R.; Novack, V. Epidemiological characteristics, safety and efficacy of medical cannabis in the elderly. Eur. J. Intern. Med. 2018, 49, 44–50. Available online: https://www.ejinme.com/article/S0953-6205(18)30019-0/fulltext (accessed on 4 May 2019). [CrossRef]
- Agornyo, P. Older adults’ use of medical marijuana for chronic pain: A multi-site community-based survey. In Proceedings of the American Geriatrics Society Annual Meeting, Orlando, FL, USA, 3–5 May 2018. [Google Scholar]
- Briscoe, J.; Casarett, D. Medical Marijuana Use in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 859–863. [Google Scholar] [CrossRef]
- Mücke, M.; Phillips, T.; Radbruch, L.; Petzke, F.; Häuser, W. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane Database Syst. Rev. 2018. [Google Scholar] [CrossRef]
- Torres-Moreno, M.; Papaseit, E.; Torrens, M.; Farré, M. Assessment of Efficacy and Tolerability of Medicinal Cannabinoids in Patients with Multiple Sclerosis. JAMA Netw. Open 2018, 1, e183485. Available online: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2706499 (accessed on 4 May 2019). [CrossRef] [PubMed] [Green Version]
- Grayson, L.; Vines, B.; Nichol, K.; Szaflarski, J. An interaction between warfarin and cannabidiol, a case report. Epilepsy Behav. Case Rep. 2018, 9, 10–11. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5789126/ (accessed on 3 May 2019). [CrossRef] [PubMed]
- Stockings, E.; Campbell, G.; Hall, W.; Nielsen, S.; Zagic, D.; Rahman, R.; Murnion, B.; Farrell, M.; Weier, M.; Degenhardt, L. Cannabis and cannabinoids for the treatment of people with chronic noncancer pain conditions. Pain 2018, 159, 1932–1954. [Google Scholar] [CrossRef] [PubMed]
- Mahvan, T.; Hilaire, M.; Mann, A.; Brown, A.; Linn, B.; Gardner, T.; Lai, B. Marijuana Use in the Elderly: Implications and Considerations. Consult. Pharm. 2017, 32, 341–351. [Google Scholar] [CrossRef] [PubMed]
- Katz, I.; Katz, D.; Shoenfield, Y.; Porat-Katz, B. Clinical Evidence for Utilizing Cannabinoids in the Elderly. Isr. Med. Assoc. J. 2017, 19, 71–75. [Google Scholar] [PubMed]
- Bellnier, T.; Brown, G.; Ortega, T. Preliminary evaluation of the efficacy, safety, and costs associated with the treatment of chronic pain with medical cannabis. Ment. Health Clin. 2017, 8, 110–115. [Google Scholar] [CrossRef]
- Hansra, D. Evaluation of safety, efficacy, and other clinical endpoints of delta-9-tetrahydrocannabinol in older patients with hem/onc malignancies. J. Clin. Oncol. 2017, 35 (Suppl. 15), e21671. [Google Scholar] [CrossRef]
- Schimrigk, S.; Marziniak, M.; Neubauer, C.; Kugler, E.; Werner, G.; Abramov-Sommariva, D. Dronabinol Is a Safe Long-Term Treatment Option for Neuropathic Pain Patients. Eur. Neurol. 2017, 78, 320–329. Available online: https://www.karger.com/Article/Pdf/481089 (accessed on 4 May 2019). [CrossRef]
- Lim, K.; See, Y.; Lee, J. A Systematic Review of the Effectiveness of Medical Cannabis for Psychiatric, Movement and Neurodegenerative Disorders. Clin. Psychopharmacol. Neurosci. 2017, 15, 301–312. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5678490/ (accessed on 4 May 2019). [CrossRef] [Green Version]
- Stampanoni Bassi, M.; Sancesario, A.; Morace, R.; Centonze, D.; Iezzi, E. Cannabinoids in Parkinson’s Disease. Cannabis Cannabinoid Res. 2017, 2, 21–29. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5436333/ (accessed on 12 May 2019). [CrossRef]
- Tafelski, S.; Häuser, W.; Schäfer, M. Efficacy, tolerability, and safety of cannabinoids for chemotherapy-induced nausea and vomiting—A systematic review of systematic reviews. Der Schmerz. 2016, 30, 14–24. Available online: https://link.springer.com/article/10.1007%2Fs00482-015-0092-3 (accessed on 2 May 2019). [CrossRef] [PubMed]
- Ahmed, A.; van den Elsen, G.; Colbers, A.; Kramers, C.; Burger, D.; van der Marck, M.; Rikkert, M.G.M.O. Safety, pharmacodynamics, and pharmacokinetics of multiple oral doses of delta-9-tetrahydrocannabinol in older persons with dementia. Psychopharmacology 2015, 232, 2587–2595. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4480847/ (accessed on 4 May 2019). [CrossRef] [PubMed] [Green Version]
- Smith, L.A.; Azariah, F.; Lavender, V.T.C.; Stoner, N.S.; Bettiol, S. Cannabinoids for nausea and vomiting in adults with cancer receiving chemotherapy. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, C.; Chau, S.; Ruthirakuhan, M.; Lanctôt, K.; Herrmann, N. Cannabinoids for the Treatment of Agitation and Aggression in Alzheimer’s Disease. CNS Drugs 2015, 29, 615–623. Available online: https://link.springer.com/article/10.1007%2Fs40263-015-0270-y (accessed on 4 May 2019). [CrossRef]
- Van den Elsen, G.; Ahmed, A.; Lammers, M.; Kramers, C.; Verkes, R.; van der Marck, M.; Rikkert, M.G.M.O. Efficacy and safety of medical cannabinoids in older subjects: A systematic review. Ageing Res. Rev. 2014, 14, 56–64. [Google Scholar] [CrossRef]
- Ahmed, A.; van den Elsen, G.; Colbers, A.; van der Marck, M.; Burger, D.; Feuth, T.; Rikkert, M.G.M.O.; Kramers, C. Safety and pharmacokinetics of oral delta-9-tetrahydrocannabinol in healthy older subjects: A randomized controlled trial. Eur. Neuropsychopharmacol. 2014, 24, 1475–1482. Available online: https://www.sciencedirect.com/science/article/abs/pii/S0924977X14001758?via%3Dihub (accessed on 5 May 2019). [CrossRef]
- Lotan, I.; Treves, T.; Roditi, Y.; Djaldetti, R. Cannabis (Medical Marijuana) Treatment for Motor and Non–Motor Symptoms of Parkinson Disease. Clin. Neuropharmacol. 2014, 37, 41–44. Available online: https://insights.ovid.com/article/00002826-201403000-00001 (accessed on 4 May 2019). [CrossRef]
- Chagas, M.; Zuardi, A.; Tumas, V.; Pena-Pereira, M.; Sobreira, E.; Bergamaschi, M.; dos Santos, A.C.; Teixeira, A.L.; Hallak, J.E.C.; Crippa, J.A.S. Effects of cannabidiol in the treatment of patients with Parkinson’s disease: An exploratory double-blind trial. J. Psychopharmacol. 2014, 28, 1088–1098. Available online: https://journals.sagepub.com/doi/abs/10.1177/0269881114550355?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=jopa (accessed on 5 May 2018). [CrossRef]
- Ahmed, A.; van den Elsen, G.; van der Marck, M.; Olde Rikkert, M. Medicinal Use of Cannabis and Cannabinoids in Older Adults: Where Is the Evidence? J. Am. Geriatr. Soc. 2014, 62, 410–411. [Google Scholar] [CrossRef]
- Wolff, V.; Armspach, J.; Lauer, V.; Rouyer, O.; Bataillard, M.; Marescaux, C.; Geny, B. Cannabis-related Stroke. Stroke 2013, 44, 558–563. Available online: https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.112.671347 (accessed on 5 May 2019). [CrossRef] [Green Version]
- Yamaori, S.; Koeda, K.; Kushihara, M.; Hada, Y.; Yamamoto, I.; Watanabe, K. Comparison in the In Vitro Inhibitory Effects of Major Phytocannabinoids and Polycyclic Aromatic Hydrocarbons Contained in Marijuana Smoke on Cytochrome P450 2C9 Activity. Drug Metab. Pharmacokinet. 2012, 27, 294–300. Available online: https://www.jstage.jst.go.jp/article/dmpk/27/3/27_DMPK-11-RG-107/_article (accessed on 5 May 2019). [CrossRef] [PubMed] [Green Version]
- Bergamaschi, M.; Queiroz, R.; Chagas, M.; de Oliveira, D.; De Martinis, B.; Kapczinski, F.; Quevedo, J.; Roesler, R.; Schröder, N.; Nardi, A.E.; et al. Cannabidiol Reduces the Anxiety Induced by Simulated Public Speaking in Treatment-Naïve Social Phobia Patients. Neuropsychopharmacology 2011, 36, 1219–1226. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3079847/ (accessed on 4 May 2019). [CrossRef] [PubMed]
- Patel, T.; Yosipovitch, G. The management of chronic pruritus in the elderly. Skin Ther. Lett. 2020, 15, 5–9. [Google Scholar]
- Fusar-Poli, P.; Crippa, J.; Bhattacharyya, S.; Borgwardt, S.; Allen, P.; Martin-Santos, R.; Seal, M.; Surguladze, S.A.; O’Carrol, C.; Atakan, Z.; et al. Distinct Effects of Δ9-Tetrahydrocannabinol and Cannabidiol on Neural Activation During Emotional Processing. Arch. Gen. Psychiatry 2009, 66, 95. Available online: https://jamanetwork.com/journals/jamapsychiatry/fullarticle/482939 (accessed on 4 May 2019). [CrossRef] [Green Version]
- Narang, S.; Gibson, D.; Wasan, A.; Ross, E.; Michna, E.; Nedeljkovic, S.; Jamison, R.N. Efficacy of Dronabinol as an Adjuvant Treatment for Chronic Pain Patients on Opioid Therapy. J. Pain 2008, 9, 254–264. Available online: https://jpain.org/retrieve/pii/S1526590007009674 (accessed on 4 May 2019). [CrossRef]
- Strasser, F.; Luftner, D.; Possinger, K.; Ernst, G.; Ruhstaller, T.; Meissner, W.; Ko, Y.-D.; Schnelle, M.; Reif, M.; Cerny, T. Comparison of Orally Administered Cannabis Extract and Delta-9-Tetrahydrocannabinol in Treating Patients With Cancer-Related Anorexia-Cachexia Syndrome: A Multicenter, Phase III, Randomized, Double-Blind, Placebo-Controlled Clinical Trial from the Cannabis-In-Cachexia-Study-Group. J. Clin. Oncol. 2006, 24, 3394–3400. Available online: https://ascopubs.org/doi/full/10.1200/JCO.2005.05.1847?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub%3Dpubmed (accessed on 4 May 2019).
- Sutton, L.; Demark-Wahnefried, W.; Clipp, E. Management of terminal cancer in elderly patients. Lancet Oncol. 2003, 4, 149–157. [Google Scholar] [CrossRef]
- Jatoi, A. Dronabinol versus Megestrol Acetate versus Combination Therapy for Cancer-Associated Anorexia: A North Central Cancer Treatment Group Study. J. Clin. Oncol. 2002, 20, 567–573. Available online: https://www.ncbi.nlm.nih.gov/pubmed/11786587 (accessed on 4 May 2019). [CrossRef] [Green Version]
- Sieradzan, K.; Fox, S.; Hill, M.; Dick, J.; Crossman, A.; Brotchie, J. Cannabinoids reduce levodopa-induced dyskinesia in Parkinson’s disease: A pilot study. Neurology 2001, 57, 2108–2111. Available online: https://n.neurology.org/content/57/11/2108.long (accessed on 5 May 2018). [CrossRef]
- Yeh, S.; Schuster, M. Geriatric cachexia: The role of cytokines. Am. J. Clin. Nutr. 1999, 70, 183–197. [Google Scholar] [CrossRef] [Green Version]
- Volicer, L.; Stelly, M.; Morris, J.; McLaughlin, J.; Volicer, B. Effects of Dronabinol on anorexia and disturbed behavior in patients with Alzheimer’s disease. Int. J. Geriatr. Psychiatry 1997, 12, 913–919. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1002/%28SICI%291099-1166%28199709%2912%3A9%3C913%3A%3AAID-GPS663%3E3.0.CO%3B2-D (accessed on 3 May 2019). [CrossRef]
- Ware, M.; Wang, T.; Shapiro, S.; Robinson, A.; Ducruet, T.; Huynh, T.; Gamsa, A.; Bennett, G.J.; Collet, J.-P. Smoked cannabis for chronic neuropathic pain: A randomized controlled trial. Can. Med. Assoc. J. 2010, 182, E694–E701. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2950205/ (accessed on 13 May 2019). [CrossRef] [PubMed] [Green Version]
- NABILONE [Internet]. BNF, 2019. Available online: https://bnf.nice.org.uk/drug/nabilone.html#indicationsAndDoses (accessed on 22 May 2019).
- Kim, J.; Grobelna, A. Nabilone for Chronic Pain Management: A Review of Clinical Effectiveness and Guidelines. CADTH: Ottowa, ON, Canada, 2017. Available online: https://www.cadth.ca/sites/default/files/pdf/htis/2017/RC0906%20Nabilone%20for%20Chronic%20Pain%20Management%20Final.pdf (accessed on 11 May 2019).
- Cannabinoid Buccal Spray for Chronic Non-Cancer or Neuropathic Pain: A Review of Clinical Effectiveness and Guidelines. CADTH: Ottowa, ON, Canada, 2016. Available online: https://www.ncbi.nlm.nih.gov/books/NBK395789/pdf/Bookshelf_NBK395789.pdf (accessed on 11 May 2019).
- Cannabis [Internet]. 2019. Available online: https://www.mssociety.org.uk/about-ms/treatments-and-therapies/cannabis (accessed on 11 May 2019).
- Volkert, D.; Chourdakis, M.; Faxen-Irving, G.; Frühwald, T.; Landi, F.; Suominen, M.; Vandewoude, M.; Wirth, R.; Schneider, S.M. ESPEN guidelines on nutrition in dementia. Clin. Nutr. 2015, 34, 1052–1073. Available online: https://www.clinicalnutritionjournal.com/article/S0261-5614(15)00237-X/fulltext (accessed on 6 May 2019). [CrossRef] [PubMed]
- Wolitzky-Taylor, K.; Castriotta, N.; Lenze, E.; Stanley, M.; Craske, M. Anxiety disorders in older adults: A comprehensive review. Depress. Anxiety 2010, 27, 190–211. Available online: https://doi.org/10.1002/da.20653 (accessed on 6 May 2019). [CrossRef] [PubMed]
- Choi, N.; Marti, C.; DiNitto, D.; Choi, B. Older adults’ marijuana use, injuries, and emergency department visits. Am. J. Drug Alcohol Abus. 2017, 44, 215–223. [Google Scholar] [CrossRef] [Green Version]
- Desrosiers, N.; Ramaekers, J.; Chauchard, E.; Gorelick, D.; Huestis, M. Smoked Cannabis’ Psychomotor and Neurocognitive Effects in Occasional and Frequent Smokers. J. Anal. Toxicol. 2015, 39, 251–261. [Google Scholar] [CrossRef] [Green Version]
- Herrmann, N.; Ruthirakuhan, M.; Gallagher, D.; Verhoeff, N.; Kiss, A.; Black, S.; Lanctôt, K.L. Randomized Placebo-Controlled Trial of Nabilone for Agitation in Alzheimer’s Disease. Am. J. Geriatr. Psychiatry 2019, 27, 1161–1173. [Google Scholar] [CrossRef]
- Woodward, M.; Harper, D.; Stolyar, A.; Forester, B.; Ellison, J. Dronabinol for the Treatment of Agitation and Aggressive Behavior in Acutely Hospitalized Severely Demented Patients with Noncognitive Behavioral Symptoms. Am. J. Geriatr. Psychiatry 2014, 22, 415–419. [Google Scholar] [CrossRef]
- Riva, N.; Mora, G.; Sorarù, G.; Lunetta, C.; Ferraro, O.; Falzone, Y.; Leocani, L.; Fazio, R.; Comola, M.; Comi, G.; et al. Safety and efficacy of nabiximols on spasticity symptoms in patients with motor neuron disease (CANALS): A multicentre, double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2019, 18, 155–164. [Google Scholar] [CrossRef]
| Author | Year | Study Type | Main Findings |
|---|---|---|---|
| Minerbi A. [7] | 2019 | Review | Evidence for efficacy is sparse, and considerable adverse effects have been documented on cognitive, cardiovascular and gait function. |
| McMaster University [8] | 2019 | RCT protocol | Protocol for a trial that will assess the efficacy of CBD versus a placebo for post-operative pain following knee arthroplasty. |
| Van Den Elsen G. [9] | 2019 | RCT | THC had no significant effect on neuropsychiatric symptoms, but was well tolerated by participants. |
| Beauchet O. [10] | 2018 | Mini review | Some studies report improved outcomes. However, studies are not focusing on an elderly population, and are of limited quality, making any conclusions difficult to draw. |
| Abuhasira R. [11] | 2018 | Prospective study | Therapeutic cannabis is both effective and safe in an elderly population. In particular, its ability to reduce other prescriptions, such as opioids, is advantageous. |
| Agornyo P. [12] | 2018 | Survey | Regular cannabis use in older patients resulted in reduced pain, reduced medication side effects and the discontinuation of other pain medications. |
| Briscoe [13] | 2018 | Review | The volume of current research is increasing, but there is still insufficient evidence to make robust recommendations. |
| Mücke M. [14] | 2018 | Systematic review | The risks of cannabinoid treatments for neuropathic pain appear to outweigh any potential benefits. |
| Torres-Moreno M. [15] | 2018 | Systematic Review | Results favored cannabinoids over the placebo. However, there is little evidence to suggest that cannabinoids are effective for bladder dysfunction, pain and spasticity in MS patients. |
| Grayson L. [16] | 2018 | Case report | Observed reaction between cannabidiol and warfarin. INR more than doubled. |
| Stockings E. [17] | 2018 | Systematic Review | The effectiveness of cannabinoids is minimal for non-cancer pain. Studies show very high NNT for cannabinoids. |
| Mahvan T.D. [18] | 2017 | Review | There are considerable risks for elderly patients using cannabis, especially those with comorbidities. |
| Katz I. [19] | 2017 | Review | For Parkinson’s Disease (PD), cannabis can be useful as a last resort. For dementia, cannabis can help with behavioral problems. Sleep disturbance and weight loss are also areas of potential benefit from cannabis. |
| Bellnier T. [20] | 2017 | Retrospective study | Cannabis led to improved quality of life, reduced pain, reduced opioid use and led to reduced costs. |
| Hansra D.M. [21] | 2017 | Survey | Dronabinol led to significant improvements in QoL, appetite and anxiety, amongst cancer patients. |
| Schimrigk S. [22] | 2017 | RCT | Dronabinol was non-significantly better at reducing pain in MS patients. However, Dronabinol was associated with much higher rates of adverse events. |
| Lim K. [23] | 2017 | Systematic Review | Studies indicate that cannabinoids could potentially benefit anxiety, psychotic symptoms, PTSD and dyskinesia in PD. |
| Stampanoni M. [24] | 2017 | Review | The evidence for cannabinoids in PD patients is currently inconclusive. |
| Tafelski S. [25] | 2016 | Systematic review of systematic reviews | Cannabinoids should not be recommended for chemotherapy-induced nausea and vomiting, as either a first- or second-line treatment. Anti-emetics are currently superior. |
| Ahmed A.I. [26] | 2015 | RCT | THC was well tolerated by elderly participants with dementia. There were more adverse events within the placebo group. Adverse events experienced by THC users were most commonly: dizziness, fatigue and agitation. |
| Smith L.A. [27] | 2015 | Systematic review | Cannabinoids may have potential at reducing chemotherapy-induced nausea and vomiting. |
| Liu C. [28] | 2015 | Review | Some studies show significant improvement in agitation and aggression in Alzheimer’s Disease (AD) patients, but evidence is insufficient to make robust conclusions. |
| van den Elsen G.A. [29] | 2014 | Systematic Review | Studies show that THC may be useful for anorexia and behavioral symptoms in dementia. Adverse symptoms were common in the cannabinoid groups, with sedation being the most frequent. |
| Ahmed A.I. [30] | 2014 | RCT | THC was associated with more adverse events than placebo. Increasing the dose of THC increased the frequency of adverse events. |
| Lotan I. [31] | 2014 | Open label study | Smoking cannabis significantly improved sleep and reduced pain in PD patients. |
| Chagas M.H. [32] | 2014 | RCT | Cannabidiol had no significant impact upon PD symptoms, but showed an improved quality of life (QoL). |
| Ahmed A.I. [33] | 2014 | Letter | There is scanty evidence for the safety and effectiveness of cannabis and cannabinoids in the elderly. We also cannot extrapolate results from the studies of younger individuals onto an elderly population. |
| Wolff V. [34] | 2013 | Case series | It is highly likely that there is an association between cannabis and stroke. |
| Yamaori S. [35] | 2012 | In vitro study | THC and CBD both inhibited CYP2C9 activity. |
| Bergamaschi M. [36] | 2011 | RCT | CBD significantly reduced anxiety in participants giving public speeches. |
| Patel T. [37] | 2010 | Review | Cannabinoid agonists have been shown to reduce chronic pruritis in patients with atopic dermatitis, lichen simplex, prurigo nodularis, and CKD-related itching. |
| Fusar-Poli P. [38] | 2009 | RCT | CBD reduces autonomic responses to fear, whereas THC augments the autonomic response. |
| Narang S. [39] | 2008 | RCT | Dronabinol resulted in additional pain relief for individuals already using opioids for noncancer-related chronic pain. |
| Strasser F. [40] | 2006 | RCT | THC and cannabis extract were no better than the placebo at increasing appetite or QoL for patients with cancer-related cachexia. |
| Sutton L.M. [41] | 2003 | Review | Cannabinoids can be useful for dyspnoea at the end of life. However, there must be caution with these agents due to the psychotropic effect and reflex tachycardia and hypotension. |
| Jatoi A. [42] | 2002 | RCT | Megestrol acetate performed better than dronabinol for palliating anorexia in cancer patients. |
| Sieradzan F. [43] | 2001 | RCT | Nabilone significantly reduced dyskinesias in PD patients. |
| Yeh S. [44] | 1999 | Review | Anecdotal evidence has shown Dronabinol to be effective at increasing appetite in HIV patients and Alzheimer’s patients. |
| Volicer L. [45] | 1997 | RCT | Body weight increased more within the dronabinol group than with the placebo. |
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beedham, W.; Sbai, M.; Allison, I.; Coary, R.; Shipway, D. Cannabinoids in the Older Person: A Literature Review. Geriatrics 2020, 5, 2. https://doi.org/10.3390/geriatrics5010002
Beedham W, Sbai M, Allison I, Coary R, Shipway D. Cannabinoids in the Older Person: A Literature Review. Geriatrics. 2020; 5(1):2. https://doi.org/10.3390/geriatrics5010002
Chicago/Turabian StyleBeedham, William, Magda Sbai, Isabel Allison, Roisin Coary, and David Shipway. 2020. "Cannabinoids in the Older Person: A Literature Review" Geriatrics 5, no. 1: 2. https://doi.org/10.3390/geriatrics5010002





