Planning of a Health Emergency Disaster Risk Management Programme for a Chinese Ethnic Minority Community
Abstract
:1. Introduction
1.1. Disaster Health Preparedness in the Rural Poor Areas in China
1.2. Building Disaster Health Resilient Communities
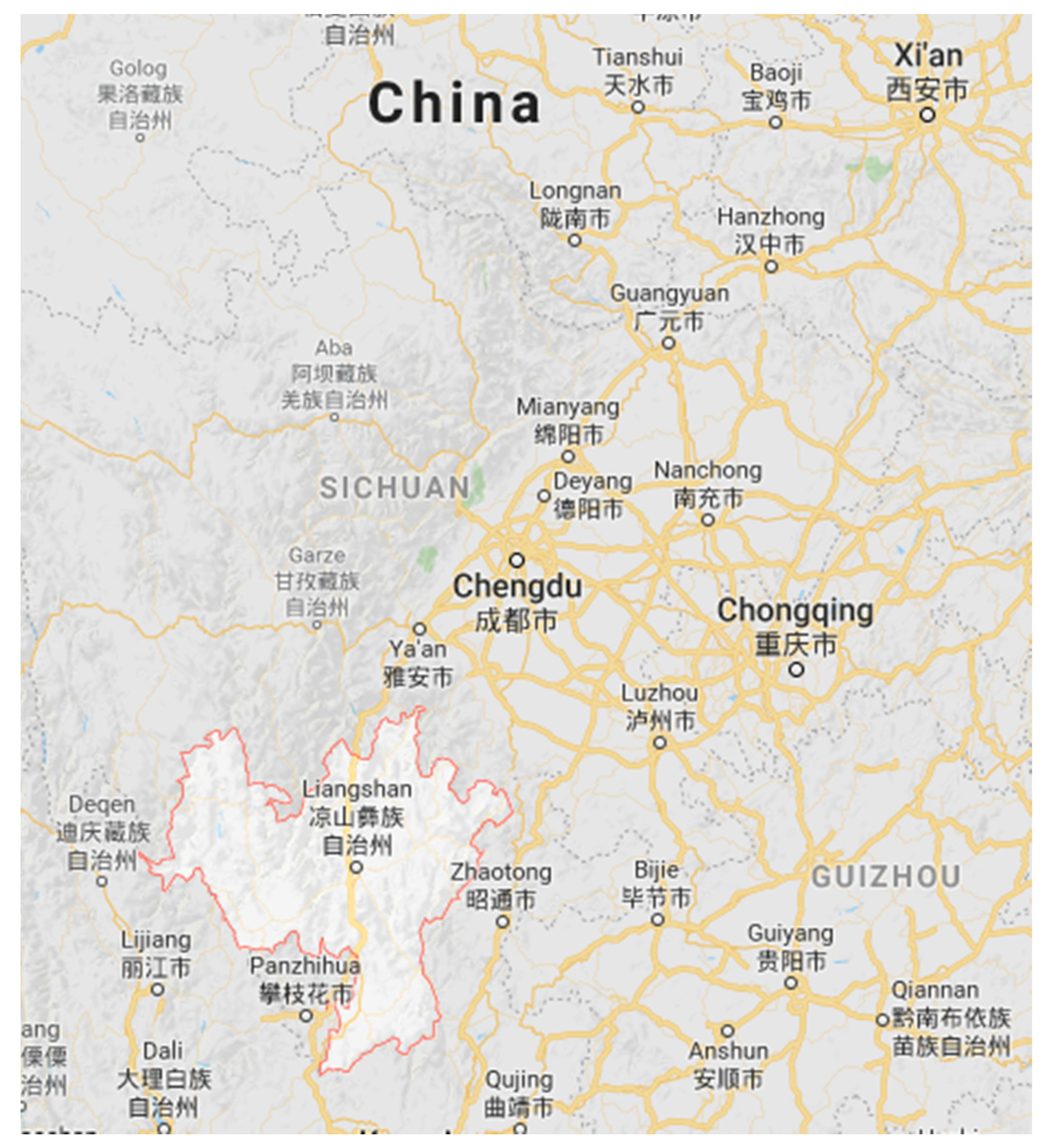
1.3. Local Epidemiological and Demographic Data of Hongyan Village, Liangshan Yi Autonomous Prefecture, China
2. Materials and Methods
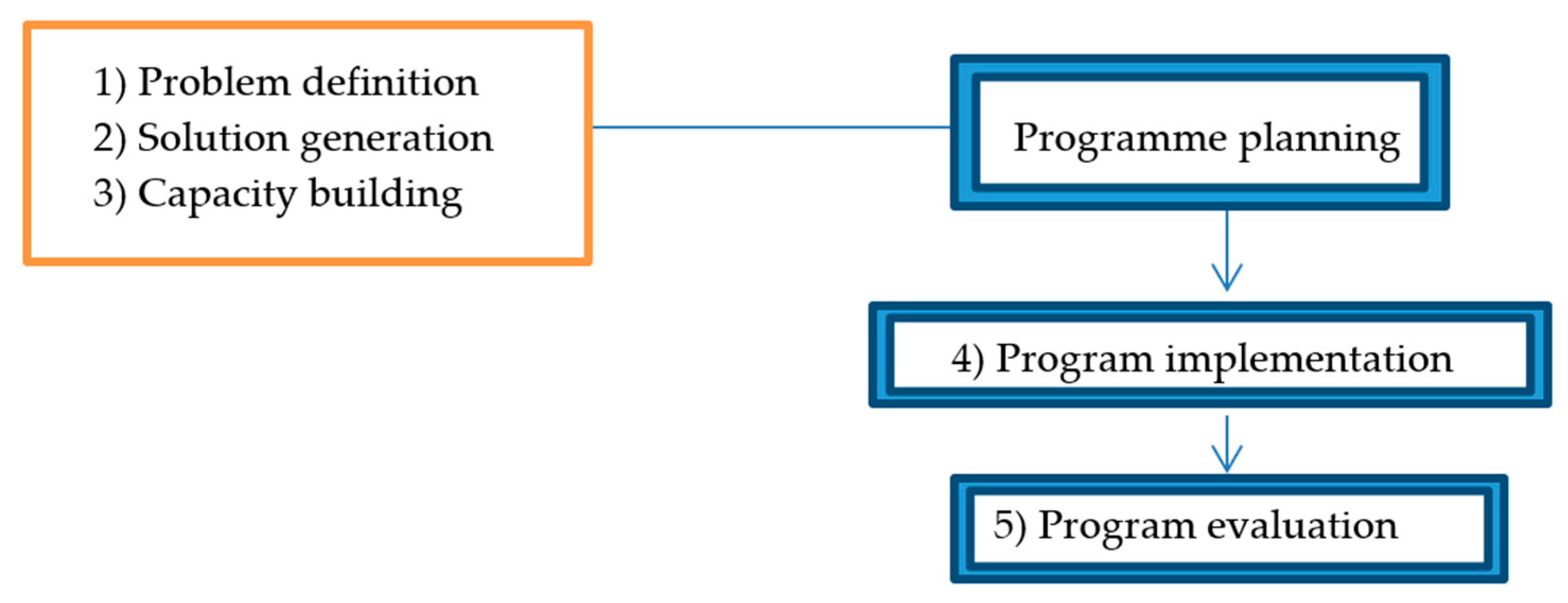
2.1. Planning Framework and Data Collection
2.2. Information for Health Planning
2.2.1. Literature Review
2.2.2. Household Survey
2.2.3. Focus Group
2.2.4. Discussion with Stakeholders
2.3. Data Analysis
3. Results
3.1. Problem Definition: Community Needs and Perceived Priorities
3.2. Problem Definition: Determinants of Lack of Disaster Preparedness
3.2.1. Theme 1: Knowledge of Consequences and Treatment of Diarrhoea
3.2.2. Theme 2: Knowledge, Attitude and Practice towards Use of Disaster Kit
3.3. Solution Generation
3.3.1. Choice of Health Promotion Model and Intervention Strategy
- That they are susceptible to the problem.
- That the problem could result in potentially severe consequences.
- That course of action can reduce risks.
- That benefits of action outweigh barriers
- Self-efficacy [19].
3.3.2. Experience from Past Programmes and Practitioners Applied to the Intervention
3.4. Capacity Building
3.4.1. Mobilizing Human, Material and Financial Resources
3.4.2. Training People and Building Sustainable Programmes
3.4.3. Raising Public and Political Awareness
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Institute of Development Studies. Rural Disaster Risk-Poverty Interface. 2008. Available online: http://www.ids.ac.uk/publication/rural-disaster-risk-poverty-interface (accessed on 1 March 2016).
- Prevention Web. Poverty and Inequality. Available online: http://www.preventionweb.net/risk/poverty-inequality (accessed on 1 March 2016).
- Chan, E.Y.Y.; Kim, J.H.; Lin, C.; Cheung, E.Y.L.; Lee, P.P.Y. Is Previous Disaster Experience a Good Predictor for Disaster Preparedness in Extreme Poverty Households in Remote Muslim Minority Based Community in China? J. Immigr. Minority Health 2014, 16, 466–472. [Google Scholar] [CrossRef] [PubMed]
- Woersching, J.; Snyder, A. Earthquakes in El Salvador: A descriptive study of health concerns in a rural community and the clinical implications, part I. Disaster Manag. Response 2003, 1, 105–109. [Google Scholar] [CrossRef]
- Woersching, J.; Snyder, A. Earthquakes in El Salvador: A descriptive study of health concerns in a rural community and the clinical implications, part II. Disaster Manag. Response 2004, 2, 10–13. [Google Scholar] [CrossRef] [PubMed]
- United Nations Office for Disaster Risk Reduction. Sendai Framework for Disaster Risk Reduction. Available online: https://www.unisdr.org/we/coordinate/sendai-framework (accessed on 1 April 2016).
- United Nations Office for Disaster Risk Reduction. Hyogo Framework for Action. Available online: https://www.unisdr.org/we/coordinate/hfa (accessed on 1 April 2016).
- United Nations Office for Disaster Risk Reduction. Terminology. Available online: https://www.unisdr.org/we/inform/terminology (accessed on 1 April 2016).
- United Nations. Building Disaster Resilient Communities. 2007. Available online: http://www.unisdr.org/files/596_10307.pdf (accessed on 1 April 2016).
- International Federation of Red Cross and Red Crescent Societies. China and Cambodia: Integrated Programming and Cooperation with Local Authorities Boost Communities’ Disaster Preparedness. Available online: http://www.ifrc.org/Global/Case%20studies/Disasters/cs-dm-china-cambodia-en.pdf (accessed on 1 April 2016).
- Charitable Foundation Cartier. Preparing for Natural Disasters in Western China. Available online: http://www.cartiercharitablefoundation.org/en/commitment/programs/planning-and-preparing-for-natural-disasters-in-western-china (accessed on 1 April 2016).
- Centre for Research on the Epidemiology of Disasters. Annual Disaster Statistical Review 2013: The Numbers and Trends. Available online: http://reliefweb.int/report/world/annual-disaster-statistical-review-2013-numbers-and-trends (accessed on 1 April 2016).
- Emily, Y.Y.; Chan, Y.J.; Zhu, P.; Lee, S.D.; Liu, C. Impact of disaster preparedness intervention in Yi-minority community in Sichuan Province, China. In Proceedings of the 12th Asia Pacific Congress on Disaster Medicine, Tokyo, Japan, 17–19 September 2014. [Google Scholar]
- Emily, Y.Y.; Chan, Y.J.; Zhu, P.; Lee, S.D.; Liu, C. The Evaluation on Disaster Preparedness Interventions in Post-flooding Yi Minority Community in Sichuan Province, China. In Proceedings of the 19th World Congress on Disaster & Emergency Medicine, Cape Town, South Africa, 21–24 April 2015. [Google Scholar]
- Chan, E.Y.Y.; Guo, C.; Lee, P.; Liu, S.; Mark, C.K.M. Health Emergency and Disaster Risk Management (Health-EDRM) in Remote Ethnic Minority Areas of Rural China: The Case of a Flood-Prone Village in Sichuan. Int. J. Disaster Risk Sci. 2017, 8, 1–8. [Google Scholar] [CrossRef]
- Yoder, P.S.; Hornik, R.C. Perceptions of severity of diarrhoea and treatment choice: A comparative study of HealthCom sites. J. Trop. Med. Hyg. 1994, 97, 1–12. [Google Scholar] [PubMed]
- Thomas, T.N.; Leander-Griffith, M.; Harp, V.; Cioffi, J.P. Influences of Preparedness. Knowledge and Beliefs on Household Disaster Preparedness. Morb. Mortal. Wkly. Rep. 2015, 64, 965–971. [Google Scholar] [CrossRef] [PubMed]
- Ejeta, L.T.; Ardalan, A.; Paton, D. Application of Behavioral Theories to Disaster and Emergency Health Preparedness: A Systematic Review. PLoS Curr. Disasters 2015, 1, 1. [Google Scholar] [CrossRef] [PubMed]
- Lewis, G.; Sheringham, J.; Kalim, K.; Crayford, T. Mastering Public Health: A Postgraduate Guide to Examinations and Revalidation; Royal Society of Medicine: London, UK, 2008. [Google Scholar]
- Teitler-Regev, S.; Shahrabani, S.; Benzion, U. Factors Affecting Intention among Students to Be Vaccinated against A/H1N1 Influenza: A Health Belief Model Approach. Adv. Prev. Med. 2011, 1, 353207. [Google Scholar] [CrossRef] [PubMed]
- Taylor, P.; Yang, Z.J. Predicting Young Adults’ Intentions to Get the H1N1 Vaccine: An Integrated Model. J. Health Commun. 2014, 20, 1–11. [Google Scholar]
- Nexøe, J.; Kragstrup, J.; Søgaard, J. Decision on influenza vaccination among the elderly. A questionnaire study based on the Health Belief Model and the Multidimensional Locus of Control Theory. Scand. J. Prim. Health Care 1999, 17, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Semenza, J.C.; Ploubidis, G.B.; George, L.A. Climate change and climate variability: Personal motivation for adaptation and mitigation. Environ. Health 2011, 10, 46. [Google Scholar] [CrossRef] [PubMed]
- Bradley, D.T.; McFarland, M.; Clarke, M. The Effectiveness of Disaster Risk Communication: A Systematic Review of Intervention Studies. PLoS Curr. Disasters 2014, 22, 1. [Google Scholar] [CrossRef] [PubMed]
- Ardalan, A.; Naieni, K.H.; Mahmoodi, M.; Zanganeh, A.M.; Keshtkar, A.A.; Honarvar, M.R.; Kabir, M.J. Flash flood preparedness in Golestan province of Iran: A community intervention trial. Am. J. Disaster Med. 2010, 5, 197–214. [Google Scholar] [CrossRef] [PubMed]
- Eisenman, D.P.; Glik, D.; Gonzalez, L.; Maranon, R.; Zhou, Q.; Tseng, C.H.; Asch, S.M. Improving Latino disaster preparedness using social networks. Am. J. Prev. Med. 2009, 37, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Clerveaux, V.; Spence, B. The Communication of Disaster Information and Knowledge to Children Using Game Technique: The Disaster Awareness Game (DAG). Int. J. Environ. Res. 2009, 3, 209–222. [Google Scholar]
- Tanes, Z. Earthquake Risk Communication with Video Games: Examining the Role of Player-Game Interaction in Influencing the Gaming Experience and Outcomes. Ph.D. Thesis, Purdue University, West Lafayette, IN, USA, 2011. [Google Scholar]
- Tanes, Z.; Cho, H. Goal setting outcomes: Examining the role of goal interaction in influencing the experience and learning outcomes of video game play for earthquake preparedness. Comput. Hum. Behav. 2013, 29, 858–869. [Google Scholar] [CrossRef]
- Chan, E.Y.Y. Building Bottom-Up Health and Disaster Risk Reduction Programmes; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- CCOUC (Collaborating Centre for Oxford University and CUHK for Disaster and Medical Humanitarian Response). The Ethnic Minority Health Project: Trip Report for Hongyan, Sichuan; CCOUC: Hong Kong, China, 2014. [Google Scholar]
- Chan, E.Y.Y. Bottom-up disaster resilience. Nat. Geosci. 2013, 6, 327–328. [Google Scholar] [CrossRef]
- Du, F.; Kobayashi, H.; Okazaki, K.; Ochiai, C. Research on the disaster coping capability of a historical village in a mountainous area of China: Case study in Shangli, Sichuan. Procedia Soc. Behav. Sci. 2016, 218, 118–130. [Google Scholar] [CrossRef]
- Kelman, I. Disaster Mitigation is Cost Effective; World Bank: Washington, DC, USA, 2013. [Google Scholar]
- Jassempour, K.; Shirazi, K.K.; Fararooei, M.; Shams, M.; Shirazi, A.R. The impact of educational intervention for providing disaster survival kit: Applying precaution adoption process model. Int. J. Disaster Risk Reduct. 2014, 10, 374–380. [Google Scholar] [CrossRef]
- WHO (World Health Organization). Health Emergency and Disaster Management Fact Sheets 2017. Available online: https://www.who.int/hac/techguidance/preparedness/risk-management-overview-december2017.pdf (acessed on 1 January 2019).
| Planning Stage | Information Needed | Source | Section |
|---|---|---|---|
| Problem definition | Local epidemiological and demographic data to determine the size and nature of the problem | Literature review | 1.3 |
| Community needs and perceived priorities | Household survey Focus group | 3.1 | |
| Determinants of lack of disaster preparedness | Literature review Household survey | 3.2 | |
| Solution generation | Theories and intervention models | Literature review | 3.3 |
| Evidence from past programmes and practitioners | Discussion with stakeholders | 3.3 | |
| Capacity building | Mobilizing resources, training and infrastructure development, raising public and political awareness | Discussion with stakeholders | 3.4 |
| Sector | Stakeholders | Roles | Expertise |
|---|---|---|---|
| Public health, medicine | Collaborating Centre for Oxford and CUHK for Disaster and Medical Humanitarian Response (CCOUC) | -Recruit volunteers -Co-ordinate stakeholders -Carry out the health needs assessment -Plan, implement and evaluate the program | -Multi-disciplinary (members include doctors and public health professionals) -Health needs assessment -Planning, implementing and evaluating program |
| Architecture/housing | Wu Zhi Qiao (WZQ) Foundation, Department of Architecture, Chinese University of Hong Kong (CUHK) | -Assessing the need for a sustainable development project (e.g., building bridges, schools and housing) | -Access to the community, local knowledge (WZQ previously conducted exploration mission on 20–22 October 2012. |
| Local stakeholders | Local village representatives 1 | -Liaise with other stakeholders on behalf of local villagers -Facilitate programme planning, implementation and evaluation | -Access to the community, local knowledge |
| Programme volunteers | Students from CUHK | -Human resources | -Manpower |
| Theme | Results | Source of Information # |
|---|---|---|
| Health needs | General health: -53.7% had good health status, but 43.5% complained of deteriorating health compared to 5 years ago. Diseases requiring long-term medication: -Gastrointestinal symptoms were most frequently reported (16.7%), followed by arthritis (6.2%) and respiratory complaints (2%) -38.9% reported experiencing diarrhoea in the last 3 months | -Survey |
| Healthcare access | -No village doctor was available in Hongyan village. No local emergency service is available: The closest ambulance station is in Xide county, with a response time of 1 h. -For health visits, 51.8% went to the township clinic, 20.4% went to the hospital, while 3.7% preferred to buy over-the-counter medicine -Many villagers only seek medical consultation when they cannot withstand discomfort, due to the cost of medical care. -50% had avoided medical care in the past 3 months as they were unable to afford it. | -Focus group -Survey -Focus group -Survey |
| Health needs during a disaster | -Only 38.9% of villagers thought they had the ability to protect their family’s health and safety during a disaster -In the 2012 flood, 31.5% reported falling sick. Of those, the most common complaint was gastrointestinal symptoms (37.5%). | -Survey |
| Disaster preparation and response | -To prepare for disasters, regular exercises were held to demonstrate the route of evacuation. No other disaster preparation was done, due to lack of knowledge and financial support. -68.5% of respondents had no preparation before flooding. -The only warning system used mobile phones, which did not work during disasters, due to serious damage to communication infrastructure. During the 2012 flood, most villagers moved higher up the mountain to avoid landslides and house collapse. They stayed in temporary shelters for an average of 62 days. | -Focus group -Survey -Focus group |
| Category | Item | Cost (USD) in 2012 | Estimated Budget (USD) for 2014 |
|---|---|---|---|
| Manpower for background survey and focus group (2012 trip) | Air-tickets and road transportation costs for 10 team members | 7987 | |
| Accommodation for 10 team members and drivers | 459 | ||
| Meal expenses for 10 team members | 764 | ||
| Incentives for 54 interview participants | 103 | ||
| Honorarium for local staff | 267 | ||
| Manpower for background survey and intervention (2014 trip) | Air-tickets and road transportation costs for 24 team members | 19,200 | |
| Accommodation for 24 team members and drivers | 1100 | ||
| Meal expenses for 24 team members | 2000 | ||
| Incentives for 100 interview participants | 200 | ||
| Honorarium for local staff | 300 | ||
| Intervention materials | Printing 5 posters and 100 flyers | 130 | |
| ORS souvenirs: 100 plastic teaspoons and cups | 25 | ||
| 100 disaster kits | 380 | ||
| Polaroid films | 100 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tam, G.; Chan, E.Y.Y.; Liu, S. Planning of a Health Emergency Disaster Risk Management Programme for a Chinese Ethnic Minority Community. Int. J. Environ. Res. Public Health 2019, 16, 1046. https://doi.org/10.3390/ijerph16061046
Tam G, Chan EYY, Liu S. Planning of a Health Emergency Disaster Risk Management Programme for a Chinese Ethnic Minority Community. International Journal of Environmental Research and Public Health. 2019; 16(6):1046. https://doi.org/10.3390/ijerph16061046
Chicago/Turabian StyleTam, Greta, Emily Ying Yang Chan, and Sida Liu. 2019. "Planning of a Health Emergency Disaster Risk Management Programme for a Chinese Ethnic Minority Community" International Journal of Environmental Research and Public Health 16, no. 6: 1046. https://doi.org/10.3390/ijerph16061046





