Abstract
Suicidality poses a significant public health threat and stands as a leading cause of death and disability. Aside from committed suicides, a substantial portion of suicidal behaviors comprises suicide attempts and suicidal ideation. These events may be characterized by a non-fatal outcome, shedding light on the possibility of recurrence. The objectives of the present study were to assess hospitalization rate trends related to any suicidal event and to elucidate the risk factors associated with recurrent suicidal behaviors. In this population-based study, an observational descriptive analysis was conducted on all hospital discharge forms (HDRs, Italian SDO) registered for the residents of the Veneto Region from 2012 to 2021. Cases of attempted suicide (AS) and suicidal ideation (SI) were defined according to ICD coding. Age-standardized hospitalization rates were computed with the direct method. Join Point Regression was used to assess the significance of variations in trends. Factor risks for the reiteration of suicidal behaviors were assessed by multivariate logistic regression. Higher prevalence of SI occurred among individuals under 40 years of age and those affected by psychiatric disorders. Conversely, among individuals aged 60 and above, AS was more common. SI turned out to be associated with a higher likelihood of reiteration compared to AS. Individuals suffering from personality disorders and those with a history of AS as index case exhibited increased risk for the reiteration of AS. Females, younger individuals, and individuals experiencing SI as first episode were instead identified as more likely to repeat this form of suicidal behavior. Contemporary economic and environmental crises, a recent pandemic, and numerous conflicts represent significant additional menaces to mental well-being. Our analysis highlights a concerning positive trend in suicide attempts and ideations, underscoring the imperative for Public Health Systems to implement targeted preventive strategies and mental health promotion campaigns. In the absence of structured suicide registries, we demonstrated that HDRs can serve as an invaluable foundation for preventionists to address the phenomenon and strategically plan interventions.
1. Introduction
Suicidality is a major public health threat and a leading cause of deaths and disabilities worldwide [1]. Specifically, suicide ranks as the 15th-leading cause of death, constituting 1.3% of all fatalities and resulting in over 703,000 deaths annually [2,3]. The latest GBD (Global Burden of Disease) study estimates Disability-Adjusted Life Years (DALYs) attributable to self-harm globally at 441.02 per 100,000 [4]. However, the actual burden of suicide in terms of disability and years of life lost remains unclear.
Given the profound impact of suicides on worldwide public health, various strategies have been deployed to alleviate the burden that they impose. A key objective outlined in the WHO Mental Health Action Plan 2013–2020, which has been extended to 2030, is the reduction of suicide mortality [5].
In 2019, according to the WHO estimations [6], the global suicide rate was 9.2 per 100,000 people, with considerable variation observed among countries, ranging from 0.4 to 72.4 deaths per 100,000 people. In Europe, the overall rate stood at 12.93. Despite an overall decline in suicide mortality of approximately 50% across Europe from 2000 to 2017 [7], contemporary economic and environmental crises, along with numerous conflicts, pose serious menaces to the whole population’s mental health and wellbeing. Additionally, in the last couple of years, the COVID-19 pandemic and its consequent non-pharmaceutical interventions, such as lockdowns, have represented a significant psychological and social burden [7]. Indeed, several studies have shown that collective quarantine measures are associated with an elevated risk of suicide. The pandemic has generated a profound sense of fear and heightened anxiety about the future, which could impact mental health and contribute to suicide risk by interacting with pre-existing risk factors [8,9], like alcohol consumption or domestic violence.
Italy emerged as one of the European countries with the lowest suicide rates [10]. According to ISTAT data, in Italy, 3680 individuals died by suicide in 2019, with crude suicide death rates of 6.7 per 100,000 people [11]. Notably, in northern Italy, particularly in the northeast, the incidence of suicides tends to be higher compared to southern Italy [12,13]. This particularly concerns the Veneto Region, one of the richest regions.
In 2012, the region launched “inOltre”, a 24 h service addressing all psychological needs within the community. The initiative includes a suicide prevention hotline (800 334343), with ten psychologists available seven days per week, ensuring utmost confidentiality [14]. While initially designed to address the heightened risk of suicides among business owners impacted by the economic crisis, the service has progressively broadened its scope to accommodate the needs of all segments of the population. The Veneto Region also enacted the Italian recommendations and national plans for the prevention of self-harm and suicide risk in prisons and hospitals [15,16,17].
Although “inOltre” stands as a highly successful example, it represents only the initial stride towards achieving community welfare. The Veneto Region, like many others, still lacks regional guidelines for psychological support and taking care of individuals with self-harm potential or with a history of attempts.
Indeed, policymakers and preventionists all over the world are called upon, now more than ever, to address social and health planning. Suicide prevention and control necessitate coordination and collaboration across various societal sectors, encompassing health, education, justice, law, politics, and media. Nevertheless, effective prevention and control interventions also rely on data. Unfortunately, the scarcity of suitable records and the poor quality of data remain significant obstacles [3]. These particularly affect cases of attempted or ideated suicide, without fatal consequences [1].
In fact, the definition of suicidal behavior encompasses not only completed suicide but also suicidal ideation and suicide attempts. Suicidal ideation involves thoughts associated with carrying out planned or unplanned actions that are capable of causing one’s own death. A suicide attempt refers to self-injurious behavior intended to bring about one’s own death that does not result in a fatal outcome [18,19]. It is estimated that suicide attempts occur up to 20 times more frequently than deaths by suicide [20]. However, capturing suicidal behaviors poses challenges, contributing to the lack of data and uncertainty in the literature [1,3].
Previous research conducted in Italy revealed a lifetime prevalence of 3% for suicidal ideation and 0.5% for suicide attempts [21]. Moreover, several risk factors were found to be associated with suicidal behavior, including female sex, younger age, lower educational level and income, loss of spouse or job, previous suicide attempts, spontaneous self-injury, psychiatric disorders, alcohol and drug abuse, anxiety and major depressive disorder, loneliness, family history of suicide, previous suicidal ideation, and inadequate social support [22,23,24,25,26]. Recently, several studies also identified specific loci associated with a higher risk of suicide attempts [27,28] and that certain genes correlate with the severity of suicide attempts, revealing a significant overlap with genetic risk factors for major depressive disorder [24,26].
The aim of the present study is to analyze suicidality in the Veneto Region during the period 2012–2021. Specifically, we assessed the temporal trends in hospitalization rates for both suicide attempts and suicidal ideation, utilizing HDR (Hospital Discharge Records) as the primary data. Additionally, we evaluated the risk factors associated with suicide attempts, suicidal ideation, and the recurrence of both. Our main objective is to investigate what factors should be addressed by preventive actions and to assess whether HDRs can be a suitable source in the absence of appropriate high-resolution registries.
2. Materials and Methods
2.1. Study Population
In this population-based study, a descriptive observational analysis was conducted on hospital discharge records (HDRs; Italian “Schede di dimissione ospedaliera (SDO)”). All HDRs generated by Veneto inpatient facilities in the period 2012–2021 were included, regardless of the type of admission (scheduled, urgent, outpatient compulsory treatment, or nonurgent delivery), and the hospitalization regimen (ordinary, day, or week surgery admissions). All inpatient facilities in the region, both public and private, were considered in the study. HDRs concerning individuals who did not reside in the Veneto Region were excluded.
The Veneto Region, positioned in the northeast of Italy and recognized as one of the wealthiest regions in the country (with a GDP of USD 234,995 million in 2023 [29]), is ranked 13th among the 20 Italian regions in terms of population age. As of 2020, the Veneto region had an age index of 170.5, a population density of 265.5 individuals per square kilometer, an average population of 4.8 million, a mean age of 45.6 years, and 51.0% of its population were females [30].
2.2. Case Definition
The cases of suicidal behavior were identified through the diagnosis codes reported in the HDRs. According to regional guidelines for compiling HDRs [31], diagnoses were encoded using the International Classification of Diseases (ICD). Please note that the administrative databases of the Veneto Region use the version ICD-9. For conversion to the most recent version, refer to Appendix A, Table A1.
Suicidal events were categorized as attempted suicide (AS) or suicidal ideation (SI). Suicide attempt was defined as a hospital admission with one of the following conditions:
- External Cause Code (“Codice Causa Esterna”) = ICD-9-CM E950-E959 (suicide and self-inflicted injury) AND Trauma or intoxication (“Traumatismi o intossicazioni”) = 5 (self-injury or suicide attempt);
- Secondary diagnosis = ICD-9-CM 300.9 (unspecified nonpsychotic mental disorder) AND (Principal diagnosis = ICD-9-CM 800–999 (injury and poisoning) OR Principal diagnosis = ICD-9-CM 290–319 (mental disorders)).
Suicidal ideation was instead defined as a hospitalization with any diagnosis (primary OR secondary) = ICD-9-CM V62.84 (suicidal ideations) without other codes for trauma or intoxication (ICD-9-CM 800–999).
SI or AS hospitalizations were further categorized as the “first” suicidal event if not preceded by another SI or AS related hospital admission within the preceding 24 months. Otherwise, they were labeled as “repeated”.
The decision to adopt a 2-year time frame was informed by the existing literature. Multiple studies indicate that the risk of a subsequent suicide attempt remains elevated within the 24-month period following the initial episode [32,33,34]. The DSM-5 diagnostic system [34] also suggests including a personal history of AS within the last 24 months in the diagnostic criteria for Behavior Disorder. Hospitalizations without recurrence were designated as “single”, while those with repeated admissions were referred to as “multiple”.
Physical and mental comorbidities were identified by examining both the primary and secondary diagnoses from hospital discharge records. Mental disorders were categorized into the following:
- “Psychotic and mood disorders” (ICD-9-CM 290–299), including organic, e.g., symptomatic, mental disorders; mental and behavioral disorders due to psychoactive substance use; schizophrenia, schizotypal and delusional disorders; dementia; and mood (affective) disorders;
- “Neurotic, behavioral and personality disorders” (ICD-9-CM 300–316), including anxiety, dissociative, stress-related, somatoform and other nonpsychotic mental disorders; behavioral syndromes associated with physiological disturbances and physical factors; disorders of adult personality and behavior; pervasive and specific developmental disorders; and behavioral and emotional disorders with onset usually occurring in childhood and adolescence;
- Intellectual disabilities (ICD-9-CM 317–319).
Specifically, “Neurotic, behavioral and personality disorders” were additionally subcategorized into “borderline personality disorder” (ICD-9-CM 301.83), “acute event reaction” (ICD-9-CM 308–309), and “other”.
Physical comorbidities were assessed through the Charlson Comorbidity Index (CCI). For the purposes of this study, dementia criteria were omitted from the computation. Subsequently, the comorbidities of hospitalized patients were categorized as “Physical” (CCI > 0) or “Non-Physical” (CCI = 0).
2.3. Statistical Analysis
Chi-square tests and Student’s t-tests were employed to assess differences in percentages and averages, respectively. Join Point Regression was conducted to evaluate the significance of trends over time, expressed as annual percentage change (APC). Age-standardized hospitalization rates were computed through direct standardization, utilizing five-year age groups, with the population of Italy as of 1 January 2019 as the reference. The risk of a new suicide event was evaluated through multivariate logistic regression, considering the main associated factors (sex, age group, educational level, physical and mental comorbidities, and type of index event—SI or AS). Both adjusted odds ratios (adjORs) and corresponding 95% confidence intervals (95% CI) were estimated. A significance threshold of p < 0.05 was adopted. Statistical analyses were performed using SPSS Statistics version 28.0.
2.4. Ethics Statement
Hospital Discharge Records (HDRs) were obtained from the administrative databases of the Veneto Region, and the disclosure and utilization of such records for educational and scientific purposes do not necessitate approval from ethical committees. On 24 January 2023, the Veneto Region implemented the Code of Conduct for the use of health data for educational and scientific publication purposes (Official Bulletin of the Region, “Bollettino Ufficiale della Regione” n. 10), as established by the European Committee (European Regulation 2016/679). This implementation received approval from the Italian Personal Data Protection Authority on 24 January 2021.
Adhering to the current Italian privacy legislation, the publication and utilization of HDR data, along with the processing methods, must occur exclusively in aggregate form, without any reference to patients’ personal information. Prior to providing access to the authors, all personal data that could potentially lead to identification was substituted with anonymous codes, in accordance with current privacy regulations (Legislative Decree no. 196 of 30 June 2003).
3. Results
3.1. Hospitalizations for Suicidal Events
In the period from 2012 to 2021, the Veneto Region documented 3491 initial admissions related to suicidal events. Notably, 76.3% (2662 cases) were attributed to attempted suicide, while 23.7% (829 cases) were linked to suicidal ideation. The average annual hospitalization rate for suicide-related incidents was 7.1 per 100,000 people, with specific rates of 5.4 for attempted suicide (AS) and 1.7 for suicidal ideation (SI) (Figure 1).
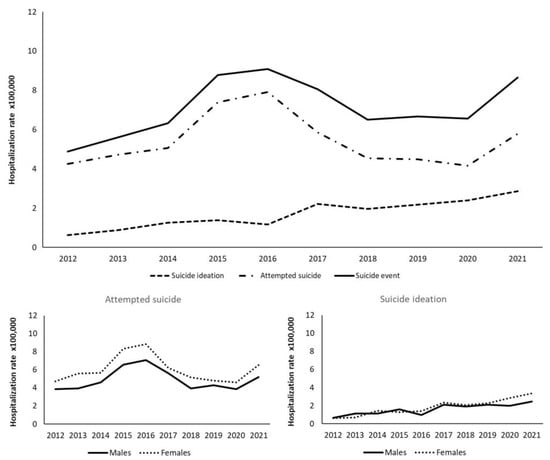
Figure 1.
Standardized annual hospitalization rates for suicide event by type and gender.
Admissions for attempted suicide exhibited a significant upward trend from 2012 to 2016, with hospitalization rates rising from 4.3 to 7.9 per 100,000 people (APC 15.3, 95% CI 1.9; 30.3). Subsequently, there was a notable decreasing trend from 2016 to 2020 (APC −15.6, 95% CI −25.3; −4.5). However, a reversal occurred in 2021, with a renewed increase in the hospitalization rate from 4.2 cases (recorded in the previous year) to 5.8 cases per 100,000 people. Suicidal ideation displayed a significant increasing trend from 2012 to 2021 (APC 16.4, 95% CI 11.4; 21.5), going from 0.6 cases per 100,000 people in 2012 to 2.9 in 2021 (Figure 1).
When stratified by sex, the rates of attempted suicide were consistently higher in females throughout the period, averaging 4.9 and 6.0 cases per 100,000 inhabitants in men and women, respectively. Conversely, suicidal ideation rates followed a similar trend until 2019, with an average rate of 1.5 cases per 100,000 people. However, in 2020–2021, there was an increase in the suicidal ideation rate among females, with 3.4 cases compared to 2.4 cases per 100,000 people recorded among males in 2021 (Figure 1).
Among individuals under 40, the female attempted suicide rate (6.20, 95% CI 5.70; 6.70) was significantly higher than the rate among males (4.36, 95% CI 3.95; 4.77). A similar pattern was observed in individuals aged 40 to 59, where attempted suicide rates among females and males were 7.79 (95% CI 7.16; 8.41) and 5.81 (95% CI 5.27; 6.34), respectively. No significant differences across sex were observed among people over 60. Regarding suicidal ideation, a significant difference was noted between females (2.28, 95% CI 1.98; 2.58) and males (1.55, 95% CI 1.31; 1.79) under 40.
3.2. Characteristics of the Sample
Among the 3491 individuals hospitalized for a suicidal event, 55.6% (1942) are females. Overall, the mean age is 45.0 ± 18.8 years, with significant differences between gender (males 46.2 ± 18.8 years vs. females 42.9 ± 19.3 years; p = 0.001) and between type of event (AS 45.2 ± 18.8 years and SI 41.8 ± 19.9 years; p = 0.001). Table 1 summarizes the main characteristics of the sample. Among individuals with a suicidal event, 79.2% are under 60. Among those who idealize suicide, there is a higher frequency of individuals under 40 (45.5% vs. 39.0%, OR 1.30, 95% CI 1.11; 1.52, p = 0.001) and a lower percentage of people over 60 (17.6% vs. 21.8%, OR 0.77, 95% CI 0.63; 0.94, p = 0.010).

Table 1.
Description of the sample.
It turns out that 3.5% of the total sample has physical comorbidities while 83.0% has mental disorders. Specifically, 60.9% (2126) of the individuals are affected by neurotic, behavioral, or personality disorders, whereas 35.8% (1250) have psychotic or mood disorders. Among all the neurotic disorders, 33.8% (719 out of 2126) are acute reactions and 13.1% (279 out of 2126) borderline personality disorder. Mental disorders are significantly more likely to occur among those who idealize suicide than in those who attempt it (93.8% vs. 79.6%). This latter finding holds both for neurotic disorders (65.9% vs. 59.4%) and psychotic or mood disorders (47.6% vs. 32.1%).
Death among hospitalized individuals occurred in 3.0% of those who attempted suicide, of which 69.1% (56 out of 81) were males. A higher success rate is observed in males than in females (3.6% vs. 1.3%; OR 2.88, 95% CI 1.79; 4.63). As for the execution method, almost half of the suicide attempts occurred through drug or psychoactive substance poisoning (47.9%), with a higher frequency among females (56.7% vs. 36.8%). Instead, the methods that are most frequently implemented by the male gender are self-injury by cutting (20.4% vs. 11.0%, OR 2.08, 95% CI 1.68; 2.58), hanging or suffocation (6.4% vs. 1.4, OR 4.82, 95% CI 2.95; 7.87), the use of gas (2.4% vs. 0.5, OR 4.57, 95% CI 2.07; 10.06), and the use of firearms (2.5% vs. 0.3, OR 9.50, 95% CI 3.33; 27.10).
3.3. Repeated Suicide Events
About 93% (3246 out of 3491) of the hospitalizations for suicidal events are not recurrent behaviors. Two hundred forty-five individuals (7.0%) attempt or ideate suicide several times, with a higher percentage among those who just idealize suicide for the first time than in those who actually try to commit suicide for the first time (10.3% vs. 6.0%, OR 1.79, 95% CI 1.36; 2.35) (Table 1).
Overall, there is an average of 2.4 suicidal events per individual. Specifically, 77.1% (189 out of 245) have 2 suicidal events, 13.9% (34 out of 245) have 3, and 9.0% (22 out of 245) present 4 to 8 suicide events. About 62.9% (154 out of 245) of individuals with multiple hospitalizations have a subsequent hospitalization for attempted suicide, with the latter occurring on average after 150.1 days (median 84, min–max 1–596 days). In contrast, 43.7% (107 out of 245) present a subsequent hospitalization for suicidal ideation, with the latter occurring on average after 154.2 days (median 110, min–max 6–660 days). A subsequent ideation event is significantly more frequent in those who have the first index case for SI (78.8% vs. 25.0%, OR 11.17, 95% CI 5.94; 21.00), whereas a subsequent attempt is more frequent in those who attempted suicide first (80.6% vs. 29.4%, OR 9.99, 95% CI 5.43; 18.37) (Table 1). The multivariate analysis enlightens that the risk of repeated suicidal ideation is higher in females (adjOR 2.04, 95% CI 1.31; 3.19), in individuals less than 60 years old, specifically in those under 40 (adjOR 4.97, 95% CI 1.93; 12.78), in those aged 40 to 59 (adjOR 4.18, 95% CI 1.61; 10.84), and in those for which the index case was a suicidal ideation (adjOR 5.28, 95% CI 3.48; 8.02). On the other hand, the risk of a repeated attempt is significantly higher in individuals with borderline personality disorder (adjOR 4.45, 95% CI 2.77; 7.16), and in those for which the index case was a suicide attempt (adjOR 1.77, 95% CI 1.13; 2.77) (Table 2).

Table 2.
Frequencies of repeated suicidal events and adjusted odds ratios (adjOR) for reiteration risk.
4. Discussion
In the Veneto Region, the overall average rate of hospitalizations in the period 2012–2021 was 5.4 cases per 100,000 people for suicide attempts and 1.7 cases per 100,000 people for suicidal ideation.
The number of hospitalizations for suicidal ideation consistently increased over the considered period, while hospitalizations for suicide attempts exhibited a notable rise from 2012 to 2016, followed by a decline from 2016 to 2020. In 2021, the rate of hospitalization for suicide attempts experienced an uptick, possibly attributed to social restrictions (such as social distancing and lockdowns), economic challenges, and difficulties in accessing services caused by the COVID-19 pandemic.
Indeed, various studies have indicated that suicide rates increased during the implementation of restrictive measures and lockdowns to counteract COVID-19 [35,36], and that these interventions may pose a threat to mental health and elevate the risk of suicide [37]. Furthermore, prior research has reported that suicide rates tend to rise during economic downturns, likely due to increases in unemployment rates and reduced availability of health and social services [38,39].
Our data reveal that the female population exhibits higher rates of suicide attempts among individuals under 60. Conversely, rates of suicidal ideation are more prevalent in females under 40. This observation aligns with several studies that indicate that females and younger individuals are more susceptible to suicidal ideation [40].
It was observed that the rate of suicidal ideation is higher in individuals under 40 and lower in individuals over 60. These findings are consistent with the literature, suggesting that suicidal ideation tends to affect young and middle-aged people, while suicide attempt rates are concentrated in the elderly [21,41]. In countries like Japan or among minorities such as Chinese people living in the US, similar trends are observed. However, suicide attempts are less common in certain populations, such as older African Americans, compared to whites [42]. Cross-cultural disparities are pivotal in interpreting this effect. The perceived influence of family bonds and religiosity–spirituality in the lives of individuals could play a fundamental role in treatment adherence and outcomes for fragile patients with mental illnesses [43]. Additionally, they may influence exposure to environmental risk factors and enhance the management of comorbid medical conditions, thereby addressing the evolving challenges associated with aging.
No significant differences in educational levels were identified between individuals who have experienced suicidal ideation and those who have actually attempted suicide. This could be attributed to the substantial amount of missing data concerning educational level, which was absent for approximately 22% of the study population.
Examining overall suicide cases, we observe that the percentage of cases decreases with each subsequent study year. This trend has also been noted in another study on suicidal ideation, although it is not corroborated for suicide attempts [23]. The rise in suicide events among individuals with lower levels of education may be linked to a more challenging economic situation and limited job opportunities, potentially resulting in poorer health and a subsequent increase in suicidal intentions [44].
Regarding physical and mental comorbidities, it is noteworthy that mental illnesses, particularly psychotic, mood, neurotic, behavioral, and personality disorders, are significantly more prevalent in individuals who ideate suicide compared to those who attempt it. It is important to note that, in the literature, mental disorders are commonly regarded as risk factors for both suicidal ideation and suicide attempts [45,46].
Our findings indicate that the success rate of suicide attempts is higher in the male population than in the female population. Nevertheless, women are three times more likely to attempt suicide than men [47]. This observation may be attributed to the methodology of suicide, as women generally employ less lethal methods than men [48,49].
In our study population, fewer than half of suicide attempts involved drug intoxication, with this method being the most common among females. In contrast, males were more inclined to commit self-injury through cutting, hanging, suffocation, the use of gases, and firearms.
Our findings revealed that the majority (93%) of hospitalizations were due to a single suicide attempt, while only a small fraction resulted from multiple suicide attempts. Previous studies have indicated that individuals who reattempt suicide constitute a subgroup with specific characteristics and risk factors [50]. In our study, the population with a single suicidal event displayed a higher frequency of attempted suicide, whereas the reiteration of suicidal events was more commonly associated with ideation.
The literature reports that individuals who make multiple suicide attempts typically exhibit suicidal ideation and borderline personality traits [50].
From our data, reiterated suicidal ideation appears to be significantly more prevalent among individuals who experience the first index case for suicidal ideation, females, and individuals under 60. On the other hand, the frequency of a repeated suicide attempt is higher among those who have the first index event for suicide attempts and borderline personality disorder. Our results align with the literature, supporting the notion that younger age and personality disorders are risk factors for repeated suicidal behavior [32]. Furthermore, previous studies confirm that individuals who have previously attempted suicide, especially those with mental disorders, lower social support, and greater hopelessness, are more likely to attempt suicide again [51].
Our study is not without limitations. Firstly, the sample composition was drawn from hospital discharge records of the Veneto Region, making it challenging to generalize the results to other population; additionally, suicide cases not resulting in hospitalization may have been neglected. It is also noteworthy that the Veneto Region’s population is predominantly elderly, which could have led to an overestimation of attempted suicide compared to suicidal ideation, given that the former is more common among the elderly. Furthermore, we considered only a few socio-demographic and individual variables, which means that we may not have accounted for all potential socio-economic and social fragility confounding factors (marital status, poverty, human insecurity, addiction, illiteracy, social inequality, unemployment, inflation, dependency, ethnicity, prison history, violence victim, etc.). Our dataset is confined to information extracted solely from the HDRs of the Veneto Region. Accessing the complete medical records was not feasible within the scope of this study. Consequently, our classification is restricted to the diagnosis codes documented in the HDR, which, in the Veneto Region, are still coded using the ICD-9-CM system. We acknowledge that this constraint may introduce bias and limitations to our findings, particularly considering the availability of more contemporary classification systems such as the ICD-10-CM or DSM-5. HDRs data may also not fully capture personal and family medical history. Lastly, this study only encompasses hospital admissions up to the year 2021, potentially too early to comprehensively assess the potential impact of the Sars-CoV-2 pandemic on suicidal behavior.
Despite these limitations, this study spans a long-term trend, allowing for the collection of a substantial sample of data. To our knowledge, this study is one of the first to provide a comparison between ideated and attempted suicide, distinctly addressing both and not solely focusing on completed suicide. Moreover, our work shares valuable information regarding the demographic and individual variables associated with an increased risk of either suicide attempts or suicidal ideation. It is also notable that only a few other studies consider a range of mental disorders as risk factors for suicidal ideation and attempted suicide.
Finally, we assessed sociodemographic factors associated with an increased risk of reattempting suicide, providing useful information for the implementation of effective and tailored preventive strategies.
5. Conclusions
While suicide mortality rates are experiencing a global decline, our analysis highlights a concerning upward trajectory in suicide attempts and ideations. This underscores the persistent and substantial health burden posed by suicides. The contemporary landscape, marked by economic and environmental crises, a recent pandemic, and numerous conflicts, poses a significant threat to the mental well-being of entire populations. Our population-based study points out the imperative for Public Health Systems to implement targeted and effective preventive interventions tailored to both suicidal behaviors and reattempts, and, more generally, to promote emotional and mental health through ad hoc campaigns. The development and implementation of tools for enhancing the prevention and control of these extreme phenomena are paramount. Mapping out the groups who are most susceptible to suicide ideation or attempts is crucial for the early identification of high-risk individuals, including those with or without mental disorders, with specific attention to vulnerable groups such as women, migrants, LGBTQI+ individuals, and prisoners [3]. This approach allows for a more precise targeting of both existing and novel promotion strategies and support services. In the absence of structured data or registries for suicidal behavior, we demonstrated that hospital discharge records, appropriately classified with ICD codes, can serve as an invaluable foundation for preventionists to comprehend the magnitude of the phenomenon and strategically plan interventions.
Author Contributions
Conceptualization, S.C. and M.F.; methodology, P.F. and C.C.; software, P.F.; validation, M.S., M.T., F.R., M.F. and V.B.; formal analysis, S.C. and P.F.; investigation, S.C. and V.B.; resources, V.B.; data curation, M.S.; writing—original draft preparation, G.T., N.C., P.F. and C.C.; writing—review and editing, S.C., M.S., M.T., F.R., M.F. and V.B.; visualization, P.F.; supervision, S.C, M.S., M.T. and F.R.; project administration, V.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Hospital Discharge Records (HDRs) were obtained from the administrative databases of the Veneto Region, and the disclosure and utilization of such records for educational and scientific purposes do not necessitate approval from ethical committees. On 24 January 2023, the Veneto Region implemented the Code of Conduct for the use of health data for educational and scientific publication purposes (Official Bulletin of the Region, “Bollettino Ufficiale della Regione” n. 10), as established by the European Committee (European Regulation 2016/679). This implementation received approval from the Italian Personal Data Protection Authority on 14 January 2021.
Informed Consent Statement
Patient consent was waived because the HDR data are exclusively utilized and published in aggregate form, without any reference to patients’ personal information, in accordance with current Italian privacy legislation. Prior to providing access to the authors, all personal data that could potentially lead to identification were substituted with anonymous codes, in accordance with current privacy regulations (Legislative Decree no. 196 of 30 June 2003).
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Conversion of ICD-9-CM codes to ICD-10-CM.
Table A1.
Conversion of ICD-9-CM codes to ICD-10-CM.
| ICD-9-CM | ICD-10-CM | ||
|---|---|---|---|
| E950–959 | Suicide And Self-Inflicted Injury
| Multiple codes/intervals [52] |
|
| 300.9 | Unspecified nonpsychotic mental disorder | Multiple codes/intervals |
|
| 800–999 | Injury And Poisoning | S00-T98 | Injury, poisoning and certain other consequences of external causes |
| 290–319 | Mental Disorders | F00–F99 | Mental, Behavioral and Neurodevelopmental disorders |
| V62.84 | Suicidal ideations | R45.851 | Suicidal ideations |
| 290–299 |
| F00–F39 |
|
| 300–316 | Neurotic Disorders, Personality Disorders, And Other Nonpsychotic Mental Disorders | Multiple codes/intervals |
|
| 317–319 | Intellectual Disabilities | F70–F79 | Intellectual disabilities |
| 301.83 | Borderline personality disorder | F60.3 | Borderline personality disorder |
| 308–309 |
| Multiple codes/intervals |
|
References
- Shafiee, M.; Shanbehzadeh, M.; Kazemi-Arpanahi, H. Establishing a minimum data set for suicide and attempted suicide registry system in Iran. BMC Public Health 2022, 22, 857. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Mental Health and Substance Use. In Suicide Worldwide in 2019; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications-detail-redirect/9789240026643 (accessed on 12 December 2023).
- World Health Organization (WHO). Suicide. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 12 December 2023).
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019); Institute for Health Metrics and Evaluation (IHME): Seattle, WA, USA, 2020. [Google Scholar]
- World Health Organization (WHO). Mental Health and Substance Use. In Mental Health Action Plan 2013–2020; World Health Organization: Geneva, Switzerland, 2013; Available online: https://www.who.int/publications-detail-redirect/9789241506021 (accessed on 12 December 2023).
- World Health Organization (WHO) Data. Suicide Mortality Rate (per 100,000 Population). Available online: https://data.who.int/indicators/i/16BBF41 (accessed on 12 December 2023).
- Organization for Economic Cooperation and Development (OECD). Health at a Glance: Europe 2020: State of Health in the EU Cycle; Organisation for Economic Co-Operation and Development: Paris, France, 2020; Available online: https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-europe-2020_82129230-en;jsessionid=DNSPLIkip_mYzeGjbbfQ-1cZC4lXx6T1Z-2ysreC.ip-10-240-5-95 (accessed on 12 December 2023).
- Gunnell, D.; Appleby, L.; Arensman, E.; Hawton, K.; John, A.; Kapur, N.; Khan, M.; O’Connor, R.C.; Pirkis, J.; Caine, E.D. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 468–471. [Google Scholar] [CrossRef] [PubMed]
- Delmastro, M.; Zamariola, G. Depressive symptoms in response to COVID-19 and lockdown: A cross-sectional study on the Italian population. Sci. Rep. 2020, 10, 22457. [Google Scholar]
- Ghirini, S.; Vichi, M. Caratteristiche e andamento temporale della mortalità per suicidio in Italia: uno studio descrittivo sugli ultimi 30 anni. Boll Epidemiol. 2020, 1, 1–8. [Google Scholar] [CrossRef]
- Istituto Nazionale di Statistica (ISTAT). Annuario statistico italiano 2021; ISTAT: Rome, Italy, 2021; Available online: https://www.istat.it/storage/ASI/2021/ASI_2021.pdf (accessed on 12 December 2023).
- Zanone Poma, S.; Vicentini, S.; Siviero, F.; Grossi, A.; Toniolo, E.; Cocchio, S.; Baldo, V.; De Leo, D. Life span history of non-fatal suicidal behaviours in a large sample of general practitioners’ patients: Data from Rovigo, Northern Italy. Community Ment. Health J. 2014, 50, 981–986. [Google Scholar] [CrossRef] [PubMed]
- Zenone Poma, S.; Toniolo, E.; Grossi, A.; Pizzo, R.; Cocchio, S.; Baldo, V. Epidemiology of suicide attempts in a psychiatric setting of Northern Italy. G. Ital. Psicopatol. 2013, 19, 119–125. [Google Scholar]
- Regione del Veneto. Numero Verde Anti Suicidi e Servizio Inoltre. Zaia, “Da Oltre 10 Anni Punto di Riferimento Psicologico”. Available online: https://www.regione.veneto.it/web/guest/article-detail?articleId=13902937 (accessed on 12 December 2023).
- Presidenza del Consiglio dei Ministri. Conferenza Unificata. Accordo, ai Sensi Dell’articolo 9 del Decreto Legislativo 28 Agosto 1997, n. 281, sul Documento Recante ‘Piano Nazionale per la Prevenzione del Rischio Autolesivo e Suicidario nei Servizi Residenziali Minorili del Dipartimento per la Giustizia Minorile e di Comunità’. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2017-12-07&atto.codiceRedazionale=17A08166&elenco30giorni=false (accessed on 26 October 2017).
- Presidenza del Consiglio dei Ministri. Conferenza Unificata. Accordo, ai Sensi Dell’articolo 9 del Decreto Legislativo 28 Agosto 1997, n. 281, sul Documento Recante ‘Piano Nazionale per la Prevenzione delle Condotte Suicidarie nel Sistema Penitenziario per Adulti’. Available online: https://www.gazzettaufficiale.it/atto/vediMenuHTML;jsessionid=c0RxoaoFuclE5TxYGBjaNw__.ntc-as3-guri2a?atto.dataPubblicazioneGazzetta=2017-08-14&atto.codiceRedazionale=17A05612&tipoSerie=serie_generale&tipoVigenza=originario (accessed on 27 July 2017).
- Ministero della Salute, Dipartimento della Qualità Direzione Generale della Programmazione Sanitaria, dei Livelli di Assistenza e dei Principi Etici di Sistema Ufficio iii. Prevenzione del Suicidio di Paziente in Ospedale. Available online: https://www.salute.gov.it/portale/sicurezzaCure/dettaglioPubblicazioniSicurezzaCure.jsp?lingua=italiano&id=592 (accessed on 4 March 2008).
- Nock, M.K.; Borges, G.; Bromet, E.J.; Cha, C.B.; Kessler, R.C.; Lee, S. Suicide and Suicidal Behavior. Epidemiol. Rev. 2008, 30, 133–154. [Google Scholar] [CrossRef]
- Nock, M.K.; Green, J.G.; Hwang, I.; McLaughlin, K.A.; Sampson, N.A.; Zaslavsky, A.M.; Kessler, R.C. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry 2013, 70, 300–310. [Google Scholar] [CrossRef] [PubMed]
- EpiCentro, Istituto Superiore di Sanità. Oms, Suicidi: La Dimensione del Problema. Available online: https://www.epicentro.iss.it/mentale/schedasuicidi (accessed on 12 December 2023).
- Scocco, P.; de Girolamo, G.; Vilagut, G.; Alonso, J. Prevalence of suicide ideation, plans, and attempts and related risk factors in Italy: Results from the European Study on the Epidemiology of Mental Disorder–World Mental Health study. Compr. Psychiatry 2008, 49, 13–21. [Google Scholar] [CrossRef]
- Dendup, T.; Zhao, Y.; Dorji, T.; Phuntsho, S. Risk factors associated with suicidal ideation and suicide attempts in Bhutan: An analysis of the 2014 Bhutan STEPS Survey data. PLoS ONE 2020, 15, e0225888. [Google Scholar]
- Nock, M.K.; Borges, G.; Bromet, E.J.; Alonso, J.; Angermeyer, M.; Beautrais, A.; Bruffaerts, R.; Chiu, W.T.; de Girolamo, G.; Gluzman, S.; et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br. J. Psychiatry 2008, 192, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Levey, D.F.; Polimanti, R.; Cheng, Z.; Zhou, H.; Nuñez, Y.Z.; Jain, S.; He, F.; Sun, X.; Ursano, R.J.; Kessler, R.C.; et al. Genetic associations with suicide attempt severity and genetic overlap with major depression. Transl. Psychiatry 2019, 9, 22. [Google Scholar] [CrossRef] [PubMed]
- Bernal, M.; Haro, J.; Bernert, S.; Brugha, T.; de Graaf, R.; Bruffaerts, R.; Lépine, J.; de Girolamo, G.; Vilagut, G.; Gasquet, I.; et al. Risk factors for suicidality in Europe: Results from the ESEMED study. J. Affect. Disord. 2007, 101, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Lengvenyte, A.; Conejero, I.; Courtet, P.; Olié, E. Biological bases of suicidal behaviours: A narrative review. Eur. J. Neurosci. 2021, 53, 330–351. [Google Scholar] [CrossRef]
- Erlangsen, A.; Appadurai, V.; Wang, Y.; Turecki, G.; Mors, O.; Werge, T.; Mortensen, P.B.; Starnawska, A.; Børglum, A.D.; Schork, A.; et al. Genetics of suicide attempts in individuals with and without mental disorders: A population-based genome-wide association study. Mol. Psychiatry 2020, 25, 2410–2421. [Google Scholar] [CrossRef] [PubMed]
- Mullins, N.; Bigdeli, T.B.; Børglum, A.D.; Coleman, J.R.; Demontis, D.; Mehta, D.; Power, R.A.; Ripke, S.; Stahl, E.A.; Starnawska, A.; et al. GWAS of Suicide Attempt in Psychiatric Disorders and Association With Major Depression Polygenic Risk Scores. Am. J. Psychiatry 2019, 176, 651–660. [Google Scholar] [CrossRef] [PubMed]
- OOSGA. GDP of Italy in 2023-Expenditure Approach, Sector Output, and Regional GDP. Available online: https://oosga.com/gdp/ita/ (accessed on 10 May 2024).
- Demographic Statistics Veneto Region (Population Density, Population, Median Age, Households, Foreigners). Available online: https://ugeo.urbistat.com/adminstat/it/it/demografia/dati-sintesi/veneto/5/2 (accessed on 12 December 2023).
- Portale della Sanità della Regione del Veneto. Documentazione di Riferimento Flussi Informativi Regionali SDO. Available online: https://salute.regione.veneto.it/web/aziendazero/tabelle-di-riferimento-generali?p_p_id=20&p_p_lifecycle=0&p_p_state=maximized&p_p_mode=view&_20_struts_action=%2Fdocument_library%2Fview&_20_folderId=1026448 (accessed on 12 December 2023).
- Parra-Uribe, I.; Blasco-Fontecilla, H.; Garcia-Parés, G.; Martínez-Naval, L.; Valero-Coppin, O.; Cebrià-Meca, A.; Oquendo, M.A.; Palao-Vidal, D. Risk of re-attempts and suicide death after a suicide attempt: A survival analysis. BMC Psychiatry 2017, 17, 163. [Google Scholar] [CrossRef]
- Taron, M.; Nunes, C.; Maia, T. Suicide and suicide attempts in adults: Exploring suicide risk 24 months after a psychiatric emergency room visit. Braz. J. Psychiatry 2020, 42, 367–371. [Google Scholar] [CrossRef]
- Fehling, K.B.; Selby, E.A. Suicide in DSM-5: Current Evidence for the Proposed Suicide Behavior Disorder and Other Possible Improvements. Front. Psychiatry 2020, 11, 499980. [Google Scholar] [CrossRef]
- Menculini, G.; Moretti, P.; Pandolfi, L.M.; Bianchi, S.; Valentini, E.; Gatto, M.; Amantini, K.; Tortorella, A. Suicidality and COVID-19: Data from an Emergency Setting in Italy. Psychiatr. Danub. 2021, 33 (Suppl. 9), 158–163. [Google Scholar]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, A.; Sampogna, G.; Giallonardo, V.; Del Vecchio, V.; Luciano, M.; Albert, U.; Carmassi, C.; Carrà, G.; Cirulli, F.; Dell’osso, B.; et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. Eur. Psychiatry 2020, 63, e87. [Google Scholar] [CrossRef]
- Almaghrebi, A.H. Risk factors for attempting suicide during the COVID-19 lockdown: Identification of the high-risk groups. J. Taibah Univ. Med. Sci. 2021, 16, 605–611. [Google Scholar] [CrossRef]
- Merzagora, I.; Mugellini, G.; Amadasi, A.; Travaini, G. Suicide Risk and the Economic Crisis: An Exploratory Analysis of the Case of Milan. PLoS ONE 2016, 11, e0166244. [Google Scholar] [CrossRef]
- Rainone, A.; Tenore, K.; Bertuzzi, A.; Cantarano, S.; Carenti, M.L.; Cruciani, L.; Angelis, A.D.; Fabene, G.; Govetto, C.; Gregni, E.; et al. The phenomenon of suicide: Epidemiology and definitions. Cogn. Clin. 2014, 11, 169–184. [Google Scholar]
- Lee, H.; Seol, K.H.; Kim, J.W. Age and sex-related differences in risk factors for elderly suicide: Differentiating between suicide ideation and attempts. Int. J. Geriatr. Psychiatry 2018, 33, e300–e306. [Google Scholar] [CrossRef]
- Makri, E.; Giannouli, V. Cross-cultural cognitive and affective differences in aging: Can culture shape the expression and perception of psychopathology in old age. Encephalos 2022, 59, 34–43. [Google Scholar]
- Giannouli, V. Ethnicity, mortality, and severe mental illness. Lancet Psychiatry 2017, 4, 517. [Google Scholar] [CrossRef]
- Jo, A.; Jeon, M.; Oh, H. Age-differentiated Risk Factors of Suicidal Ideation among Young and Middle-aged Korean Adults. Osong Public Health Res. Perspect. 2017, 8, 201–210. [Google Scholar] [CrossRef]
- Nock, M.K.; Hwang, I.; Sampson, N.; Kessler, R.C.; Angermeyer, M.; Beautrais, A.; Borges, G.; Bromet, E.; Bruffaerts, R.; de Girolamo, G.; et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: Findings from the WHO World Mental Health Surveys. PLoS Med. 2009, 6, e1000123. [Google Scholar] [CrossRef]
- Zhu, H.; Yao, J.; Fan, H.; Wang, Q.; Wang, X.; Gao, Q. Prevalence and risk factors of suicidal ideation in adult inpatients with five different types of mental disorders. J. Affect. Disord. 2021, 291, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Vijayakumar, L. Suicide in women. Indian J. Psychiatry 2015, 57 (Suppl. 2), S233–S238. [Google Scholar] [CrossRef] [PubMed]
- Callanan, V.J.; Davis, M.S. Gender differences in suicide methods. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 857–869. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Data, Analytics & Delivery. In World Health Statistics 2019: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/publications-detail-redirect/9789241565707 (accessed on 12 December 2023).
- Berardelli, I.; Forte, A.; Innamorati, M.; Imbastaro, B.; Montalbani, B.; Sarubbi, S.; De Luca, G.P.; Mastrangelo, M.; Anibaldi, G.; Rogante, E.; et al. Clinical Differences Between Single and Multiple Suicide Attempters, Suicide Ideators, and Non-suicidal Inpatients. Front. Psychiatry 2020, 11, 605140. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, J.; Sun, L. Who are likely to attempt suicide again? A comparative study between the first and multiple timers. Compr. Psychiatry 2017, 78, 54–60. [Google Scholar] [CrossRef]
- Gabella, B.A.; Hume, B.; Li, L.; Mabida, M.; Costich, J. Multi-site medical record review for validation of intentional self-harm coding in emergency departments. Inj. Epidemiol. 2022, 9, 16. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).