Abstract
Background: Trapeziometacarpal osteoarthritis (TMC OA) is a prevalent degenerative disorder that causes considerable pain and functional limitations, especially in older individuals, whose ideal treatment is still debated in the literature. Various treatments are described to restore a good functional outcome of the thumb; over the past 50 years, biological arthroplasties have been considered the gold standard for treating advanced stages of TMC OA. However, in the last decade, the use of dual mobility cup prostheses has significantly increased, with numerous studies reporting excellent clinical outcomes. In this case report, we show the results of a patient treated on the left hand with suspension arthroplasty and on his right hand with dual mobility arthroplasty in one-stage surgery. The aim of this case report is to directly compare outcomes between trapeziometacarpal prosthesis and suspension arthroplasty performed simultaneously in the same patient. Case Presentation: The present case reports a 71-year-old male patient with bilateral TMC osteoarthritis, referred to our clinic in May 2024. His medical history included hypertension, hypertriglyceridemia, paroxysmal atrial fibrillation, and benign prostatic hyperplasia. On examination, the right hand showed grade 3 osteoarthritis according to the Eaton–Littler classification, with the trapezium maintaining adequate bone stock, making the patient eligible for trapeziometacarpal prosthesis implantation. Conversely, the left hand demonstrated scaphotrapezoid arthritis with a slight reduction in trapezial bone stock, indicating the need for trapeziectomy followed by suspension arthroplasty. Both procedures were performed during the same surgical session by the same experienced hand surgeon using a lateral approach. On the right side, the trapeziometacarpal joint surfaces were resected and replaced with a dual mobility prosthesis, while on the left side, the trapezium was excised, and suspension arthroplasty was performed using a slip of the flexor carpi radialis (FCR) tendon. Methods: The patient underwent simultaneous treatment with a dual mobility trapeziometacarpal prosthesis on the right hand and trapeziectomy with suspension arthroplasty on the left hand. Clinical outcomes (grip and pinch strength, pain, QuickDASH, satisfaction, and range of motion) were evaluated at 1, 3, 6, and 12 months. Paired comparative statistics were applied with significance set at p < 0.05. Results: At all follow-up intervals (1, 3, 6, and 12 months), the hand treated with a trapeziometacarpal prosthesis demonstrated superior grip and pinch strength compared to the hand treated with trapeziectomy and suspension arthroplasty, with the greatest difference observed at 3 months. At 12 months, grip strength increased from 28 kg to 40 kg in the prosthesis-treated hand and from 25 kg to 33 kg in the suspension arthroplasty hand. Paired comparisons were performed at each follow-up interval up to 12 months, confirming a significant difference for grip strength. Pain levels (VAS, Visual Analogue Scale) decreased progressively in both hands, with a more rapid reduction in the hand treated with a trapeziometacarpal prosthesis, reaching statistical significance. QuickDASH scores indicated an earlier return to daily activities in the hand treated with the prosthesis, although this difference was not statistically significant. Patient satisfaction was consistently higher for the hand treated with a trapeziometacarpal prosthesis, with the patient reporting a ‘very satisfied’ rating at all timepoints. Range of motion recovery, assessed through the Kapandji score and measurements of thumb abduction and extension, also favored the hand treated with the prosthesis, with statistically significant differences for abduction and extension, whereas the hand treated with trapeziectomy and suspension arthroplasty demonstrated more gradual improvement over time. Conclusions: This case highlights the functional efficacy of both surgical approaches—biological arthroplasty and trapeziometacarpal prosthesis—in the treatment of TMC osteoarthritis. Both procedures resulted in a good clinical outcome and high patient satisfaction. However, recovery was noticeably faster in the hand treated with a trapeziometacarpal prosthesis, which is consistent with findings previously reported in the literature. These observations suggest that, while both techniques are valid and effective, trapeziometacarpal prosthetic replacement may offer a quicker return to function in appropriately selected patients.
1. Introduction
Trapeziometacarpal osteoarthritis (TMC OA), commonly referred to as basal thumb osteoarthritis, is a widespread degenerative disorder that impacts the joint at the base of the thumb. This condition frequently results in pain, limited mobility, and functional difficulties, particularly with activities that involve pinching or gripping [1]. It is more commonly observed in women [2] with a high prevalence in individuals over 60 year and usually occurs as a consequence of aging or repetitive motions of the thumb [3].
Various treatment strategies are available for addressing TMC osteoarthritis, including conservative approaches [4] like splinting and corticosteroid injections, as well as surgical options for more severe cases. Surgical interventions may involve trapeziectomy, biological arthroplasty [5], or the implantation of a trapeziometacarpal prosthesis [6]. The selection of the appropriate procedure is influenced by factors such as the patient’s age, level of physical activity, and the degree of osteoarthritis present.
A significant topic of discussion in the surgical treatment of TMC OA revolves around the comparison between biological arthroplasty and total joint replacement with a prosthetic implant. Biological arthroplasty aims to maintain some level of natural joint movement by reconstructing or enhancing the surrounding soft tissues, while prosthetic options, including dual mobility designs, provide stability and durability but carry risks such as loosening or dislocation of the implant [7,8]. In contrast, biological arthroplasty typically involves ligament reconstruction and tendon interposition, which can mitigate the complications associated with artificial implants; however, the long-term outcomes of this approach can be inconsistent.
In this article, we describe the case of a patient who received surgical treatments on both hands in one-stage surgery by the same surgeon, for trapeziometacarpal osteoarthritis: a dual mobility trapeziometacarpal prosthesis was placed in the right hand, while the left hand underwent trapeziectomy followed by suspension arthroplasty. This case report aims to directly compare pain relief, functional recovery, and strength between suspension arthroplasty and dual mobility trapeziometacarpal prosthesis performed simultaneously in the same patient.
2. Case Presentation
A 71-year-old male patient was referred to our clinic in May 2024 with a diagnosis of bilateral trapeziometacarpal osteoarthritis. His medical history included hypertension and paroxysmal atrial fibrillation, with no conditions affecting hand function or influencing surgical planning. Radiographic evaluation revealed grade 3 osteoarthritis of the right trapeziometacarpal joint according to the Eaton–Littler classification. Despite the degenerative changes, the trapezium maintained adequate bone stock, making the patient a suitable candidate for trapeziometacarpal prosthesis implantation.
Conversely, the left hand presented combined scaphotrapeziotrapezoidal (STT) and trapeziometacarpal arthritis. A slight reduction in trapezial bone stock was observed, but the primary indication for trapeziectomy was the presence of STT arthritis, which represented the predominant pathological finding and guided the choice of suspension arthroplasty.
Preoperative radiographs illustrating the bilateral TMC pathology are shown in Figure 1.

Figure 1.
Preoperative radiographs showing bilateral trapeziometacarpal joint osteoarthritis: grade 3 degeneration with preserved trapezium on the right, and advanced scaphotrapezial–trapeziometacarpal arthritis with a slight reduction in trapezial bone height on the left.
2.1. Right Hand: Trapeziometacarpal Prosthesis
The prosthetic surgery was carried out with the patient in the supine position and a tourniquet applied at the root of the right arm under locoregional anesthesia. The trapeziometacarpal joint was exposed through a lateral surgical approach. The degenerated articular surfaces were resected, and a dual mobility prosthesis (Touch®; Mikai, Italy) was implanted (Figure 2). Capsule closure was performed using absorbable sutures, followed by an intradermal skin suture. A thumb-including bandage was applied for 7 days. After removal of the bandage, a thumb splint was applied, and the patient was encouraged to begin gentle active thumb motion. Fourteen days after surgery, the intradermal sutures were removed, and the patient was allowed to move the thumb freely with a full range of motion.
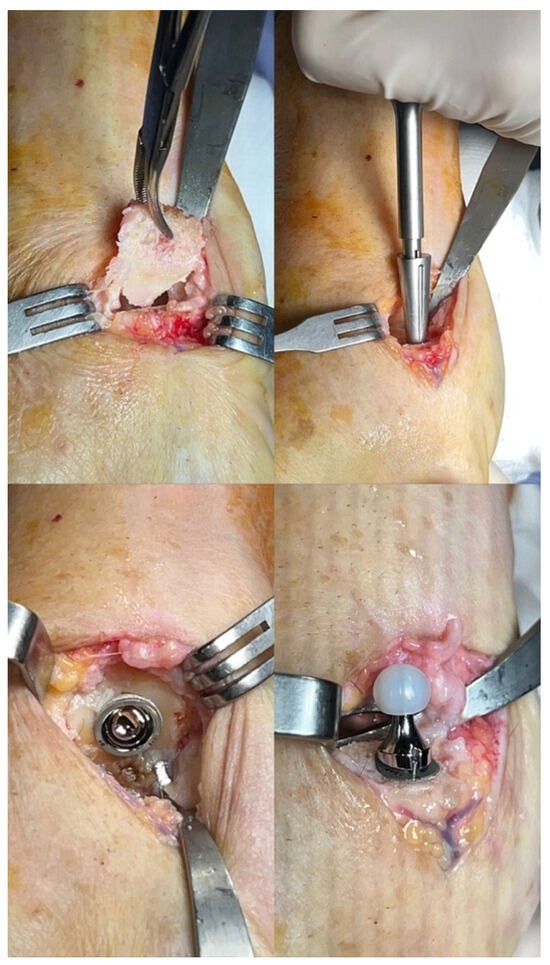
Figure 2.
Intraoperative view showing implantation of the dual mobility prosthesis (Touch®; Mikai, Italy) in the right trapeziometacarpal joint following resection of the degenerated surfaces.
2.2. Left Hand: Trapeziectomy and Suspension Arthroplasty
Using the same positioning and locoregional anesthesia, a lateral approach was used for the left hand. The trapezium was excised completely, and a tendon interposition arthroplasty was performed using a slip of the flexor carpi radialis tendon fixed with an anchor on the base of the first metacarpal bone (Figure 3). The joint capsule and soft tissues were sutured to ensure stability and mobility. The wound was closed in layers and dressed, and a cast was applied, with the wrist and thumb included.
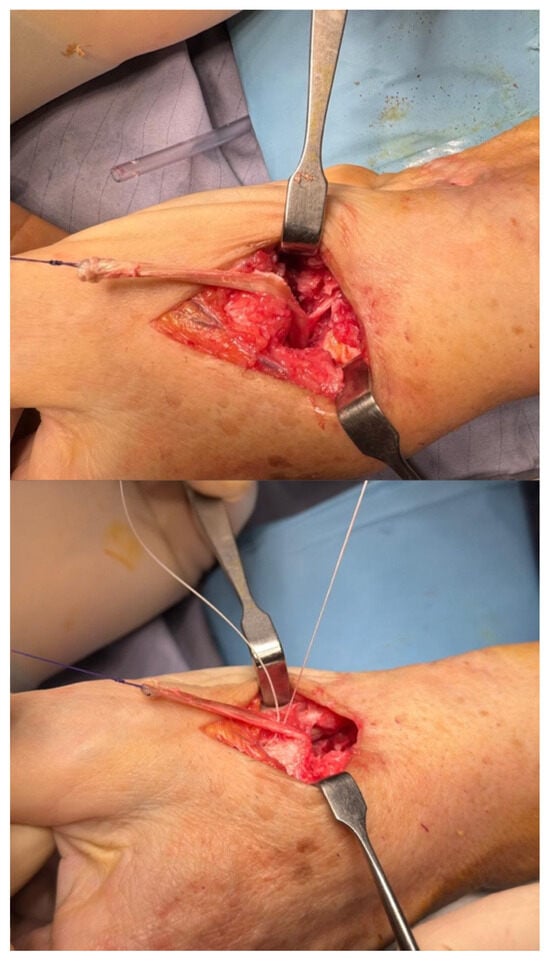
Figure 3.
Intraoperative view during left hand trapeziectomy with tendon interposition arthroplasty. The trapezium is excised, and a slip of the flexor carpi radialis tendon is fixed with an anchor at the base of the first metacarpal to restore joint function. The wound is closed, and a cast is applied with the wrist and thumb immobilized.
A minimally invasive surgical approach of approximately 2.5 cm, as per our technique, was employed and is demonstrated at the end of the procedure (Figure 4). Immediate postoperative radiographs of both procedures are shown in Figure 5.

Figure 4.
Intraoperative view at the end of the procedure demonstrating the minimally invasive surgical approach (approximately 2.5 cm), which characterizes our technique.
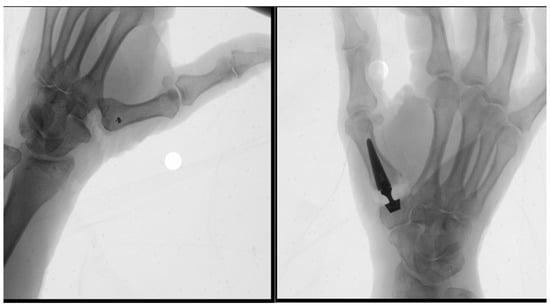
Figure 5.
Immediate postoperative radiographs following the right trapeziometacarpal prosthetic implantation and left trapeziectomy with tendon interposition arthroplasty. Proper positioning of the dual mobility prosthesis and tendon graft is confirmed.
Both hands were immobilized initially with a thumb-including bandage followed by a thumb splint, and active motion was progressively started after wound healing. Formal hand therapy was continued according to functional needs.
Written informed consent was obtained for publication of this case and accompanying images.
2.3. Clinical Evaluation
All clinical evaluations were performed at 1, 3, 6, and 12 months after surgery. We evaluated pain levels with the VAS score preoperatively and postoperatively, and the grip strength with Jamar dynamometers. The return to normal daily activities was investigated using the Quick DASH score, and the patient’s satisfaction was investigated for both hands, using four degrees of satisfaction (very satisfied, satisfied, not satisfied, dissatisfied). The recovery of ROM was evaluated using the Kapandji score for the opposition of the thumb, and the thumb’s extension and abduction were compared on both hands.
Statistical analysis was performed using R software version 4.2.2. (R Foundation for Statistical Computing, Vienna, Austria). Descriptive statistics were used to summarize the data, and paired comparative tests were applied as appropriate based on data distribution. Statistical significance was set at p < 0.05. Given the single-patient design, the analysis is descriptive in nature, and p-values should be interpreted with caution.
3. Results
Grip strength assessments performed with the Jamar dynamometer at 1, 3, 6, and 12 months postoperatively showed consistently higher values in the hand treated with a trapeziometacarpal prosthesis compared to the hand treated with trapeziectomy and suspension arthroplasty (Table 1) (Figure 6). The greatest difference was noted at 3 months, reflecting the earlier functional recovery typically associated with prosthetic implants. By 6 and 12 months, the hand treated with trapeziectomy and suspension arthroplasty showed progressive improvement, although recovery remained slower than in the hand treated with a trapeziometacarpal prosthesis, consistent with the more gradual restoration typically expected after suspension arthroplasty. At 12 months, grip strength improved from 28 to 40 kg (prosthesis) and from 25 to 33 kg (suspension arthroplasty). Statistical analysis, performed using all available data up to the 12-month follow-up, confirmed that the differences between the two treatments were statistically significant.

Table 1.
Grip and pinch strength measurements (in kilograms) recorded at 1, 3, 6, and 12 months postoperatively for the hand treated with a trapeziometacarpal prosthesis and the hand treated with trapeziectomy and suspension arthroplasty. The values demonstrate progressive functional recovery over time, with consistently higher strength observed in the hand treated with the trapeziometacarpal prosthesis. An asterisk marks statistically significant p values. The p-value analysis showed statistically significant results for hand grip (p = 0.003).
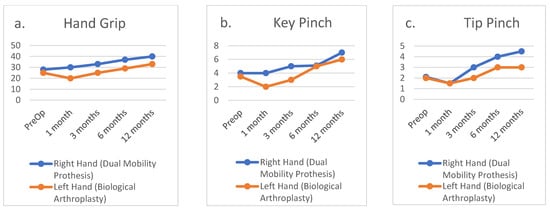
Figure 6.
(a) Hand grip; (b) key pinch; (c) tip pinch.
Pain levels, assessed with the Visual Analogue Scale (VAS), decreased significantly in both hands over time, with a faster and more pronounced reduction observed in the hand treated with a trapeziometacarpal prosthesis. A substantial improvement was already evident at the first postoperative month, confirming the earlier recovery profile typically associated with prosthetic implants. Statistical analysis performed across all follow-up points up to 12 months confirmed that this difference was significant. Functional outcomes, measured using the QuickDASH (Disabilities of the Arm, Shoulder and Hand) score, consistently favored the hand treated with the prosthesis at all time points, indicating lower disability scores and an earlier resumption of daily activities—particularly within the first three months—although this difference did not reach statistical significance. Patient satisfaction, assessed using a four-point scale, was also consistently higher in the hand treated with the trapeziometacarpal prosthesis, with the patient reporting maximal satisfaction at all follow-up evaluations. In contrast, satisfaction with the hand treated with trapeziectomy and suspension arthroplasty improved more gradually over time (Table 2) (Figure 7).

Table 2.
Patient-reported outcomes included pain levels measured using the Visual Analogue Scale (VAS), functional status assessed with the QuickDASH score, and satisfaction ratings for the hand treated with a trapeziometacarpal prosthesis and the hand treated with trapeziectomy and suspension arthroplasty at 1, 3, 6, and 12 months postoperatively. An asterisk marks statistically significant p values. Paired comparisons were performed at each follow-up interval up to 12 months, showing a significant difference only for the VAS.
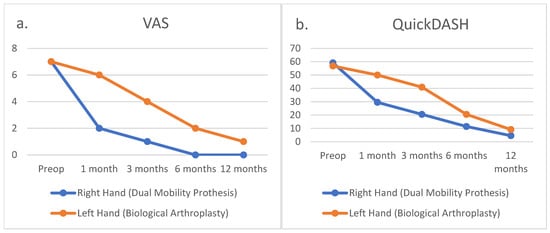
Figure 7.
(a) VAS scores; (b) QuickDASH scores.
Range of motion (ROM) recovery was assessed using the Kapandji score for thumb opposition and by directly comparing thumb abduction and extension between the two hands. The hand treated with a trapeziometacarpal prosthesis showed higher Kapandji scores during the early postoperative period; however, the hand treated with trapeziectomy and suspension arthroplasty achieved comparable opposition by 9–12 months. In contrast, differences in thumb abduction and extension consistently favored the hand treated with the trapeziometacarpal prosthesis throughout follow-up. Statistical analysis performed across all data up to 12 months confirmed that these differences were significant for both abduction and extension, while no significant difference was observed for the Kapandji score (Table 3) (Figure 8).

Table 3.
Kapandji scores and measurements of thumb abduction and extension recorded at 1, 3, 6, and 12 months postoperatively for the hand treated with a trapeziometacarpal prosthesis and the hand treated with trapeziectomy and suspension arthroplasty. The values demonstrate progressive functional recovery over time, with earlier and consistently greater improvements observed on the hand treated with the trapeziometacarpal prosthesis. An asterisk marks statistically significant p values. Statistical analysis showed significant results for Thumb abduction (p < 0.001) and Thumb extension (p = 0.004).
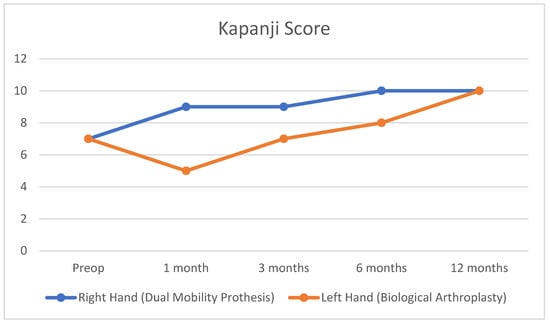
Figure 8.
Kapandji scores.
Taken together, both objective (grip strength, ROM) and subjective (VAS, QuickDASH, satisfaction) outcomes indicate a faster and more predictable functional recovery on the hand treated with the trapeziometacarpal prosthesis. These findings underscore the importance of comprehensive follow-up assessments in capturing not only radiological outcomes but also real-world functional and patient-centered measures of surgical success.
4. Discussion
The management of trapeziometacarpal osteoarthritis continues to be a topic of significant discussion, as both biological arthroplasty and prosthetic replacement have demonstrated effectiveness in treating patients with advanced disease. Each method has its unique set of benefits and drawbacks, making the selection of the appropriate procedure largely reliant on individual patient characteristics, including age, level of activity, and specific anatomical factors.
Biological arthroplasty, which generally involves the reconstruction of ligaments and suspension or interposition of tendons, is a technique designed to facilitate pain recovery through a noninvasive approach (trapeziectomy and tendon graft). Its objective is pain recovery, restoring stability and function by enhancing or reconstructing the existing soft tissues [8]. A notable benefit of biological arthroplasty is that it does not involve the use of an implant, thereby eliminating the associated risks of implant failure, loosening, or dislocation. This technique is often more suitable for younger, more active patients who prioritize the preservation of natural joint motion [9]. However, the recovery period following biological arthroplasty can be lengthy, requiring patients to undergo extended periods of immobilization and rehabilitation to achieve full functional recovery. Additionally, there may be inconsistencies in long-term outcomes, particularly concerning the potential recurrence of pain or the reduction in thumb strength.
Conversely, the trapeziometacarpal prosthesis provides the advantage of achieving immediate joint stability and pain relief [10]. Contemporary designs, including dual mobility prostheses, have enhanced the range of motion and minimized the risk of dislocation, offering a stable and long-lasting solution. Generally, prosthetic replacement tends to be linked with a quicker recovery process [11] compared to biological arthroplasty, enabling patients to regain functionality and return to their daily activities sooner. In this case, the patient underwent simultaneous surgical interventions, allowing for a direct comparison of recovery and outcomes between biological arthroplasty on the left hand and trapeziometacarpal prosthesis on the right. Both surgical techniques effectively resolve pain and restore function; however, significant differences in the recovery process were noted. The hand treated with a trapeziometacarpal prosthesis demonstrated a faster return to function and required less intensive postoperative rehabilitation. In contrast, the hand treated with trapeziectomy and suspension arthroplasty showed a slower recovery profile, necessitating a more structured physiotherapy program to restore strength and mobility. These findings highlight that both techniques are effective and suitable options for managing trapeziometacarpal osteoarthritis, although they differ in terms of recovery trajectory and long-term functional implications.
In our case, the use of a contemporary dual mobility prosthesis likely contributed to the excellent early functional outcomes and the absence of complications such as dislocation or implant migration. Conversely, recovery of the hand treated with trapeziectomy and suspension arthroplasty was slower, and a minor complication—left wrist synovitis—was reported 12 months postoperatively, successfully managed with conservative treatment through local corticosteroid injections. These observations suggest that emerging prosthetic technologies may further refine the indications for total joint replacement in TMC osteoarthritis and potentially broaden its application to a wider patient population.
Although limited by its single-patient design, the outcomes observed closely align with those reported in larger studies, supporting the consistency and clinical relevance of our findings.
5. Conclusions
The choice between trapeziectomy with suspension arthroplasty and trapeziometacarpal prosthesis should be carefully tailored to the individual characteristics, demands, and expectations of each patient. In this case, although both surgical techniques effectively reduced pain and restored thumb function, the hand treated with a trapeziometacarpal prosthesis demonstrated superior outcomes in terms of grip strength, faster functional recovery, and earlier return to daily activities. These findings align with the growing body of literature supporting the advantages of prosthetic implants, particularly for patients who require a quicker return to function. Overall, our results emphasize the importance of individualized surgical planning, with trapeziometacarpal prosthesis representing a promising option, especially for patients with higher functional requirements.
Author Contributions
Conceptualization, M.G.; Methodology, S.P.; Validation, R.D.V.; Formal analysis, S.C.; Data curation, C.B.; Writing—original draft preparation, A.P.; Writing—review and editing, C.B.; Visualization, S.C.; Supervision, M.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
According to the Italian legislative framework (Italian D.Lgs. 211/2003 and related national guidance), retrospective single-patient case reports are not considered clinical research and therefore do not require approval from an Ethics Committee/Institutional Review Board. Written informed consent was obtained from the patient for the publication of this case report and all accompanying images.
Informed Consent Statement
Written informed consent was obtained.
Data Availability Statement
No new data were created or analyzed in this stugy. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kanak, M.; Rokicki, R.; Wojna, J. Trapeziometacarpal Osteoarthritis Anatomy, Biomechanics, Epidemiology, and Diagnosis. Ortop. Traumatol. Rehabil. 2022, 24, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Gay, A.M.; Cerlier, A.; Iniesta, A.; Legré, R. Surgery for trapeziometacarpal osteoarthritis. Hand Surg. Rehabil. 2016, 35, 238–249. [Google Scholar] [CrossRef] [PubMed]
- Kirkeby, L.; Frost, P.; Svendsen, S.W.; Hansen, T.B. Revision rates of trapeziometacarpal total joint arthroplasty in relation to occupational hand force requirements. J. Hand Surg. Eur. Vol. 2021, 46, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Falkner, F.; Tümkaya, M.A.; Thomas, B.; Bigdeli, A.K.; Kneser, U.; Harhaus, L.; Bickert, B. Konservative Therapieverfahren zur Behandlung der symptomatischen Daumensattelgelenksarthrose [Conservative treatment options for symptomatic thumb trapeziometacarpal joint osteoarthritis]. Orthopade 2022, 51, 2–8. (In German) [Google Scholar] [CrossRef] [PubMed]
- Jörheim, M.; Isaxon, I.; Flondell, M.; Kalén, P.; Atroshi, I. Short-term outcomes of trapeziometacarpal artelon implant compared with tendon suspension interposition arthroplasty for osteoarthritis: A matched cohort study. J. Hand Surg. Am. 2009, 34, 1381–1387. [Google Scholar] [CrossRef] [PubMed]
- Remy, S.; Detrembleur, C.; Libouton, X.; Bonnelance, M.; Barbier, O. Trapeziometacarpal prosthesis: An updated systematic review. Hand Surg. Rehabil. 2020, 39, 492–501. [Google Scholar] [CrossRef] [PubMed]
- Falkner, F.; Tümkaya, A.M.; Thomas, B.; Böcker, A.; Aman, M.; Bickert, B.; Harhaus, L.; Panzram, B. Resection arthroplasty versus dual mobility prosthesis in the treatment of trapeziometacarpal joint osteoarthritis: A 3 year non-randomized prospective study. J. Orthop. 2024, 57, 72–78. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guzzini, M.; Perugia, D.; Proietti, L.; Iorio, R.; Mazza, D.; Masi, V.; Ferretti, A. Suspension arthroplasty versus interposition arthroplasty in the treatment of trapeziometacarpal osteoarthritis: A clinical and magnetic resonance imaging study. Int. Orthop. 2019, 43, 647–651. [Google Scholar] [CrossRef] [PubMed]
- Langer, M.F.; Grünert, J.G.; Unglaub, F.; Richter, M.; van Schoonhoven, J.; Oeckenpöhler, S. Resektionsarthroplastik des Daumensattelgelenks mit ihren Varianten [Resection arthoplasty of the trapezium with ligament reconstruction and tendon interposition and variation]. Oper. Orthop. Traumatol. 2021, 33, 183–199. [Google Scholar] [CrossRef] [PubMed]
- Guzzini, M.; Arioli, L.; Annibaldi, A.; Pecchia, S.; Latini, F.; Ferretti, A. Interposition Arthroplasty versus Dual Cup Mobility Prosthesis in Treatment of Trapeziometacarpal Joint Osteoarthritis: A Prospective Randomized Study. Hand 2024, 19, 1260–1268. [Google Scholar] [CrossRef] [PubMed]
- Herren, D.B.; Marks, M.; Neumeister, S.; Schindele, S. Short-term recovery after implant versus resection arthroplasty in trapeziometacarpal joint osteoarthritis. J. Hand Surg. Eur. Vol. 2023, 48, 1048–1055. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).