2. Case Report
A 76-year-old female presented to the outpatient otolaryngology clinic with a four year history of gradually progressive right periorbital swelling with associated diplopia upon upward gaze. She noted intermittent mild pain in the bilateral frontal regions for several years, which had been evaluated at several different institutions without intervention. She had not received any prior sinonasal imaging. She denied sinonasal symptoms including nasal obstruction or rhinorrhea. She had a remote history of prior nasal fractures and right orbital injury over 50 years prior, for which she did not receive treatment. The patient had no previous sinonasal surgeries or procedures.
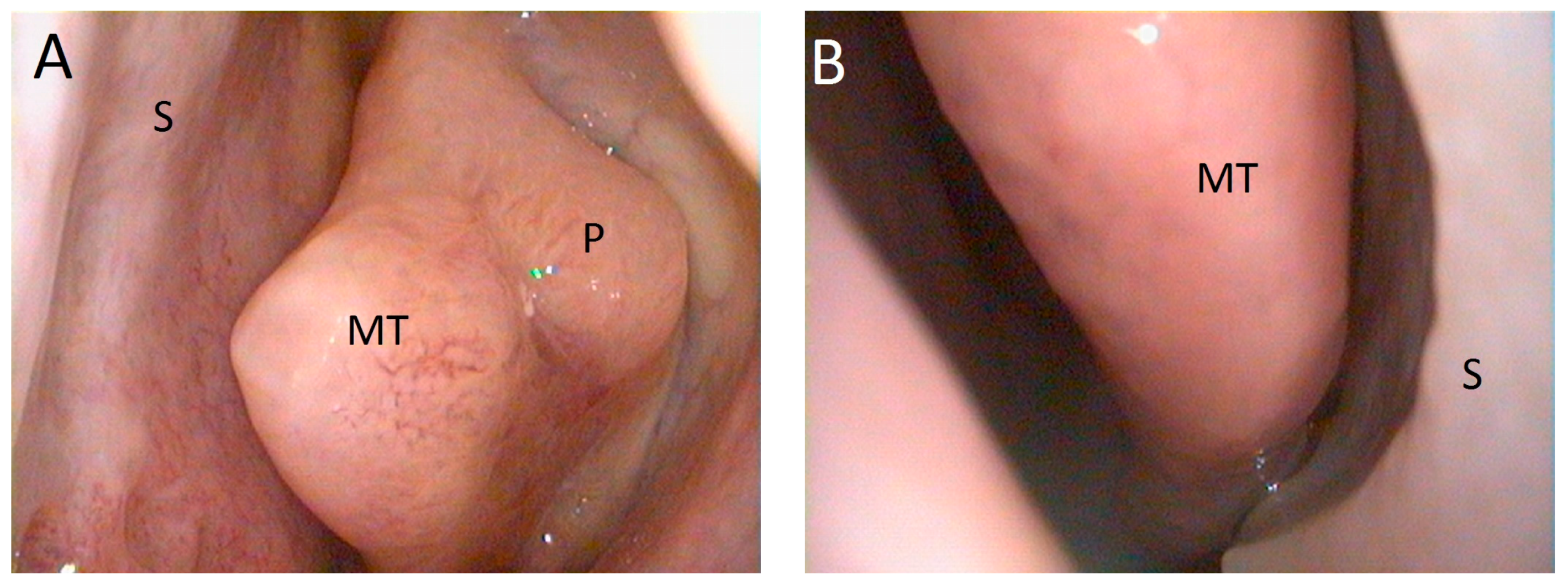
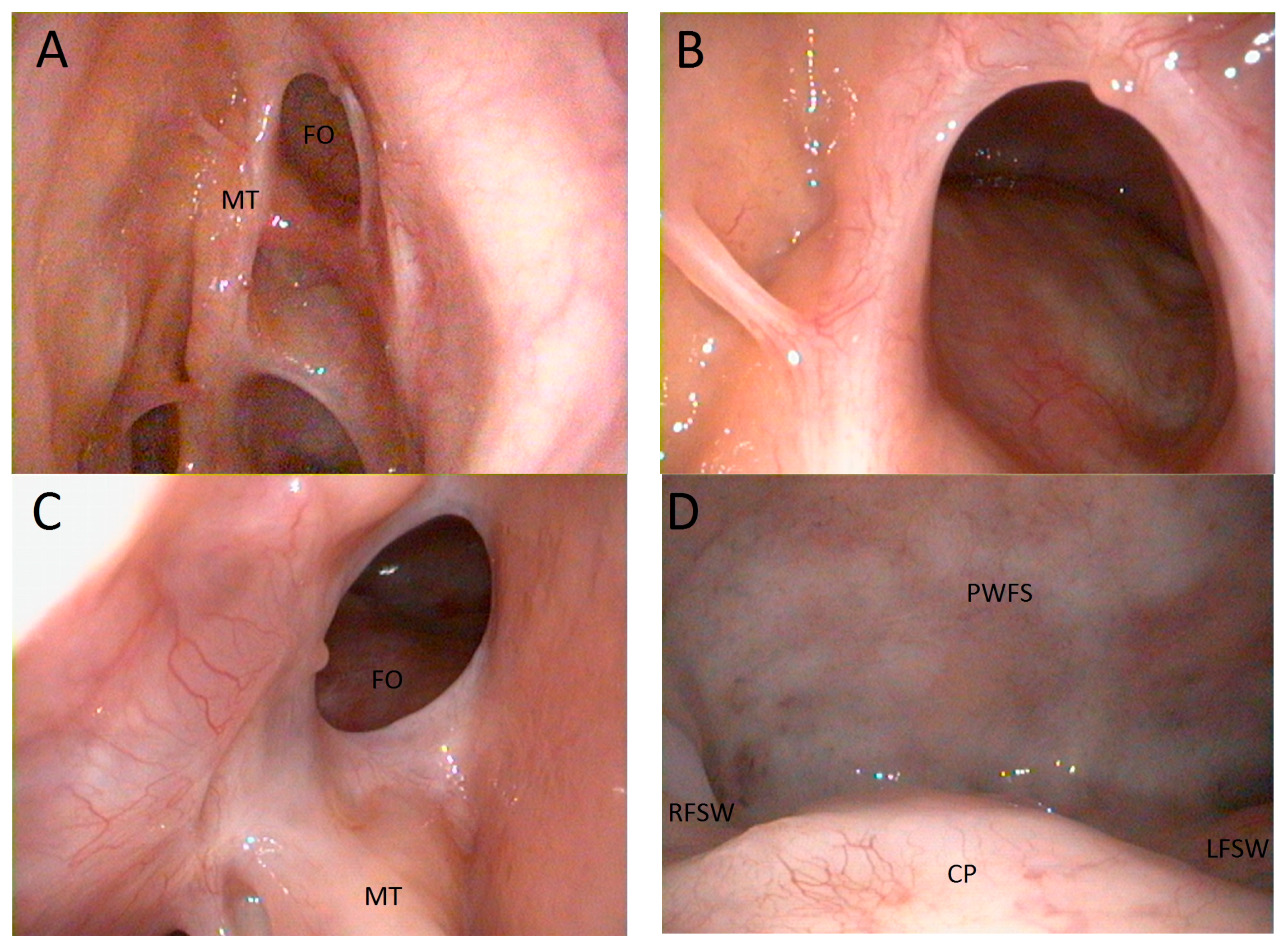
Physical examination revealed a compressible, mildly tender, fluctuant mass within the soft tissues of the right superior orbit with prominent inferior displacement of the right globe. Nasal endoscopy revealed polyposis in the left middle meatus, with a normal appearance on the right (
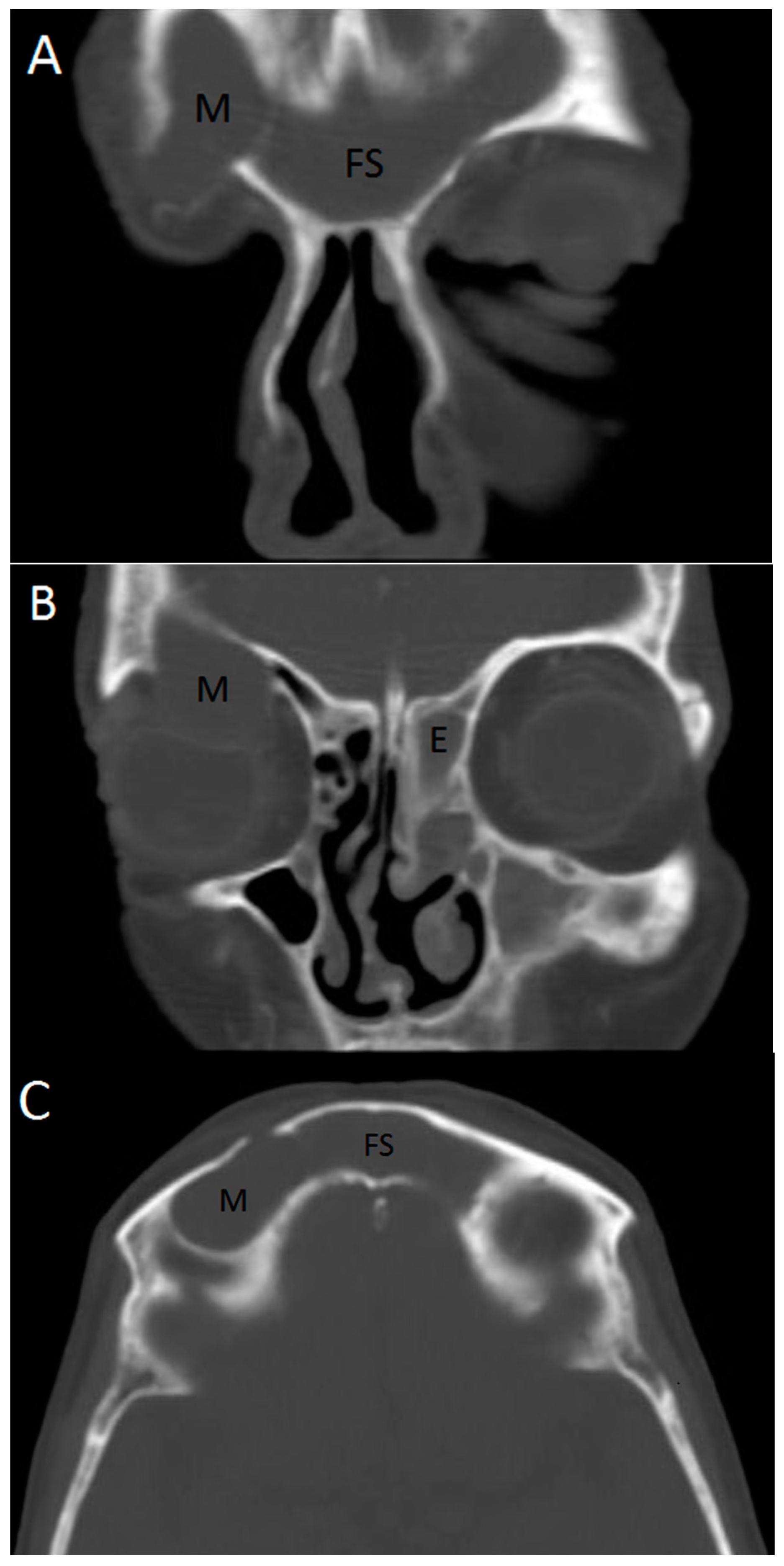
Figure 1). Computerized tomography (CT) imaging of the sinuses displayed a cystic mass lateral to the right frontal sinus, with complete opacification of both frontal sinuses, as well as the left maxillary sinus and left anterior ethmoid cells (
Figure 2). The sphenoid sinuses, right ethmoid sinus, and right maxillary sinus were clear. Magnetic-resonance imaging (MRI) of the orbits confirmed the presence of a mucus-filled extra-axial mass compressing the right globe. Ophthalmologic evaluation was within normal limits, with the exception of hypoglobus.
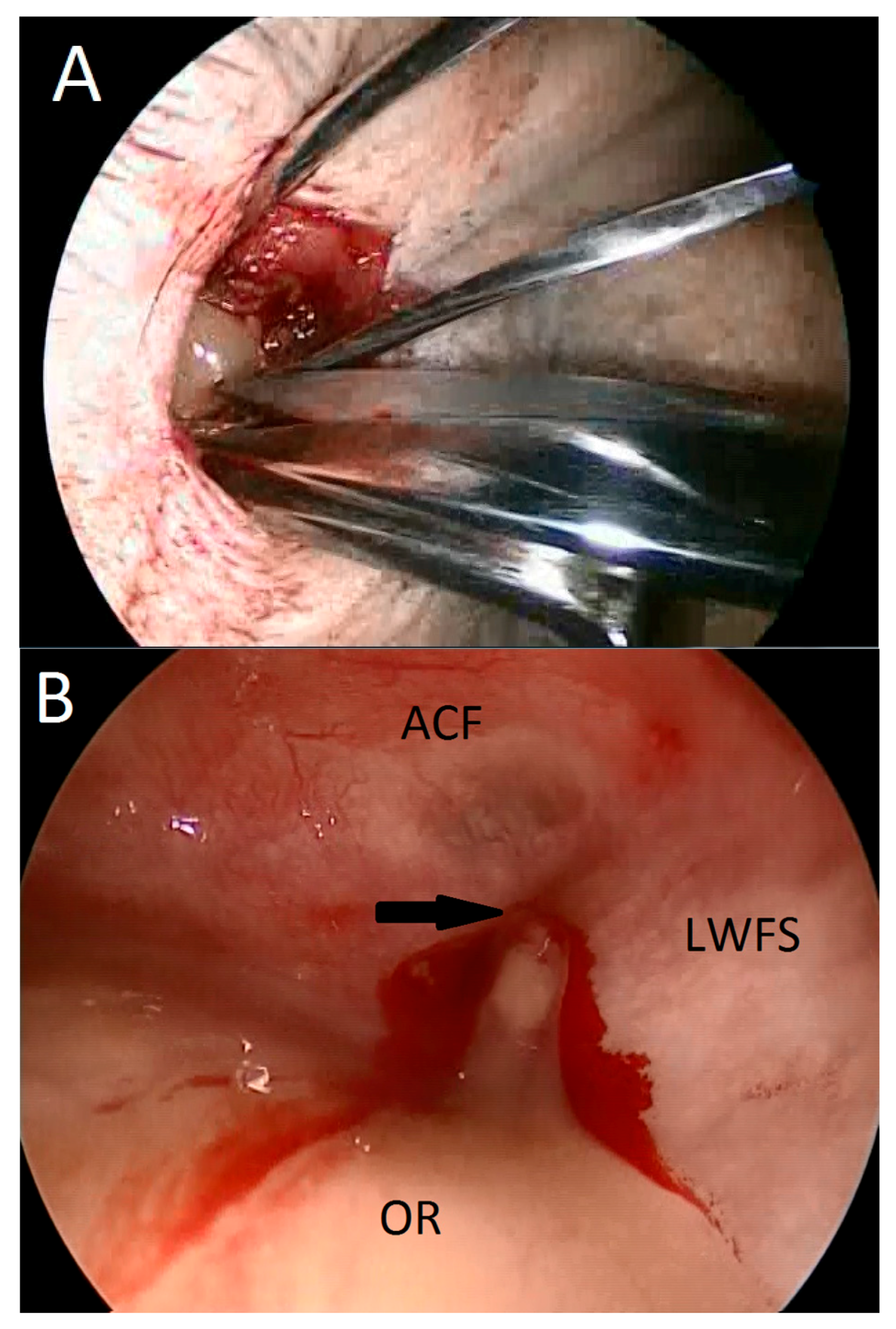
The patient underwent surgical treatment via a combined external and endoscopic approach. This was motivated by preoperative imaging studies, which indicated a mucocele that occupied a separate compartment which may not be adequately decompressed by frontal sinusotomy. The mucocele was drained via a right brow incision with release of purulent mucus (
Figure 3A). Endoscopic visualization of the mucocele cavity revealed a pinpoint communication with the lateral wall of the frontal sinus (
Figure 3B). Bilateral endoscopic frontal sinus exploration with Draf IIB sinusotomy was performed with a 70-degree endoscope and non-powered instrumentation. This revealed a common frontal sinus cavity filled with purulent material, in which the intersinus septum between right and left frontal sinuses was absent. The right frontal ostium could not be identified, whereas the left frontal ostium was occluded by polyposis. Intraoperative electromagnetic image-guided navigation (Medtronic, Minneapolis, MN, USA) was used to confirm the location of the frontal ostia and ensure completeness of the procedure. Left-sided ethmoidectomy and maxillary antrostomy with polypectomy was also performed. Pathologic evaluation was consistent with benign polyposis and chronic sinusitis.
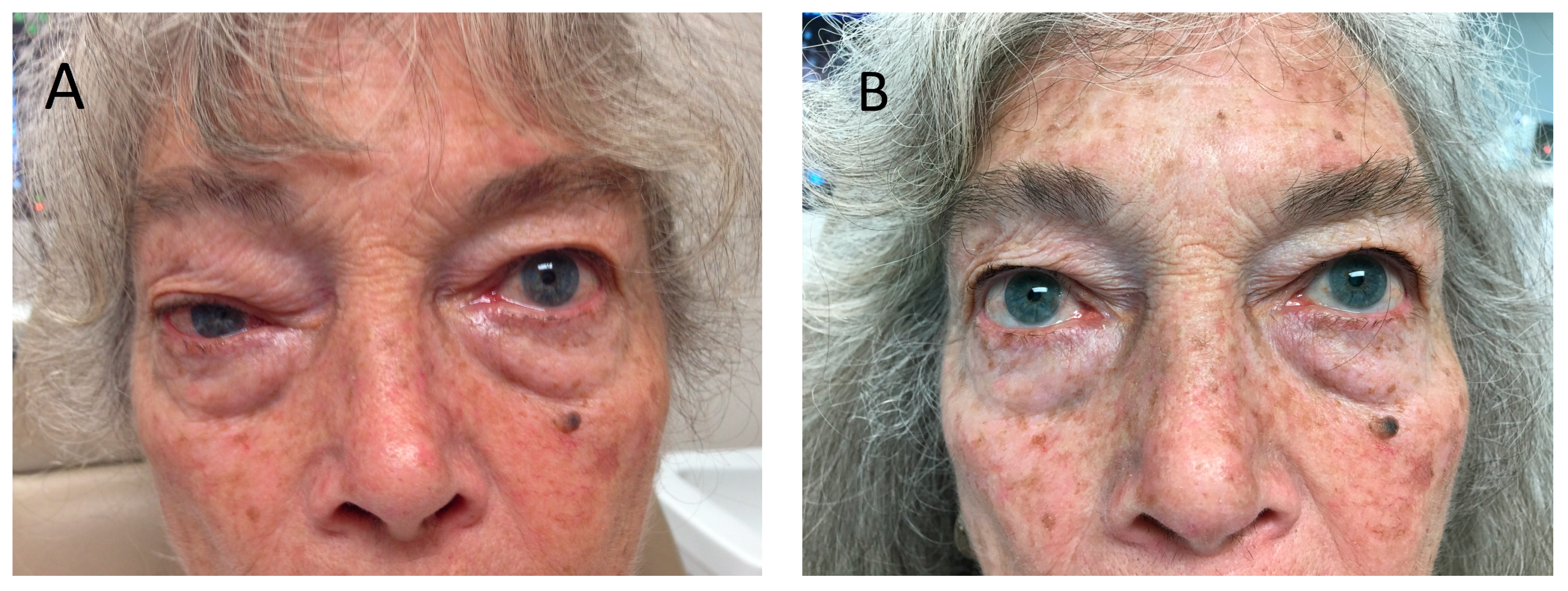
The patient tolerated the procedure well. At four weeks postoperatively, her vision had normalized with resolution of diplopia and no residual swelling (
Figure 4). After one year she remained asymptomatic with full healing of the surgical site and common frontal cavity (
Figure 5).
3. Discussion
Longstanding disruption of a paranasal sinus outflow tract can lead to inadequate mucus clearance and mucocele formation. These epithelium-lined cysts are locally erosive due to pressure exerted on surrounding bony structures. Mucocele is an uncommon occurrence, and is usually seen as a complication of prior sinus surgery. Other contributing factors include mucosal atopy, polyposis, neoplasia, and chronic rhinosinusitis. A history of trauma is occasionally elicited in patients with a sinus mucocele, often years or decades after the injury [
3]. Mucocele that occurs in the frontal sinus may erode inferiorly into the orbit, producing orbital edema, diplopia, ptosis, enophthalmos, hypoglobus, or retro-orbital pain [
4]. Sinonasal symptoms are typically absent. The differential diagnosis includes orbital cellulitis, abscess, orbital pseudotumor, thyroid ophthalmopathy, and lacrimal gland neoplasm.
The present case is instructive in multiple respects. First, although a mucocele typically arises adjacent to a diseased sinus, in this case the mucocele occurred contralateral to the site of sinus disease. Polyposis represents a subtype of chronic rhinosinusitis which is often bilateral, though may also be unilateral. In this case, polyposis and marked sinus inflammation were present in the left ethmoid sinus, whereas the right ethmoid sinus was completely normal. The polyposis on the left produced obstruction of mucus in the left frontal sinus, which is presumed over the course of time to have eroded the inter-sinus septum to allow extension into the right frontal sinus. Attenuation and resorption of bone may be observed in the setting of chronic sinusitis, in which chemical mediators of inflammation activate local osteoclastic activity [
5,
6,
7].
Secondly, in the presence of normal sinus anatomy, the crossover of mucus from left to right frontal sinuses would be expected to drain through the right frontal duct and into the nose. However, the prior history of right orbital and nasal trauma contributed to obstruction of the right frontal duct, so that retrograde drainage could not occur. The resulting mucus accumulation instead eroded through the lateral wall of the right frontal sinus to create a mucocele above the right orbit, which in turn eroded inferiorly into the orbit. Thirdly, the prolonged delay in diagnosis was most likely enabled by a delay in obtaining imaging of the orbit and sinuses. Irrespective of history of trauma, unilateral swelling around the face or eye that does not resolve with medical therapy should be evaluated with imaging studies.
Sinus CT is the preferred modality for the diagnosis of mucocele [
8]. However, derangements of sinus drainage are often not appreciated on imaging, since the bony laminae may lie oblique to the plane of the image slices. MRI is necessary to rule out other possible pathologies, including meningoencephalocele [
4].
Definitive treatment of a mucocele is surgical, which may include trephination, osteoplastic flap, endoscopic sinusotomy, or a combination of approaches, depending on the location and size of the lesion. The goals of treatment are to assure complete removal of mucus and prevent recurrence. Contemporary practice favors an endoscopic approach to frontal sinusotomy, with open approaches reserved for specific cases with unfavorable anatomy, scarring, and disease in the far lateral extent of the frontal sinus [
9]. Simple frontal sinusotomy (Draf I, Draf IIA) may provide initial drainage, but may have unclear benefit for long-term ventilation. Extended unilateral frontal sinusotomy (Draf IIB) has been shown to effectively treat frontal sinus mucocele without the potential risk of more aggressive frontal approaches [
10]. Endoscopic modified Lothrop procedure (Draf III) is the most aggressive endoscopic approach, and is appropriate for cases of bilateral mucocele with hyperostosis where long-term frontal sinus patency is not anticipated from less aggressive approaches [
9].