Concealed Peritonitis Due to Stomach Perforation from a Fish Otolith: A Case Report
Abstract
1. Introduction
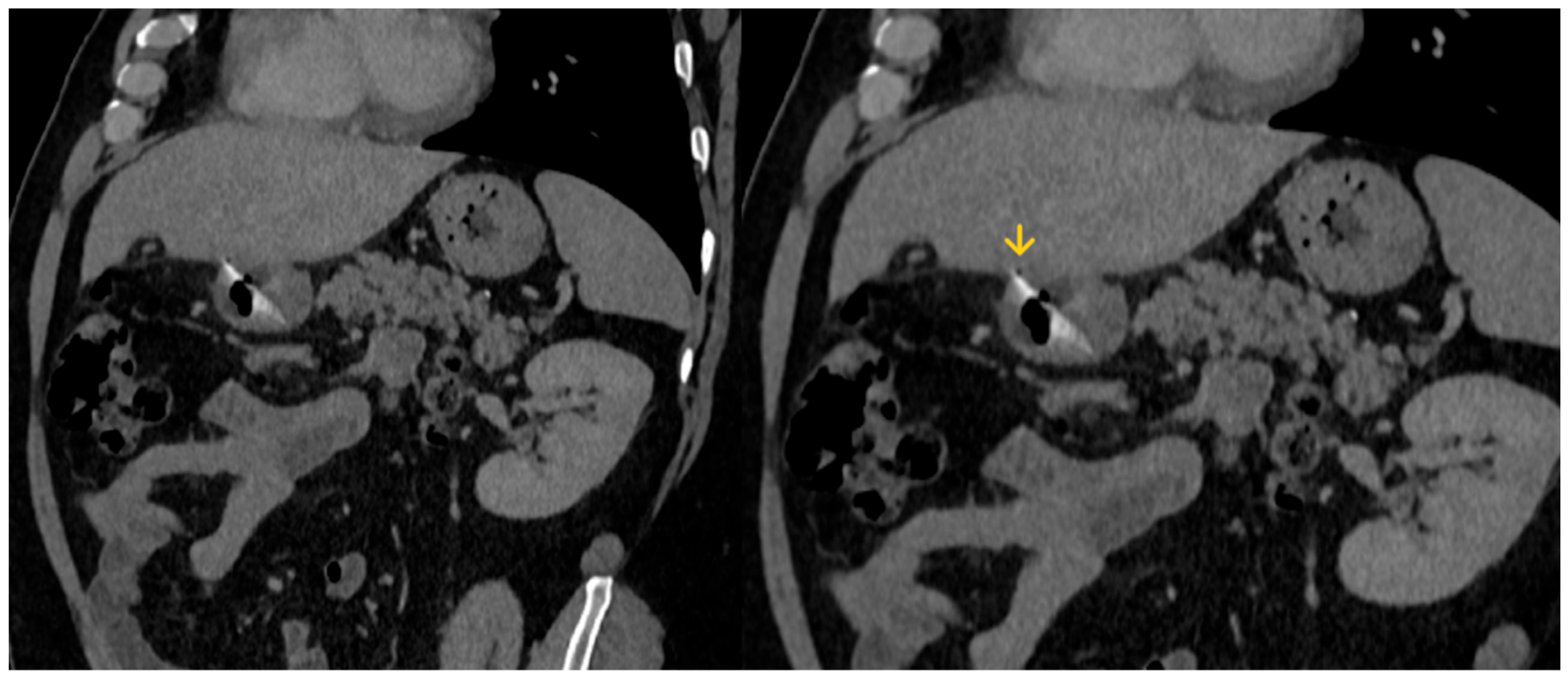
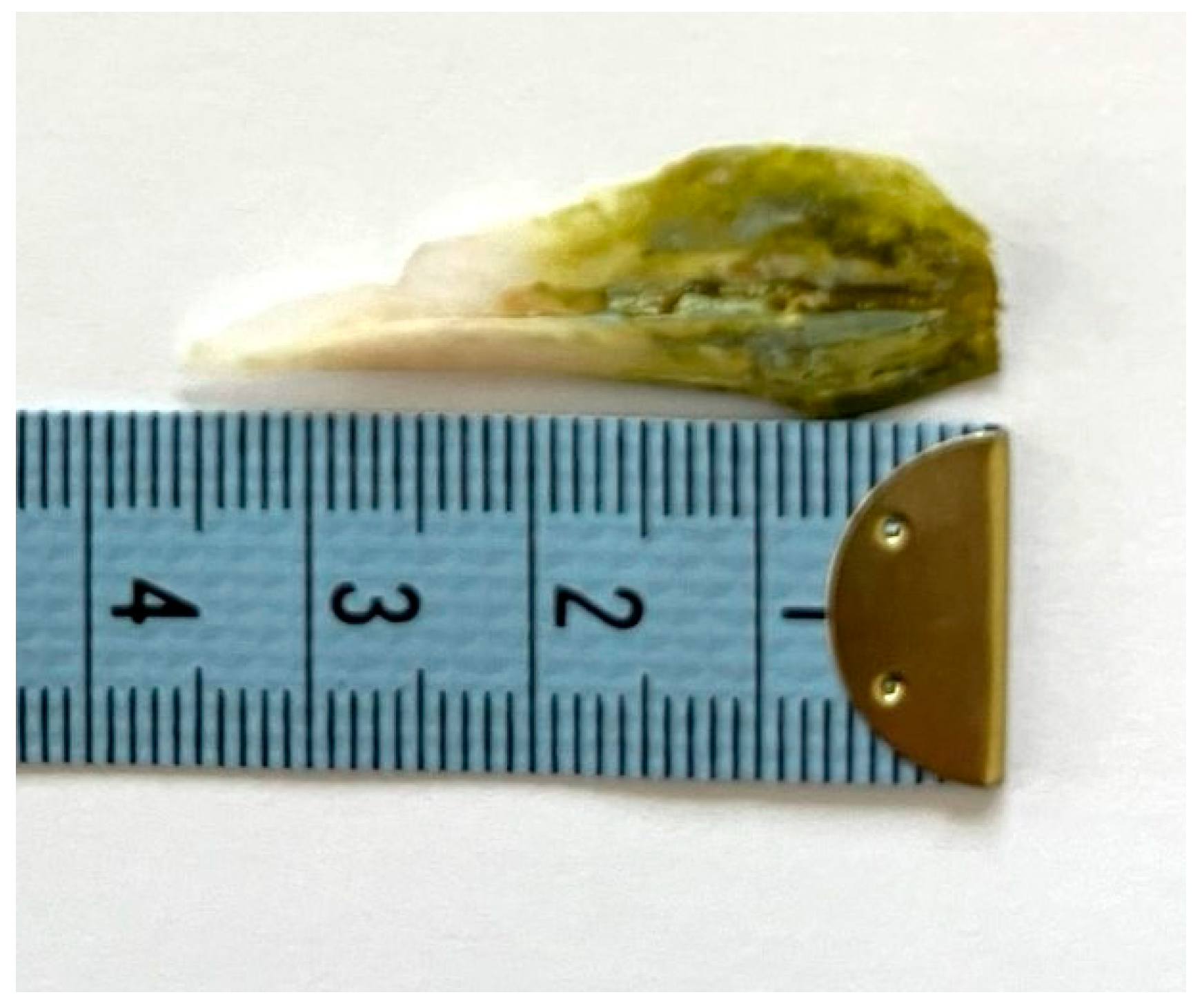
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tomono, N.; Niiro, N.; Fujita, Y.; Amagai, T. Emergency Laparoscopic Removal of an Ingested Fishbone Perforating the Stomach After Endoscopy: A Case Report. Cureus 2025, 17, e81060. [Google Scholar] [CrossRef]
- Abuzneid, Y.S.; Alzeerelhouseini, H.I.A.; Rabee, A.; Aqel, W.; Ayyad, R.F.; Asad, T.M.; Abukarsh, R. Double Magnet Ingestion Causing Intestinal Perforation with Peritonitis: Case Report and Review of the Literature. Case Rep. Surg. 2022, 2022, 4348787. [Google Scholar] [CrossRef]
- Fleres, F.; Ieni, A.; Saladino, E.; Speciale, G.; Aspromonte, M.; Cannaò, A.; Macrì, A. Rectal Perforation by Inadvertent Ingestion of a Blister Pack: A Case Report and Review of Literature. World J. Clin. Cases 2018, 6, 384–392. [Google Scholar] [CrossRef]
- Tavarez, M.M.; Saladino, R.A.; Gaines, B.A.; Manole, M.D. Prevalence, Clinical Features and Management of Pediatric Magnetic Foreign Body Ingestions. J. Emerg. Med. 2013, 44, 261–268. [Google Scholar] [CrossRef]
- Hauser, H.; Pfeifer, J.; Uranüs, S.; Klimpfinger, M. Perforation of the Cecum by a Toothpick. Case Report and Review of the Literature. Langenbecks Arch. Chir. 1994, 379, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Gardner, J.A. Perforation of the Sigmoid Colon by Swallowed Chicken Bone: Case Reports and Review of Literature. Int. Surg. 1981, 66, 181–183. [Google Scholar]
- AlAbdullah, H.S.; Kabbani, M.S.; Ismail, S.R.; Hijaz, O.; AlGhamdi, A. Esophageal Perforation with Mediastinitis Leading to Mycotic Aortic Pseudoaneurysm in a Pediatric Patient: A Complication of Sharp Foreign Body Ingestion. SAGE Open Med. Case Rep. 2025, 13, 2050313X251366363. [Google Scholar] [CrossRef]
- Liu, B.; Kuang, S.; Cao, M.; Li, X. Esophageal Foreign Bodies: A Retrospective Analysis of 275 Cases. J. Thorac. Dis. 2025, 17, 4136–4144. [Google Scholar] [CrossRef]
- Letrillart, J.; Talbotec, C.; Payen, E.; Abi-Nader, E.; Lambe, C.; Campeotto, F.; Ronconi, M.; Ruemmele, F.; Simon, F.; Thierry, B.; et al. Oesophageal Impaction of Button Batteries in Children: A Tertiary Centre Experience. Arch. Dis. Child. 2025, 110, 997–1002. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Liu, H.; Shu, X.; Liu, X. Risk Factors for the Poor Prognosis of Benign Esophageal Perforation: 8-Year Experience. BMC Gastroenterol. 2022, 22, 537. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Baek, S.-E.; Lee, C.W.; Kim, Y.C.; Kim, M.-J. Foreign Body Ingestion: Radiologic Evaluation, Findings, and Management. Korean J. Radiol. 2025, 26, 638–649. [Google Scholar] [CrossRef] [PubMed]
- Arcia, A.; Muñoz, G.A.; Jimenez, G.E.; Albuja, M.G.; Yumbla, T.S.; Venegas, O.H.; Velasco, A.G.; Parrales, D.; Molina, G.A. Fishbone Perforation of the Stomach into the Lesser Sac and Pancreas with Abscess, a Fishy Business. J. Surg. Case Rep. 2024, 2024, rjae787. [Google Scholar] [CrossRef]
- Abboud, B.; Dar, R.; Bramnick, Z.; Farraj, M. Gastric Perforation Secondary to Prolonged Multiple Foreign Body Ingestions in a Patient with Schizophrenia. Isr. Med. Assoc. J. IMAJ 2024, 26, 52–53. [Google Scholar] [PubMed]
- Peyron, P.-A.; Villard, C.; Baccino, E. Fatal Bowel Perforation Caused by Ingestion of High-Powered Magnets in a 6-Year-Old Boy. Int. J. Legal Med. 2024, 138, 1659–1662. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Fang, W.; Chen, Z.; Tang, S. Bowel Perforation Caused by Foreign Body Ingestion Presenting as Intestinal Obstruction: A Case Report Highlighting the Importance of Early Diagnosis. Ann. Med. Surg. 2025, 87, 5205–5208. [Google Scholar] [CrossRef]
- Claassens, E.L.; van Berckel, M.M.G.; Wevers, K.P. A Case Report of a Sigmoid Perforation within an Inguinoscrotal Hernia Sac Caused by Ingestion of a Chicken Wishbone. Int. J. Surg. Case Rep. 2025, 128, 111062. [Google Scholar] [CrossRef]
- Okumura, M.; Koga, H.; Eguchi, H.; Sato, N.; Utsunomiya, R.; Wakahara, Y.; Morimoto, K.; Sugiyama, K. Ascending Colon Perforation by a Migrated Pancreatic Spontaneous Dislodgment Stent: A Case Report. Clin. J. Gastroenterol. 2025, 18, 383–388. [Google Scholar] [CrossRef]
- Dupont, D.H.; Umejiego, L.M.; Satoskar, S.; Soumya, N.; Rosa Santana, M.; Sikka, A.; Ayele, N.; Riera Gonzalez, C.; Bahadur, N.; Singh, A. Fishbone Foreign Body Ingestion with Gastric Impaction and Intestinal Micro-Perforation in an Adult Female: A Case Report. Cureus 2024, 16, e72099. [Google Scholar] [CrossRef]
- Mokbul, M.I.; Roy, S.; Roy, A.N.; Shrestha, A.; Nawys, M. Not Your Typical Abdominal Pain: Case Report of a Fisherman Presenting to the Trauma & Emergency Surgery Department with Intestinal Perforation Due to an Eel Fish. Int. J. Surg. Case Rep. 2024, 124, 110401. [Google Scholar] [CrossRef]
- Panday, B.; Bhatta, O.P.; Gyawali, P.; Dangol, R.S.; Joshi, M.D.; Neupane, B.R. Ileal Perforation Peritonitis Secondary to Accidental Ingestion of a Chicken Bone: A Case Report. Int. J. Surg. Case Rep. 2024, 123, 110284. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Pu, T.-W. Colon Perforation with Severe Peritonitis Caused by Erotic Toy Insertion and Treated Using Vacuum-Assisted Closure: A Case Report. World J. Clin. Cases 2024, 12, 3548–3554. [Google Scholar] [CrossRef]
- Ndoye, N.A.; Welle, I.B.; Lamega, B.; Diawara, A.; Zeng, F.T.A.; Ngom, G. Ileal Perforation Peritonitis Secondary to Ingestion of Magnetic Beads in the Older Child: A Case Report. Int. J. Surg. Case Rep. 2024, 121, 109915. [Google Scholar] [CrossRef]
- Mejri, A.; Yaacoubi, J.; Mseddi, M.A.; Omry, A. Gastrointestinal Perforations by Ingested Foreign Bodies: A Preoperative Diagnostic Flowchart-Based Experience. A Case Series Report. Int. J. Surg. Case Rep. 2022, 95, 107216. [Google Scholar] [CrossRef]
- Zamary, K.R.; Davis, J.W.; Ament, E.E.; Dirks, R.C.; Garry, J.E. This Too Shall Pass: A Study of Ingested Sharp Foreign Bodies. J. Trauma Acute Care Surg. 2017, 82, 150–155. [Google Scholar] [CrossRef]
- Demiroren, K. Management of Gastrointestinal Foreign Bodies with Brief Review of the Guidelines. Pediatr. Gastroenterol. Hepatol. Nutr. 2023, 26, 1. [Google Scholar] [CrossRef]
- Odeghe, E.; Osueni, A.; Owoseni, O.O.; Adeniyi, F.; Lesi, O. Upper Gastrointestinal Bleeding Secondary to an Incidental, Impacted Foreign Body in the Duodenum. Cureus 2020, 12, e6971. [Google Scholar] [CrossRef]
- Ambe, P.; Weber, S.A.; Schauer, M.; Knoefel, W.T. Swallowed Foreign Bodies in Adults. Dtsch. Arzteblatt Int. 2012, 109, 869–875. [Google Scholar] [CrossRef]
- Ebrahimi, M.; Malmir, J.; Mahmoudi-Gharaee, A.; Foroughian, M. A Rare Case of Gastrointestinal Tract Foreign Body; Glassy Stomach. Emerg. Tehran Iran 2017, 5, e44. [Google Scholar]
- Almoudaris, A.M.; Chow, A.; Kaneria, S.; Jiyad, Z.; Hadjiminas, D.J. Fish Bone Perforation Mimicking Acute Appendicitis. J. Med. Cases 2011, 2, 296–299. [Google Scholar] [CrossRef]
- Gopinath, B.; Mishra, P.R.; Dash, N.R.; Kumar, G.; Rajendran, J.; Panwar, R. Ingestion of a Saw-Edge Knife in a Patient with Mental Illness: A Unique and Uncommon Presentation. JEM Rep. 2023, 2, 100044. [Google Scholar] [CrossRef]
- Pîrvulescu, I.C.; Najm, A.; Popa, E.C.; Chiotoroiu, A.L.; Cretoiu, S.M.; Gaspar, B.S. A Unique Case of Foreign Body Acquired by Stabbing and Retained for 7 Years in the Sigmoid Colon. Reports 2023, 6, 24. [Google Scholar] [CrossRef]
- Bhasin, S.; Kachroo, S.; Kumar, V.; Kumar, R.; Chandail, V. 7” Long Knife for 7 Years in the Duodenum: A Rare Case Report and Review of Literature. Int. Surg. J. 2014, 1, 29. [Google Scholar] [CrossRef]
- Li, C.; Yong, C.-C.; Encarnacion, D.D. Duodenal Perforation Nine Months after Accidental Foreign Body Ingestion, a Case Report. BMC Surg. 2019, 19, 132. [Google Scholar] [CrossRef]
- Herrera Hernández, D.; Barragán Jiménez, E.M.; Cano Herrera, P.; Flores García, P.P.; Paternina Gonzalez, I.Y.; Páramo Hernández, D.L.; Burciaga Castañeda, R.; Treviño Flores, J.C. Perforation of the Large Intestine by a Fish Bone Mimicking Cancer: A Rare Case Report. Cureus 2025, 17, e85867. [Google Scholar] [CrossRef]
- Wadie, W.F.; Reskalla, S.I.; Dowidar, N.M. Age and Growth Studies of the Sphyraenidae Family in the Southeastern Mediterranean Based on Otolith Measurements. Folia Morphol. 1989, 37, 38–56. [Google Scholar]
- Bellodi, A.; Asciutto, E.; Malara, D.; Longo, F.; Agus, B.; Bacchiani, C.; Follesa, M.C.; Porcu, C.; Mangano, M.C.; Battaglia, P. Age Determination, Growth and Otolith Shape Analysis of Lepidotrigla Cavillone from Sardinian and Sicilian Waters (Mediterranean Sea). J. Fish Biol. 2025, 107, 1018–1029. [Google Scholar] [CrossRef] [PubMed]
- You, H.; Sweeny, A.; Cooper, M.L.; Von Papen, M.; Innes, J. The Management of Diverticulitis: A Review of the Guidelines. Med. J. Aust. 2019, 211, 421–427. [Google Scholar] [CrossRef]
- Haddad, N.; Kanj, S.S.; Awad, L.S.; Abdallah, D.I.; Moghnieh, R.A. The 2018 Lebanese Society of Infectious Diseases and Clinical Microbiology Guidelines for the Use of Antimicrobial Therapy in Complicated Intra-Abdominal Infections in the Era of Antimicrobial Resistance. BMC Infect. Dis. 2019, 19, 293. [Google Scholar] [CrossRef] [PubMed]
- Lalisang, T.J.M.; Usman, N.; Hendrawidjaya, I.; Handaya, A.Y.; Nasution, S.; Saunar, R.Y.; Loho, T.; Karuniawati, A.; Moenadjat, Y.; Widyahening, I.S. Clinical Practice Guidelines in Complicated Intra-Abdominal Infection 2018: An Indonesian Perspective. Surg. Infect. 2019, 20, 83–90. [Google Scholar] [CrossRef]
- Mazuski, J.E.; Tessier, J.M.; May, A.K.; Sawyer, R.G.; Nadler, E.P.; Rosengart, M.R.; Chang, P.K.; O’Neill, P.J.; Mollen, K.P.; Huston, J.M.; et al. The Surgical Infection Society Revised Guidelines on the Management of Intra-Abdominal Infection. Surg. Infect. 2017, 18, 1–76. [Google Scholar] [CrossRef]
- Falagas, M.E.; Barefoot, L.; Griffith, J.; Ruthazar, R.; Snydman, D.R. Risk Factors Leading to Clinical Failure in the Treatment of Intra-Abdominal or Skin/Soft Tissue Infections. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 1996, 15, 913–921. [Google Scholar] [CrossRef]
- Salö, M.; Tiselius, C.; Rosemar, A.; Öst, E.; Sohlberg, S.; Andersson, R.E. Swedish National Guidelines for Diagnosis and Management of Acute Appendicitis in Adults and Children. BJS Open 2025, 9, zrae165. [Google Scholar] [CrossRef]
- Huston, J.M.; Barie, P.S.; Dellinger, E.P.; Forrester, J.D.; Duane, T.M.; Tessier, J.M.; Sawyer, R.G.; Cainzos, M.A.; Rasa, K.; Chipman, J.G.; et al. The Surgical Infection Society Guidelines on the Management of Intra-Abdominal Infection: 2024 Update. Surg. Infect. 2024, 25, 419–435. [Google Scholar] [CrossRef]
- Falagas, M.E.; Matthaiou, D.K.; Bliziotis, I.A. Systematic Review: Fluoroquinolones for the Treatment of Intra-Abdominal Surgical Infections. Aliment. Pharmacol. Ther. 2007, 25, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.K.; Moon, C.; Kim, J.; Heo, S.T.; Lee, M.S.; Lee, S.; Kwon, K.-T.; Kim, S.-W.; Korean Society for Antimicrobial Therapy. Korean Society of Infectious Diseases Korean Guidelines for Use of Antibiotics for Intra-Abdominal Infections in Adults. Infect. Chemother. 2022, 54, 812–853. [Google Scholar] [CrossRef]
- Mavros, M.N.; Theochari, N.A.; Kyriakidou, M.; Economopoulos, K.P.; Sava, J.A.; Falagas, M.E. Fluoroquinolone-Based versus β-Lactam-Based Regimens for Complicated Intra-Abdominal Infections: A Meta-Analysis of Randomised Controlled Trials. Int. J. Antimicrob. Agents 2019, 53, 746–754. [Google Scholar] [CrossRef]
- Collard, M.K.; Christou, N.; Lakkis, Z.; Mege, D.; Bridoux, V.; Millet, I.; Sabbagh, C.; Loriau, J.; Lefevre, J.H.; Ronot, M.; et al. Adult Appendicitis: Clinical Practice Guidelines from the French Society of Digestive Surgery and the Society of Abdominal and Digestive Imaging. J. Visc. Surg. 2021, 158, 242–252. [Google Scholar] [CrossRef]
- Rafailidis, P.I.; Ioannidou, E.N.; Falagas, M.E. Ampicillin/Sulbactam: Current Status in Severe Bacterial Infections. Drugs 2007, 67, 1829–1849. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Wu, J.; Wang, P.; Fang, X.; Yu, Y.; Tang, J.; Xiao, Y.; Wang, M.; Li, S.; Zhang, Y.; et al. Diagnosis and Management of Intraabdominal Infection: Guidelines by the Chinese Society of Surgical Infection and Intensive Care and the Chinese College of Gastrointestinal Fistula Surgeons. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020, 71, S337–S362. [Google Scholar] [CrossRef] [PubMed]
- Pan, D.; Hills, G.; Hamilton, A.R.; Nash, T.; Hine, T.; Whitehorn, S.; Barlow, G. Recommended Antimicrobial Therapy for Common Inpatient Infections: A Comparative Review of Guidelines across 51 Hospital Trusts in England. Postgrad. Med. J. 2021, 97, 782–788. [Google Scholar] [CrossRef]
- Zeineddin, S.; Pitt, J.B.; Linton, S.; De Boer, C.; Hu, A.; Carter, M.; Alayleh, A.; Abdullah, F.; Raval, M.; Goldstein, S.D. Postoperative Antibiotics for Complicated Appendicitis in Children: Piperacillin/Tazobactam Versus Ceftriaxone with Metronidazole. J. Pediatr. Surg. 2023, 58, 1128–1132. [Google Scholar] [CrossRef] [PubMed]
- Matthaiou, D.K.; Peppas, G.; Bliziotis, I.A.; Falagas, M.E. Ciprofloxacin/Metronidazole versus Beta-Lactam-Based Treatment of Intra-Abdominal Infections: A Meta-Analysis of Comparative Trials. Int. J. Antimicrob. Agents 2006, 28, 159–165. [Google Scholar] [CrossRef]
- Kashtan, M.A.; Graham, D.A.; Melvin, P.; Hills-Dunlap, J.L.; Anandalwar, S.P.; Rangel, S.J. Ceftriaxone with Metronidazole versus Piperacillin/Tazobactam in the Management of Complicated Appendicitis in Children: Results from a Multicenter Pediatric NSQIP Analysis. J. Pediatr. Surg. 2022, 57, 365–372. [Google Scholar] [CrossRef]
- Kashtan, M.A.; Graham, D.A.; Melvin, P.; Cameron, D.B.; Anandalwar, S.P.; Hills-Dunlap, J.L.; Rangel, S.J. Ceftriaxone Combined with Metronidazole Is Superior to Cefoxitin Alone in the Management of Uncomplicated Appendicitis in Children: Results from a Multicenter Collaborative Comparative Effectiveness Study. Ann. Surg. 2021, 274, e995–e1000. [Google Scholar] [CrossRef] [PubMed]
- Hamdy, R.F.; Handy, L.K.; Spyridakis, E.; Dona, D.; Bryan, M.; Collins, J.L.; Gerber, J.S. Comparative Effectiveness of Ceftriaxone plus Metronidazole versus Anti-Pseudomonal Antibiotics for Perforated Appendicitis in Children. Surg. Infect. 2019, 20, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Hurst, A.L.; Olson, D.; Somme, S.; Child, J.; Pyle, L.; Ranade, D.; Stamatoiu, A.; Crombleholme, T.; Parker, S.K. Once-Daily Ceftriaxone Plus Metronidazole Versus Ertapenem and/or Cefoxitin for Pediatric Appendicitis. J. Pediatr. Infect. Dis. Soc. 2017, 6, 57–64. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Falagas, M.E.; Romanos, L.T.; Hopkins, A.; Sioulas, A.; Tsitskari, M. Concealed Peritonitis Due to Stomach Perforation from a Fish Otolith: A Case Report. Reports 2025, 8, 252. https://doi.org/10.3390/reports8040252
Falagas ME, Romanos LT, Hopkins A, Sioulas A, Tsitskari M. Concealed Peritonitis Due to Stomach Perforation from a Fish Otolith: A Case Report. Reports. 2025; 8(4):252. https://doi.org/10.3390/reports8040252
Chicago/Turabian StyleFalagas, Matthew E., Laura T. Romanos, Annabel Hopkins, Athanasios Sioulas, and Maria Tsitskari. 2025. "Concealed Peritonitis Due to Stomach Perforation from a Fish Otolith: A Case Report" Reports 8, no. 4: 252. https://doi.org/10.3390/reports8040252
APA StyleFalagas, M. E., Romanos, L. T., Hopkins, A., Sioulas, A., & Tsitskari, M. (2025). Concealed Peritonitis Due to Stomach Perforation from a Fish Otolith: A Case Report. Reports, 8(4), 252. https://doi.org/10.3390/reports8040252




