Surgical Treatment of Displaced Supracondylar Pediatric Humerus Fractures: Comparison of Two Pinning Techniques
Abstract
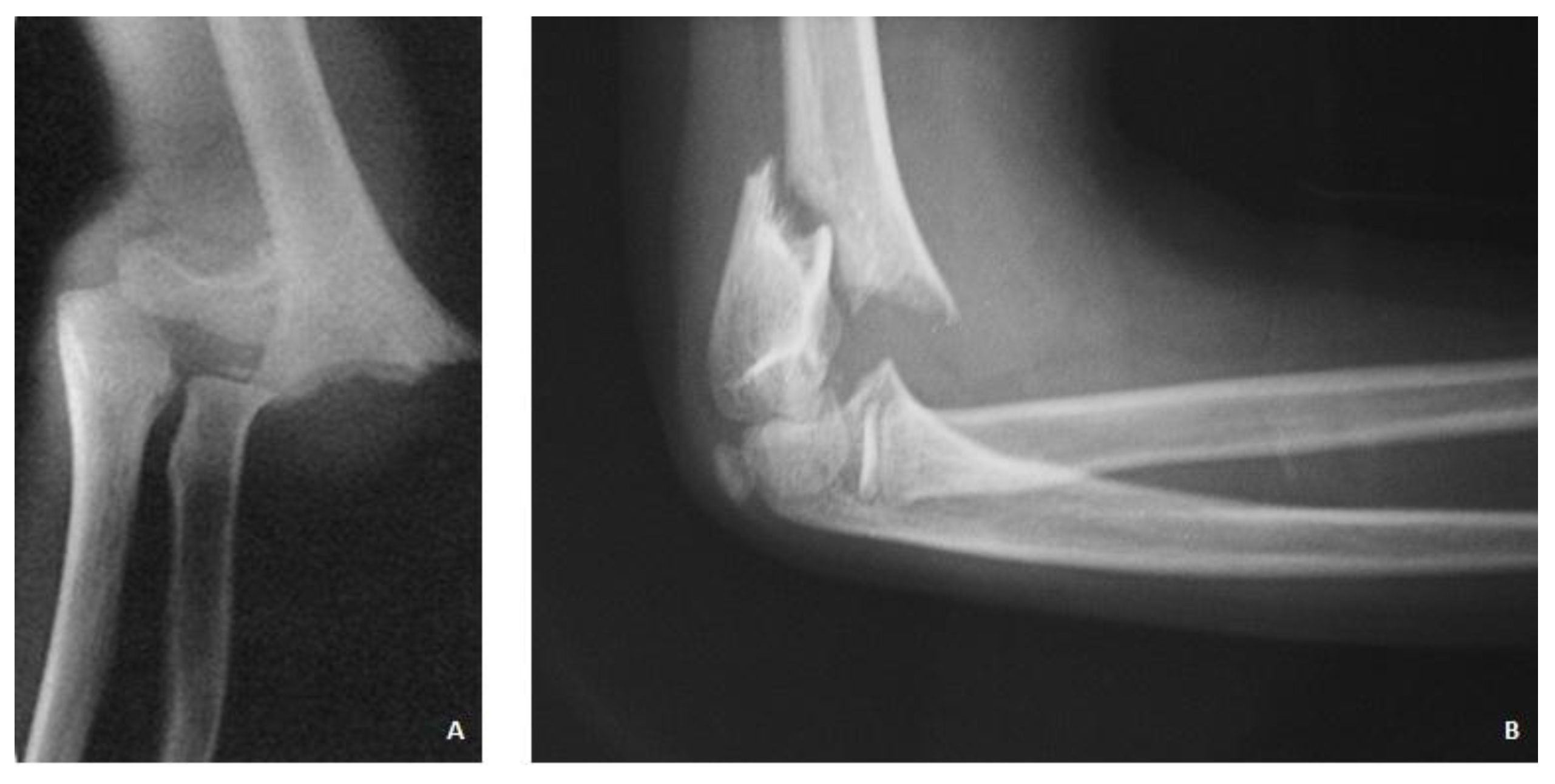
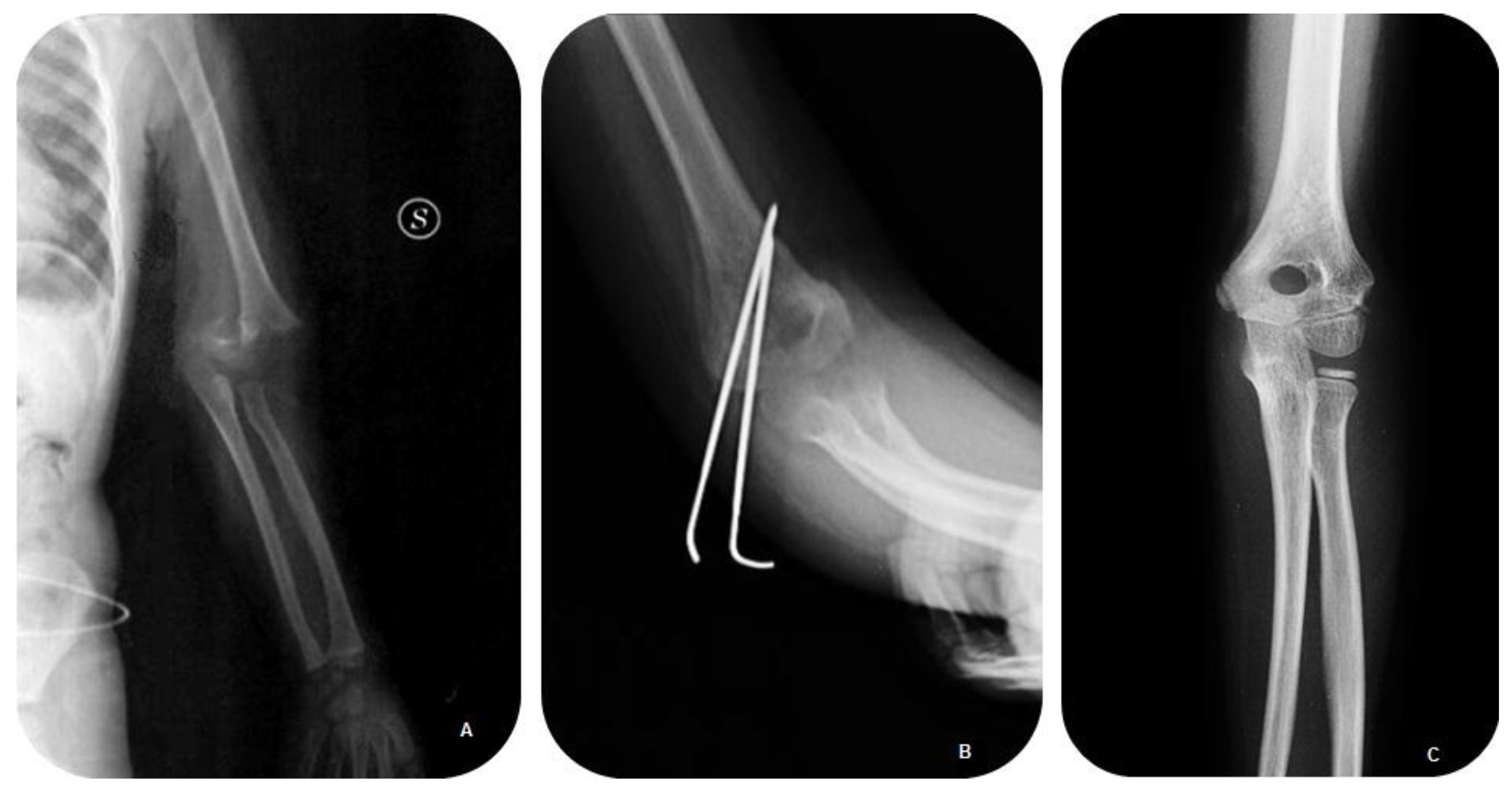
:1. Introduction
2. Patients and Methods
3. Results

| Characteristics | Group 1—K-Wire Cross Configuration (n = 22) | Group 2—Lateral K-Wire Configuration (n = 13) | p Value |
|---|---|---|---|
| Age * (years) | 6.26 ± 2.48 | 5.69 ± 2.52 | 0.55 ¤ |
| Gender † (% of patients) | 0.66 § | ||
| Male † | 16 (72) | 9 (73) | |
| Female † | 6 (28) | 4 (27) | |
| Side † (% of patients) | 0.53 § | ||
| Left Side † | 15 (67) | 9(73) | |
| Right Side † | 7 (33) | 4(27) | |
| Type of Displacement † (% of patients) | 0.59 § | ||
| Posteromedial (III A) † | 17 (78) | 11 (82) | |
| Posterolateral (III B) † | 5 (22) | 2 (18) | |
| Dynamics of injury † (% of patients) | 0.68 § | ||
| Childish games † | 19 (89) | 12 (91) | |
| Motor Accident † | 3 (11) | 1 (9) | |
| Time between admission to surgery * (h) | 7.8 ± 2.98 | 8.64 ± 3.51 | 0.49 ¤ |
| Time between injury to admission * (h) | 43.61 ± 9.5 | 41.18 ± 8.5 | 0.45 ¤ |
| Follow up * (months) | 44.39 ± 10.74 | 42.91 ± 15.77 | 0.76 ¤ |
| Flynn Criteria Cosmetic Factor †(% of patients) | 0.62 § | ||
| Excellent | 21 (94) | 13 (100) | |
| Good | 1 (6) | 0 | |
| Fair | 0 | 0 | |
| Poor | 0 | 0 | |
| Flynn Criteria Functional Factor † (% of patients) | |||
| Flexion—Extension | 103 ± 12.05 | 110.27 ± 14.39 | 0.16 |
| Supination—Pronation | 87 ± 2.42 | 87.7 ± 1.62 | 0.39 |
| Modification Carrying Angle (deg) * | 4.4 ± 2.11 | 4.46 ± 1.91 | 0.94 ¤ |
| Mayo Elbow Performance Score | 96/100 | 98/100 | |
| Modification Baumann’s Angle (deg) * | 5.3 ± 2.12 | 4.9 ± 2.82 | 0.53 ¤ |
| Reoperations † | 0 | 0 | 1.0 § |
| Return to function † | 0.92 § | ||
| Full † | 21 (94) | 13 (100) | |
| Minor Complication † | 4 (17) | 3 (27) | |
| Major Complications † | None | None | |
| Result | Rating | Cosmetic Factor Loss of Carrying Angle (Degrees) | Functional Factor Motion Loss (Degrees) |
|---|---|---|---|
| Satisfactory | Excellent | 0–5 | 0–5 |
| Good | 5–10 | 5–10 | |
| Fair | 10–15 | 10–15 | |
| Unsatisfactory | Poor | >15 | >15 |
| Feature | Rating | Score |
|---|---|---|
| Pain Intensity | None | 45 |
| Mild | 30 | |
| Moderate | 15 | |
| Severe | 0 | |
| Arc of Motion | >100° | 20 |
| 50°–100° | 15 | |
| <50° | 5 | |
| Stability | Stable | 10 |
| Moderate instability | 5 | |
| Grossly Unstable | 0 | |
| Function | Can comb hair | 5 |
| Can eat | 5 | |
| Can perform hygiene | 5 | |
| Can put on shirt | 5 | |
| Can lace shoe | 5 | |
| Maximum Score | 100 |
| Minor Complication † (n. Patients) | Group 1 (n = 22) | Group 2 (n = 13) |
|---|---|---|
| Deviation in Varus and deficit to extension | 1 (5) | 0 |
| Hyperextension | 0 | 1 (9) |
| Paresthesia | 2 (11) | 0 |
| Superficial Infections Wires | 0 | 2 (18) |
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Babal, J.C.; Mehlman, C.T.; Klein, G. Nerve injuries associated with pediatric supracondylar humeral fractures: A meta-analysis. J. Pediatr. Orthop. 2010, 30, 253–263. [Google Scholar] [CrossRef] [PubMed]
- Omid, R.; Choi, P.D.; Skaggs, D.L. Supracondylar humeral fractures in children. J. Bone Joint Surg. Am. 2008, 90, 1121–1132. [Google Scholar] [PubMed]
- Robb, J.E. The pink, pulseless hand after supracondylar fracture of the humerus in children. J. Bone Joint Surg. Br. 2009, 91, 1410–1412. [Google Scholar] [CrossRef] [PubMed]
- Barron-Torres, E.A.; Sanchez-Cruz, J.F.; Cruz-Melendez, J.R. Clinical and epidemiological characteristic of humeral supracondylar fractures in pediatric patients in a Regional General Hospital. Cir. Cir. 2015, 83, 29–34. [Google Scholar] [PubMed]
- De Pellegrin, M.; Brivio, A.; Pescatori, E.; Tessari, L. Supracondylar humerus fractures in children: Closed reduction and cross pin fixation in prone position. GIOT. 2008, 34, 199–204. [Google Scholar]
- Dua, A.; Eachempati, K.K.; Malhotra, R.; Sharma, L.; Gidaganti, M. Closed reduction and percutaneous pinning of displaced supracondylar fractures of humerus in children with delayed presentation. Chin. J. Traumatol. 2011, 14, 14–19. [Google Scholar] [PubMed]
- Eren, A.; Güven, M.; Erol, B.; Cakar, M. Delayed surgical treatment of supracondylar humerus fractures in children using a medial approach. J. Child Orthop. 2008, 2, 21–27. [Google Scholar] [PubMed]
- Gupta, N.; Kay, R.M.; Leitch, K.; Femino, J.D.; Tolo, V.T.; Skaggs, D.L. Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J. Pediatr. Orthop. 2004, 24, 245–248. [Google Scholar] [PubMed]
- Mangwani, J.; Nadarajah, R.; Paterson, J.M. Supracondylar humeral fractures in children: Ten years’ experience in a teaching hospital. J. Bone Joint Surg. Br. 2006, 88, 362–365. [Google Scholar] [CrossRef] [PubMed]
- Mommsen, P.; Zeckey, C.; Hildebrand, F.; Frink, M.; Khaladj, N.; Lange, N.; Krettek, C.; Probst, C. Traumatic extremity arterial injury in children: Epidemiology, diagnostics, treatment and prognostic value of Mangled Extremity Severity Score. J. Orthop. Surg. Res. 2010, 15, 25–35. [Google Scholar]
- Pretell-Mazzini, J.; Rodriguez-Martin, J.; Andres-Esteban, E.M. Does open reduction and pinning affect outcome in severely displaced supracondylar humeral fractures in children? A systematic review. Strateg. Trauma Limb Reconstr. 2010, 2, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Slobogean, B.L.; Jackman, H.; Tennant, S. Iatrogenic ulnar nerve injury after the surgical treatment of displaced supracondylar fractures of the humerus: Number needed to harm, a systematic review. J. Pediatr. Orthop. 2010, 30, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Flynn, J.C.; Matthews, J.G.; Benoit, R.L. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J. Bone Joint Surg. Am. 1974, 56, 263–272. [Google Scholar] [PubMed]
- Longo, U.G.; Franceschi, F.; Loppini, M.; Maffulli, N.; Denaro, V. Rating systems for evaluation of the elbow. Br. Med. Bull. 2008, 87, 131–161. [Google Scholar] [CrossRef] [PubMed]
- Mallo, G.; Stanat, S.J.; Gaffney, J. Use of the Gartland classification system for treatment of pediatric supracondylar humerus fractures. Orthopedics 2010, 33. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.; Pandarinath, R.; Farng, E.; Park, S.; Caneda, C.; Fong, Y.J.; Penman, A. Inter- and intra-observer reliability of the Baumann angle of the humerus in children with supracondylar humeral fractures. Int. Orthop. 2010, 34, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, K.E. The operative management of supracondylar fractures. Orthop. Clin. North Am. 1990, 21, 269–289. [Google Scholar] [PubMed]
- Schmid, T.; Joeris, A.; Slongo, T.; Ahmad, S.S.; Ziebarth, K. Displaced supracondylar humeral fractures: Influence of delay of surgery on the incidence of open reduction, complications and outcome. Arch. Orthop. Trauma Surg. 2015, 135, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Oetgen, M.E.; Mirick, G.E.; Atwater, L.; Lovejoy, J.F. Complications and predictors of need for return to the operating room in the treatment of supracondylar humerus fractures in children. Open Orthop. J. 2015, 9, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Flierl, M.A.; Carry, P.M.; Scott, F.; Georgopoulos, G.; Hadley-Miller, N. Rotation and displacement predict adverse events in pediatric supracondylar fractures. Orthopedics 2015, 38, e690–e695. [Google Scholar] [CrossRef] [PubMed]
- Koehler, S.M.; Sakamoto, S.; Abernathie, B.L.; Hausman, M.R. Arthroscopic correction of a supracondylar malunion in a child. Arthorosc. Technol. 2015, 4, e215–e221. [Google Scholar] [CrossRef] [PubMed]
- Brauer, C.A.; Lee, B.M.; Bae, D.S.; Waters, P.M.; Kocher, M.S. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J. Pediatr. Orthop. 2007, 27, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Larson, L.; Firoozbakhsh, K.; Passarelli, R.; Bosch, P. Biomechanical analysis of pinning techniques for pediatric supracondylar humerus fractures. J. Pediatr. Orthop. 2006, 26, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Sibinski, M.; Sharma, H.; Sherlock, D.A. Lateral versus crossed wire fixation for displaced extension supracondylar humeral fractures in children. Injury 2006, 37, 961–965. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.G.; Wang, J.; Zhang, P. Is lateral pin fixation for displaced supracondylar fractures of the humerus better than crossed pins in children? Clin. Orthop. Relat. Res. 2013, 471, 2942–2953. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Park, M.S.; Chung, C.Y.; Kwon, D.G.; Sung, K.H.; Kim, T.W.; Choi, I.H.; Cho, T.J.; Yoo, W.J.; Lee, K.M. Consensus and different perspectives on treatment of supracondylar fractures of the humerus in children. Clin. Orthop. Surg. 2012, 4, 91–97. [Google Scholar] [CrossRef] [PubMed]
- El-Adl, W.A.; El-Said, M.A.; Boghdady, G.W.; Ali, A.S. Results of treatment of displaced supracondylar humeral fractures in children by percutaneous lateral cross-wiring technique. Strateg. Trauma Limb Reconstr. 2008, 3, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Sankar, W.N.; Hebela, N.M.; Skaggs, D.L.; Flynn, J.M. Loss of pin fixation in displaced supracondylar humeral fractures in children: Causes and prevention. J. Bone Joint Surg. Am. 2007, 89, 713–717. [Google Scholar] [CrossRef] [PubMed]
- Zamzam, M.M.; Bakarman, K.A. Treatment of displaced supracondylar humeral fractures among children: Crossed versus lateral pinning. Injury 2009, 40, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Yen, Y.M.; Kocher, M.S. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. Surgical technique. J. Bone Joint Surg. Am. 2008, 90, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Skaggs, D.L.; Cluck, M.W.; Mostofi, A.; Flynn, J.M.; Kay, R.M. Lateral-entry pin fixation in the management of supracondylar fractures in children. J. Bone Joint Surg. Am. 2004, 86, 702–707. [Google Scholar] [PubMed]
- Gaston, R.G.; Cates, T.B.; Devito, D.; Schmitz, M.; Schrader, T.; Busch, M.; Fabregas, J.; Rosenberg, E.; Blanco, J. Medial and lateral pin versus lateral-entry pin fixation for Type 3 supracondylar fractures in children: A prospective, surgeon-randomized study. J. Pediatr. Orthop. 2010, 30, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Ladenhauf, H.N.; Schaffert, M.; Bauer, J. The displaced supracondylar humerus fracture: Indications for surgery and surgical options: A 2014 update. Curr. Opin. Pediatr. 2014, 26, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Mulpuri, K.; Wilkins, K. The treatment of displaced supracondylar humerus fractures: Evidence-based guideline. J. Pediatr. Orthop. 2012, 32, S143–S152. [Google Scholar] [CrossRef] [PubMed]
- Spencer, H.T.; Wong, M.; Fong, Y.J.; Penman, A.; Silva, M. Prospective longitudinal evaluation of elbow motion following pediatric supracondylar humeral fractures. J. Bone Joint Surg. Am. 2010, 92, 904–910. [Google Scholar] [CrossRef] [PubMed]
- Zionts, L.E.; Woodson, C.J.; Manjra, N.; Zalavras, C. Time of return of elbow motion after percutaneous pinning of pediatric supracondylar humerus fractures. Clin. Orthop. Relat. Res. 2009, 467, 2007–2010. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pavone, V.; Riccioli, M.; Testa, G.; Lucenti, L.; De Cristo, C.; Condorelli, G.; Avondo, S.; Sessa, G. Surgical Treatment of Displaced Supracondylar Pediatric Humerus Fractures: Comparison of Two Pinning Techniques. J. Funct. Morphol. Kinesiol. 2016, 1, 39-47. https://doi.org/10.3390/jfmk1010039
Pavone V, Riccioli M, Testa G, Lucenti L, De Cristo C, Condorelli G, Avondo S, Sessa G. Surgical Treatment of Displaced Supracondylar Pediatric Humerus Fractures: Comparison of Two Pinning Techniques. Journal of Functional Morphology and Kinesiology. 2016; 1(1):39-47. https://doi.org/10.3390/jfmk1010039
Chicago/Turabian StylePavone, Vito, Maria Riccioli, Gianluca Testa, Ludovico Lucenti, Claudia De Cristo, Giuseppe Condorelli, Sergio Avondo, and Giuseppe Sessa. 2016. "Surgical Treatment of Displaced Supracondylar Pediatric Humerus Fractures: Comparison of Two Pinning Techniques" Journal of Functional Morphology and Kinesiology 1, no. 1: 39-47. https://doi.org/10.3390/jfmk1010039






