Barriers to the Implementation of Newborn Pulse Oximetry Screening: A Different Perspective
Abstract
:1. Introduction
2. Australian/New Zealand Progress
3. Challenges in Introducing Pulse Oximetry Screening for CCHD
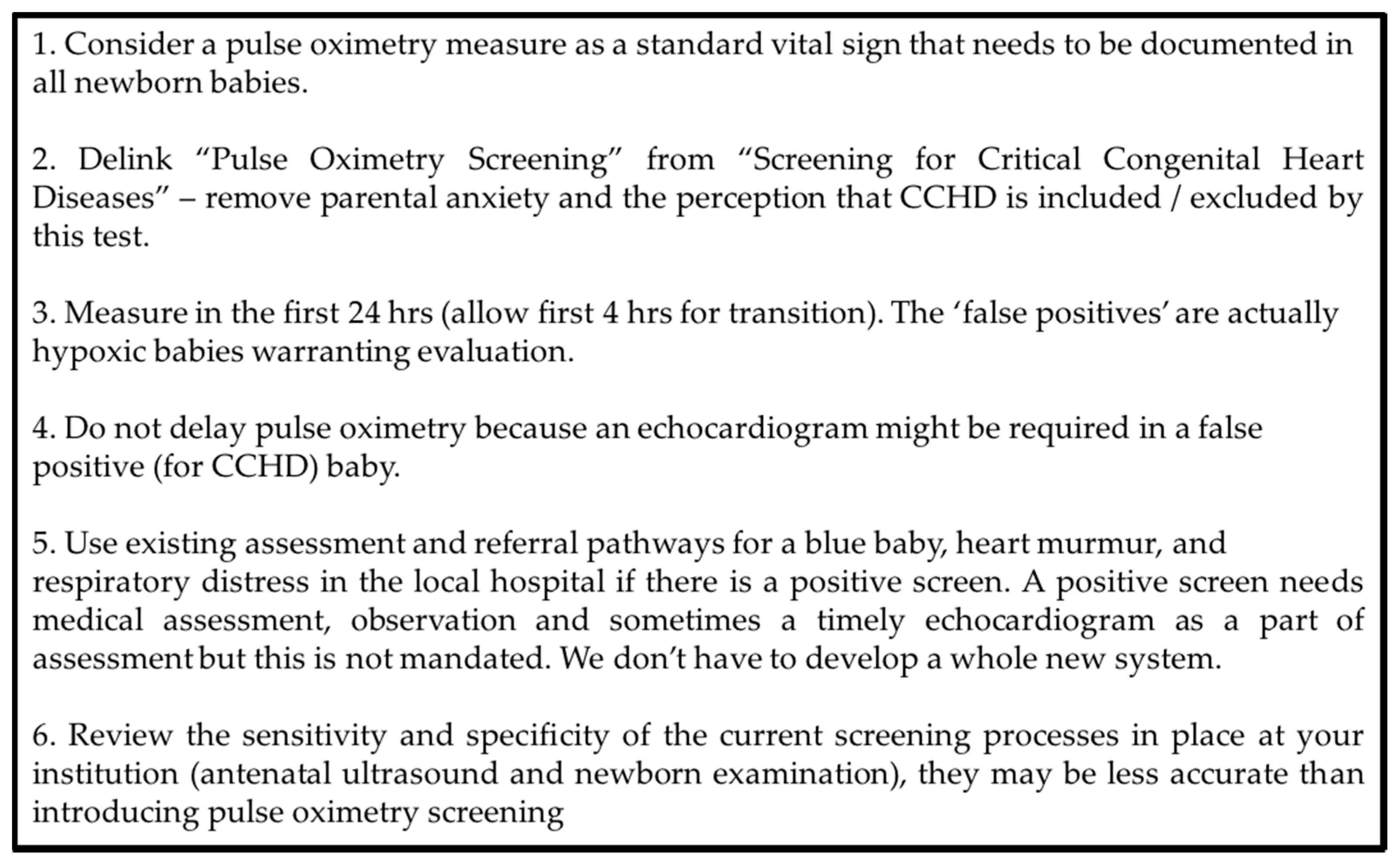
3.1. Screening for CCHD or Documentation of a Vital Sign
3.2. Linking ‘Pulse Oximetry Screening’ to ‘Screening for CCHD’
3.3. Timing of Pulse Oximetry Screening and Significance of False Positives
3.4. Response to a Positive Screen
4. Pulse Oximetry of the Well Newborn versus Screening for CCHD
5. Conclusions
Conflicts of Interest
References
- Hoffman, J.I. It is time for routine neonatal screening by pulse oximetry. Neonatology 2011, 99, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kuehl, K.S.; Loffredo, C.A.; Ferencz, C. Failure to diagnose congenital heart disease in infancy. Pediatrics 1999, 103, 743–747. [Google Scholar] [CrossRef] [PubMed]
- Snookes, S.H.; Gunn, J.K.; Eldridge, B.J.; Donath, S.M.; Hunt, R.W.; Galea, M.P.; Shekerdemian, L. A systematic review of motor and cognitive outcomes after early surgery for congenital heart disease. Pediatrics 2010, 125, e818–e827. [Google Scholar] [CrossRef] [PubMed]
- Sholler, G.F.; Kasparian, N.A.; Pye, V.E.; Cole, A.D.; Winlaw, D.S. Fetal and post-natal diagnosis of major congenital heart disease: Implications for medical and psychological care in the current era. J. Paediatr. Child Health 2011, 47, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Sharland, G. Fetal cardiac screening: Why bother? Arch. Dis. Child. Fetal Neonatal Ed. 2010, 95, F64–F68. [Google Scholar] [PubMed]
- Mellander, M.; Sunnegardh, J. Failure to diagnose critical heart malformations in newborns before discharge—An increasing problem? Acta Paediatr. 2006, 95, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Ewer, A.K.; Middleton, L.J.; Furmston, A.T.; Bhoyar, A.; Daniels, J.P.; Thangaratinam, S.; Deeks, J.J.; Khan, K.S.; PulseOx Study Group. Pulse oximetry screening for congenital heart defects in newborn infants (pulseox): A test accuracy study. Lancet 2011, 378, 785–794. [Google Scholar] [CrossRef]
- Thangaratinam, S.; Brown, K.; Zamora, J.; Khan, K.S.; Ewer, A.K. Pulse oximetry screening for critical congenital heart defects in asymptomatic newborn babies: A systematic review and meta-analysis. Lancet 2012, 379, 2459–2464. [Google Scholar] [CrossRef]
- Kemper, A.R.; Mahle, W.T.; Martin, G.R.; Cooley, W.C.; Kumar, P.; Morrow, W.R.; Kelm, K.; Pearson, G.D.; Glidewell, J.; Grosse, S.D.; et al. Strategies for implementing screening for critical congenital heart disease. Pediatrics 2011, 128, e1259–e1267. [Google Scholar] [CrossRef] [PubMed]
- Cloete, E.; Gentles, T.L.; Alsweiler, J.M.; Dixon, L.A.; Webster, D.R.; Rowe, D.L.; Bloomfield, F.H. Should new zealand introduce nationwide pulse oximetry screening for the detection of critical congenital heart disease in newborn infants? N. Z. Med. J. 2017, 130, 64–69. [Google Scholar] [PubMed]
- Mikrou, P.; Singh, A.; Ewer, A.K. Pulse oximetry screening for critical congenital heart defects: A repeat UK national survey. Arch. Dis. Child. Fetal Neonatal Ed. 2017, 102, F558. [Google Scholar] [CrossRef] [PubMed]
- Edwards, E.D.; Powell, C.V.; Mason, B.W.; Oliver, A. Prospective cohort study to test the predictability of the cardiff and vale paediatric early warning system. Arch. Dis. Child. 2009, 94, 602–606. [Google Scholar] [CrossRef] [PubMed]
- Health, N. Children and Infants—Recognition of a Sick Baby or Child in the Emergency Department; NSW Health: Sydney, Australia, 2011. [Google Scholar]
- Katzman, G.H. The newborn’s spo2: A routine vital sign whose time has come? Pediatrics 1995, 95, 161–162. [Google Scholar] [PubMed]
- Mower, W.R.; Sachs, C.; Nicklin, E.L.; Baraff, L.J. Pulse oximetry as a fifth pediatric vital sign. Pediatrics 1997, 99, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Powell, R.; Pattison, H.M.; Bhoyar, A.; Furmston, A.T.; Middleton, L.J.; Daniels, J.P.; Ewer, A.K. Pulse oximetry screening for congenital heart defects in newborn infants: An evaluation of acceptability to mothers. Arch. Dis. Child. Fetal Neonatal Ed. 2013, 98, F59–F63. [Google Scholar] [CrossRef] [PubMed]
- Hom, L.A.; Silber, T.J.; Ennis-Durstine, K.; Hilliard, M.A.; Martin, G.R. Legal and ethical considerations in allowing parental exemptions from newborn critical congenital heart disease (cchd) screening. Am. J. Bioeth. 2016, 16, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Bhola, K.; Kluckow, M.; Evans, N. Post-implementation review of pulse oximetry screening of well newborns in an australian tertiary maternity hospital. J. Paediatr. Child Health 2014, 50, 920–925. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.A.; Vento, M.; Finer, N.N.; Rich, W.; Saugstad, O.D.; Morley, C.J.; Davis, P.G. Managing oxygen therapy during delivery room stabilization of preterm infants. J. Pediatr. 2012, 160, 158–161. [Google Scholar] [CrossRef] [PubMed]
- Narayen, I.C.; Blom, N.A.; Ewer, A.K.; Vento, M.; Manzoni, P.; te Pas, A.B. Aspects of pulse oximetry screening for critical congenital heart defects: When, how and why? Arch. Dis. Child. Fetal Neonatal Ed. 2016, 101, F162–F167. [Google Scholar] [CrossRef] [PubMed]
- Meberg, A.; Brugmann-Pieper, S.; Due, R., Jr.; Eskedal, L.; Fagerli, I.; Farstad, T.; Froisland, D.H.; Sannes, C.H.; Johansen, O.J.; Keljalic, J.; et al. First day of life pulse oximetry screening to detect congenital heart defects. J. Pediatr. 2008, 152, 761–765. [Google Scholar] [CrossRef] [PubMed]
- Arlettaz, R.; Bauschatz, A.S.; Monkhoff, M.; Essers, B.; Bauersfeld, U. The contribution of pulse oximetry to the early detection of congenital heart disease in newborns. Eur. J. Pediatr. 2006, 165, 94–98. [Google Scholar] [CrossRef] [PubMed]
- de-Wahl Granelli, A.; Wennergren, M.; Sandberg, K.; Mellander, M.; Bejlum, C.; Inganas, L.; Eriksson, M.; Segerdahl, N.; Agren, A.; Ekman-Joelsson, B.M.; et al. Impact of pulse oximetry screening on the detection of duct dependent congenital heart disease: A swedish prospective screening study in 39,821 newborns. Bmj 2009, 338, a3037. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.M.; Ma, X.J.; Ge, X.L.; Liu, F.; Yan, W.L.; Wu, L.; Ye, M.; Liang, X.C.; Zhang, J.; Gao, Y.; et al. Pulse oximetry with clinical assessment to screen for congenital heart disease in neonates in china: A prospective study. Lancet 2014, 384, 747–754. [Google Scholar] [CrossRef]
- Schultz, A.H.; Localio, A.R.; Clark, B.J.; Ravishankar, C.; Videon, N.; Kimmel, S.E. Epidemiologic features of the presentation of critical congenital heart disease: Implications for screening. Pediatrics 2008, 121, 751–757. [Google Scholar] [CrossRef] [PubMed]
- de-Wahl Granelli, A.; Meberg, A.; Ojala, T.; Steensberg, J.; Oskarsson, G.; Mellander, M. Nordic pulse oximetry screening--implementation status and proposal for uniform guidelines. Acta Paediatr. 2014, 103, 1136–1142. [Google Scholar] [CrossRef] [PubMed]
| <24 h of Age | >24 h of Age |
|---|---|
| Increased detection of significant and major CHD | Increased detection of significant and major CHD |
| Optimal for prevention of postnatal hypoxia | Not optimal but still prevents some hypoxic events |
| Higher false positive rate for CCHD (0.5%) | Lower false positive rate for CCHD (0.05%) |
| Detection of other pathology (up to 50% of all false positives) | Detection of other pathology (up to 50% of all false positives) |
| Often still in hospital: doesn’t disrupt discharge process | May disrupt discharge process |
| Screening Program | Hospital Led/5th Vital Sign |
|---|---|
| Meeting screening test criteria, Competing with other national screening programs for funding | More easily achievable without a complex application process |
| Research based: almost 500,000 babies tested | Harder to justify as not linked to CCHD research |
| Country-wide introduction, mandated, uniformity of coverage | Gaps in provision, Ad Hoc screening |
| Properly resourced and funded. Quality improvement more easily achieved | Resourcing is not excessive so achievable by most hospitals |
| CHD is a tested hard outcome | Importance of other diagnoses and timing of the test |
| Follows existing research based algorithms: reduced flexibility | Delink from CCHD terminology: reduces pressure from false positives and need for echocardiogram. |
© 2018 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kluckow, M. Barriers to the Implementation of Newborn Pulse Oximetry Screening: A Different Perspective. Int. J. Neonatal Screen. 2018, 4, 4. https://doi.org/10.3390/ijns4010004
Kluckow M. Barriers to the Implementation of Newborn Pulse Oximetry Screening: A Different Perspective. International Journal of Neonatal Screening. 2018; 4(1):4. https://doi.org/10.3390/ijns4010004
Chicago/Turabian StyleKluckow, Martin. 2018. "Barriers to the Implementation of Newborn Pulse Oximetry Screening: A Different Perspective" International Journal of Neonatal Screening 4, no. 1: 4. https://doi.org/10.3390/ijns4010004




