Bilateral Transverse Mandibular Second Molars: A Case Report
Abstract
:1. Introduction
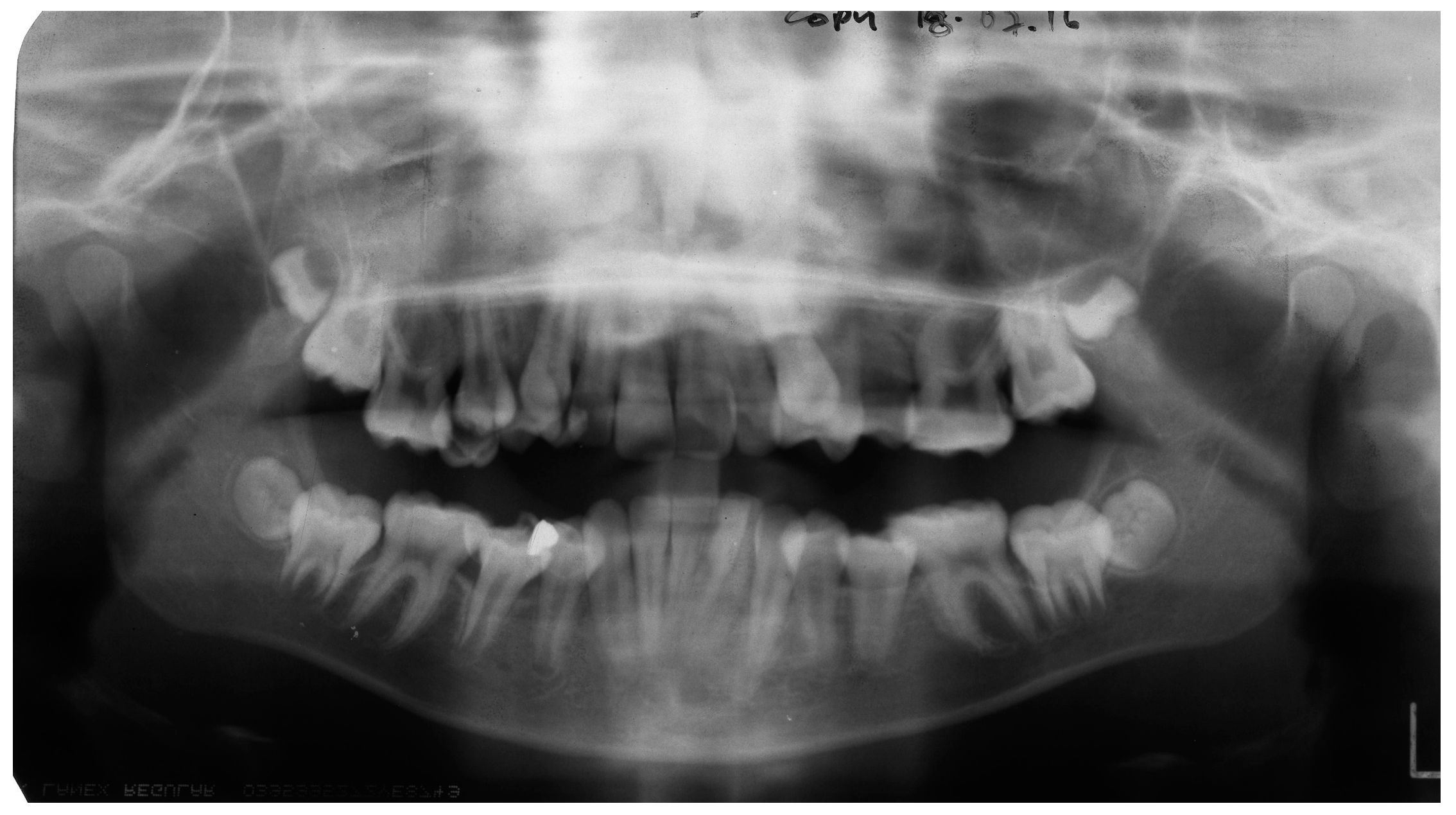
2. Case Report
3. Discussion
4. Conclusions
Conflicts of Interest
References
- Ten Cate, A.R. Oral Histology, Development, Structure and Function, 3rd ed.; Mosby: St Louis, MO, USA, 1989; pp. 275–289. [Google Scholar]
- Jensen, B.L.; Kreiborg, S. Development of the dentition in cleidocranial dysplasia. J. Oral Pathol. Med. 1990, 19, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Raghoebar, G.M.; Boering, G.; Vissink, A.; Stegenga, B. Eruption disturbances of permanent molars: A review. J. Oral Pathol. Med. 1991, 20, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O.; Kurol, J. The impacted first and second molar. In Textbook and Color Atlas of Tooth Impactions; Andreasen, J.O., Petersen, J.K., Eds.; Munksgaard: Copenhagen, Denmark, 1977; pp. 197–218. [Google Scholar]
- Farman, A.G.; Eloff, J.; Nortje, C.J.; Joubert, J.J. Clinical absence of the first and second permanent molars. Br. J. Orthod. 1978, 5, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Pindborg, J.J. Pathology of the Dental Hard Tissues; Munksgaard: Copenhagen, Denmark, 1970; pp. 225–255. [Google Scholar]
- Fu, P.S.; Wang, J.C.; Wu, Y.M.; Huang, T.K.; Chen, W.C.; Tseng, Y.C.; Tseng, C.H.; Hung, C.C. Impacted mandibular second molars. Angle Orthod. 2012, 82, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Altieri, F.; Di Mambro, A.; Galluccio, G.; Barbato, E. Impaction of permanent mandibular second molar. A retrospective study. Med. Oral Patol. Cir. Bucal 2013, 18, e564. [Google Scholar] [CrossRef]
- Bondemark, L.; Tsiopa, J. Prevalence of ectopic eruption, impaction, retention and agenesis of the permanent second molar. Angle Orthod. 2007, 77, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Magnusson, C.; Kjellberg, H. Impaction and retention of second molars: Diagnosis, treatment and outcome. A retrospective follow-up study. Angle Orthod. 2009, 79, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Calderon, M.; Torres-Lagares, D.; Gonzalez-Martin, M.; Gutierrez-Perez, J.L. Rescue surgery (surgical repositioning of impacted lower second molars. Med. Oral Patol. Cir. Bucal 2005, 10, 448–453. [Google Scholar]
- Johnson, J.V.; Quirk, G.P. Surgical repositioning of impacted mandibular second molar teeth. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 242–251. [Google Scholar] [CrossRef]
- Proffit, W.; Fields, H. Contemporary Orthodontics, 3rd ed.; Mosby: St Louis, MO, USA, 2000; Volume 11, p. 541. [Google Scholar]
- Evans, R. Incidence of lower second permanent molar impaction. Br. J. Orthod. 1998, 15, 199–203. [Google Scholar] [CrossRef]
- Shafer, W.G.; Hine, M.K.; Levy, B.M. A Textbook of Oral Pathology, 4th ed.; Saunders: Philadelphia, PA, USA, 1983; pp. 66–69. [Google Scholar]
- Wellfelt, B.; Varpio, M. Disturbed eruption of the permanent lower second molar: Treatment and results. ASDC J. Dent. Child. 1988, 55, 183–189. [Google Scholar] [PubMed]
- Raghoebar, G.M.; Jansen, H.W.; Jongebloed, W.L.; Boering, G.; Vissink, A. Secondary retention of permanent molars: An assessment of ankylosis by scanning electron and light microscopy. Br. J. Oral Maxillofac. Surg. 1992, 30, 50–55. [Google Scholar] [CrossRef]
- Alessandri Bonetti, G.; Pelliccioni, G.A.; Checchi, L. Management of bilaterally impacted mandibular second and third molars. J. Am. Dent. Assoc. 1999, 130, 1190–1194. [Google Scholar] [CrossRef] [PubMed]
- Going, R.E., Jr.; Reyes-Lois, D.B. Surgical exposure and bracketing technique for uprighting impacted mandibular second molars. J. Oral Maxillofac. Surg. 1999, 57, 209–212. [Google Scholar] [CrossRef]
- Davis, W.H.; Patakas, B.M.; Kaminishi, R.M.; Parsch, N.E. Surgically uprighting and grafting mandibular second molars. Am. J. Orthod. 1976, 69, 555–561. [Google Scholar] [CrossRef]
- Cerny, R. Jumbo separators for partial molar impactions. J. Clin. Orthod. 2003, 37, 33–35. [Google Scholar] [PubMed]
- Miao, Y.Q.; Zhong, H. An uprighting appliance for impacted mandibular second and third molars. J. Clin. Orthod. 2006, 40, 110–116. [Google Scholar] [PubMed]
- Sato, K. Impacted mandibular second molar with extruded maxillary second molar: A case report. World J. Orthod. 2005, 6, 25–29. [Google Scholar] [PubMed]
- McAboy, C.P.; Grumet, J.T.; Siegel, E.B.; Iacopino, A.M. Surgical uprighting and repositioning of severely impacted mandibular second molars. J. Am. Dent. Assoc. 2003, 134, 1459–1462. [Google Scholar] [CrossRef] [PubMed]
- Valmaseda-Castellon, E.; De-la-Rosa-Gay, C.; Gay-Escoda, C. Eruption disturbances of the first and second permanent molars: Results of treatment in 43 cases. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 651–658. [Google Scholar] [CrossRef]
- Kayser, A.F. Shortened dental arches and oral function. J. Oral Rehabil. 1981, 8, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Casseta, M.; Altieri, F.; Calasso, S. Etiological factors in second mandibular molar impaction. J. Clin. Exp. Dent. 2014, 6, e150–e154. [Google Scholar] [CrossRef] [PubMed]
- British Orthodontic Society. Guidelines for the Use of Radiographs in Clinical Orthodontics; British Orthodontic Society: London, UK, 2015. [Google Scholar]
- Horner, K.; Eaton, K. (Eds.) Selection Criteria for Dental Radiography, 3rd ed.; Faculty of General Dental Practice (UK): London, UK, 2013.
- American Dental Association. Dental Radiographic Examinations: Recommendations for Patient Selection and Limiting Radiation Exposure (Revised); American Dental Association: Chicago, IL, USA, 2012. [Google Scholar]
- European Commission. Radiation Protection 136. European Guidelines on Radiation Protection in Dental Radiology; European Commission: Manchester, UK, 2004. [Google Scholar]

© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puryer, J.; Mittal, T.; McNamara, C.; Ireland, T.; Sandy, J. Bilateral Transverse Mandibular Second Molars: A Case Report. Dent. J. 2016, 4, 43. https://doi.org/10.3390/dj4040043
Puryer J, Mittal T, McNamara C, Ireland T, Sandy J. Bilateral Transverse Mandibular Second Molars: A Case Report. Dentistry Journal. 2016; 4(4):43. https://doi.org/10.3390/dj4040043
Chicago/Turabian StylePuryer, James, Tarun Mittal, Catherine McNamara, Tony Ireland, and Jonathan Sandy. 2016. "Bilateral Transverse Mandibular Second Molars: A Case Report" Dentistry Journal 4, no. 4: 43. https://doi.org/10.3390/dj4040043





