Factors Driving Users’ Engagement in Patient Social Network Systems
Abstract
:1. Introduction
2. Theoretical Framework
2.1. User’s Engagement in Online Communities
2.2. Affective Events Theory
2.3. Self-Determination Theory
3. Materials and Methods
3.1. Hypotheses Development
3.2. Data Collection and Analysis
4. Results
4.1. Respondent Profiles
4.2. Measurement Model Evaluation
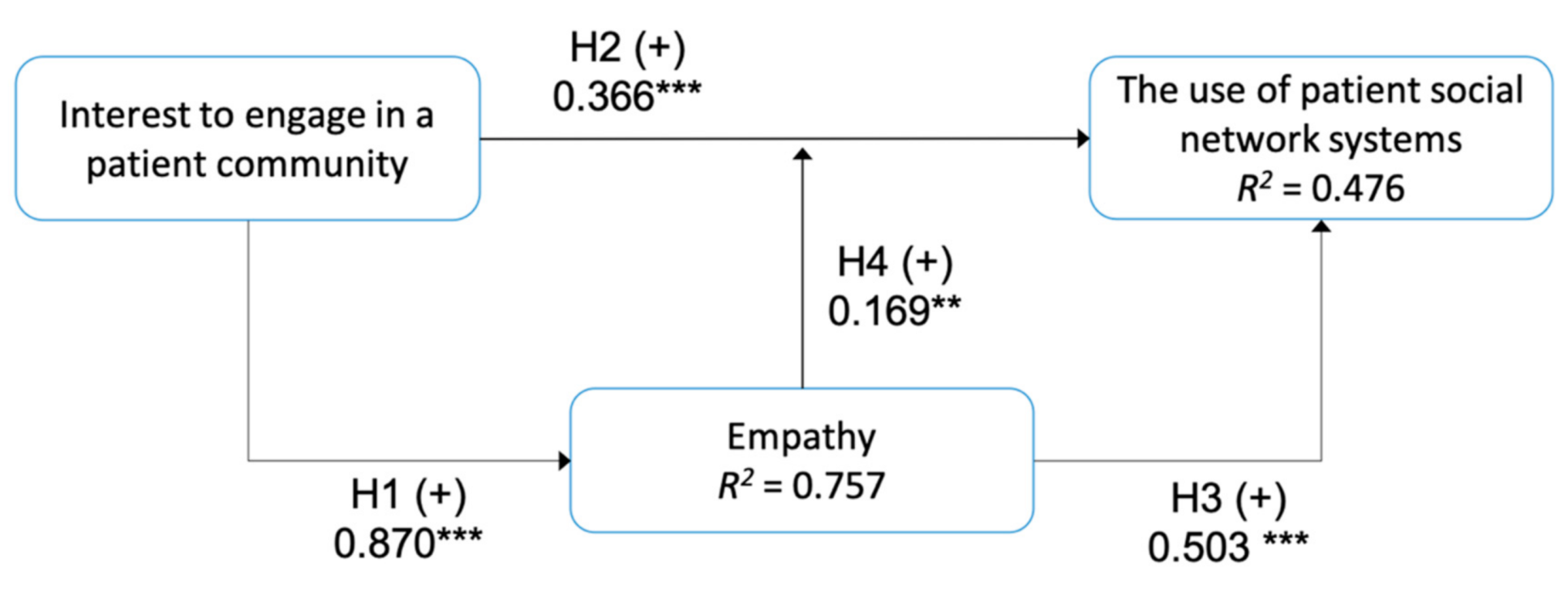
4.3. Structural Model and Hypotheses Test
5. Discussion
5.1. Factors Affecting a User’s Engagement in a PSNS
5.2. Implications
5.3. Limitations and Future Studies
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fox, S.; Duggan, M. Health Online 2013. Available online: http://www.pewinternet.org/2013/01/15/health-online-2013/ (accessed on 26 August 2018).
- Mc Daid, D.; Park, A.-L. Online Health: Untangling the Web. Available online: https://www.bupa.com.au/staticfiles/Bupa/HealthAndWellness/MediaFiles/PDF/LSE_Report_Online_Health.pdf (accessed on 26 August 2018).
- Moreland, J.; French, T.L.; Cumming, G.P. The Prevalence of Online Health Information Seeking Among Patients in Scotland: A Cross-Sectional Exploratory Study. JMIR Res. Protoc. 2015, 4, e4010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, F.-C.; Chiu, C.-H.; Chen, P.-H.; Miao, N.-F.; Lee, C.-M.; Chiang, J.-T.; Pan, Y.-C. Relationship Between Parental and Adolescent eHealth Literacy and Online Health Information Seeking in Taiwan. Cyberpsychol. Behav. Soc. Netw. 2015, 18, 618–624. [Google Scholar] [CrossRef]
- Bauer, R.; Conell, J.; Glenn, T.; Alda, M.; Ardau, R.; Baune, B.T.; Berk, M.; Bersudsky, Y.; Bilderbeck, A.; Bocchetta, A.; et al. Internet use by patients with bipolar disorder: Results from an international multisite survey. Psychiatry Res. 2016, 242, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Suka, M.; Odajima, T.; Okamoto, M.; Sumitani, M.; Igarashi, A.; Ishikawa, H.; Kusama, M.; Yamamoto, M.; Nakayama, T.; Sugimori, H. Relationship between health literacy, health information access, health behavior, and health status in Japanese people. Patient Educ. Couns. 2015, 98, 660–668. [Google Scholar] [CrossRef] [PubMed]
- Puspitasari, I.; Fukui, K.-I.; Moriyama, K.; Numao, M. Predicting consumer familiarity with health topics by query formulation and search result interaction. In Proceedings of the Pacific RIM International Conference on Artificial Intelligence; Springer: Cham, Switzerland, 2014; Volume 8862, pp. 1016–1022. [Google Scholar]
- Puspitasari, I. The impacts of consumer’s health topic familiarity in seeking health information online. In Proceedings of the 2017 15th IEEE/ACIS International Conference on Software Engineering Research, Management and Applications, London, UK, 7–9 June 2017; pp. 104–109. [Google Scholar]
- Puspitasari, I.; Firdauzy, A. Characterizing Consumer Behavior in Leveraging Social Media for E-Patient and Health-Related Activities. Int. J. Environ. Res. Public Health 2019, 16, 3348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Medlock, S.; Eslami, S.; Askari, M.; Arts, D.L.; Sent, D.; De Rooij, S.E.; Abu-Hanna, A. Health information-seeking behavior of seniors who use the internet: A survey. J. Med. Internet Res. 2015, 17, e10. [Google Scholar] [CrossRef]
- Lee, Y.J.; Boden-Albala, B.; Jia, H.; Wilcox, A.; Bakken, S. The association between online health information-seeking behaviors and health behaviors among hispanics in New York city: A community-based cross-sectional study. J. Med. Internet Res. 2015, 17, e261. [Google Scholar] [CrossRef]
- Song, H.; Omori, K.; Kim, J.; Tenzek, K.E.; Hawkins, J.M.; Lin, W.Y.; Kim, Y.C.; Jung, J.Y. Trusting social media as a source of health information: Online surveys comparing the United States, Korea, and Hong Kong. J. Med. Internet Res. 2016, 18, e25. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, S.; Deng, Z.; Chen, X. Knowledge sharing motivations in online health communities: A comparative study of health professionals and normal users. Comput. Human Behav. 2017, 75, 797–810. [Google Scholar] [CrossRef]
- Wicks, P.; Thorley, E.M.; Simacek, K.; Curran, C.; Emmas, C. Scaling PatientsLikeMe via a “generalized platform” for members with chronic illness: Web-based survey study of benefits arising. J. Med. Internet Res. 2018, 20, e175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, S.S.L.; Goonawardene, N. Internet health information seeking and the patient-physician relationship: A systematic review. J. Med. Internet Res. 2017, 19, e9. [Google Scholar] [CrossRef] [PubMed]
- An, L.C.; Wallner, L.; Kirch, M.A. Online Social Engagement by Cancer Patients: A Clinic-Based Patient Survey. JMIR Cancer 2016, 2, e10. [Google Scholar] [CrossRef] [Green Version]
- Bernell, S.; Howard, S.W. Use Your Words Carefully: What Is a Chronic Disease? Front. Public Heal. 2016, 4, 159. [Google Scholar] [CrossRef] [Green Version]
- Wicks, P.; Massagli, M.; Frost, J.; Brownstein, C.; Okun, S.; Vaughan, T.; Bradley, R.; Heywood, J. Sharing health data for better outcomes on patientslikeme. J. Med. Internet Res. 2010, 12, e19. [Google Scholar] [CrossRef] [Green Version]
- Sav, A.; Whitty, J.A.; McMillan, S.S.; Kendall, E.; Kelly, F.; King, M.A.; Wheeler, A.J. Treatment Burden and Chronic Illness: Who is at Most Risk? Patient 2016, 9, 559–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, X.L.; Zhou, Z.; Lee, M.K.O.; Cheung, C.M.K. Why users keep answering questions in online question answering communities: A theoretical and empirical investigation. Int. J. Inf. Manage. 2013, 33, 93–104. [Google Scholar] [CrossRef]
- Ma, W.W.K.; Chan, A. Knowledge sharing and social media: Altruism, perceived online attachment motivation, and perceived online relationship commitment. Comput. Human Behav. 2014, 39, 51–58. [Google Scholar] [CrossRef]
- Xu, A.; Bailey, B.P. What Do You Think? A Case Study of Benefit, Expectation, and Interaction in a Large Online Critique Community. In Proceedings of the ACM 2012 Conference on Computer Supported Cooperative Work, CSCW’12, Seattle, WA, USA, 11–15 February 2012. [Google Scholar]
- Jin, J.; Li, Y.; Zhong, X.; Zhai, L. Why users contribute knowledge to online communities: An empirical study of an online social Q&A community. Inf. Manag. 2015, 52, 840–849. [Google Scholar]
- Welbourne, J.L.; Blanchard, A.L.; Wadsworth, M.B. Motivations in virtual health communities and their relationship to community, connectedness and stress. Comput. Human Behav. 2013, 29, 129–139. [Google Scholar] [CrossRef]
- Hwang, M.I.; Thorn, R.G. The effect of user engagement on system success: A meta-analytical integration of research findings. Inf. Manag. 1999, 35, 229–236. [Google Scholar] [CrossRef]
- Di Gangi, P.M.; Wasko, M. Social media engagement theory: Exploring the infuence of user engagement on social media usage. J. Organ. End User Comput. 2016, 28, 53–73. [Google Scholar] [CrossRef] [Green Version]
- Calder, B.J.; Malthouse, E.C.; Schaedel, U. An Experimental Study of the Relationship between Online Engagement and Advertising Effectiveness. J. Interact. Mark. 2009, 23, 321–331. [Google Scholar] [CrossRef]
- Lo Presti, L.; Testa, M.; Marino, V.; Singer, P. Engagement in healthcare systems: Adopting digital tools for a sustainable approach. Sustainability 2019, 11, 220. [Google Scholar] [CrossRef] [Green Version]
- Brodie, R.J.; Hollebeek, L.D.; Jurić, B.; Ilić, A. Customer engagement: Conceptual domain, fundamental propositions, and implications for research. J. Serv. Res. 2011, 14, 252–271. [Google Scholar] [CrossRef]
- Breidbach, C.F.; Brodie, R.; Hollebeek, L. Beyond virtuality: From engagement platforms to engagement ecosystems. Manag. Serv. Qual. 2014, 24, 592–611. [Google Scholar] [CrossRef]
- Weiss, H.M.; Cropanzano, R. Affective Events Theory: A Theoretical Discussion of the Structure, Causes and Consequences of Affective Experiences at Work; Elsevier Science/JAI Press: Greenwich, CT, USA, 1996; Volume 18. [Google Scholar]
- Luo, M.M.; Chea, S. Cognitive appraisal of incident handling, affects, and post-adoption behaviors: A test of affective events theory. Int. J. Inf. Manage. 2018, 40, 120–131. [Google Scholar] [CrossRef]
- Luo, M.M.; Chea, S.; Bui, T.X. Post-adoption behavior of digital media: The merge of U&G theory and affect event theory. In Proceedings of the Pacific Asia Conference on Information Systems, PACIS 2016, Chiayi City, Taiwan, 27 June–1 July 2016. [Google Scholar]
- Wakefield, R.; Wakefield, K. Social media network behavior: A study of user passion and affect. J. Strateg. Inf. Syst. 2016, 25, 140–156. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68. [Google Scholar] [CrossRef]
- Huang, Y.C.; Backman, S.J.; Backman, K.F.; McGuire, F.A.; Moore, D.W. An investigation of motivation and experience in virtual learning environments: A self-determination theory. Educ. Inf. Technol. 2019, 24, 591–611. [Google Scholar] [CrossRef]
- Proulx, J.N.; Romero, M.; Arnab, S. Learning Mechanics and Game Mechanics Under the Perspective of Self-Determination Theory to Foster Motivation in Digital Game Based Learning. Simul. Gaming 2017, 48, 81–97. [Google Scholar] [CrossRef]
- Zhang, Y. Understanding the sustained use of online health communities from a self-determination perspective. J. Assoc. Inf. Sci. Technol. 2016, 67, 2842–2857. [Google Scholar] [CrossRef]
- Hagger, M.S.; Sultan, S.; Hardcastle, S.J.; Chatzisarantis, N.L.D. Perceived autonomy support and autonomous motivation toward mathematics activities in educational and out-of-school contexts is related to mathematics homework behavior and attainment. Contemp. Educ. Psychol. 2015, 41, 111–123. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.K.J.; Liu, W.C.; Kee, Y.H.; Chian, L.K. Competence, autonomy, and relatedness in the classroom: Understanding students’ motivational processes using the self-determination theory. Heliyon 2019, 5, e01983. [Google Scholar] [CrossRef] [Green Version]
- Fathali, S.; Okada, T. Technology acceptance model in technology-enhanced OCLL contexts: A self-determination theory approach. Australas. J. Educ. Technol. 2018, 34. [Google Scholar] [CrossRef] [Green Version]
- Gorozidis, G.S.; Tzioumakis, Y.S.; Krommidas, C.; Papaioannou, A.G. Facebook group PETCoN (Physical Education Teacher Collaborative Network). An innovative approach to PE teacher in-service training: A self-determination theory perspective. Teach. Teach. Educ. 2020, 96, 103184. [Google Scholar] [CrossRef]
- Wang, X.; Li, Y. Users’ Satisfaction with Social Network Sites: A Self-Determination Perspective. J. Comput. Inf. Syst. 2016, 56, 48–54. [Google Scholar] [CrossRef]
- Pijnenborg, G.H.M.; Spikman, J.M.; Jeronimus, B.F.; Aleman, A. Insight in schizophrenia: Associations with empathy. Eur. Arch. Psychiatry Clin. Neurosci. 2013, 263, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Oh, S. The characteristics and motivations of health answerers for sharing information, knowledge, and experiences in online environments. J. Am. Soc. Inf. Sci. Technol. 2012, 63, 543–557. [Google Scholar] [CrossRef]
- Ringle, C.M.; Wende, S.; Becker, J.M. SmartPLS 3; SmartPLS: Bönningstedt, Germany, 2015. [Google Scholar]
- Hair, J.F., Jr.; Sarstedt, M.; Hopkins, L.; Kuppelwieser, V.G. Partial least squares structural equation modeling (PLS-SEM). Eur. Bus. Rev. 2014, 26, 106–121. [Google Scholar] [CrossRef]
- Ryan, T.P. Sample Size Determination and Power; Wiley: Hoboken, NJ, USA, 2013; ISBN 9781118439241. [Google Scholar]
- Chin, W.W. The partial least squares approach for structural equation modeling. In Modern Methods for Business Research; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1998; ISBN 9780805826777. [Google Scholar]
- Hair, J.F.; Risher, J.J.; Sarstedt, M.; Ringle, C.M. When to use and how to report the results of PLS-SEM. Eur. Bus. Rev. 2019, 31, 2–24. [Google Scholar] [CrossRef]
- Benitez, J.; Henseler, J.; Castillo, A.; Schuberth, F. How to perform and report an impactful analysis using partial least squares: Guidelines for confirmatory and explanatory IS research. Inf. Manag. 2020, 57, 103168. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioural Sciences; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Tseng, F.C.; Kuo, F.Y. A study of social participation and knowledge sharing in the teachers’ online professional community of practice. Comput. Educ. 2014, 72, 37–47. [Google Scholar] [CrossRef]
- Zaglia, M.E. Brand communities embedded in social networks. J. Bus. Res. 2013, 66, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Abrahamson, K.; Anderson, J.G.; Ha, S.; Widdows, R. Trust, empathy, social identity, and contribution of knowledge within patient online communities. Behav. Inf. Technol. 2013, 32, 1041–1104. [Google Scholar] [CrossRef]
- Massimi, M.; Bender, J.; Witteman, H.O.; Ahmed, O.H. Life transitions and online health communities: Reflecting on adoption, use, and disengagement. In Proceedings of the ACM Conference on Computer Supported Cooperative Work, CSCW, Baltimore, MD, USA, 15–19 February 2014; pp. 1491–1501. [Google Scholar]
- Puspitasari, I.; Jie, F. Making the Information Technology (IT) Business Alignment Works: A Framework of IT-based Competitive Strategy. Int. J. Bus. Inf. Syst. 2020, 34, 59–82. [Google Scholar] [CrossRef]
- Zheng, J. SARS-coV-2: An emerging coronavirus that causes a global threat. Int. J. Biol. Sci. 2020, 16, 1678–1685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, D.; Wu, T.; Liu, Q.; Yang, Z. The SARS-CoV-2 outbreak: What we know. Int. J. Infect. Dis. 2020, 94, 44–48. [Google Scholar] [CrossRef]
- Dalager-Pedersen, M.; Bodilsen, J. Thromboprophylaxis for medical inpatients with coronavirus disease 2019. Clin. Microbiol. Infect. 2020, 26, 1125. [Google Scholar] [CrossRef]

| Category | n (%), N = 428 |
|---|---|
| Age group (in years) | |
| 18–30 | 46 (10.75) |
| 31–40 | 113 (26.40) |
| 41–50 | 174 (40.65) |
| 51–60 | 79 (18.46) |
| >60 | 16 (3.74) |
| Gender | |
| Male | 181 (42.29) |
| Female | 247 (57.71) |
| Role | |
| Patient | 263 (61.45) |
| Family | 121 (28.27) |
| Caregiver | 44 (10.28) |
| Frequency of Use | |
| Daily | 36 (8.41) |
| Weekly | 155 (36.21) |
| Monthly | 147 (34.35) |
| As the need arises | 90 (21.03) |
| Construct | Indicator | Measurement Item (Survey’s Question) | Loading Factor | AVE |
|---|---|---|---|---|
| Interest to engage in a patient community | P1 | I joined a PSNS because I would like to help other patients with similar health conditions. | 0.887 | 0.731 |
| P2 | I am interested in sharing my experience and knowledge about specific health topics to others. | 0.931 | ||
| P3 | I am willing to go the extra mile to participate in a PSNS. | 0.736 | ||
| Empathy | E1 | I can feel the distress of other patients who have just been diagnosed with a disease. | 0.840 | 0.625 |
| E2 | I am willing to share my detailed experiences coping with a disease to support other patients. | 0.884 | ||
| E3 | I open myself more to others in a PSNS. | 0.712 | ||
| E4 | I enjoy participating and having good discussions via a PSNS. | 0.790 | ||
| E5 | It feels good to know that my contribution benefits others in a PSNS. | 0.712 | ||
| Use of patient social network systems | U1 | I frequently engage in a PSNS. | 0.775 | 0.606 |
| U2 | I intend to continue using a PSNS. | 0.823 | ||
| U3 | My interest to use a PSNS is high. | 0.735 |
| Interest to Engage in a Patient Community | Empathy | Use of Patient Social Network Systems | Composite Reliability | |
|---|---|---|---|---|
| Interest to engage in a patient community | 0.855 | 0.890 | ||
| Empathy | 0.840 | 0.790 | 0.892 | |
| Use of patient social network systems | 0.625 | 0.645 | 0.778 | 0.821 |
| Assessment | Value |
|---|---|
| Coeeficient of determination | R2 |
| Empathy | 0.757 (substantial) |
| Use of patient social network systems | 0.476 (moderate) |
| The predictive sample reuse technique | Q2 |
| Empathy | 0.503 |
| Use of patient social network systems | 0.355 |
| Effect size | f2 |
| H1: Interest to engage in a patient community → Empathy | 1.114 |
| H2: Interest to engage in a patient community → Use of patient social network systems | 0.159 |
| H3: Empathy → Use of patient social network systems | 0.413 |
| H4: Empathy -> Interest to engage in a patient community → Use of patient social network systems | 0.182 |
| Relationships among the hypothesized constructs and observable variables | Path coefficient (p value), [T-value] |
| H1: Interest to engage in a patient community → Empathy | 0.870 (p < 0.001), [46.819] |
| H2: Interest to engage in a patient community → Use of patient social network systems | 0.366 (p < 0.001), [3.480] |
| H3: Empathy → Use of patient social network systems | 0.503 (p < 0.001), [5.529] |
| H4: Empathy → Interest to engage in a patient community → Use of patient social network systems | 0.169 (p < 0.001), [4.862] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puspitasari, I.; Fauzi, S.S.M.; Ho, C.-Y. Factors Driving Users’ Engagement in Patient Social Network Systems. Informatics 2021, 8, 8. https://doi.org/10.3390/informatics8010008
Puspitasari I, Fauzi SSM, Ho C-Y. Factors Driving Users’ Engagement in Patient Social Network Systems. Informatics. 2021; 8(1):8. https://doi.org/10.3390/informatics8010008
Chicago/Turabian StylePuspitasari, Ira, Shukor Sanim Mohd Fauzi, and Cheng-Yuan Ho. 2021. "Factors Driving Users’ Engagement in Patient Social Network Systems" Informatics 8, no. 1: 8. https://doi.org/10.3390/informatics8010008





