Mathematical Modeling of Obstetric Variables: Influence of COVID-19, Periodontal Disease and Dental Care During Pregnancy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Initial Considerations
2.2. Ethical Considerations
2.3. Population and Sample
2.4. Analysis of Information
2.5. Defining Sets, Variables, and Operations
3. Results
3.1. Stage 1: Initial Exploratory Descriptive Analysis (5 Clinics)
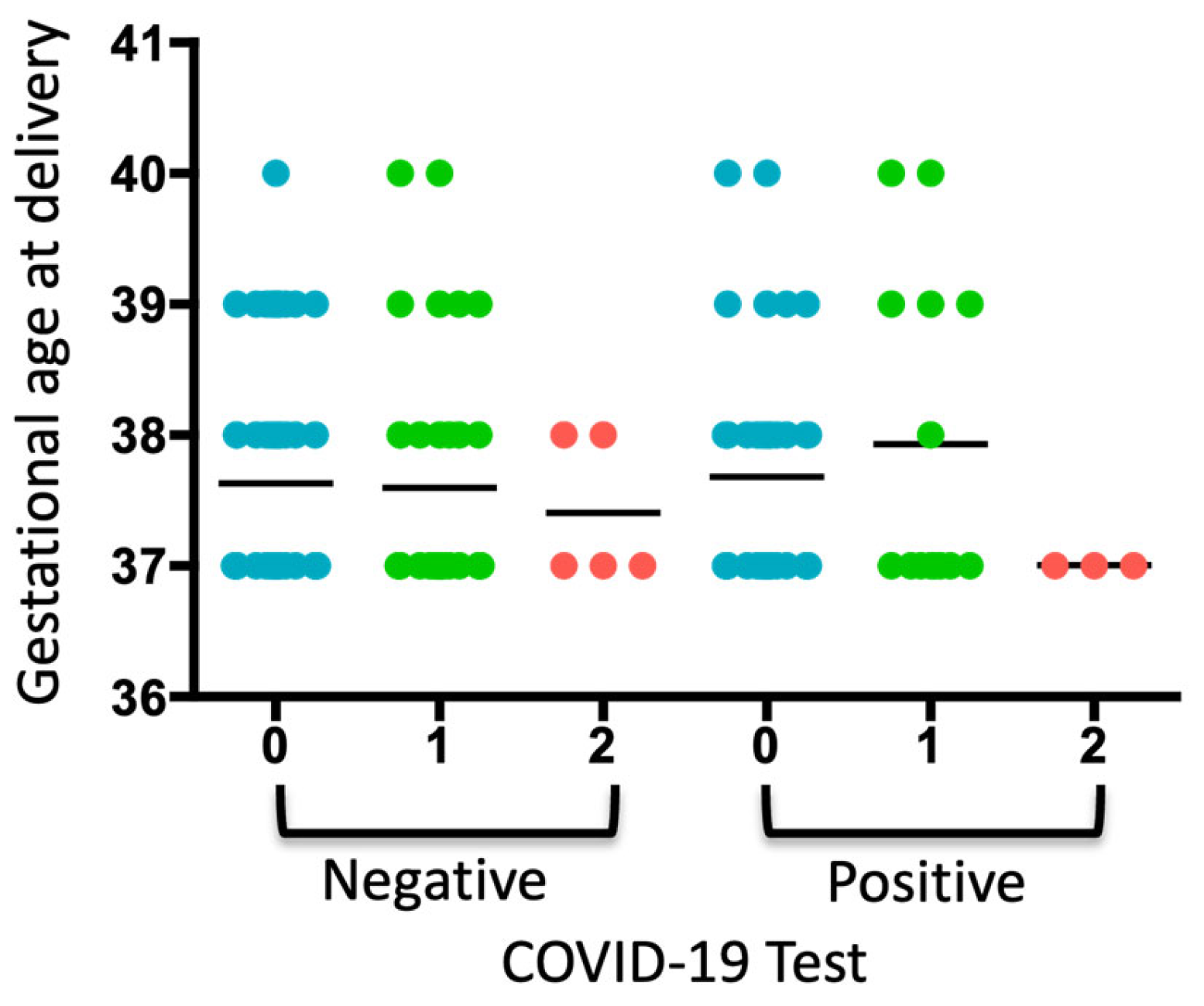
Bivariate Analysis
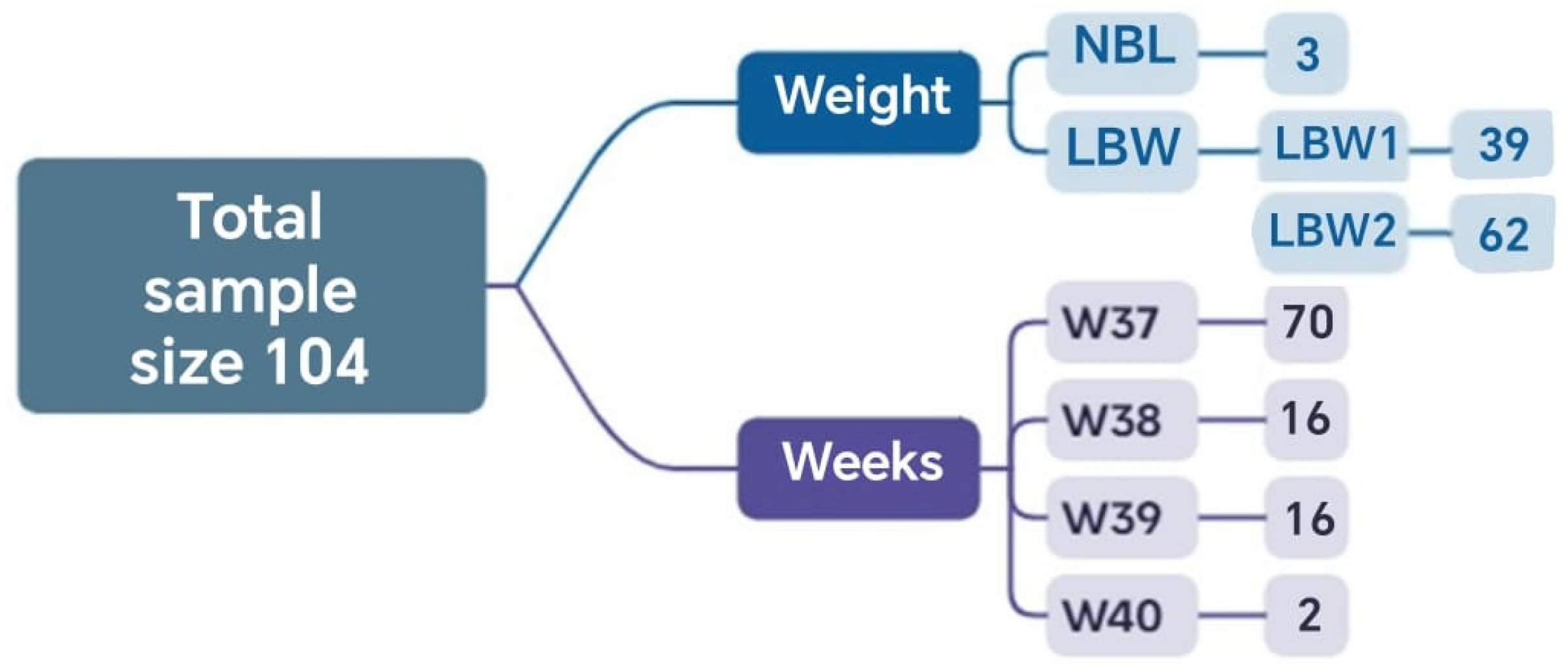
3.2. Stage 2: Analysis Using Set Theory and Probability—Hospital Universitario Clínica San Rafael (HUCSR)
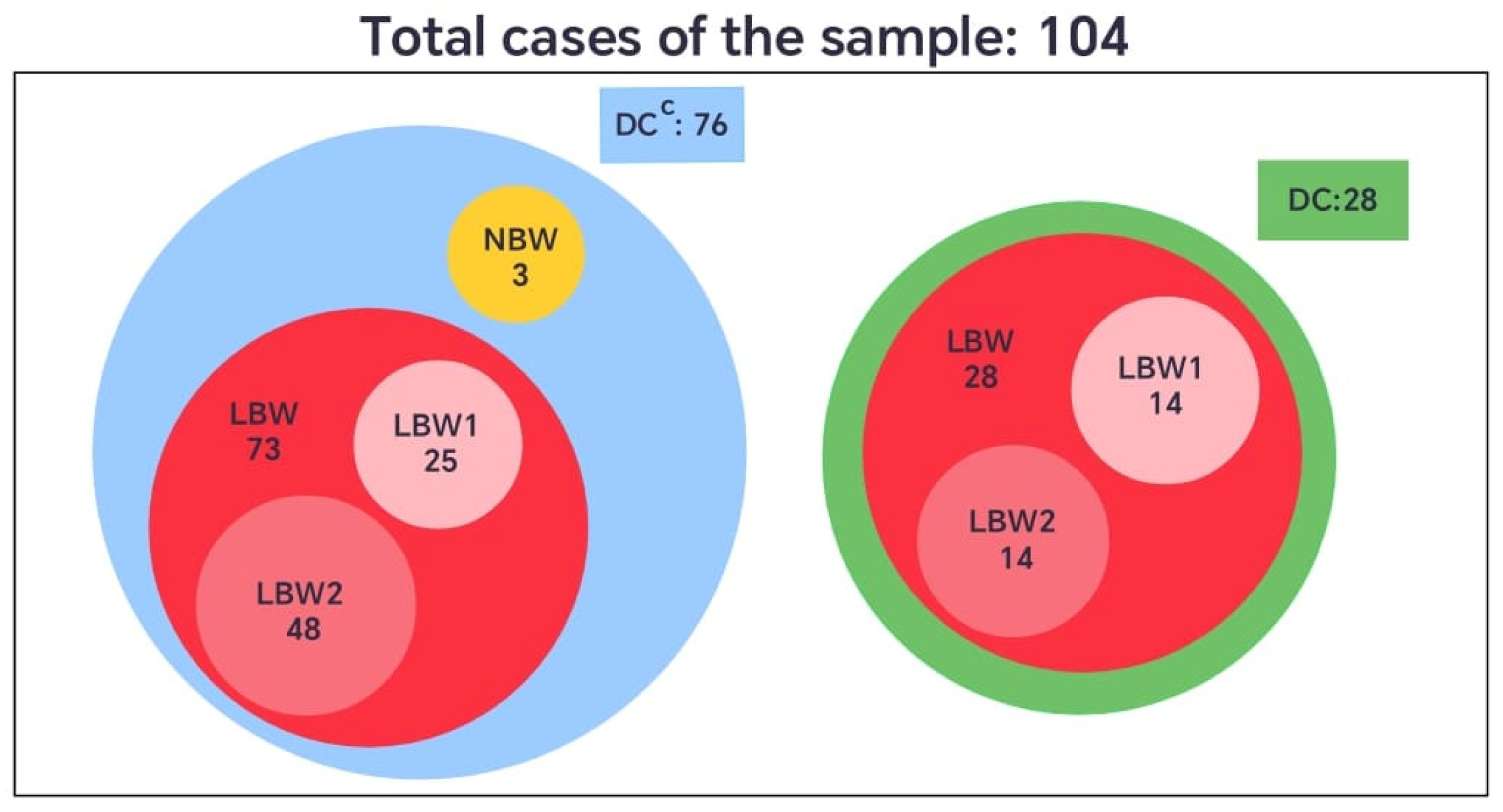
3.2.1. Phase 1: Analysis and Comparison of Groups of Pregnant Women with and Without Dental Care (DC vs. DCC)—HUCSR
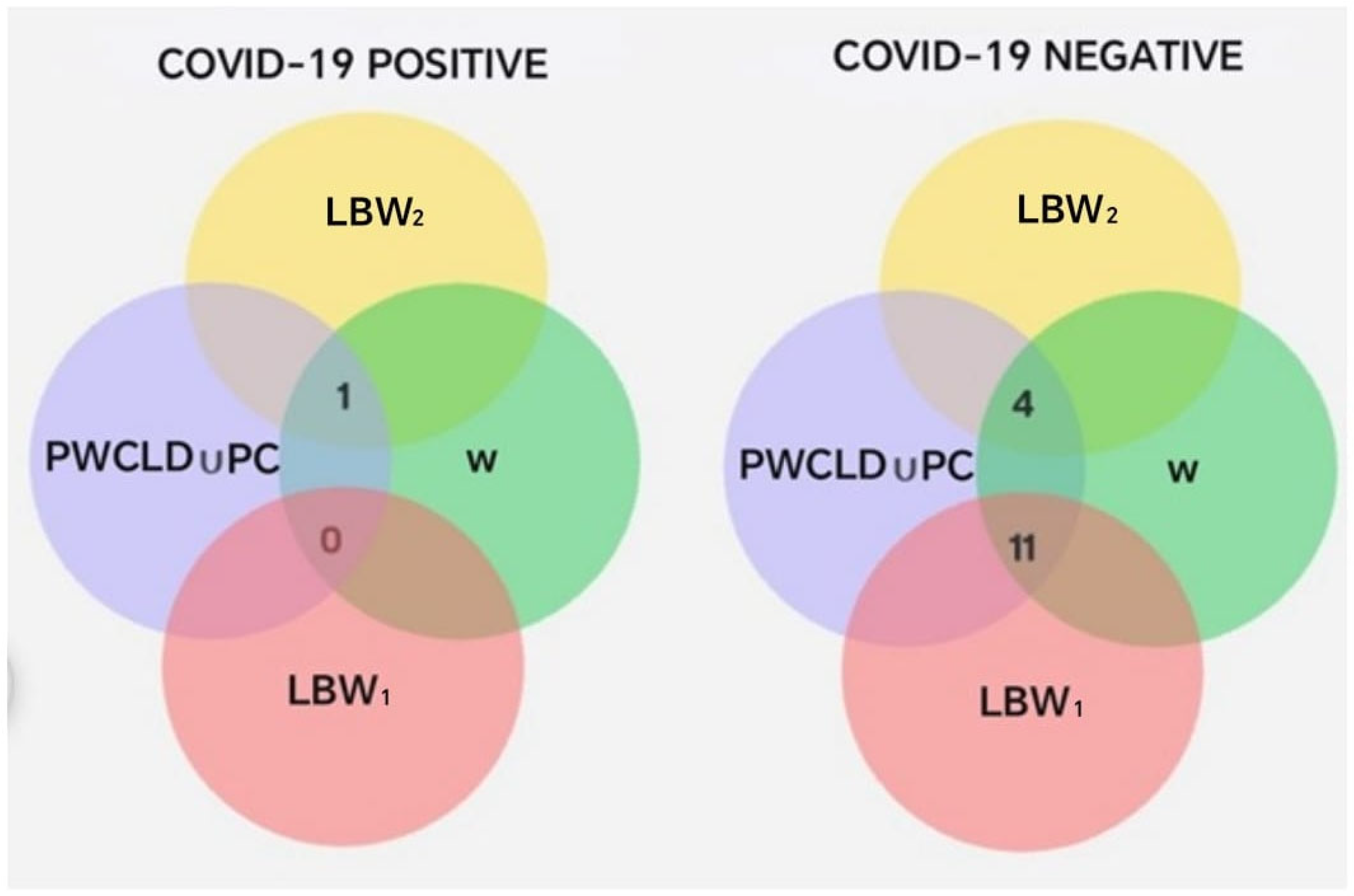
3.2.2. Phase 2: Analysis of Pregnant Women Who Received Dental Care, in Relation to COVID-19 Status, Gestational Age, Birth Weight, and Presence of Complications. HUCSR
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Caneiro-Queija, L.; Lopez-Carral, J.; Martin-Lancharro, P.; Limeres-Posse, J.; Diz-Dios, P.; Blanco-Carrion, J. Non-Surgical Treatment of Periodontal Disease in a Pregnant Caucasian Women Population: Adverse Pregnancy Outcomes of a Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2019, 16, 3638. [Google Scholar] [CrossRef]
- Latorre Uriza, C.; Velosa-Porras, J.; Roa, N.S.; Quinones Lara, S.M.; Silva, J.; Ruiz, A.J.; Escobar Arregoces, F.M. Periodontal Disease, Inflammatory Cytokines, and PGE2 in Pregnant Patients at Risk of Preterm Delivery: A Pilot Study. Infect. Dis. Obstet. Gynecol. 2018, 2018, 7027683. [Google Scholar] [CrossRef]
- Ohuma, E.O.; Moller, A.B.; Bradley, E.; Chakwera, S.; Hussain-Alkhateeb, L.; Lewin, A.; Okwaraji, Y.B.; Mahanani, W.R.; Johansson, E.W.; Lavin, T.; et al. National, regional, and global estimates of preterm birth in 2020, with trends from 2010: A systematic analysis. Lancet 2023, 402, 1261–1271. [Google Scholar] [CrossRef] [PubMed]
- Bradley, E.; Blencowe, H.; Moller, A.B.; Okwaraji, Y.B.; Sadler, F.; Gruending, A.; Moran, A.C.; Requejo, J.; Ohuma, E.O.; Lawn, J.E. Born too soon: Global epidemiology of preterm birth and drivers for change. Reprod. Health 2025, 22 (Suppl. S2), 105. [Google Scholar] [CrossRef] [PubMed]
- Boboshko, M.Y.; Savenko, I.V.; Garbaruk, E.S.; Knyazeva, V.M.; Vasilyeva, M.J. Impact of Prematurity on Auditory Processing in Children. Pathophysiology 2023, 30, 505–521. [Google Scholar] [CrossRef] [PubMed]
- Perunovic, N.; Rakic, M.M.; Nikolic, L.I.; Jankovic, S.M.; Aleksic, Z.M.; Plecas, D.V.; Madianos, P.N.; Cakic, S.S. The Association Between Periodontal Inflammation and Labor Triggers (Elevated Cytokine Levels) in Preterm Birth: A Cross-Sectional Study. J. Periodontol. 2016, 87, 248–256. [Google Scholar] [CrossRef]
- Presicce, P.; Roland, C.; Senthamaraikannan, P.; Cappelletti, M.; Hammons, M.; Miller, L.A.; Jobe, A.H.; Chougnet, C.A.; DeFranco, E.; Kallapur, S.G. IL-1 and TNF mediates IL-6 signaling at the maternal-fetal interface during intrauterine inflammation. Front. Immunol. 2024, 15, 1416162. [Google Scholar] [CrossRef]
- Park, J.Y.; Romero, R.; Lee, J.; Chaemsaithong, P.; Chaiyasit, N.; Yoon, B.H. An elevated amniotic fluid prostaglandin F2alpha concentration is associated with intra-amniotic inflammation/infection, and clinical and histologic chorioamnionitis, as well as impending preterm delivery in patients with preterm labor and intact membranes. J. Matern. Fetal. Neonatal. Med. 2016, 29, 2563–2572. [Google Scholar]
- Hong, J.S.; Romero, R.; Lee, D.C.; Than, N.G.; Yeo, L.; Chaemsaithong, P.; Ahn, S.; Kim, J.S.; Kim, C.J.; Kim, Y.M. Umbilical cord prostaglandins in term and preterm parturition. J. Matern. Fetal. Neonatal. Med. 2016, 29, 523–531. [Google Scholar] [CrossRef]
- Sanz, M.; Kornman, K.; Working Group 3 of the Joint EFP/AAP Workshop. Periodontitis and adverse pregnancy outcomes: Consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J. Periodontol. 2013, 84 (Suppl. S4), S164–S169. [Google Scholar] [CrossRef]
- Collins, J.G.; Smith, M.A.; Arnold, R.R.; Offenbacher, S. Effects of Escherichia coli and Porphyromonas gingivalis lipopolysaccharide on pregnancy outcome in the golden hamster. Infect. Immun. 1994, 62, 4652–4655. [Google Scholar] [CrossRef]
- da Silva, H.E.C.; Stefani, C.M.; de Santos Melo, N.; de Almeida de Lima, A.; Rosing, C.K.; Porporatti, A.L.; Canto, G.L. Effect of intra-pregnancy nonsurgical periodontal therapy on inflammatory biomarkers and adverse pregnancy outcomes: A systematic review with meta-analysis. Syst. Rev. 2017, 6, 197. [Google Scholar] [CrossRef]
- Tarannum, F.; Faizuddin, M. Association between gingival crevicular fluid prostaglandin E (2) level and preterm low birth weight. Indian J. Dent. Res. 2012, 23, 120. [Google Scholar] [CrossRef] [PubMed]
- Nannan, M.; Xiaoping, L.; Ying, J. Periodontal disease in pregnancy and adverse pregnancy outcomes: Progress in related mechanisms and management strategies. Front. Med. 2022, 9, 963956. [Google Scholar] [CrossRef] [PubMed]
- Pockpa, Z.A.D.; Soueidan, A.; Koffi-Coulibaly, N.T.; Limam, A.; Badran, Z.; Struillou, X. Periodontal Diseases and Adverse Pregnancy Outcomes: Review of Two Decades of Clinical Research. Oral. Health Prev. Dent. 2021, 19, 77–83. [Google Scholar] [PubMed]
- Mahendra, J.; Mahendra, L.; Mugri, M.H.; Sayed, M.E.; Bhandi, S.; Alshahrani, R.T.; Balaji, T.M.; Varadarajan, S.; Tanneeru, S.; Rao, P.A.N.; et al. Role of Periodontal Bacteria, Viruses, and Placental mir155 in Chronic Periodontitis and Preeclampsia-A Genetic Microbiological Study. Curr. Issues Mol. Biol. 2021, 43, 831–844. [Google Scholar] [CrossRef]
- Meric, P.; Silbereisen, A.; Emingil, G.; Ozturk, V.O.; Bostanci, N. Clinical, oral immunological and microbiological shifts during and after pregnancy. Clin. Oral. Investig. 2023, 28, 60. [Google Scholar] [CrossRef]
- Wang, W.; Sung, N.; Gilman-Sachs, A.; Kwak-Kim, J. T Helper (Th) Cell Profiles in Pregnancy and Recurrent Pregnancy Losses: Th1/Th2/Th9/Th17/Th22/Tfh Cells. Front. Immunol. 2020, 11, 2025. [Google Scholar] [CrossRef]
- Karimi, N.; Samiee, N.; Moradi, Y. The association between periodontal disease and risk of adverse maternal or neonatal outcomes: A systematic review and meta-analysis of analytical observational studies. Health Sci. Rep. 2023, 6, e1630. [Google Scholar] [CrossRef]
- Wu, M.; Ye, C.; Li, H.; Yang, X.; Zhu, S.; Zhou, F.; Hao, Y.; Chen, S.; Jiang, S. A Nested Case-Control Study of the Relationship between Salivary Inflammatory Mediators, Periodontal Parameters, and Preterm Birth in a Chinese Population. Biomed. Res. Int. 2022, 2022, 8629680. [Google Scholar] [CrossRef]
- Michalowicz, B.S.; Novak, M.J.; Hodges, J.S.; DiAngelis, A.; Buchanan, W.; Papapanou, P.N.; Mitchell, D.A.; Ferguson, J.E.; Lupo, V.; Bofill, J.; et al. Serum inflammatory mediators in pregnancy: Changes after periodontal treatment and association with pregnancy outcomes. J. Periodontol. 2009, 80, 1731–1741. [Google Scholar] [CrossRef]
- Stadelmann, P.; Alessandri, R.; Eick, S.; Salvi, G.E.; Surbek, D.; Sculean, A. The potential association between gingival crevicular fluid inflammatory mediators and adverse pregnancy outcomes: A systematic review. Clin. Oral. Investig. 2013, 17, 1453–1463. [Google Scholar] [CrossRef]
- AlSharief, M.; Alabdurubalnabi, E. Periodontal Pathogens and Adverse Pregnancy Outcomes: A Narrative Review. Life 2023, 13, 1559. [Google Scholar] [CrossRef] [PubMed]
- Gajbhiye, R.; Modi, D.; Mahale, S. Pregnancy outcomes, Newborn complications and Maternal-Fetal Transmission of SARS-CoV-2 in women with COVID-19: A systematic review of 441 cases. medRxiv 2020. [Google Scholar] [CrossRef]
- Gajbhiye, R.K.; Sawant, M.S.; Kuppusamy, P.; Surve, S.; Pasi, A.; Prusty, R.K.; Mahale, S.D.; Modi, D.N. Differential impact of COVID-19 in pregnant women from high-income countries and low- to middle-income countries: A systematic review and meta-analysis. Int. J. Gynaecol. Obstet. 2021, 155, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Guo, J.; Fan, C.; Juan, J.; Yu, X.; Li, J.; Feng, L.; Li, C.; Chen, H.; Qiao, Y.; et al. Coronavirus disease 2019 in pregnant women: A report based on 116 cases. Am. J. Obstet. Gynecol. 2020, 223, 111.e111–111.e114. [Google Scholar] [CrossRef]
- Hu, B.; Huang, S.; Yin, L. The cytokine storm and COVID-19. J. Med. Virol. 2021, 93, 250–256. [Google Scholar] [CrossRef]
- Allotey, J.; Stallings, E.; Bonet, M.; Yap, M.; Chatterjee, S.; Kew, T.; Debenham, L.; Llavall, A.C.; Dixit, A.; Zhou, D.; et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ 2020, 370, m3320. [Google Scholar] [CrossRef]
- Liu, H.; Wang, L.L.; Zhao, S.J.; Kwak-Kim, J.; Mor, G.; Liao, A.H. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J. Reprod. Immunol. 2020, 139, 103122. [Google Scholar] [CrossRef]
- Panahi, L.; Amiri, M.; Pouy, S. Risks of Novel Coronavirus Disease (COVID-19) in Pregnancy; a Narrative Review. Arch. Acad. Emerg. Med. 2020, 8, e34. [Google Scholar]
- Zhao, X.; Jiang, Y.; Zhao, Y.; Xi, H.; Liu, C.; Qu, F.; Feng, X. Analysis of the susceptibility to COVID-19 in pregnancy and recommendations on potential drug screening. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 39, 1209–1220. [Google Scholar] [CrossRef]
- Butera, A.; Maiorani, C.; Morandini, A.; Simonini, M.; Colnaghi, A.; Morittu, S.; Barbieri, S.; Ricci, M.; Guerrisi, G.; Piloni, D.; et al. Assessment of Oral Microbiome Changes in Healthy and COVID-19-Affected Pregnant Women: A Narrative Review. Microorganisms 2021, 9, 2385. [Google Scholar] [CrossRef]
- Green, J.; Petty, J.; Whiting, L.; Fowler, C. Exploring modifiable risk-factors for premature birth in the context of COVID-19 mitigation measures: A discussion paper. J. Neonatal. Nurs. 2021, 27, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Basso, L.; Chacun, D.; Sy, K.; Grosgogeat, B.; Gritsch, K. Periodontal Diseases and COVID-19: A Scoping Review. Eur. J. Dent. 2021, 15, 768–775. [Google Scholar] [CrossRef] [PubMed]
- Anand, P.S.; Jadhav, P.; Kamath, K.P.; Kumar, S.R.; Vijayalaxmi, S.; Anil, S. A case-control study on the association between periodontitis and coronavirus disease (COVID-19). J. Periodontol. 2022, 93, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Budhram, S.; Vannevel, V.; Botha, T.; Chauke, L.; Bhoora, S.; Balie, G.M.; Odell, N.; Lombaard, H.; Wise, A.; Georgiou, C.; et al. Maternal characteristics and pregnancy outcomes of hospitalized pregnant women with SARS-CoV-2 infection in South Africa: An International Network of Obstetric Survey Systems-based cohort study. Int. J. Gynaecol. Obstet. 2021, 155, 455–465. [Google Scholar] [CrossRef]
- Aabakke, A.J.M.; Krebs, L.; Petersen, T.G.; Kjeldsen, F.S.; Corn, G.; Wojdemann, K.; Ibsen, M.H.; Jonsdottir, F.; Ronneberg, E.; Andersen, C.S.; et al. SARS-CoV-2 infection in pregnancy in Denmark-characteristics and outcomes after confirmed infection in pregnancy: A nationwide, prospective, population-based cohort study. Acta Obstet. Gynecol. Scand. 2021, 100, 2097–2110. [Google Scholar] [CrossRef]
- Cosma, S.; Carosso, A.R.; Cusato, J.; Borella, F.; Bertero, L.; Bovetti, M.; Bevilacqua, F.; Mengozzi, G.; Mazzone, R.; Ghisetti, V.; et al. Obstetric and neonatal outcomes after SARS-CoV-2 infection in the first trimester of pregnancy: A prospective comparative study. J. Obstet. Gynaecol. Res. 2022, 48, 393–401. [Google Scholar] [CrossRef]
- Iheozor-Ejiofor, Z.; Middleton, P.; Esposito, M.; Glenny, A.M. Treating periodontal disease for preventing adverse birth outcomes in pregnant women. Cochrane Database Syst. Rev. 2017, 6, CD005297. [Google Scholar] [CrossRef]
- Bobetsis, Y.A.; Graziani, F.; Gursoy, M.; Madianos, P.N. Periodontal disease and adverse pregnancy outcomes. Periodontol. 2000 2020, 83, 154–174. [Google Scholar] [CrossRef]
- Wu, J.; Wu, J.; Tang, B.; Zhang, Z.; Wei, F.; Yu, D.; Li, L.; Zhao, Y.; Wang, B.; Wu, W.; et al. Effects of different periodontal interventions on the risk of adverse pregnancy outcomes in pregnant women: A systematic review and network meta-analysis of randomized controlled trials. Front. Public Health 2024, 12, 1373691. [Google Scholar] [CrossRef]
- Hrbacek, K.; Jech, T. Introduction to Set Theory, 3rd ed.; Marcel Dekker: New York, NY, USA, 1999. [Google Scholar]
- De Laplace, M. Philosophical Essay on Probabilities; Altaya: Barcelona, Spain, 1995. [Google Scholar]
- Feynman, R.P.; Leighton, R.B.; Sands, M. The Feynman Lectures on Physics; Addison-Wesley Iberoamericana: Wilmington, DE, USA, 1964; Volume 1, p. 46. [Google Scholar]
- Mood, A.; Graybill, F.D.B. Introduction to the Theory of Statistics; McGraw-Hill: Singapore, 1974. [Google Scholar]
- Montoya-Restrepo, N.E.; Correa-Morales, J.C. Curvas de peso al nacer. Rev. Salud Pública 2007, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Marouf, N.; Cai, W.; Said, K.N.; Daas, H.; Diab, H.; Chinta, V.R.; Hssain, A.A.; Nicolau, B.; Sanz, M.; Tamimi, F. Association between periodontitis and severity of COVID-19 infection: A case-control study. J. Clin. Periodontol. 2021, 48, 483–491. [Google Scholar] [CrossRef]
- Sari, A.; Dikmen, N.K.; Nibali, L. Association between periodontal diseases and COVID-19 infection: A case-control study with a longitudinal arm. Odontology 2023, 111, 1009–1017. [Google Scholar] [CrossRef] [PubMed]
- Al-Maweri, S.A.; Alhajj, M.N.; Halboub, E.; Tamimi, F.; Salleh, N.M.; Al-Ak’hali, M.S.; Kassim, S.; Abdulrab, S.; Anweigi, L.; Mohammed, M.M.A. The impact of periodontal disease on the clinical outcomes of COVID-19: A systematic review and meta-analysis. BMC Oral Health 2023, 23, 658. [Google Scholar] [CrossRef] [PubMed]
- Qi, M.; Sun, W.; Wang, K.; Li, W.; Lin, J.; Gong, J.; Wang, L. Periodontitis and COVID-19: Immunological Characteristics, Related Pathways, and Association. Int. J. Mol. Sci. 2023, 24, 3012. [Google Scholar] [CrossRef]
- Rodríguez-Montaño, R.; Baltazar-Díaz, T.A.; Hernández-Mora, O.; Isiordia-Espinoza, M.A.; Del Muro-Casas, F.; González-González, R.; Bologna-Molina, R.; López-Verdín, S. Periodontal Disease Elevates IL-6 Levels During Initial Symptoms of COVID-19. Diagnostics 2025, 15, 1650. [Google Scholar] [CrossRef]
- Macherla, S.; Chopra, A.; Ramanarayanan, V.; Das, R.S.; Garg, R. Can periodontitis affect the COVID-19 severity, symptoms, hospital stay, and mortality? A case-control study. Front. Public Health 2024, 12, 1421380. [Google Scholar] [CrossRef]
- Ide, M.; Papapanou, P.N. Epidemiology of association between maternal periodontal disease and adverse pregnancy outcomes--systematic review. J. Clin. Periodontol. 2013, 40 (Suppl. S14), S181–S194. [Google Scholar] [CrossRef]
- Zhang, Y.; Feng, W.; Li, J.; Cui, L.; Chen, Z.J. Periodontal Disease and Adverse Neonatal Outcomes: A Systematic Review and Meta-Analysis. Front. Pediatr. 2022, 10, 799740. [Google Scholar] [CrossRef]
- Daalderop, L.A.; Wieland, B.V.; Tomsin, K.; Reyes, L.; Kramer, B.W.; Vanterpool, S.F.; Been, J.V. Periodontal Disease and Pregnancy Outcomes: Overview of Systematic Reviews. JDR Clin. Trans. Res. 2018, 3, 10–27. [Google Scholar] [CrossRef]
- Corbella, S.; Taschieri, S.; Francetti, L.; De Siena, F.; Del Fabbro, M. Periodontal disease as a risk factor for adverse pregnancy outcomes: A systematic review and meta-analysis of case-control studies. Odontology 2012, 100, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Corbella, S.; Taschieri, S.; Del Fabbro, M.; Francetti, L.; Weinstein, R.; Ferrazzi, E. Adverse pregnancy outcomes and periodontitis: A systematic review and meta-analysis exploring potential association. Quintessence Int. 2016, 47, 193–204. [Google Scholar] [PubMed]
- Khader, Y.S.; Ta’ani, Q. Periodontal diseases and the risk of preterm birth and low birth weight: A meta-analysis. J. Periodontol. 2005, 76, 161–165. [Google Scholar] [CrossRef]
- Le, Q.A.; Akhter, R.; Coulton, K.M.; Vo, N.T.N.; Duong, L.T.Y.; Nong, H.V.; Yaacoub, A.; Condous, G.; Eberhard, J.; Nanan, R. Periodontitis and Preeclampsia in Pregnancy: A Systematic Review and Meta-Analysis. Matern. Child. Health J. 2022, 26, 2419–2443. [Google Scholar] [CrossRef]
- Machado, V.; Ferreira, M.; Lopes, L.; Mendes, J.J.; Botelho, J. Adverse Pregnancy Outcomes and Maternal Periodontal Disease: An Overview on Meta-Analytic and Methodological Quality. J. Clin. Med. 2023, 12, 3635. [Google Scholar] [CrossRef]
- Castaño-Suárez, L.; Paternina-Mejía, G.Y.; Vásquez-Olmos, L.D.; Rodríguez-Medina, C.; Botero, J.E. Linking Periodontitis to Adverse Pregnancy Outcomes: A Comprehensive Review and Meta-analysis. Curr. Oral Health Rep. 2024, 11, 125–137. [Google Scholar] [CrossRef]
- Yao, X.D.; Zhu, L.J.; Yin, J.; Wen, J. Impacts of COVID-19 pandemic on preterm birth: A systematic review and meta-analysis. Public Health 2022, 213, 127–134. [Google Scholar] [CrossRef]
- Fernández, M.C.; del Mazo, L.D.; Toledo, L.S.; Pérez, Y.U.; Lobaina, Y.M.L. Clinical and epidemiological aspects in pregnant women with gingival disease. Medisan 2017, 21, 3350–3361. [Google Scholar]
- Saaqib, S.; Saaqib, Y.; Zeeshan, M. COVID-19 in pregnancy—A literature review. J. Pak. Med. Assoc. 2022, 72, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, M.; Garcia-Ruiz, I.; Maiz, N.; Rodo, C.; Garcia-Manau, P.; Serrano, B.; Lopez-Martinez, R.M.; Balcells, J.; Fernandez-Hidalgo, N.; Carreras, E.; et al. Pre-eclampsia-like syndrome induced by severe COVID-19: A prospective observational study. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 1374–1380. [Google Scholar] [CrossRef]
- Juan, J.; Gil, M.M.; Rong, Z.; Zhang, Y.; Yang, H.; Poon, L.C. Effect of coronavirus disease 2019 (COVID-19) on maternal, perinatal and neonatal outcome: Systematic review. Ultrasound Obstet. Gynecol. 2020, 56, 15–27. [Google Scholar] [CrossRef]
- Martínez-González, B.; Garza-Reséndez, N.; Contreras-Garza, N.Y.; González-Oropeza, D. Risk combination: COVID-19 and preeclampsia. Case series and bibliographic review. Ginecol. Obstet. Méx. 2021, 89, 622–634. [Google Scholar]
- Rodriguez-Wallberg, K.A.; Nilsson, H.P.; Rothe, E.B.; Zhao, A.; Shah, P.S.; Acharya, G. Outcomes of SARS-CoV-2 infection in early pregnancy-A systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 2024, 103, 786–798. [Google Scholar] [CrossRef] [PubMed]
- Metz, T.D.; Clifton, R.G.; Hughes, B.L.; Sandoval, G.J.; Grobman, W.A.; Saade, G.R.; Manuck, T.A.; Longo, M.; Sowles, A.; Clark, K.; et al. Association of SARS-CoV-2 Infection With Serious Maternal Morbidity and Mortality from Obstetric Complications. JAMA 2022, 327, 748–759. [Google Scholar] [CrossRef] [PubMed]
- Fallach, N.; Segal, Y.; Agassy, J.; Perez, G.; Peretz, A.; Chodick, G.; Gazit, S.; Patalon, T.; Ben Tov, A.; Goldshtein, I. Pregnancy outcomes after SARS-CoV-2 infection by trimester: A large, population-based cohort study. PLoS ONE 2022, 17, e0270893. [Google Scholar] [CrossRef]
- Boettcher, L.B.; Metz, T.D. Maternal and neonatal outcomes following SARS-CoV-2 infection. Semin. Fetal Neonatal. Med. 2023, 28, 101428. [Google Scholar] [CrossRef]
- Newton, S.M.; Reeves, E.L.; O’Malley Olsen, E.; Woodworth, K.R.; Farr, S.L.; Galang, R.R.; Reynolds, M.R.; Harvey, E.; Shi, J.; Nestoridi, E.; et al. Preterm birth among pregnant persons with severe acute respiratory syndrome Coronavirus 2 infection. J. Perinatol. 2022, 42, 1328–1337. [Google Scholar] [CrossRef]
- Lopez, N.J.; Smith, P.C.; Gutierrez, J. Periodontal therapy may reduce the risk of preterm low birth weight in women with periodontal disease: A randomized controlled trial. J. Periodontol. 2002, 73, 911–924. [Google Scholar] [CrossRef]
- Tarannum, F.; Faizuddin, M. Effect of periodontal therapy on pregnancy outcome in women affected by periodontitis. J. Periodontol. 2007, 78, 2095–2103. [Google Scholar] [CrossRef]
- Murakami, S.; Mealey, B.L.; Mariotti, A.; Chapple, I.L.C. Dental plaque-induced gingival conditions. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S17–S27. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-Filho, E.S.; de Melo, N.R.; Sorpreso, I.C.E.; Bahamondes, L.; Simoes, R.D.S.; Soares-Junior, J.M.; Baracat, E.C. Contraception and reproductive planning during the COVID-19 pandemic. Expert Rev. Clin. Pharmacol. 2020, 13, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Takeshita, Y.; Kanda, T. [The Blood-Brain Barrier (BBB) and in vitro BBB Models]. Brain Nerve 2015, 67, 1035–1042. [Google Scholar] [PubMed]
- Cupul-Uicab, L.A.; Hernandez-Mariano, J.A.; Vazquez-Salas, A.; Leyva-Lopez, A.; Barrientos-Gutierrez, T.; Villalobos Hernandez, A. COVID-19 durante el embarazo: Revisión rápida y metaanálisis. Salud Publica Mex. 2021, 63, 242–252. [Google Scholar] [CrossRef]
- Metz, T.D.; Clifton, R.G.; Hughes, B.L.; Sandoval, G.; Saade, G.R.; Grobman, W.A.; Manuck, T.A.; Miodovnik, M.; Sowles, A.; Clark, K.; et al. Disease Severity and Perinatal Outcomes of Pregnant Patients With Coronavirus Disease 2019 (COVID-19). Obstet. Gynecol. 2021, 137, 571–580. [Google Scholar] [CrossRef]
- Wei, S.Q.; Bilodeau-Bertrand, M.; Liu, S.; Auger, N. The impact of COVID-19 on pregnancy outcomes: A systematic review and meta-analysis. Can. Med Assoc. J. 2021, 193, E540–E548. [Google Scholar] [CrossRef]
- Vousden, N.; Bunch, K.; Morris, E.; Simpson, N.; Gale, C.; O’Brien, P.; Quigley, M.; Brocklehurst, P.; Kurinczuk, J.J.; Knight, M. The incidence, characteristics and outcomes of pregnant women hospitalized with symptomatic and asymptomatic SARS-CoV-2 infection in the UK from March to September 2020: A national cohort study using the UK Obstetric Surveillance System (UKOSS). PLoS ONE 2021, 16, e0251123. [Google Scholar] [CrossRef]
- Garrido, J.M.; Martinez-Rodriguez, D.; Rodriguez-Serrano, F.; Perez-Villares, J.M.; Ferreiro-Marzal, A.; Jimenez-Quintana, M.M.; Study Group, C.G.; Villanueva, R.J. Mathematical model optimized for prediction and health care planning for COVID-19. Med. Intensiva. (Engl. Ed.) 2022, 46, 248–258. [Google Scholar] [CrossRef]
- Espinosa, C.; Becker, M.; Maric, I.; Wong, R.J.; Shaw, G.M.; Gaudilliere, B.; Aghaeepour, N.; Stevenson, D.K. Data-Driven Modeling of Pregnancy-Related Complications. Trends. Mol. Med. 2021, 27, 762–776. [Google Scholar] [CrossRef]
- Devlin, K. The Joy of Sets: Fundamentals of Contemporary Set Theory; Springer Science & Business Media: New York, NY, USA, 1994. [Google Scholar]
- Halmos, P.R. Naive Set Theory; Van Nostrand: Princeton, NJ, USA, 1960. [Google Scholar]
- Rodríguez, J.; Prieto, S.; Bernal, P.; Pérez, C.; Correa, C.; Vitery, S. Set theory applied to populations of leukocytes, lymphocytes and CD4 of patients with HIV. Prediction of CD4 T lymphocytes, for clinical application. Rev. Fac. Med. 2011, 19, 148–156. [Google Scholar]
- Alaminos-Fernández, A.F. Introducción a la Teoría de Conjuntos Difusos y Sus Aplicaciones en Investigación Social e IA; Limencop, S.L., Ed.; Universidad de Alicante: San Vicente del Raspeig, Spain, 2023. [Google Scholar]
- Singh, R.; Bhardwaj, N. Fuzzy Soft Set Theory Applications in Medical Diagnosis: A Comprehensive Review and the Roadmap for Future Studies. New Math. Nat. Comput. 2025, 21, 597–619. [Google Scholar] [CrossRef]




| Mathematical Sets | |
|---|---|
| Name | Description |
| DCC | Pregnant women who did not receive dental care during pregnancy. DC complement. |
| DC | Pregnant women who received dental care during pregnancy. |
| CO | Pregnant women diagnosed with COVID-19 in DC. |
| COC | Complement of CO. Pregnant women not diagnosed with COVID-19 in DC. |
| OD | Pregnant women diagnosed with oral diseases in DC |
| ODC | Pregnant women without any oral disease in DC. Complement of OD. |
| LBW | Neonates with low birth weight [46]. |
| LBW1 | Neonates with low birth weight ranging from 1501 g to 2284 g. |
| LBW2 | Neonates with low birth weight ranging from 2285 g to 2499 g. |
| NBW | Neonates with normal birth weight [46]. |
| W37 | Neonates born at 37 weeks of gestation |
| W38 | Neonates born at 38 weeks of gestation |
| W39 | Neonates born at 39 weeks of gestation |
| W40 | Neonates born at 40 weeks of gestation |
| PWCLD | Pregnant women who experienced complications during labor and delivery |
| PWCLDC | Pregnant women who did not experience complications during labor and delivery. Complement of PWCLD |
| PC | Pregnant women with pregnancy-related complications. |
| UCPC | Pregnant women with uncomplicated pregnancies. Complement of PC. |
| Variables | |
|---|---|
| Name | Description |
| P | The variable representing neonatal birth weight was analyzed using the LBW and NBW sets. Additionally, the LBW set was subdivided into smaller subsets (LBW1 and LBW2) to achieve a clearer understanding and more detailed analysis of this group. |
| S | The variable representing gestational age, defined as the number of weeks elapsed until delivery, was analyzed using the W37, W38, W39, and W40 sets. |
| C | The Complications variable was analyzed using the PWCLD, PWCLDC, PC, and UCPC sets. |
| Complications of Childbirth | N (%) |
|---|---|
| Fetal distress | 6 (10.9%) |
| Induction failure | 6 (10.9%) |
| Abnormalities in the dynamics of childbirth | 6 (10.09%) |
| Edema, proteinuria, and hypertensive disorders in pregnancy, childbirth, and the postpartum period | 5 (9.09%) |
| Fetal abnormalities and lesions | 3 (5.5%) |
| Fetus and amniotic cavity with possible delivery problems | 3 (5.5%) |
| Unspecified abnormality of the fetus | 2 (3.6%) |
| Infection of the amniotic sac and/or membranes | 1 (1.8%) |
| Complications in labor | 1 (1.8%) |
| Resuscitation in the womb | 1 (1.8%) |
| Periodontal Diagnosis (n = 156) | Weight of the Newborn (g) | p Value |
|---|---|---|
| No diagnosis | 2302 (SD: 376) | 0.45 |
| Gingivitis | 2302 (SD: 150) | |
| Periodontitis | 2396 (SD: 98) | |
| Gestational age of delivery (weeks) | ||
| No diagnosis | 37.65 (SD: 0.84) | 0.47 |
| Gingivitis | 37.69 (SD: 1.04) | |
| Periodontitis | 37.25 (SD: 0.46) |
| Periodontal Therapy (156) | Weight of the Newborn (g) | p Value |
|---|---|---|
| No therapy | 2319 (SD: 323) | 0.50 |
| Supragingival | 2309 (SD: 142) | |
| SRP | 2295 (SD: 106) | |
| OHI | 2180 (SD: 0.00) | |
| Gestational age at delivery (weeks) | ||
| No therapy | 37.69 (SD: 0.90) | 0.07 |
| Supragingival | 37.10 (SD: 0.31) | |
| SRP | 37.00 (SD: 0.0) | |
| OHI | 37.00 (SD: 0.0) |
| Intersection | (P) | DC(P) | Intersection | (P) | (P) |
|---|---|---|---|---|---|
| 49 (0.471) | 21 (0.202) | 0 (0.000) | 0 (0.000) | ||
| 13 (0.125) | 2 (0.019) | 1 (0.010) | 0 (0.000) | ||
| 10 (0.096) | 4 (0.038) | 2 (0.019) | 0 (0.000) | ||
| 1 (0.010) | 1 (0.010) | 0 (0.000) | 0 (0.000) |
| Intersection | ||
|---|---|---|
| 19 (0.188) | 10 (0.099) | |
| 30 (0.297) | 11 (0.109) | |
| 2 (0.020) | 1 (0.010) | |
| 11 (0.109) | 1 (0.010) | |
| 4 (0.040) | 3 (0.030) | |
| 6 (0.059) | 1 (0.010) | |
| 0 (0.000) | 0 (0.000) | |
| 1 (0.010) | 1 (0.010) |
| Intersection | CO | COC | Intersection | CO | COC |
|---|---|---|---|---|---|
| 1 (0.036) | 0 (0.000) | 5 (0.178) | 0 (0.000) | ||
| 0 (0.000) | 9 (0.321) | 0 (0.000) | 6 (0.214) | ||
| 0 (0.000) | 1 (0.036) | 0 (0.000) | 1 (0.036) | ||
| 0 (0.000) | 3 (0.107) | 0 (0.000) | 1 (0.036) | ||
| 0 (0.000) | 0 (0.000) | 0 (0.000) | 1 (0.036) |
| Intersection | LBW1 | LBW2 |
|---|---|---|
| ∩ PC ∩ | 5 (0.013) | 1 (0.063) |
| ∩ PWCLD ∩ | 3 (0.188) | 1 (0.063) |
| ∩ PWCLD ∩ | 0 (0.000) | 1 (0.063) |
| ∩ PWCLD ∩ | 3 (0.188) | 1 (0.063) |
| ∩ PC ∩ | 0 (0.000) | 1 (0.063) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Velosa-Porras, J.; Correa Herrera, S.C.; Mejía Reyes, K.L.; Fuentes Rojas, P.S.; Ardila Ortiz, L.D.; Ospina, O.L.; Prieto-Bohórquez, S.; Jattin Balcázar, J.J.; Guevara Muñoz, J.E.; Bonilla Cortés, L.; et al. Mathematical Modeling of Obstetric Variables: Influence of COVID-19, Periodontal Disease and Dental Care During Pregnancy. Biomedicines 2025, 13, 2919. https://doi.org/10.3390/biomedicines13122919
Velosa-Porras J, Correa Herrera SC, Mejía Reyes KL, Fuentes Rojas PS, Ardila Ortiz LD, Ospina OL, Prieto-Bohórquez S, Jattin Balcázar JJ, Guevara Muñoz JE, Bonilla Cortés L, et al. Mathematical Modeling of Obstetric Variables: Influence of COVID-19, Periodontal Disease and Dental Care During Pregnancy. Biomedicines. 2025; 13(12):2919. https://doi.org/10.3390/biomedicines13122919
Chicago/Turabian StyleVelosa-Porras, Juliana, Sandra Catalina Correa Herrera, Katherine Lucia Mejía Reyes, Paula Sofía Fuentes Rojas, Laura Daniela Ardila Ortiz, Olga Lucía Ospina, Signed Prieto-Bohórquez, Jairo Javier Jattin Balcázar, Jorge Edgar Guevara Muñoz, Leonardo Bonilla Cortés, and et al. 2025. "Mathematical Modeling of Obstetric Variables: Influence of COVID-19, Periodontal Disease and Dental Care During Pregnancy" Biomedicines 13, no. 12: 2919. https://doi.org/10.3390/biomedicines13122919
APA StyleVelosa-Porras, J., Correa Herrera, S. C., Mejía Reyes, K. L., Fuentes Rojas, P. S., Ardila Ortiz, L. D., Ospina, O. L., Prieto-Bohórquez, S., Jattin Balcázar, J. J., Guevara Muñoz, J. E., Bonilla Cortés, L., Mora-Méndez, J. M., Latorre Uriza, C., Escobar Arregoces, F. M., & Roa, N. S. (2025). Mathematical Modeling of Obstetric Variables: Influence of COVID-19, Periodontal Disease and Dental Care During Pregnancy. Biomedicines, 13(12), 2919. https://doi.org/10.3390/biomedicines13122919







