Highlights
What are the main findings?
- Older adults in rural areas reported lower self-rated successful aging (SSAS) and personal wellbeing (PWI) than those in urban/suburban areas. PWI was the strongest positive predictor while rural residence and chronic illness were negative predictors.
- Active community involvement was positively associated with quality of life, whereas regret over missed opportunities or past actions had negative associations; no significant gender differences were observed in SSAS or PWI.
What are the implications of the main findings?
- Promoting social engagement and psychosocial support could improve successful aging in rural areas
- Considering wellbeing alongside health status and addressing rural disparities could improve aging programs.
Abstract
Background: Population aging has increased attention on the quality of life and successful aging of older adults. Objective: To examine urban–rural differences in subjective quality of life and self-rated successful aging, explore associations with psychosocial factors, and identify predictors of successful aging, including potential moderating effects of place of residence and chronic illness. Methods: A cross-sectional study was conducted among 403 adults aged ≥ 60 years in Eastern Croatia. Measures included a sociodemographic questionnaire, the Self-assessment of Successful Aging Scale (SSAS), and the Personal Wellbeing Index (PWI). Data were analyzed using nonparametric tests (Mann–Whitney U, Spearman’s correlation), linear regression, and moderation analyses. Significance was set at p < 0.05. Ethical approval was obtained (Class: 602-01/24-12/02; IRB: 2158/97-97-10-24-36). Results: Rural participants reported lower PWI scores (p = 0.005) and self-rated successful aging (p < 0.001) than urban participants. Active community involvement was positively associated with quality of life (Rho = 0.46; p < 0.001), whereas regret about missed opportunities and past actions was negatively associated (Rho = −0.20; p < 0.01). Regression analyses explained 48.3% of the variance in SSAS, with higher PWI scores being strongly associated with higher SSAS scores, and rural residence and chronic illness being associated with lower SSAS scores. Moderation analyses indicated that the association between PWI and SSAS was consistent across different environmental contexts and in the presence of illness. Conclusions: Older adults living in rural areas reported lower quality of life and self-rated successful aging compared with those in urban and suburban areas, with subjective wellbeing emerging as a key predictor. Promoting social engagement and addressing psychosocial barriers may enhance successful aging, particularly in rural populations. Findings suggest that social engagement and psychosocial support are associated with higher level of perceived successful aging, indicating potential areas for future community-based or healthcare interventions.
1. Introduction
The pace of global population aging has accelerated markedly compared with previous decades. In 2020, the number of individuals aged 60 years and older surpassed the number of children under five [1], and current projections indicate that this demographic will increase from approximately one billion in 2020 to more than two billion by 2050, with one in six people worldwide expected to be aged 60 years or older by 2030 [2]. Concurrently, the population of adults aged 80 years and above is projected to triple, rising from about 140 million in 2020 to approximately 426 million by 2050 [1].
Although increased life expectancy is widely recognized as an indicator of biomedical, social, and economic advancement [3], population aging simultaneously poses a substantial challenge to the sustainability of these systems [4]. Accelerating demographic trends, coupled with systemic pressures, may compromise the living conditions and overall wellbeing of older adults. Population aging is therefore characterized not only by changes in the age structure of the population but also by shifts in the health and social care needs of older adults, the availability and organization of care systems, and the social dynamics shaped by the specific contexts in which older adults live.
Older adults are considered a high-risk group in terms of health and quality of life [5], being particularly vulnerable to chronic diseases, geriatric syndromes, and multimorbidity, which in turn increases the demand for healthcare services [6,7,8,9]. Moreover, they face a higher likelihood of requiring both formal and informal long-term care [10,11]. Therefore, it is crucial to ensure environments in which additional years of life are spent living in good health and within supportive settings, where individuals’ ability to remain functional, independent, and active is minimally constrained [12]. In this context, ensuring a high quality of life in later life occupies a central role.
1.1. Biopsychosocial Perspectives on Quality of Life in Older Adults
Quality of life is defined as an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns [13]. It is a complex, multidimensional construct encompassing physical health, psychological state, level of independence, social relationships, personal beliefs, and one’s relationship to key features of the environment. Quality-of-life assessment is inherently subjective and shaped by the context in which a person lives [13], reflecting the interplay of biological, psychological, and social factors [14]. Accordingly, the present study examines the subjective dimension of quality of life, with particular attention given to the personal wellbeing of older adults.
Although quality of life tends to decline in very old age, its association with chronological age is not linear, as periods of relative stability and even potential improvement may occur [15]. The process is highly dynamic and individualized [16], supporting an understanding of aging as a heterogeneous phenomenon characterized by concurrent losses and compensatory adaptations [17].
Given this dynamic and heterogeneous nature of aging, quality of life in older adults is examined within a biopsychosocial framework [5], extending beyond earlier approaches that focused solely on health status. Notably, self-perceived quality of life can remain high despite physical decline [14], underscoring its subjective and complex nature. Due to its multidimensionality, a variety of factors influence quality of life among older adults [16]. This framework conceptualizes quality of life as a dynamic process, in which daily opportunities and available resources shape individuals’ perceptions of their own aging. Subjective assessments are thus oriented toward incorporating factors and resources that enable older adults to perceive themselves as successful in the aging process, even amidst health or social limitations.
1.2. Successful Aging
Successful aging involves the preservation of physical, cognitive, and social functioning, along with the maintenance of high quality of life, including its subjective dimensions [18]. It entails the ability of older adults to maintain daily independence, participate actively in their communities, and adapt to life with chronic conditions or functional limitations [8]. The relationship between quality of life and successful aging has become an increasingly important area of research, particularly in societies with a growing proportion of older adults [19]. Implementing strategies that promote biological, psychological, and social wellbeing can enhance quality of life and support successful aging [20].
Considering the pronounced differences in resource availability, social networks, and living conditions between urban and rural areas [21], there is a need for a deeper understanding of how these contexts shape the quality of life and successful aging of older adults.
1.3. Integrated and Community-Oriented Approaches to Supporting Subjective Quality of Life and Successful Aging
Beyond individual biopsychosocial determinants, contemporary approaches to aging increasingly emphasize the role of integrated and community-oriented models of care and support [22] in supporting functional ability, independence, and quality of life among older adults. As aging is frequently accompanied by chronic conditions, multimorbidity, and complex care needs [5,6,7,8,9], older adults often interact with multiple health and social care providers, which places them at heightened risk of fragmented and poorly coordinated care. Fragmented care is associated with unmet needs, lower patient satisfaction, inefficient use of health services, and poorer health outcomes [23], highlighting the importance of integrated care models that ensure continuity and coordination across sectors and levels of care. In response to these challenges, the World Health Organization has promoted the Integrated Care for Older People (ICOPE) approach, which focuses on maintaining and optimizing intrinsic capacity and functional ability through person-centered, coordinated health and social services, particularly within community settings [24]. Importantly, the effectiveness of integrated care models for older adults is increasingly evaluated not only through clinical or service-related indicators, but also through patient-reported outcomes, including subjective quality of life and functional performance in everyday life. Umbrella reviews and systematic evidence syntheses identify quality of life as an outcome in the assessment of integrated and community-based care interventions for older populations [22]. These considerations are particularly relevant in contexts characterized by urban–rural disparities in service availability, accessibility, and social infrastructure, including geographical remoteness and transport-related barriers [25,26]. Additional structural barriers to care, reduced access to specialized services, and more limited social resources can shape older adults’ quality of life and opportunities for successful aging. Understanding how subjective quality of life and perceptions of successful aging vary across different living environments is therefore essential for informing the development and contextual adaptation of integrated, community-oriented approaches to supporting older adults.
1.4. Aims and Hypoteses
The primary aims of this study were to examine urban–rural differences in subjective quality of life and self-rated successful aging among older adults and to analyze their associations with psychosocial factors. The secondary aims were to identify predictors of successful aging, including the potential moderating effects of place of residence and chronic illness. To address these aims, the following hypotheses were formulated:
Hypothesis 1.
There are significant differences in subjective quality of life, measured by the Personal Well-Being Index (PWI), and self-rated successful aging (SSAS) between older adults living in urban and rural areas.
Hypothesis 2.
Higher subjective quality of life (PWI) is associated with higher levels of self-rated successful aging (SSAS).
Hypothesis 3.
Subjective quality of life (PWI), place of residence (urban vs. rural), and the presence of chronic illness predict self-rated successful aging (SSAS).
Hypothesis 4.
Place of residence (urban vs. rural) and the presence of chronic illness moderate the relationship between subjective quality of life (PWI) and self-rated successful aging (SSAS).
2. Materials and Methods
2.1. Study Design
This quantitative cross-sectional study across urban and rural settings was conducted between January and June 2024 in the Eastern region of Croatia—Slavonia in participants’ homes. The study is part of a larger research project on successful aging, from which a previous article has been published [27]. However, this study focuses on new analyses examining urban–rural differences in self-rated successful aging (SSAS) and subjective quality of life (PWI), their associations with psychosocial factors (community involvement and regret), and predictors of successful aging, including potential moderating effects of place of residence and chronic illness.
2.2. Participants
The study population comprised community-dwelling older adults, defined according to the United Nations classification as individuals aged 60 years and above [28]. Eligibility criteria included: (1) chronological age ≥ 60 years, (2) ability to provide informed consent, and (3) residence in the community, excluding individuals living in institutionalized care facilities. Participants’ place of residence was classified according to administrative boundaries in line with European statistical approaches [29]. Urban and suburban areas included settlements within city administrative boundaries or administratively connected suburban settlements, while rural areas encompassed villages.
Based on these criteria, the minimum required sample size (n = 384) was calculated using an online Sample Size Calculator [30], assuming a 95% confidence level and a 5% margin of error for a population of 181,904 older adults aged 60 years and older in the Eastern region of Croatia (Slavonia). The final sample included 403 participants, exceeding the minimum required sample size.
The final sample consisted of 175 men (43.4%) and 228 women (56.6%), with a median age of 70 years (range: 60–92). No participants identified as “Other” gender.
Power analysis confirmed that the achieved sample size provided sufficient statistical power (≥0.80) for all analyses performed, including multivariate regression (observed power = 0.95) [31].
A non-probability quota sampling strategy was applied to ensure proportional representation of urban and rural participants, followed by snowball sampling. The response rate was 83%. The participant selection process is illustrated in Figure 1 in accordance with STROBE recommendations.
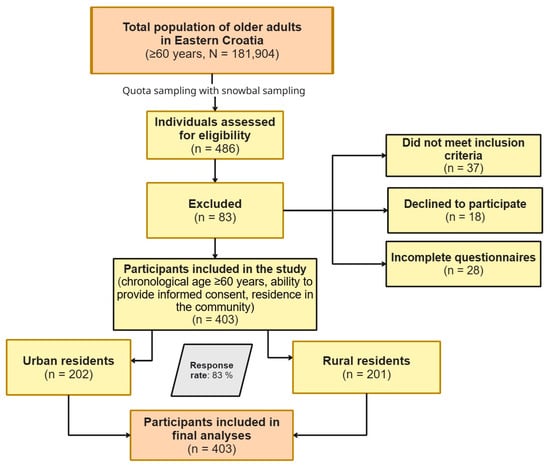
Figure 1.
Flow diagram of participant recruitment and allocation of urban and rural older adults using quota and snowball sampling.
2.3. Instruments
The study employed validated instruments, including the Personal Wellbeing Index (PWI) [32] and the Self-assessment of Successful Aging Scale (SSAS) [33].
The PWI measures personal wellbeing through seven items of satisfaction, each corresponding to a quality of life domain: standard of living, health, achievements in life, personal relationships, sense of security, community connectedness, and future security. These domains are theoretically embedded, representing the first level of deconstruction of the global question, “How satisfied are you with your life as a whole?”. Responses are rated on an 11-point scale (0–10), ranging from “no satisfaction at all” to “completely satisfied,” with the overall score calculated as the mean of all domains. In this study, PWI scores are interpreted as reflecting the subjective dimension of quality of life, and the scale demonstrates high internal consistency (Cronbach’s α = 0.85, McDonald’s ω = 0.87).
The SSAS [34] consists of 20 items evaluating individuals’ perceptions of their own aging experience, using a five-point Likert scale (1 = “does not apply to me at all” to 5 = “fully applies to me”). The total score, calculated as the mean of all items, ranges from 20 to 100, with higher scores indicating a more positive perception of successful aging. The scale demonstrates high internal consistency (Cronbach’s α = 0.88, McDonald’s ω = 0.89).
The survey also included general and sociodemographic questions, followed by three additional items assessing participants’ perceived level of engagement in their community, regret over missed opportunities, and regret regarding past actions they now consider unwise. These items, drawn from the literature [33], relate to constructs discussed in the context of personal wellbeing and successful aging, particularly community engagement and regret as self-evaluative experiences.
2.4. Data Collection
Data were gathered using a non-probability quota sampling framework to achieve proportional representation of urban and rural participants, reflecting the study’s emphasis on socio-environmental determinants. Recruitment was further facilitated through a chain-referral procedure (snowball sampling technique), whereby enrolled individuals identified additional eligible participants. Data were collected in participants’ homes. Prior to fieldwork, research staff completed targeted training in communication strategies and psychological approaches relevant to engagement with older adults. Prospective participants received comprehensive written and verbal briefings on study objectives, procedures, and ethical safeguards, and provided written informed consent. Participation was fully voluntary and anonymous, with the option to withdraw at any point. Surveys were completed independently using the paper-and-pen method, with researchers providing clarification only to support comprehension without influencing responses. During the assessment of the Personal Wellbeing Index, researchers followed the authors’ administration guidelines, which require allowing respondents to skip items they do not understand and avoiding any additional explanations or examples that could shape item interpretation [32]. No time restrictions were imposed.
2.5. Ethical Considerations
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki (1975, revised in 2013) [35]. Participation was voluntary and anonymous, and participants could withdraw at any time. Written approval was obtained from the Higher Institution Ethical Committee of the Faculty of Dental Medicine and Health Osijek (Class: 602-01/24-12/02; IRB: 2158/97-97-10-24-36). All participants received written and verbal information regarding the study’s aims, procedures, and ethical considerations, and provided written informed consent. Surveys were completed independently; researchers offered clarification only to support comprehension without guiding responses. Anonymity was maintained during and after data collection by separating the survey from the informed consent forms.
2.6. Data Analysis
The frequency distributions of variables were described using descriptive statistical methods. The distribution of continuous variables was assessed using the Shapiro–Wilk test, which indicated statistically significant deviations from normality (p < 0.05). Accordingly, measures of central tendency and dispersion were reported as medians (Me) and interquartile ranges (IQR). Differences between two independent groups were examined using the Mann–Whitney U test. Associations between variables were assessed using Spearman’s rank correlation coefficient (ρ).
Linear regression analysis using a stepwise method was conducted to examine predictors of SSAS. Prior to the regression analysis, assumptions of linearity, normality of residuals, homoscedasticity, and absence of multicollinearity were assessed and met. Although regression models were applied to examine the predictive relationships between variables, the cross-sectional nature of the study precludes causal interpretation of the observed associations. Additional moderation analyses were performed to examine whether the association between PWI and SSAS was moderated by place of residence or the presence of chronic illness. Statistical significance was set at p < 0.05.
All analyses were conducted using MedCalc® Statistical Software version 22.023 (MedCalc Software Ltd., Ostend, Belgium), IBM SPSS Statistics version 23.0 (IBM Corp., Armonk, NY, USA), and JASP version 0.19.3 (University of Amsterdam, The Netherlands).
3. Results
A total of 403 participants from the eastern region of Croatia–Slavonia took part in the study. Their median age was 70 years (range 60–92), and the majority were female (n = 228, 56.6%). Participants were almost equally divided by place of residence, with 202 (50.1%) living in a city/suburban area and 201 (49.9%) living in a village. Regarding educational attainment, most participants had completed secondary education (n = 183, 45.4%), followed by primary education (n = 172, 42.7%). The majority were married (n = 210, 52.1%). Household monthly income varied, with 11 participants (2.7%) reporting no income, while the largest proportion (n = 120, 29.8%) reported income of 132.72–318.54 EUR per month. More than half of the participants (n = 206, 51.1%) reported at least one chronic illness, most commonly cardiovascular disorders (n = 108, 51.4%) and endocrine system disorders (n = 71, 34.0%), while no respondents reported integumentary or lymphatic system disorders.
Participants also rated their community involvement, regret regarding missed opportunities, and regret about past actions with a median score of 3 (IQR 2–4) for all three items (Table 1).

Table 1.
Sociodemographic characteristics of respondents.
Between-group differences in self-perceived successful aging and quality-of-life indicators were assessed using the Mann–Whitney U test. Participants residing in rural areas reported significantly lower levels of self-assessed successful aging (median 67, IQR 58–75) compared with their urban/suburban counterparts (median 72, IQR 64–78; p < 0.001). They also had lower scores on the PWI (median 64, IQR 50–78 vs. 69, IQR 57–80; p = 0.005). Within the PWI domains, rural participants reported significantly lower satisfaction with Health (p = 0.02), Achieving in life (p = 0.01), Relationships (p = 0.04), Safety (p < 0.001), Community (p = 0.02), and Future security (p = 0.02). No significant difference was observed for the Standard of living domain (p = 0.06) (Table 2).

Table 2.
Differences in SSAS and PWI scores between urban/suburban and rural older adults.
Between-group differences between male and female older adults in self-perceived successful aging and quality-of-life indicators were assessed using the Mann–Whitney U test. No statistically significant differences were observed (Table 3).

Table 3.
Differences in SSAS and PWI scores between male and female older adults.
Spearman’s rank correlation coefficient (ρ) was used to assess the relationships between the scales, subscales, and participants’ age, perceived level of active involvement in the community, extent of regret for missed opportunities in life, and extent of regret for actions now considered wrong.
Age was negatively correlated with scores on the standard of living and self-rated successful aging scales (−0.145; p <0.001), indicating that older participants tended to report lower levels on these measures, while correlations with the PWI scale and its subscales were not significant. Perceived active involvement in the community was positively correlated with the PWI scale and all its subscales (ρ = 0.258–0.438; p <0.001), including standard of living, health, life achievements, close relationships, security, sense of belonging, future security, and the personal quality-of-life index. Extent of regret for missed opportunities and regret for actions now considered wrong were negatively correlated with several subscales, including life achievements, close relationships, safety, and the PWI (Table 4).

Table 4.
Associations between SSAS and PWI domains and age, community involvement, and regret measures.
Correlation between the Self-assessment of Successful Aging Scale and the Personal Wellbeing Index (PWI) with its subscales was assessed using Spearman’s rank correlation coefficient. The Self-assessment of Successful Ageing Scale was positively correlated with the PWI total score and all subscales. Correlation coefficients ranged from moderate (ρ = 0.397–0.490) for PWI total, Achieving, Safety, and Community, to strong (ρ > 0.50) for Standard of living, Health, Relationships, and Future, with all statistically significant (p < 0.001) (Table 5).

Table 5.
Correlations between SSAS and PWI domains.
Prior to conducting linear regression, assumptions of multicollinearity, normality, linearity, and homoscedasticity were assessed. Variance inflation factors (VIFs) indicated no multicollinearity among predictors (VIF < 2). Residuals were examined using Q–Q plots and scatterplots, which confirmed approximate normality and linearity. No influential cases were identified (Cook’s distance < 0.05). Subsequently, a linear regression using a stepwise method was conducted to examine predictors of SSAS. Four models were tested: the intercept-only model (M0), a model including only the total PWI (M1), a model including PWI and place of residence (0 = City/suburban, 1 = Village; M2), and a model including PWI, place of residence and dummy variable in presence of chronic illness (0 = No, 1 = Yes; M3). The intercept-only model (M0) is omitted as it provides no meaningful information.
M1 was significant and explained 45.9% of the variance in SSAS (R2 = 0.459, Adjusted R2 = 0.457; F(1, 396) = 335.51, p < 0.001). Higher PWI scores predicted higher SSAS scores (B = 0.608, SE = 0.033, β = 0.677, t = 18.32, p < 0.001).
M2 added place of residence and further increased explained variance to 47.8% (R2 = 0.478, Adjusted R2 = 0.475; F(2, 395) = 180.492, p < 0.001). Higher PWI scores remained a strong positive predictor (B = 0.589, SE = 0.033, β = 0.656, t = 17.818, p < 0.001), and living in a village was associated with lower SSAS scores (B = –3.232, SE = 0.856, β = –0.139, t = –3.775, p < 0.001).
M3 was significant and explained 48.3% of the variance in SSAS (R2 = 0.483, Adjusted R2 = 0.475; F(3, 394) = 122.495, p < 0.001). Higher PWI scores remained a strong positive predictor (B = 0.571, SE = 0.034, β = 0.636, t = 16.747, p < 0.001), living in a village remained associated with lower SSAS scores (B = −3.293, SE = 0.854, β = −0.142, t = −3.857, p < 0.001), and the presence of chronic illness was associated with lower SSAS scores (B = −1.719, SE = 0.873, t = −1.968, p = 0.05) (Table 6).

Table 6.
Linear regression of PWI, place of residence and chronic illness as a predictors of SSAS.
Additional moderation analyses were conducted to examine whether the relationship between PWI and SSAS was moderated by place of residence or the presence of chronic illness. The overall model was significant (R2 = 0.487, Adjusted R2 = 0.479, F(6, 391) = 61.820, p < 0.001). PWI was a significant positive predictor of SSAS (B = 0.589, β = 0.656, t = 9.145, p < 0.001). None of the interaction terms were statistically significant (all p > 0.05), and therefore, only the main effects were interpreted. Neither the presence of chronic illness (B = −1.934, t = −0.544, p = 0.587) nor place of residence (B = 1.235, β = 0.053, t = 0.341, p = 0.737) were significant predictors.
4. Discussion
Due to the global trend of population aging, there has been a growing emphasis on studying quality of life and successful aging among older adults [36,37]. This study specifically examined differences and factors associated with successful aging, considering the contrasts between urban and rural areas as well as accounting for the presence of chronic illness, which are theoretically expected to negatively affect successful aging [18]. In particular, the study aimed to determine whether quality of life, as a subjective dimension that can typically be enhanced through psychosocial interventions and community-based public health programs [38], represents the factor most strongly associated with successful aging, potentially independent of comorbid conditions. To address these questions, the study included equally distributed participants, with 202 (50.1%) residing in urban areas and 201 (49.9%) in rural areas. The median age was 70 years, and approximately half of the participants had chronic illness, which is expected given the increased risk of various health conditions in older age [39].
Although the conceptualization of successful aging in this study is theoretically grounded in the classical model proposed by Rowe and Kahn [18], it is important to acknowledge the limitations inherent in approaches that equate successful aging primarily with the absence of disease and high levels of functional capacity [40,41,42]. The findings of the present study partially challenge this biomedical emphasis. Subjective quality of life was independently associated with self-rated successful aging, regardless of the presence of chronic illness. This suggests that successful aging, as operationalized in this study, should not be understood solely as an outcome of optimal health status, but rather as a subjective and contextually embedded process shaped by personal wellbeing, adaptive capacities, and lived experience. These results align with contemporary shifts toward more inclusive and person-centered conceptualizations of aging well [40].
Furthermore, the observed urban–rural disparities underscore the importance of examining successful aging within broader socio-environmental contexts. The results indicate a persistent disparity between urban and rural areas, highlighting the need to examine various dimensions of quality of life and successful aging while considering sociodemographic factors that may shape these outcomes. Therefore, this discussion focuses on sociodemographic determinants, the subjective dimension of quality of life, and successful aging. Although studies often examine separate constructs, such as quality of life and personal wellbeing, their combined interpretation is justified because they are theoretically linked, with personal wellbeing considered as a subjective dimension of quality of life [32].
4.1. Sociodemographic Differences Between Urban and Rural Areas
The analysis of sociodemographic determinants revealed no statistically significant gender differences in personal wellbeing or in successful aging. These findings are consistent with the results reported by Vuletić and Stapić [43], who likewise observed no significant gender differences in personal wellbeing among older adults. However, evidence from other studies suggests that gender differences in quality of life [44] and successful aging [45,46] do exist. Such differences appear to be strongly shaped by cultural and social contexts, including gender roles and broader environmental conditions. Consequently, gender-related variations in self-perceptions of quality of life and successful aging are not universal but vary across countries and sociocultural settings. In the present study, chronological age was found to be significantly and negatively associated with successful aging. This finding contrasts with the results reported by Tucak Junaković et al. [47], in which age emerged as a significant positive predictor of successful aging. The authors interpreted this association by suggesting that individuals who reach advanced age may perceive longevity itself as an indicator of successful aging. The discrepancy between these findings may be partly explained by regional characteristics of the studied populations. The present study was conducted in Eastern Croatia (Slavonia), the least developed macroregion in the country [48], characterized by particularly unfavorable demographic trends compared with other Croatian regions [49]. The population of this area was heavily affected by war related losses in the early 1990s, and the age group examined in this study largely belonged to the adult population at that time. As a result, a substantial portion of their lives was spent under conditions of prolonged socioeconomic insecurity [50], which may negatively shape perceptions of one’s own aging. In contrast, the study by Tucak Junaković et al. [47] was conducted in Dalmatian counties and the City of Zagreb. According to the Organization for Economic Cooperation and Development (OECD) report [51], the City of Zagreb represents the most productive region in Croatia, while residents of Zagreb and, to a lesser extent, coastal areas tend to have higher incomes, higher educational attainment, and longer life expectancy than those living in other continental regions of Croatia. Such a context may provide a more supportive social environment for older adults, fostering greater social participation, more stable social networks, and a more positive experience of aging.
4.2. Urban–Rural Differences in Personal Wellbeing as the Subjective Dimension of Quality of Life
The subjective dimension of quality of life, measured using the Personal Wellbeing Index encompassing seven domains, showed notable differences between urban and rural areas. Participants residing in rural settings scored lower across most domains of subjective quality of life. These results align with the findings reported by Pekçetin et al. [52].
Consistent with the findings of lower rated health among participants from rural areas, Jiang et al. [53] report that older adults in rural areas more frequently perceive their health as poor, experience higher rates of depressive symptoms, and encounter greater difficulties in functional abilities. As a result, functional decline tends to occur earlier in rural populations than in urban ones. These rural and urban differences are largely associated with the socioeconomic status of older adults [53].
Lower satisfaction with close relationships among older adults should be interpreted in the context of urban–rural differences in social support networks. According to Iverson et al. [54], older adults in rural settings most often rely on family and friends as primary sources of support, particularly for practical daily needs, while formal services are less accessible. In contrast, participants from urban areas highlight broader access to formal and professional support resources, although some report lower satisfaction with social support and a weaker sense of safety in their neighborhoods. Social support is shaped by the specific characteristics of the environment, with older adults in rural areas relying more on informal networks and those in urban areas more on formal sources of help [54]. These differences should be considered when planning support for the older population.
In rural settings, participants reported lower levels of satisfaction with safety and future security, which may reflect limited quality and availability of services, including healthcare, as well as deteriorating environmental conditions and infrastructure [55]. Moreover, perceiving one’s immediate environment as safe is crucial for maintaining quality of life in older adulthood [56]. Feelings of insecurity among older adults are often linked to neighborhood problems and reduced trust in other residents. Those facing the most pronounced neighborhood issues report greater insecurity both in their surroundings and within their own homes, as well as an increased fear of crime [56]. Together, these findings underscore the important role of the immediate environment in shaping older adults’ subjective sense of safety.
Lower perceived life achievement among older adults reflects the combined effects of multiple interrelated factors accumulating across the life course. Older adults in rural settings often experience reduced social functioning and higher levels of social isolation, frequently linked to limited transportation options and fewer opportunities for participation in social and community activities [57]. These social constraints are accompanied by a higher burden of chronic conditions, more pronounced depressive symptoms, and greater memory difficulties, all of which are strongly associated with lower quality of life [57]. Furthermore, educational attainment in rural populations is often lower compared with urban counterparts, while higher education has consistently been associated with better quality of life and lower levels of disability in later life [58]. From a life-course perspective, these disadvantages are not isolated but accumulate over time, as conceptualized in cumulative advantage/disadvantage theory [59]. Individuals residing in rural areas may face limited educational and occupational opportunities, lower income, and restricted access to health and social services throughout their lives. Such prolonged exposure to socioeconomic adversity may contribute to lower perceived life achievement among rural older adults. Taken together, these findings suggest that lower self-rated life achievement in rural older adults is likely the product of interacting social, health, educational, and cumulative socioeconomic disadvantages.
Community belonging in rural areas is shaped by both structural constraints and social dynamics. Although rural areas are often characterized by a strong sense of mutual connectedness and greater perceived support within the local community [60], and longer-term residence contributes to stronger relationships with community members, better knowledge of the neighborhood, and a stronger sense of belonging [61], rural participants in the study reported lower levels of perceived community participation. This discrepancy can potentially be explained by structural constraints, such as greater physical isolation due to limited transportation and fewer opportunities to engage in social activities [57]. Additionally, increased migration among newer generations modifies the social composition of rural communities; the absence of neighbors during the day negatively affects older adults’ perception of belonging [60]. Economic and infrastructural limitations in rural areas further reduce opportunities for participation in organized activities [21], providing additional context for understanding the study findings. Neville et al. [62] emphasize that engagement in a rural community depends on the interconnection between physical and social environments, with transportation being a key factor for older adults’ ability to engage, a resource that is often less adapted to their needs in rural areas. Thus, differences in perceived community belonging between urban and rural settings can be interpreted within the context of interactions between resource availability and specific social relationships, both of which shape older adults’ sense of inclusion in the community.
4.3. Urban–Rural Differences in Successful Aging and Quality of Life
Lower levels of SSAS and wellbeing as a component of subjective quality of life among rural participants are the result of multiple factors. Song et al. [21] note that slower economic development in rural regions, combined with limited access to key resources that support an enabling environment for older adults, such as communal spaces, recreational facilities, and healthcare services, restricts their opportunities. Economic constraints in these areas reduce work and social opportunities, leading to less frequent participation in organized activities [21]. Limited access to transportation further reduces opportunities to utilize healthcare, social, and recreational services [63]. Older adults’ willingness and ability to travel to healthcare services are influenced by age, socioeconomic status, and transportation challenges, including mode of transport, costs, safety, and availability of public transit [64], which are often more pronounced in rural regions. Additionally, research suggests a higher prevalence of chronic diseases, more depressive symptoms, and memory difficulties in rural areas [57]. These findings contrast with the theoretical model of successful aging [18], which emphasizes the preservation of physical, cognitive, and social functioning along with the maintenance of high quality of life, as rural participants exhibited lower levels across all these domains. This discrepancy helps explain the lower self-rated successful aging observed among participants living in rural areas. Regression analyses further showed that PWI was strongly associated with SSAS, while rural residence and the presence of chronic illness were independently associated with lower SSAS scores. Moderation analyses showed that PWI predicts SSAS regardless of residence or chronic illness, suggesting that wellbeing consistently predicts perceived successful aging across different environmental contexts and in the presence of illness. Although rural residence and the presence of chronic illness are independently associated with lower SSAS and could theoretically attenuate the effects of personal wellbeing, the observed lack of significant moderation highlights the robustness of subjective quality of life as a context-independent determinant of perceived successful aging. Overall, these findings suggest that interventions aimed at enhancing wellbeing could help promote successful aging and warrant further investigation.
4.4. Psychosocial Dimensions: Community Involvement and Regret for Missed Opportunities and Past Actions
Active community involvement is positively associated with both higher quality of life and greater self-rated successful aging, emphasizing its role as a resource that allows older adults to actively influence their wellbeing and aging process despite differing life circumstances. Engagement in social and cultural activities reduces loneliness, depression, and anxiety, thereby enhancing overall functioning [65]. Conversely, regret, whether for missed opportunities or past actions, is linked to lower life satisfaction, poorer health outcomes [66,67], and reduced self-rated successful aging [68]. These findings highlight dual psychosocial pathways related to successful aging. Active community participation supports wellbeing and adaptive aging, whereas life regrets represent a psychological barrier. Interventions that foster engagement and address sources of regret may therefore promote successful aging in later life [69].
4.5. Perspectives for Clinical and Assistive Practice
The findings of this study have direct implications for the organization of integrated, person-centered care for older adults, particularly in rural settings. PWI was found to be strongly associated with SSAS across residence and chronic disease status. This suggests that interventions aimed at enhancing personal wellbeing and social inclusion may yield broad and transferable benefits across contexts and healthcare profiles. From a health management perspective, these findings support the integration of routine personal wellbeing screening into needs assessments for older adults within primary healthcare settings.
In rural areas, where subjective quality of life is generally lower, integrating healthcare, social services, and opportunities for community participation may better meet older adults’ needs. Personal wellbeing and self-rated successful aging can serve as patient-relevant, measurable outcomes for planning, monitoring, and evaluating integrated care models, aligning with outcome-oriented frameworks that prioritize domains most meaningful to older individuals, such as daily functioning and emotional wellbeing [70].
The high prevalence of chronic illness among older adults further underscores the need for coordinated care, as these individuals are more likely to utilize services from multiple providers across health and social care systems. Accordingly, the findings confirm the need for organizational mechanisms that reduce care fragmentation and strengthen collaboration through clinical networks.
The positive association between community involvement and personal wellbeing, alongside the negative impact of regret on quality-of-life domains, indicates that assistive practice should include structured psychosocial components, such as empowerment-oriented interventions, support for coping with losses, life-course evaluations, and the promotion of meaningful community roles. Evaluation of integrated care models would benefit from outcomes aligned with the Quadruple Aim framework, which emphasizes improving patient experience, population health, reducing costs, and supporting healthcare staff wellbeing [71].
4.6. Study Strengths, Limitations, and Recommendations
This study presents several strengths. It includes a sizable sample of older adults from both rural and urban areas, allowing robust comparisons across settings. The use of validated instruments to assess subjective wellbeing and self-rated successful aging enhances the reliability of the findings. Moreover, it provides novel insights into psychosocial and environmental determinants of successful aging within a region characterized by unique socio-cultural and demographic features.
Despite these strengths, several limitations should be acknowledged. The cross-sectional design prevents causal inferences, and the regional focus on Eastern Croatia—Slavonia, with its specific socio-cultural and demographic characteristics, limits generalizability. Reliance on self-report questionnaires may introduce social desirability bias.
In addition, this study employed a non-probability quota sampling strategy combined with snowball sampling, which may limit the representativeness of the sample. Although quota sampling was used to ensure an equal distribution of participants across relevant subgroups, the non-random nature of participant selection and the use of snowball sampling may have introduced selection bias and reduced sample heterogeneity. Furthermore, other potentially influential but unmeasured factors may have further affected sample composition. Although the sample was adequate for detecting main effects, it is recommended to test moderation results with a larger sample to rule out the possibility of small interaction effects, which is important when interpreting non-significant findings. These methodological limitations highlight important considerations for interpretation and highlight the need for further investigation.
Future research should adopt longitudinal designs, include probability-based sampling methods, expand to other regions, integrate quantitative and qualitative methods, and incorporate comparative samples of older adults residing in institutional settings to gain a more comprehensive understanding of successful aging.
5. Conclusions
This study provides evidence of significant urban–rural disparities in subjective quality of life and self-rated successful aging among older adults in Eastern Croatia–Slavonia. Older individuals residing in rural areas consistently reported lower levels of wellbeing across multiple life domains, as well as lower overall perceptions of successful aging. These findings suggest that successful aging is shaped not only by individual health status but also by broader environmental and social conditions associated with place of residence. Subjective quality of life was strongly associated with self-rated successful aging, explaining a substantial proportion of its variance. Despite lower scores observed among rural residents and participants with chronic illness, moderation analyses indicated that the association between wellbeing and successful aging remained consistent across environmental and health contexts. These findings underscore the robustness of personal wellbeing as a context-independent correlate of successful aging. This underscores the robustness of subjective wellbeing as a core component of successful aging in later life. Importantly, psychosocial factors played a meaningful role in shaping both quality of life and successful aging. Active involvement in the community was positively associated with higher wellbeing across all domains, whereas regret related to missed opportunities and past actions was linked to poorer outcomes. These findings highlight the interplay of adaptive and maladaptive psychosocial processes in later life and underscore the association between social participation, psychological resources, and self-perceived successful aging. Taken together, the results point to the need for integrated public health and social policies that go beyond medical care and address social participation, psychological wellbeing, and structural inequalities, particularly in rural settings. Interventions aimed at enhancing community engagement, reducing social isolation, and supporting adaptive coping strategies may contribute substantially to improved quality of life and more successful aging among older adults, particularly in socioeconomically disadvantaged and rural contexts.
Author Contributions
Conceptualization. M.B., Ž.M., Ž.D., D.D. and J.V.; methodology. M.B., Ž.M., I.B., D.D. and N.F.; software. Ž.M. and I.B.; validation. M.B., Ž.M., N.F., Š.M. and M.Č.; formal analysis. Ž.M., I.B., J.V. and R.L.; investigation. M.B., Ž.M., M.K., Š.M. and M.Č.; resources. M.B., Š.M. and M.K.; data curation. R.L., Ž.D., J.V. and M.Č.; writing—original draft preparation. M.B., Ž.M., N.F., Š.M., Ž.D. and M.K.; writing—review and editing. M.B., Ž.M., M.Č., R.L., I.B., D.D. and J.V.; visualization. M.B., M.K. and Ž.D.; supervision. N.F., D.D. and R.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Higher Institution Ethical Committee of Faculty of Dental Medicine and Health Osijek (Class: 602-01/24-12/02; IRB: 2158/97-97-10-24-36, 27 May 2024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study, and participation was voluntary and anonymous, with the option to withdraw at any time.
Data Availability Statement
The original data presented in the study are openly available on 507 FigShare at https://doi.org/10.6084/m9.figshare.30885308.
Acknowledgments
We are grateful to all the older adults who took part in this study for their time, cooperation, and valuable contributions.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PWI | Personal Wellbeing Index |
| SSAS | Self-assessment of Successful Aging Scale |
| IQR | Interquartile range |
| VIFs | Variance inflation factors |
References
- World Health Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 20 November 2025).
- United Nations, Department of Economic and Social Affairs. World Population Ageing 2023: Challenges and Opportunities of Population Ageing in Least Developed Countries. Available online: https://desapublications.un.org/publications/world-population-ageing-2023-challenges-and-opportunities-population-ageing-least (accessed on 20 November 2025).
- Crimmins, E.M.; Zhang, Y.S. Aging Populations, Mortality, and Life Expectancy. Annu. Rev. Sociol. 2019, 45, 69–89. [Google Scholar] [CrossRef]
- Hong, C.; Sun, L.; Liu, G.; Guan, B.; Li, C.; Luo, Y. Response of Global Health Towards the Challenges Presented by Population Aging. China CDC Wkly. 2023, 5, 884–887. [Google Scholar] [CrossRef] [PubMed]
- Batool, S.S.; Tanveer, S.; Chatrath, S.K.; Batool, S.A. Biopsychosocial Determinants of Quality of Life of Older Adults in Pakistan and Canada. Front. Psychiatry 2024, 15, 1364443. [Google Scholar] [CrossRef] [PubMed]
- Jaul, E.; Barron, J. Age-Related Diseases and Clinical and Public Health Implications for the 85 Years Old and Over Population. Front. Public Health 2017, 5, 335. [Google Scholar] [CrossRef]
- Amarya, S.; Singh, K.; Sabharwal, M. Changes During Aging and Their Association With Malnutrition. J. Clin. Gerontol. Geriatr. 2015, 6, 78–84. [Google Scholar] [CrossRef]
- Demir, Y.; Dağ, E.; Özpinar, S. The Effects and Determinants of Leisure Time Activities on Successful Aging and Quality of Life in Older Adults. Int. J. Gerontol. 2024, 18, 249–253. [Google Scholar] [CrossRef]
- Gianfredi, V.; Nucci, D.; Pennisi, F.; Maggi, S.; Veronese, N.; Soysal, P. Aging, longevity, and healthy aging: The public health approach. Aging Clin. Exp. Res. 2025, 37, 125. [Google Scholar] [CrossRef] [PubMed]
- Kalideen, L.; Govender, P.; van Wyk, J.M. Standards and Quality of Care for Older Persons in Long-Term Care Facilities: A Scoping Review. BMC Geriatr. 2022, 22, 226. [Google Scholar] [CrossRef]
- Ateca-Amestoy, V.; Ugidos, A. The Impact of Different Types of Resource Transfers on Individual Wellbeing: An Analysis of Quality of Life Using CASP-12. Soc. Indic. Res. 2011, 110, 973–991. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy and Action Plan on Ageing and Health. Available online: https://iris.who.int/server/api/core/bitstreams/dde7be07-eb76-4642-800c-4258ecd42e59/content (accessed on 20 November 2025).
- World Health Organization. WHOQOL User Manual. Available online: https://iris.who.int/server/api/core/bitstreams/4c5cd94a-599e-450f-9141-4a21a7b74849/content (accessed on 20 November 2025).
- Jeste, D.V.; Depp, C.A.; Vahia, I.V. Successful Cognitive and Emotional Aging. World Psychiatry 2010, 9, 78–84. [Google Scholar] [CrossRef]
- Ward, M.; McGarrigle, C.; Kenny, R. More Than Health: Quality of Life Trajectories Among Older Adults—Findings from The Irish Longitudinal Study of Ageing (TILDA). Qual. Life Res. 2019, 28, 429–439. [Google Scholar] [CrossRef] [PubMed]
- Mendorf, S.; Heimrich, K.G.; Mühlhammer, H.M.; Prell, T.; Schönenberg, A. Age-Related Trajectories of Quality of Life in Community-Dwelling Older Adults: Findings from the Survey of Health, Aging and Retirement in Europe (SHARE). Front. Aging Neurosci. 2025, 17, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Kornadt, A.; Kessler, E.; Wurm, S.; Bowen, C.; Gabrian, M.; Klusmann, V. Views on Ageing: A Lifespan Perspective. Eur. J. Ageing 2020, 17, 387–401. [Google Scholar] [CrossRef] [PubMed]
- Rowe, J.; Kahn, R.L. Successful aging. Gerontologist 1997, 37, 433–440. [Google Scholar] [CrossRef]
- Sánchez-Moreno, E.; Gallardo-Peralta, L.; Rodríguez-Rodríguez, V.; Soto Higuera, A. Successful Aging and Quality of Life: A Cross-Ethnic Comparison in Chile. In Handbook of Active Ageing and Quality of Life, 1st ed.; Rojo-Pérez, F., Fernández-Mayoralas, G., Eds.; Springer International Publishing: Cham, Germany, 2021; pp. 451–465. [Google Scholar] [CrossRef]
- Yustanti, A.S.; Annisa, N.S.; Indarwati, R.; Wahyudi, A.S. Determinants of Successful Aging in Older Adults: A Systematic Review of Psychological, Social, and Physical Factors. Med. Technol. Public Health J. 2024, 8, 28–35. [Google Scholar] [CrossRef]
- Song, K.; Luo, J.; Cao, X.; Zhao, Z. Urban-rural differences in the successful aging among older adults in China. PLoS ONE 2025, 20, e0319105. [Google Scholar] [CrossRef]
- Owusu-Addo, E.; Gilbert, A.S.; Feldman, P.; Garratt, S.M.; Mackell, P.; Brijnath, B. Integrated Care Models for Older People: An Umbrella Review. Ageing Int. 2025, 50, 35. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2025 OECD Indicators. Available online: https://www.oecd.org/en/publications/health-at-a-glance-2025_8f9e3f98-en.html (accessed on 15 January 2026).
- World Health Organization. Integrated Care for Older People (ICOPE): Guidance for Person-Centred Assessment and Pathways in Primary Care, 2nd ed.; WHO Press: Geneva, Switzerland, 2024; pp. 1–41. [Google Scholar]
- Krnjajić, M.; Mudri, Ž.; Barišić, M.; Barać, I.; Vujanić, J.; Čebohin, M.; Lovrić, R.; Major Poljak, K.; Farčić, N. Cognitive Functioning in Rural Older Adults: The Mediating Role of Perceived Social Support. Healthcare 2026, 14, 152. [Google Scholar] [CrossRef]
- Wang, S.; Liu, Y.; Yang, Y. Perceived quality of home- and community-based services and urban-rural disparities in aging-in-place intentions: Evidence from Chinese older adults. BMC Geriatr. 2026; early access. [Google Scholar] [CrossRef]
- Barišić, M.; Mudri, Ž.; Farčić, N.; Čebohin, M.; Degmečić, D.; Barać, I. Subjective Well-Being and Successful Ageing of Older Adults in Eastern Croatia—Slavonia: Exploring Individual and Contextual Predictors. Sustainability 2024, 16, 7808. [Google Scholar] [CrossRef]
- UNHCR. Older Persons. Available online: https://emergency.unhcr.org/protection/persons-risk/older-persons (accessed on 26 November 2025).
- Eurostat. GISCO Degree of Urbanization. Available online: https://ec.europa.eu/eurostat/web/gisco/geodata/population-distribution/degree-urbanisation (accessed on 15 January 2026).
- Sample Size Calculator 2025. Available online: https://www.calculator.net/sample-size-calculator.html (accessed on 26 November 2025).
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- International Wellbeing Group. Pwi Personal Wellbeing Indeks. Available online: https://www.acqol.com.au/uploads/pwi-a/pwi-a-english.pdf#page=16.09 (accessed on 26 November 2025).
- Tucak Junaković, I.; Nekić, M.; Ambrosi-Randić, N. Konstrukcija i validacija skale samoprocjene uspješnog starenja. Suvremena Psihol. 2020, 23, 7–20. [Google Scholar] [CrossRef]
- Tucak Junaković, I.; Nekić, M. Skala samoprocjene uspješnog starenja. In Zbirka Psihologijskih Skala i Upitnika: Svezak 8, 1st ed.; Tucak Junaković, I., Burić, I., Ćubela Adorić, V., Proroković, A., Slišković, A., Eds.; Morepress Books: Zadar, Croatia, 2019; Volume 8, pp. 37–45. [Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, X.; Fu, X.; Li, W.; Wang, Y.; Lu, W. Successful Aging Rates of Global Older Adults: A Systematic Review and Meta-analysis. J. Am. Med. Dir. Assoc. 2025, 26, 105334. [Google Scholar] [CrossRef]
- Jang, H.A.; Choi, J.S. Association Between Swallowing Dysfunction and Multidimensional Quality of Life Among Community-Dwelling Healthy Korean Older Adults: A Pilot Cross-Sectional Study. Healthcare 2025, 13, 2964. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Chen, D.; Li, C.; Wang, Y. Effect of community-based public health service on health-related quality of life among middle-aged and older adults with chronic diseases in China. BMC Public Health 2024, 24, 2039. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Huang, X.; Dou, L.; Yan, M.; Shen, T.; Tang, W.; Li, J. Aging and aging-related diseases: From molecular mechanisms to interventions and treatments. Signal Transduct. Target. Ther. 2022, 7, 391. [Google Scholar] [CrossRef]
- Waddell, C.; Van Doorn, G.; Power, G.; Statham, D. From Successful Ageing to Ageing Well: A Narrative Review. Gerontologist 2024, 65, gnae109. [Google Scholar] [CrossRef]
- Viljanen, A.; Salminen, M.; Irjala, K.; Löppönen, M.; Tuori, H.; Vahlberg, T.; Viitanen, M.; Viikari, L. Predicting successful ageing among older adults seems possible even as far as two decades ahead. BMC Geriatr. 2024, 24, 481. [Google Scholar] [CrossRef]
- Cosco, T.D.; Prina, A.M.; Perales, J.; Stephan, B.C.M.; Brayne, C. Operational definitions of successful aging: A systematic review. Int. Psychogeriatr. 2014, 26, 373–381. [Google Scholar] [CrossRef]
- Vuletić, G.; Stapić, M. Kvaliteta života i doživljaj usamljenosti kod osoba starije životne dobi. Klin. Psihol. 2013, 6, 45–61. [Google Scholar]
- Ahsan, M. Gender-specific differences in quality of life: A comparative review. In Proceedings of the International Scientific Research and Innovation Congress-II, Adana, Türkiye, 16–18 December 2024. [Google Scholar]
- Srivastava, S.; Muhammad, T.; Paul, R.; Khan, K.A. Multivariate decomposition of gender differentials in successful aging among older adults in India. BMC Geriatr. 2023, 23, 59. [Google Scholar] [CrossRef]
- Shi, W.H.; Zhang, H.Y.; Zhang, J.; Lyu, Y.B.; Brasher, M.S.; Yin, Z.X.; Luo, J.S.; Hu, D.S.; Fen, L.; Shi, X.M. The status and Associated Factors of Successful Aging among Older Adults Residing in Longevity Areas in China. Biomed. Environ. Sci. 2016, 29, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Tucak Junaković, I.; Ambrosi-Randić, N.; Macuka, I. Psihosocijalne determinante objektivnih i subjektivnih pokazatelja uspješnoga starenja. Društvena Istraživanja 2023, 32, 449–469. [Google Scholar] [CrossRef]
- Matišić, M.; Pejnović, D. Uzroci i posljedice zaostajanja Istočne Hrvatske u regionalnom razvoju Hrvatske. Hrvat. Georg. Glas. 2015, 77, 101–140. [Google Scholar] [CrossRef]
- Živić, D. Demografsko pražnjenje Istočne Hrvatske. Političke Anal. 2017, 8, 24–32. [Google Scholar]
- Šundalić, A. Osiromašivanje i nerazvijenost–Slavonija i Baranja u očima njezinih stanovnika. Soc. Ekol. Zagreb. 2006, 15, 125–143. [Google Scholar]
- OECD. Multi-level Governance Studies Towards Balanced Regional Development in Croatia—From Strategy Design to Implementation. Available online: https://www.oecd.org/en/publications/towards-balanced-regional-development-in-croatia_3c0779cf-en.html (accessed on 22 November 2025).
- Pekçetin, E.; Pekçetin, S.; Sağlamoğlu, E.; Ekici, G. Urban versus rural older adults: Occupational balance and quality of life comparison. BMC Geriatr. 2025, 25, 49. [Google Scholar] [CrossRef]
- Jiang, H.; Burström, B.; Chen, J.; Burström, K. Rural–Urban Inequalities in Poor Self-Rated Health, Self-Reported Functional Disabilities, and Depression among Chinese Older Adults: Evidence from the China Health and Retirement Longitudinal Study 2011 and 2015. Int. J. Environ. Res. Public Health 2021, 18, 6557. [Google Scholar] [CrossRef] [PubMed]
- Iverson, T.; Schulze, M.; Gill, K.; Switkowski, Y.; dos Santos, I.K.; Ashe, M.C. Older adults and social support in rural Canada: A rapid mixed methods systematic review to inform social prescribing. Arch. Gerontol. Geriatr. 2025, 139, 106022. [Google Scholar] [CrossRef]
- Cohen, S.A.; Greaney, M.L. Aging in Rural Communities. Curr. Epidemiol. Rep. 2023, 10, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Golovchanova, N.; Evans, B.; Hellfeldt, K.; Andershed, H.; Boersma, K. Older and feeling unsafe? Differences in underlying vulnerability, anxiety and life satisfaction among older adults. Aging Ment. Health 2023, 27, 1636–1643. [Google Scholar] [CrossRef]
- Baernholdt, M.; Yan, G.; Hinton, I.; Rose, K.; Mattos, M. Quality of life in rural and urban adults 65 years and older: Findings from the National Health and Nutrition Examination survey. J. Rural Health 2012, 28, 339–347. [Google Scholar] [CrossRef]
- Boah, M.; Cyuzuzo, C.; Uwinkindi, F.; Kalinda, C.; Yohannes, T.; Isano, S.; Greig, C.; Davies, J.; Hirschhorn, L.R.; Amberbir, A. Health and well-being of older adults in rural and urban Rwanda: Epidemiological findings from a population based cross-sectional study. J. Glob. Health 2025, 15, 04108. [Google Scholar] [CrossRef] [PubMed]
- Dannefer, D. Cumulative Advantage/Disadvantage and the Life Course: Cross-Fertilizing Age and Social Science Theory. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003, 58, S327–S337. [Google Scholar] [CrossRef] [PubMed]
- Fuller, H.R.; Huseth-Zosel, A. Older Adults’ Loneliness in Early COVID-19 Social Distancing: Implications of Rurality. J. Gerontol. B Psychol. Sci. Soc. Sci. 2022, 77, e100–e105. [Google Scholar] [CrossRef]
- Kitreerawutiwong, N.; Keeratisiroj, O.; Mekrungrongwong, S. Predictive Factors for the Sense of Community Belonging Among Older Adults in Lower Northern Thailand. Iran. J. Psychiatry Behav. Sci. 2020, 14, e105564. [Google Scholar] [CrossRef]
- Neville, S.; Adams, J.; Napier, S.; Shannon, K.; Jackson, D. Engaging in my rural community: Perceptions of people aged 85 years and over. Int. J. Qual. Stud. Health Well-Being 2018, 13, 1503908. [Google Scholar] [CrossRef]
- Yu, J.; Liu, Y. Barriers to Transportation in Rural Communities: Perspective of Older Adult Users. J. Gerontol. B Psychol. Sci. Soc. Sci. 2024, 79, gbad135. [Google Scholar] [CrossRef]
- Mseke, E.P.; Jessup, B.; Barnett, T. Impact of distance and/or travel time on healthcare service access in rural and remote areas: A scoping review. J. Transp. Health 2024, 37, 101819. [Google Scholar] [CrossRef]
- Liang, L.Y. The impact of social participation on the quality of life among older adults in China: A chain mediation analysis of loneliness, depression, and anxiety. Front. Public Health 2024, 12, 1473657. [Google Scholar] [CrossRef] [PubMed]
- Rutledge, J.A.; Williams, J.D.; Barlow, M.A. The relationship between life regrets and well-being: A systematic review. Front. Psychol. 2024, 15, 1515373. [Google Scholar] [CrossRef] [PubMed]
- Newall, N.E.; Chipperfield, J.G.; Daniels, L.M.; Hladkyj, S.; Perry, R.P. Regret in later life: Exploring relationships between regret frequency, secondary interpretive control beliefs, and health in older individuals. Int. J. Aging Hum. Dev. 2009, 68, 261–288. [Google Scholar] [CrossRef]
- Tucak Junaković, I.; Ambrosi-Randić, N.; Nekić, M. Odnos otvorenosti prema iskustvu i uspješnog starenja: Provjera posredujuće uloge životnih žaljenja. Psihol. Teme 2018, 27, 499–518. [Google Scholar] [CrossRef]
- Monteiro, J.M.; Gonçalves, R.; Bastos, A.; Barbosa, M.R. Social engagement and wellbeing in late life: A systematic review. Ageing Soc. 2025, 45, 1327–1354. [Google Scholar] [CrossRef]
- Andersson, Å.G.; Dahlkvist, L.; Kurland, L. Patient-centered outcomes and outcome measurements for people aged 65 years and older—A scoping review. BMC Geriatr. 2024, 24, 528. [Google Scholar] [CrossRef]
- D’Alleva, A.; Leigheb, F.; Rinaldi, C.; Di Stanislao, F.; Vanhaecht, K.; De Ridder, D.; Bruyneel, L.; Cangelosi, G.; Panella, M. Achieving quadruple aim goals through clinical networks: A systematic review. J. Healthc. Qual. Res. 2019, 34, 29–39. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.