Relationship Between the Sagittal and Coronary Alignment of the Tibiofemoral Joint and the Medial Meniscus Extrusion in Knee Osteoarthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study 1
2.1.1. Subjects
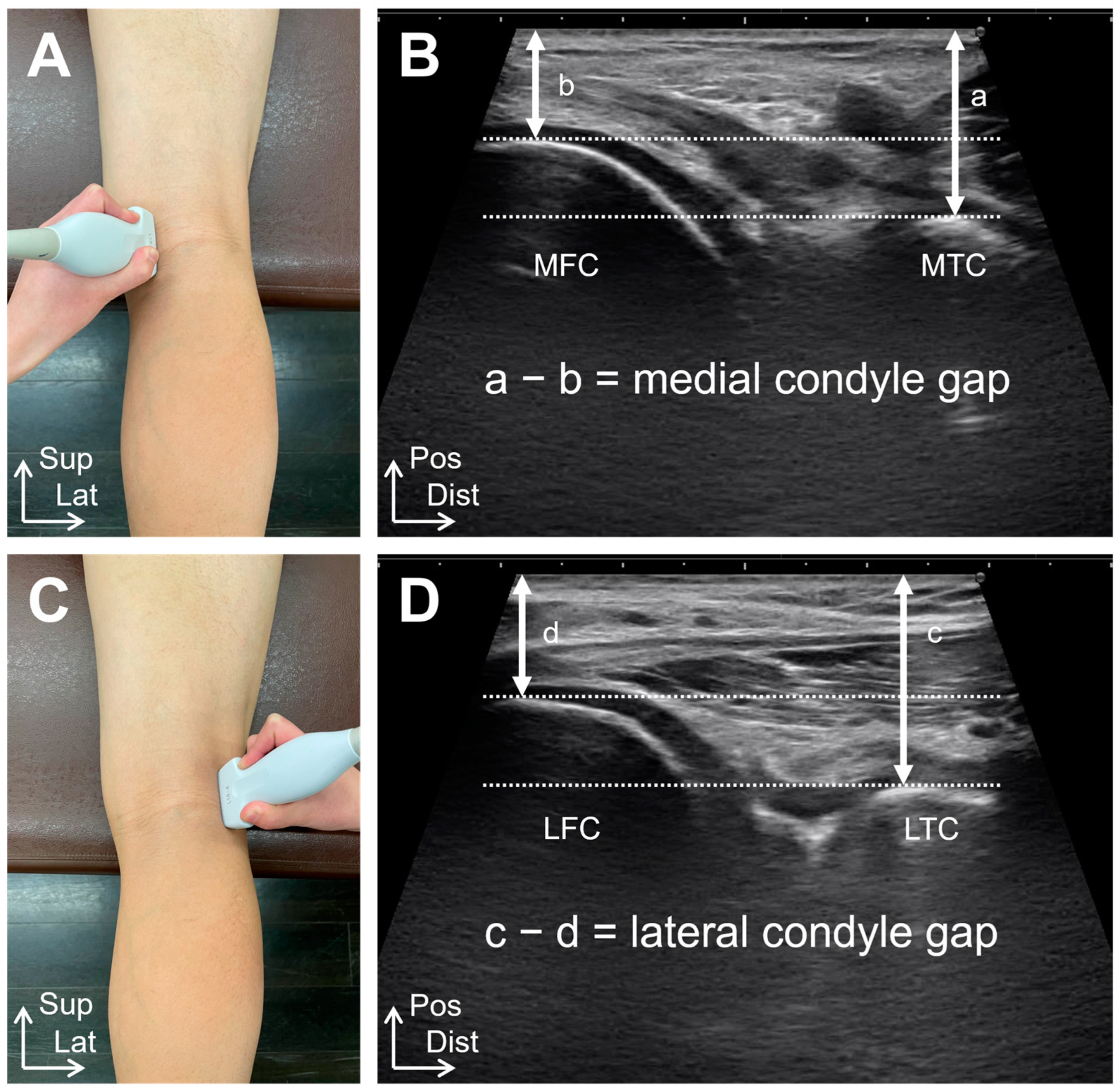
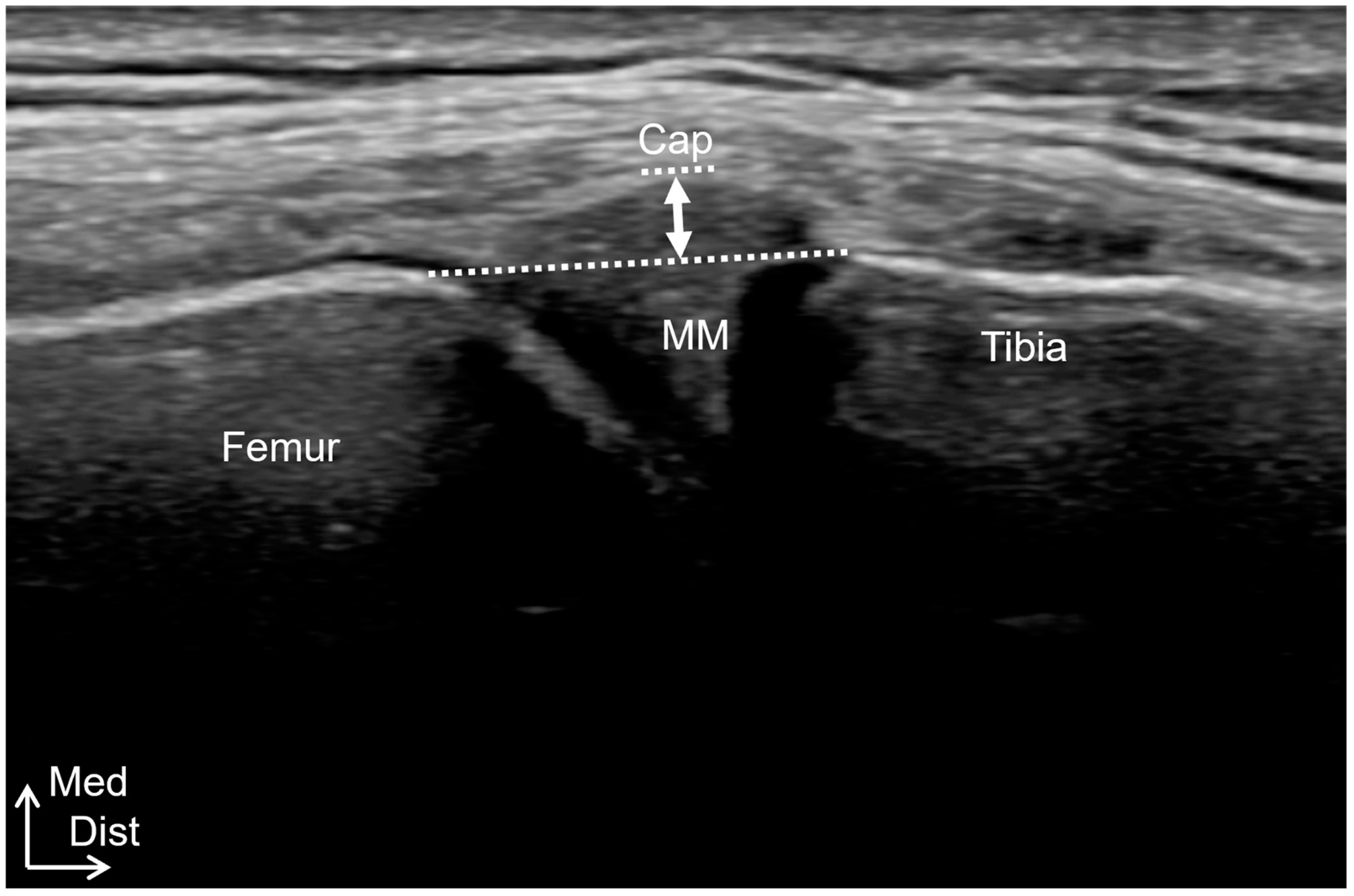
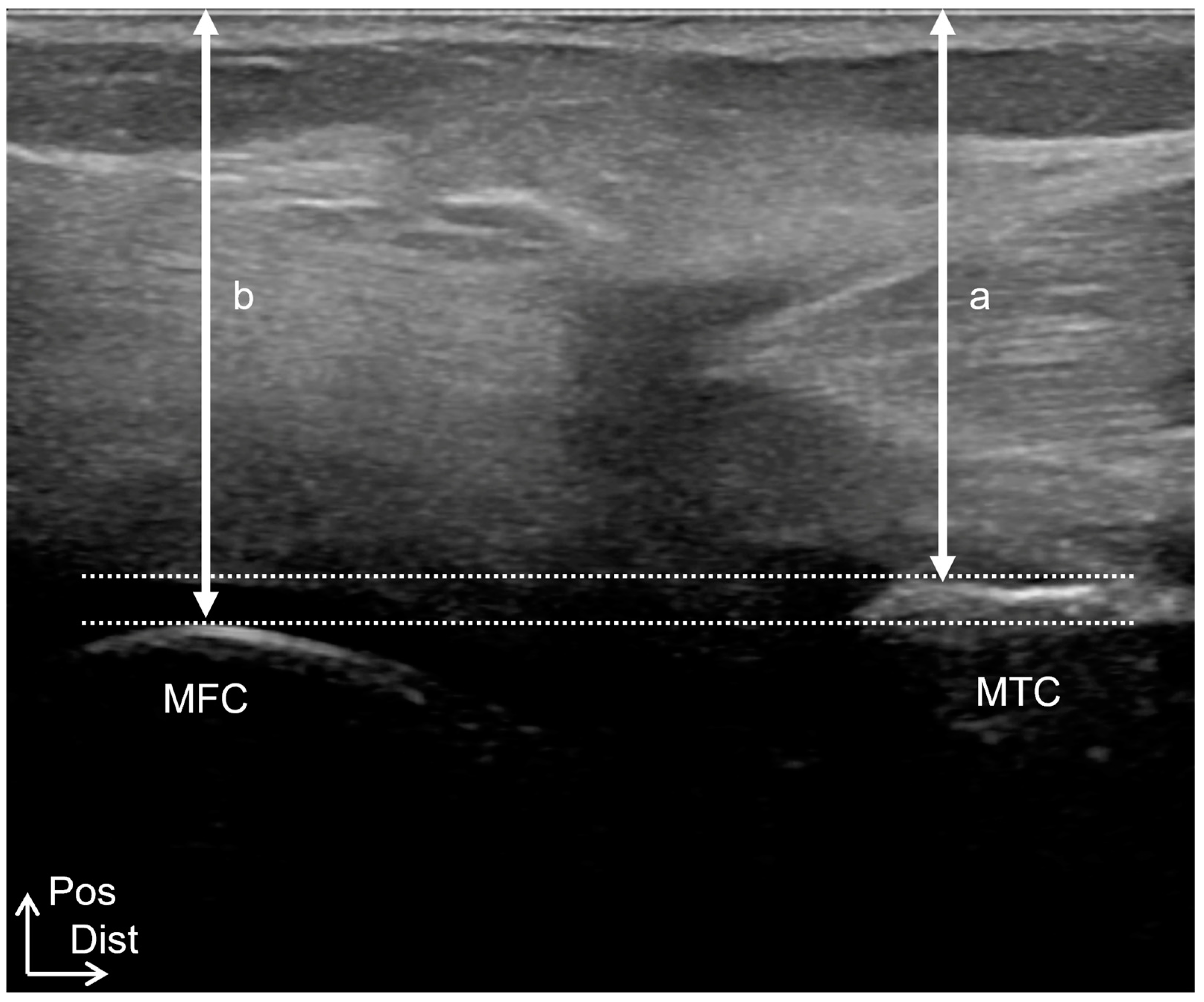
2.1.2. Ultrasound Imaging Examinations
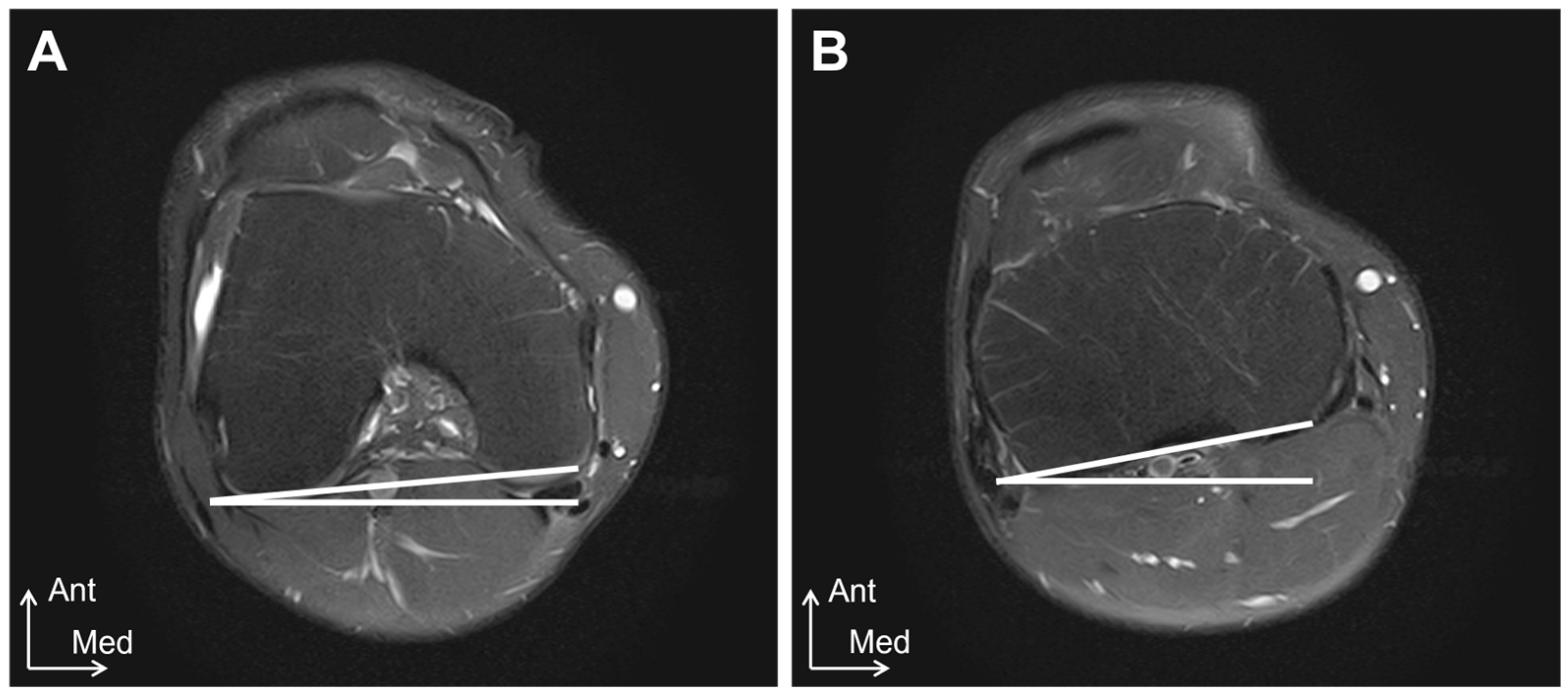
2.1.3. MRI Examinations
2.1.4. Q-Angle Examinations
2.1.5. Intra-Rater Reliability and Inter-Rater Reliability
2.1.6. Statistical Analysis
2.2. Study 2
2.2.1. Subjects
2.2.2. Procedures
2.2.3. Statistical Analysis
3. Results
3.1. Study 1
3.2. Study 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ghouri, A.; Muzumdar, S.; Barr, A.J.; Robinson, E.; Murdoch, C.; Kingsbury, S.R.; Conaghan, P.G. The relationship between meniscal pathologies, cartilage loss, joint replacement and pain in knee osteoarthritis: A systematic review. Osteoarthr. Cartil. 2022, 30, 1287–1327. [Google Scholar] [CrossRef]
- Faucett, S.C.; Geisler, B.P.; Chahla, J.; Krych, A.J.; Kurzweil, P.R.; Garner, A.M.; Liu, S.; LaPrade, R.F.; Pietzsch, J.B. Meniscus Root Repair vs Meniscectomy or Nonoperative Management to Prevent Knee Osteoarthritis After Medial Meniscus Root Tears: Clinical and Economic Effectiveness. Am. J. Sports Med. 2019, 47, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Makiev, K.G.; Vasios, I.S.; Georgoulas, P.; Tilkeridis, K.; Drosos, G.; Ververidis, A. Clinical significance and management of meniscal extrusion in different knee pathologies: A comprehensive review of the literature and treatment algorithm. Knee Surg. Relat. Res. 2022, 34, 35. [Google Scholar] [CrossRef] [PubMed]
- Ozeki, N.; Koga, H.; Sekiya, I. Degenerative Meniscus in Knee Osteoarthritis: From Pathology to Treatment. Life 2022, 12, 603. [Google Scholar] [CrossRef] [PubMed]
- Hada, S.; Ishijima, M.; Kaneko, H.; Kinoshita, M.; Liu, L.; Sadatsuki, R.; Futami, I.; Yusup, A.; Takamura, T.; Arita, H.; et al. Association of medial meniscal extrusion with medial tibial osteophyte distance detected by T2 mapping MRI in patients with early-stage knee osteoarthritis. Arthritis Res. Ther. 2017, 19, 201. [Google Scholar] [CrossRef] [PubMed]
- Ishii, Y.; Ishikawa, M.; Nakashima, Y.; Takahashi, M.; Iwamoto, Y.; Hashizume, T.; Okamoto, S.; Sunagawa, T.; Okada, K.; Takagi, K.; et al. Knee adduction moment is correlated with the increase in medial meniscus extrusion by dynamic ultrasound in knee osteoarthritis. Knee 2022, 38, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Goto, N.; Okazaki, K.; Akiyama, T.; Akasaki, Y.; Mizu-Uchi, H.; Hamai, S.; Nakamura, S.; Nakashima, Y. Alignment factors affecting the medial meniscus extrusion increases the risk of osteoarthritis development. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2019, 27, 2617–2623. [Google Scholar] [CrossRef]
- Bornes, T.D.; Kubik, J.F.; Klinger, C.E.; Altintas, B.; Dziadosz, D.; Ricci, W.M. Relative Sagittal Alignment of the Medial and Lateral Articular Surfaces of the Tibial Plateau Using Radiographic Parameters: A Radiographic Cadaveric Study. J. Orthop. Trauma 2022, 36, e405–e411. [Google Scholar] [CrossRef]
- Williams, B.A.; Oduwole, S.; Mehta, N.N.; Talwar, D.; Nguyen, J.C.; Wells, L. Reliability and Validity of an MRI-Based Knee Sagittal Alignment Measure in a Pediatric Cohort. J. Pediatr. Orthop. 2022, 42, e349–e355. [Google Scholar] [CrossRef]
- Nguyen, A.D.; Boling, M.C.; Levine, B.; Shultz, S.J. Relationships between lower extremity alignment and the quadriceps angle. Clin. J. Sport Med. 2009, 19, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.O.; Hunt, N.J.; Donell, S.T. The reliability and validity of the Q-angle: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2008, 16, 1068–1079. [Google Scholar] [CrossRef]
- Cavaignac, E.; Sylvie, R.; Teulières, M.; Fernandez, A.; Frosch, K.H.; Gomez-Brouchet, A.; Sonnery-Cottet, B. What Is the Relationship Between the Distal Semimembranosus Tendon and the Medial Meniscus? A Gross and Microscopic Analysis from the SANTI Study Group. Am. J. Sports Med. 2021, 49, 459–466. [Google Scholar] [CrossRef]
- Vassalou, E.E.; Klontzas, M.E.; Kouvidis, G.K.; Matalliotaki, P.I.; Karantanas, A.H. Rotational Knee Laxity in Anterior Cruciate Ligament Deficiency: An Additional Secondary Sign on MRI. AJR Am. J. Roentgenol. 2016, 206, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Chang, P.H.; Chen, Y.J.; Chang, K.V.; Wu, W.T.; Özçakar, L. Ultrasound measurements of superficial and deep masticatory muscles in various postures: Reliability and influencers. Sci. Rep. 2020, 10, 14357. [Google Scholar] [CrossRef] [PubMed]
- Luyten, F.P.; Bierma-Zeinstra, S.; Dell’Accio, F.; Kraus, V.B.; Nakata, K.; Sekiya, I.; Arden, N.K.; Lohmander, L.S. Toward classification criteria for early osteoarthritis of the knee. Semin. Arthritis Rheum. 2018, 47, 457–463. [Google Scholar] [CrossRef]
- Wang, Y.X.; Li, Z.L.; Li, J.; Zhao, Z.D.; Wang, H.R.; Hou, C.; Li, W.; Liu, C.H. Effect of medial meniscus extrusion on arthroscopic surgery outcome in the osteoarthritic knee associated with medial meniscus tear: A minimum 4-year follow-up. Chin. Med. J. 2019, 132, 2550–2558. [Google Scholar] [CrossRef]
- Naredo, E.; Cabero, F.; Palop, M.J.; Collado, P.; Cruz, A.; Crespo, M. Ultrasonographic findings in knee osteoarthritis: A comparative study with clinical and radiographic assessment. Osteoarthr. Cartil. 2005, 13, 568–574. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, S.; Ishii, Y.; Kono, Y.; Hashizume, T.; Okinaka, R.; Nakashima, Y.; Kamei, G.; Nekomoto, A.; Takahashi, M.; Adachi, N. Medial meniscus extrusion during gait is associated with decrease in knee rotation in early-stage knee osteoarthritis. Gait Posture 2024, 110, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Ikuta, F.; Yoneta, K.; Miyaji, T.; Kidera, K.; Yonekura, A.; Osaki, M.; Gamada, K. Association between stages of medial compartment osteoarthritis and three-dimensional knee alignment in the supine position: A cross-sectional study. J. Clin. Orthop. Trauma 2020, 11, S130–S136. [Google Scholar] [CrossRef] [PubMed]
- Nagao, N.; Tachibana, T.; Mizuno, K. The rotational angle in osteoarthritic knees. Int. Orthop. 1998, 22, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Matsui, Y.; Kadoya, Y.; Uehara, K.; Kobayashi, A.; Takaoka, K. Rotational deformity in varus osteoarthritis of the knee: Analysis with computed tomography. Clin. Orthop. Relat. Res. 2005, 433, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Yagi, T. Tibial torsion in patients with medial-type osteoarthrotic knees. Clin. Orthop. Relat. Res. 1994, 302, 52–56. [Google Scholar] [CrossRef]
- Ikuta, F.; Yoneta, K.; Miyaji, T.; Kidera, K.; Yonekura, A.; Osaki, M.; Gamada, K. Knee kinematics of severe medial knee osteoarthritis showed tibial posterior translation and external rotation: A cross-sectional study. Aging Clin. Exp. Res. 2019, 32, 1767–1775. [Google Scholar] [CrossRef] [PubMed]
- Messner, K.; Gao, J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J. Anat. 1998, 193 Pt 2, 161–178. [Google Scholar] [CrossRef] [PubMed]
- Thompson, W.O.; Thaete, F.L.; Fu, F.H.; Dye, S.F. Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am. J. Sports Med. 1991, 19, 210–215, discussion 215–216. [Google Scholar] [CrossRef]
- Okazaki, Y.; Furumatsu, T.; Yamaguchi, T.; Kodama, Y.; Kamatsuki, Y.; Masuda, S.; Okazaki, Y.; Hiranaka, T.; Zhang, X.; Ozaki, T. Medial meniscus posterior root tear causes swelling of the medial meniscus and expansion of the extruded meniscus: A comparative analysis between 2D and 3D MRI. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2020, 28, 3405–3415. [Google Scholar] [CrossRef]
- Kitagawa, T.; Kawahata, H.; Aoki, M.; Kudo, S. Inhibitory effect of low-intensity pulsed ultrasound on the fibrosis of the infrapatellar fat pad through the regulation of HIF-1α in a carrageenan-induced knee osteoarthritis rat model. Biomed. Rep. 2022, 17, 79. [Google Scholar] [CrossRef]
- Yoshizuka, H.; Taniguchi, T.; Fukuta, K.; Mitsutake, T.; Honda, S. Decrease in medial meniscal extrusion after physical therapy to improve knee pain and range of motion in patients with knee osteoarthritis: A retrospective study. PLoS ONE 2022, 17, e0277628. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, M.; Nimura, A.; Tharnmanularp, S.; Kudo, S.; Akita, K. Posteromedial capsular anatomy of the tibia for consideration of the medial meniscal support structure using a multidimensional analysis. Sci. Rep. 2023, 13, 12030. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, M.; Kanazawa, S.; Nimura, A.; Akita, K.; Kudo, S. In vivo movement interrelationships among the medial meniscus, joint capsule, and semimembranosus during tibial rotation. Sci. Rep. 2024, 14, 17022. [Google Scholar] [CrossRef] [PubMed]

| Intra-Rater Reliability | ICC (1, 3) | 95%CI | SEM | MDC95% |
|---|---|---|---|---|
| Distance from the medial condyle of the femur to the skin | 0.973 | 0.901–0.993 | 0.565 | 1.566 |
| Distance from the medial condyle of the tibia to the skin | 0.979 | 0.922–0.995 | 0.598 | 1.658 |
| Distance from the lateral condyle of the femur to the skin | 0.881 | 0.615–0.969 | 1.026 | 2.844 |
| Distance from the lateral condyle of the tibia to the skin | 0.927 | 0.750–0.981 | 1.469 | 4.073 |
| Inter-Rater Reliability | ICC (2, 3) | 95%CI | SEM | MDC95% |
| Distance from the medial condyle of the femur to the skin | 0.895 | 0.652–0.972 | 1.001 | 2.775 |
| Distance from the medial condyle of the tibia to the skin | 0.951 | 0.764–0.988 | 0.912 | 2.529 |
| Distance from the lateral condyle of the femur to the skin | 0.786 | 0.381–0.941 | 1.546 | 4.284 |
| Distance from the lateral condyle of the tibia to the skin | 0.859 | 0.369–0.966 | 2.052 | 5.687 |
| Coefficient | β | SE | t Value | p-Value | |
|---|---|---|---|---|---|
| Constant | 1.732 | 0.962 | 1.790 | 0.09 | |
| ML gap | 1.095 | 0.940 | 0.171 | 6.305 | <0.01 |
| Q angle | −0.049 | −0.115 | 0.063 | −0.774 | 0.45 |
| Control (31 Knees) | Early OA (44 Knees) | Moderate OA (19 Knees) | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |
| Age (years) † | 70.32 ± 6.49 | 64.64 ± 10.60 | 70.16 ± 8.77 |
| Height (cm) † | 163.06 ± 5.67 | 157.84 ± 6.55 | 158.53 ± 6.18 |
| Weight (kg) | 57.42 ± 8.82 | 60.52 ± 9.58 | 62.16 ± 12.29 |
| Knee extension angle (°) †§* | −0.48 ± 1.50 | −3.64 ± 3.12 | −8.16 ± 3.42 |
| Joint effusion (mm) †§* | 0.05 ± 0.13 | 1.37 ± 1.40 | 2.86 ± 1.90 |
| Medial meniscus extrusion (mm) † | 2.54 ± 0.69 | 3.05 ± 0.80 | 3.04 ± 0.98 |
| Medial Condyle gap (mm) | 5.46 ± 1.67 | 6.03 ± 3.22 | 5.15 ± 4.30 |
| Lateral Condyle gap (mm) § | 6.23 ± 1.59 | 6.80 ± 3.30 | 4.78 ± 2.90 |
| Tibial external-rotation angle (°) | 0.89 ± 2.49 | 2.18 ± 4.07 | 1.33 ± 5.44 |
| Normal Rotation (34 Knees) | Excessive Internal Rotation (16 Knees) | Excessive External Rotation (13 Knees) | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |
| Age (years) | 64.29 ± 11.52 | 69.69 ± 8.23 | 67.38 ± 8.61 |
| Height (cm) | 157.47 ± 5.05 | 158.13 ± 8.04 | 159.46 ± 7.58 |
| Weight (kg) | 59.03 ± 7.61 | 63.13 ± 13.05 | 63.62 ± 12.71 |
| Knee extension angle (°) † | −3.82 ± 3.03 | −6.56 ± 4.73 | −6.15 ± 3.63 |
| Joint effusion (mm) † | 1.38 ± 1.18 | 2.74 ± 2.18 | 1.84 ± 1.87 |
| Medial meniscus extrusion (mm) | 2.95 ± 0.85 | 3.06 ± 0.94 | 3.27 ± 0.74 |
| Medial condyle gap (mm) †§* | 5.86 ± 2.36 | 8.20 ± 3.20 | 2.51 ± 4.25 |
| Lateral condyle gap (mm) †§ | 6.17 ± 2.55 | 4.41 ± 3.89 | 8.43 ± 3.11 |
| Tibial external-rotation angle (°) †§* | 2.03 ± 1.32 | −3.42 ± 2.24 | 8.21 ± 3.55 |
| Absence of Posterior Shift (39 Knees) | Presence of Posterior Shift (24 Knees) | p-Value | Effect Size | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Age (years) | 65.38 ± 10.43 | 66.87 ± 10.09 | 0.58 | 0.14 |
| Height (cm) | 158.29 ± 6.32 | 159.90 ± 6.36 | 0.81 | 0.06 |
| Weight (kg) | 64.04 ± 11.43 | 59.15 ± 9.07 | 0.07 | 0.99 |
| Knee extension angle (°) | 3.82 ± 2.77 | −6.38 ± 4.41 | <0.01 | 0.22 |
| Joint effusion (mm) | 1.31 ± 1.42 | 2.42 ± 1.82 | <0.01 | 0.59 |
| Medial meniscus extrusion (mm) | 2.85 ± 0.73 | 3.28 ± 0.92 | 0.04 | 0.58 |
| Medial Condyle gap (mm) | 7.51 ± 2.37 | 3.71 ± 3.67 | <0.01 | 0.76 |
| Lateral Condyle gap (mm) | 8.10 ± 2.69 | 3.94 ± 2.42 | <0.01 | 1.05 |
| Tibial external-rotation angle (°) | 1.98 ± 3.42 | 1.83 ± 5.94 | 0.93 | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ikezu, M.; Kudo, S.; Mitsumori, R.; Iseki, W.; Shibukawa, M.; Iizuka, Y.; Tsutsumi, M.; Hayashi, H. Relationship Between the Sagittal and Coronary Alignment of the Tibiofemoral Joint and the Medial Meniscus Extrusion in Knee Osteoarthritis. Healthcare 2024, 12, 2412. https://doi.org/10.3390/healthcare12232412
Ikezu M, Kudo S, Mitsumori R, Iseki W, Shibukawa M, Iizuka Y, Tsutsumi M, Hayashi H. Relationship Between the Sagittal and Coronary Alignment of the Tibiofemoral Joint and the Medial Meniscus Extrusion in Knee Osteoarthritis. Healthcare. 2024; 12(23):2412. https://doi.org/10.3390/healthcare12232412
Chicago/Turabian StyleIkezu, Masahiro, Shintarou Kudo, Ryuzi Mitsumori, Wataru Iseki, Masato Shibukawa, Yasuhiko Iizuka, Masahiro Tsutsumi, and Hidetoshi Hayashi. 2024. "Relationship Between the Sagittal and Coronary Alignment of the Tibiofemoral Joint and the Medial Meniscus Extrusion in Knee Osteoarthritis" Healthcare 12, no. 23: 2412. https://doi.org/10.3390/healthcare12232412
APA StyleIkezu, M., Kudo, S., Mitsumori, R., Iseki, W., Shibukawa, M., Iizuka, Y., Tsutsumi, M., & Hayashi, H. (2024). Relationship Between the Sagittal and Coronary Alignment of the Tibiofemoral Joint and the Medial Meniscus Extrusion in Knee Osteoarthritis. Healthcare, 12(23), 2412. https://doi.org/10.3390/healthcare12232412






