Concept Analysis of Nursing Surveillance Using a Hybrid Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Theoretical Phase
2.2. Fieldwork Phase
2.3. Final Analysis Phase
3. Results
3.1. Theoretical Phase
3.1.1. The Definition of Surveillance
3.1.2. Definitions of Surveillance in Other Disciplines
3.1.3. The Concept of Surveillance in Nursing
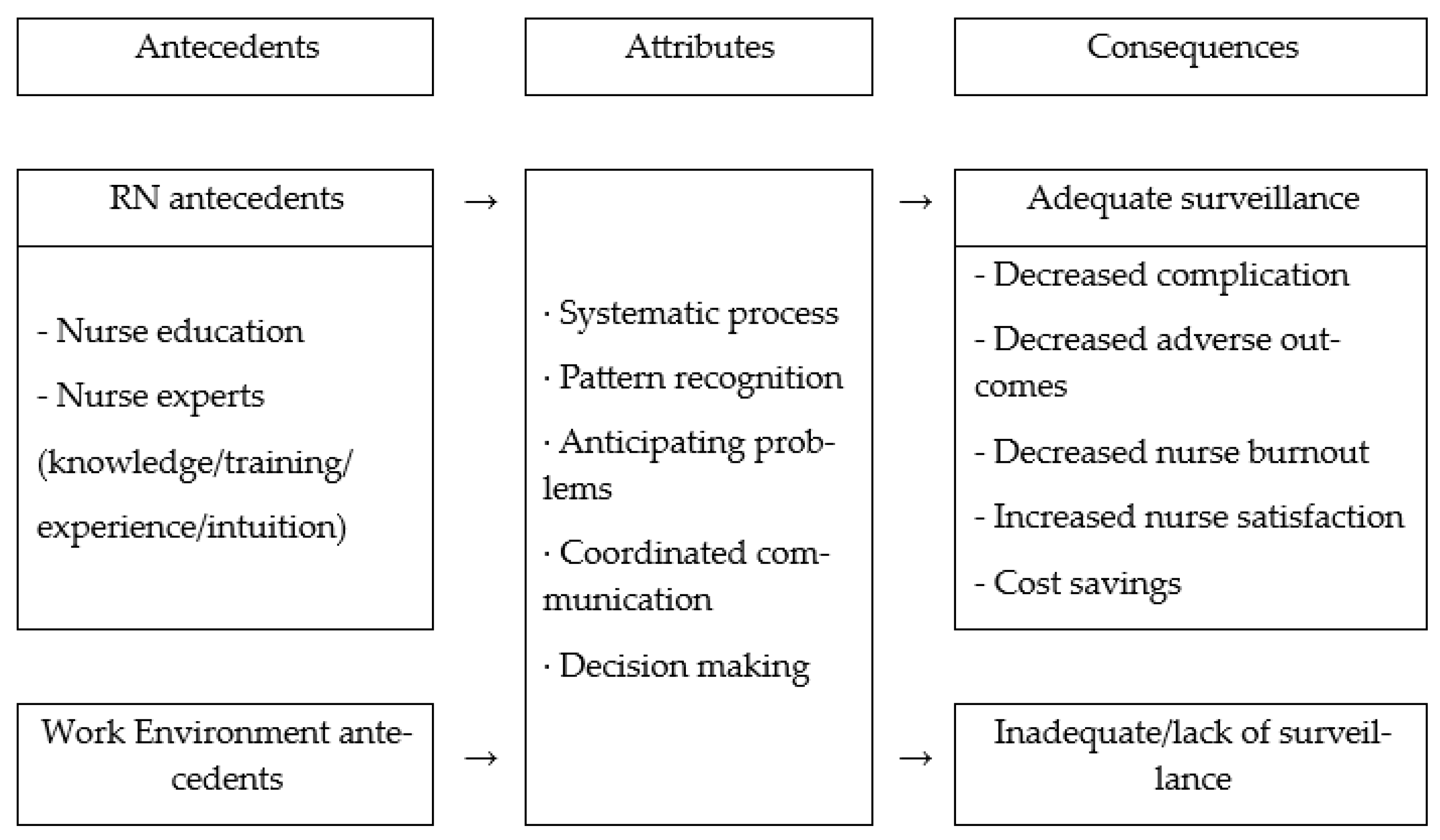
3.1.4. Attributes, Antecedents, and Consequences of Nursing Surveillance
3.2. Fieldwork Phase
Attributes of Nursing Surveillance
“In any case, I receive a general report on the patient, but when I look at them, it is like this. I mean, if a patient is in critical condition, they have a monitor anyway. Then I look at figures like EKG or SPO2 readings on the monitor. I understand that those monitors aren’t always accurate. So, I look at the patient with my own eyes and confirm the patient’s condition. First of all, if the patient’s mental status is not alert, I check their mental status first, and then if their vital signs are somewhat unstable I bring that. If they have a fever, I measure their temperature or take their blood pressure and monitor them if their blood pressure is somewhat unstable. Then intubation, any tubes I have… I check for any incidents or events that the patients may have had. I check the L-tube or Foley catheter and see if it’s in a good immobilization position and then I ask their guardians if there were any events or incidents when the patient was not being monitored and if there is any discomfort. That is how I do it.”(RN 3)
“Usually the blood pressure was 120–130 and dropped to 100, and the heart rate wasn’t that much higher than the vital signs before, but the blood pressure just dropped slightly. When I asked the patient if they were feeling dizzy, they said they were slightly dizzy at that point. And they said they felt nauseous, so I thought it was bleeding. That was what I was thinking.”(RN 1)
“A patient underwent percutaneous coronary intervention and all of a sudden they complained of chest tightness. I measured vital signs… I noticed signs of an impending arrest. There were signs of it… So, I called for an electrocardiogram… and asked for immediate assistance… I had a feeling that something serious was going to happen. So, I prepared for intubation and put the patient on oxygen. I informed the attending physician that they needed to come quickly…”(RN 2)
“A patient had an endoscopy and although they didn’t have any pain, they felt nauseous. As soon as I received a general report, I immediately went to the patient, checked their vital signs, and assessed their symptoms and whether they felt dizzy… Then, I notified the attending physician that they might need to take a look at the X-ray…”(RN 1)
“The patient had a BST of 65 and a BP of around 190… So, the BP was high, I notified the attending physician… When I asked their guardian if this had happened before… the attending physician came and explained the situation… suggested that we consult with the NP and see if there is anything we can do…”(RN 2)
“Doctors are… If there is anything abnormal with the prescription… we find it and report it… A lot of times, doctors don’t even check the results…when I report the results, they’ll order a blood transfusion or something like that… Caregivers or patients talk to the nurse first if they are experiencing discomfort. When the doctor comes rounding to see patients, they don’t say anything, and then if something comes up, they talk to the nurse first…”(RN 6)
“First of all, I look at the patient’s initial assessment history…if there’s a record of them being admitted to our hospital, I go through it all, so I do a search, I look at it all… If there’s something that needs to be done, I can notify the attending physician in advance or check it before the patient is admitted, for example, I check whether the levels of CBC, hemoglobin, or creatine level are low or not… The request is made to follow up with the patient again and then ask the patient’s thoughts on it. If necessary, medication will be prescribed.”(RN 7)
“I try to do what I can first, for example, if a patient’s saturation drops or they have difficulty breathing, I tell them to take deep breaths and check if the sedative is properly administered. I also check the mucus and make sure the monitoring is done properly. If the patient continues to experience problems, I take measures, such as performing lab tests or changing the ventilator or medication. I am doing it in that order.”(RN 4)
“If a diabetic patient’s guardian says they are unconscious, I first check if they have eaten anything if they have taken insulin before a meal, and if they haven’t, I quickly check their BST and give them 50% glucose.”(RN 3)
3.3. Final Analysis Phase
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Institute of Medicine. Keeping Patients Safe: Transforming the Work Environment of Nurses; The National Academies Press: Washington, DC, USA, 2004. [Google Scholar]
- Bulechek, G.M.; Butcher, H.K.; Dochterman, J.M. Nursing Interventions Classification (NIC), 5th ed.; Mosby: Maryland Heights, MO, USA, 2008. [Google Scholar]
- Kelly, L.; Vincent, D. The Dimensions of Nursing Surveillance: A Concept Analysis. J. Adv. Nurs. 2011, 67, 652–661. [Google Scholar] [CrossRef] [PubMed]
- Halverson, C.C.; Scott Tilley, D. Nursing Surveillance: A Concept Analysis. Nurs. Forum. 2022, 57, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Dresser, S. The Role of Nursing Surveillance in Keeping Patients Safe. J. Nurs. Adm. 2012, 42, 361–368. [Google Scholar] [CrossRef]
- Stotts, J.R.; Lyndon, A.; Chan, G.K.; Bekmezian, A.; Rehm, R.S. Nursing Surveillance for Deterioration in Pediatric Patients: An Integrative Review. J. Pediatr. Nurs. 2020, 50, 59–74. [Google Scholar] [CrossRef] [PubMed]
- Karsh, B.T.; Holden, R.J.; Alper, S.J.; Or, C.K. A Human Factors Engineering Paradigm for Patient Safety: Designing to Support the Performance of the Healthcare Professional. Qual. Saf. Health Care. 2006, 15 (Suppl. S1), i59–i65. [Google Scholar] [CrossRef]
- Leal, J.A.L.; Melo, C.M.M.D. The Nurses’ Work Process in Different Countries: An Integrative Review. Rev. Bras. Enferm. 2018, 71, 413–423. [Google Scholar] [CrossRef]
- Dougherty, D.M. Surveillance. In Nursing Intervention: Effective Nursing Treatments, 3rd ed.; Bulechek, G.M., McCloskey, J.C., Eds.; Saunders: Collingwood, AB, Canada, 1999; pp. 524–532. [Google Scholar]
- Kelly, L.A. Nursing Surveillance in the Acute Care Setting: Latent Variable Development and Analysis. Unpublished. Ph.D. Thesis, The University of Arizona, Tucson, AZ, USA, 2009. [Google Scholar]
- Yi, M.; Lee, S.W.; Kim, K.J.; Kim, M.G.; Kim, J.H.; Lee, K.H.; Hong, J.H. A Review Study on the Strategies for Concept Analysis. Taehan Kanho Hakhoe Chi 2006, 36, 493–502. [Google Scholar] [CrossRef]
- Schwartz-Barcott, D.; Kim, H.S. An Expansion and Elaboration of the Hybrid Model of Concept Development. In Concept Development in Nursing: Foundations, Techniques, and Applications, 2nd ed.; Rodgers, B.L., Knafl, K.A., Eds.; Saunders: Collingwood, AB, Canada, 2000; pp. 129–159. [Google Scholar]
- National Institute of Korean Language. Standard Korean Language Dictionary. Available online: https://stdict.korean.go.kr/search/searchResult.do (accessed on 7 February 2023).
- Wilson, D. Military Surveillance. In Routledge Handbook of Surveillance Studies; Routledge: New York, NY, USA, 2012; pp. 269–276. [Google Scholar]
- Center for Disease Control and Prevention. History and Modernization of Case Surveillance. Available online: https://www.cdc.gov/nndss/about/history.html (accessed on 22 February 2023).
- Rodgers, B.L. Concept Analysis: An Evolutionary View. In Concept Development in Nursing: Foundations, Techniques and Applications, 2nd ed.; Rodgers, B.L., Knafl, K.A., Eds.; Saunders: Collingwood, AB, Canada, 2000; pp. 77–117. [Google Scholar]
- Walker, L.O.; Avant, K.C. Strategies for Theory Construction in Nursing; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2005; Volume 4. [Google Scholar]
- Peet, J.; Theobald, K.A.; Douglas, C. Building Safety Cultures at the Frontline: An Emancipatory Practice Development Approach for Strengthening Nursing Surveillance on an Acute Care Ward. J. Clin. Nurs. 2022, 31, 642–656. [Google Scholar] [CrossRef]
- Halverson, C.C.; Scott Tilley, D. Creating a Culture of Support for Nursing Surveillance. Nurs. Forum. 2022, 57, 1204–1212. [Google Scholar] [CrossRef]
- Perry-Woodford, Z.L.; Marinova, P. Nurse-Led Surveillance of Ileoanal Pouch Patients Post-stoma Reversal: Outcomes at 12-Month Review. Br. J. Nurs. 2022, 31, S14–S21. [Google Scholar] [CrossRef]
- LeBlanc, P.; Kabbe, A.; Letvak, S. Nurses’ Knowledge Regarding Nursing Surveillance of the Septic Patient. Clin. Nurse Spec. 2022, 36, 309–316. [Google Scholar] [CrossRef]
- Christabel, S.; Sudhaker, C.; Varma, M. Nurses’ Outlook on Healthcare-Associated Infection Surveillance: Findings from Focus Group Discussions. Afr. J. Nurs. Midwif. 2022, 24, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Halverson, C.C.; Bailey, C.; Ennis, J.A.; Cox, E.E. Nursing Surveillance of Respiratory Adverse Events Among Hospitalized Adults: A Systematic Review to Guide Evidence-Based Practice. Worldviews Evid. Based Nurs. 2022, 19, 260–266. [Google Scholar] [CrossRef]
- Copanitsanou, P.; Santy-Tomlinson, J. The Nurses’ Role in the Diagnosis and Surveillance of Orthopaedic Surgical Site Infections. Int. J. Orthop. Trauma Nurs. 2021, 41, 100818. [Google Scholar] [CrossRef] [PubMed]
- Allen, D.E.; Fetzer, S.J.; Cummings, K.S. Decreasing Duration of Mechanical Restraint Episodes by Increasing Registered Nurse Assessment and Surveillance in an Acute Psychiatric Hospital [Formula: See Text]. J. Am. Psychiatr. Nurses Assoc. 2020, 26, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Henneman, E.A.; Gawlinski, A.; Giuliano, K.K. Surveillance: A Strategy for Improving Patient Safety in Acute and Critical Care Units. Crit. Care Nurse. 2012, 32, e9–e18. [Google Scholar] [CrossRef] [PubMed]
- Pfrimmer, D.M.; Johnson, M.R.; Guthmiller, M.L.; Lehman, J.L.; Ernste, V.K.; Rhudy, L.M. Surveillance: A Nursing Intervention for Improving Patient Safety in Critical Care Environment. Dimens. Crit. Care Nurs. 2017, 36, 45–52. [Google Scholar] [CrossRef]
- Milhomme, D.; Gagnon, J.; Lechasseur, K. The Clinical Surveillance Process as Carried Out by Expert Nurses in a Critical Care Context: A Theoretical Explanation. Intensive Crit. Care Nurs. 2018, 44, 24–30. [Google Scholar] [CrossRef]
- De la Cruz, F.A. Clinical Decision-Making Styles of Home Healthcare Nurses. Image. J. Nurs. Sch. 1994, 26, 222–226. [Google Scholar] [CrossRef]
- Rababa, M.; Bani-Hamad, D.; Hayajneh, A.A.; Al Mugheed, K. Nurses’ knowledge, attitudes, practice, and decision-making skills related to sepsis assessment and management. Electronic J. Gen. Med. 2022, 19, em420. [Google Scholar] [CrossRef]
- Kim, S.Y. A Study on Participation in Clinical Decision Making by Home Healthcare Nurses. J. Korean Acad. Nurs. 2010, 40, 892–902. [Google Scholar] [CrossRef] [PubMed]
- Butcher, H.K.; Bulechek, G.M.; Dochterman, J.M.; Wagner, C.M. Nursing Interventions Classification (NIC), 7th ed.; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Juvé-Udina, M.E.; Fabrellas-Padrés, N.; Adamuz-Tomás, J.; Cadenas-González, S.; Gonzalez-Samartino, M.; Cueva Ariza, L.D.L.; Delgado-Hito, P. Surveillance Nursing Diagnoses, Ongoing Assessment and Outcomes on in-Patients Who Suffered a Cardiorespiratory Arrest. Rev. Esc. Enferm. U.S.P. 2017, 51, e03286. [Google Scholar] [CrossRef]
- Kutney-Lee, A.; Lake, E.T.; Aiken, L.H. Development of the Hospital Nurse Surveillance Capacity Profile. Res. Nurs. Health. 2009, 32, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.; Choi, W.J.; Choi, W.H.; Kim, M.K. The Adoptions and Use of Electronic Nursing Records in Korean Hospitals: Findings of a Nationwide Survey. J. Korean Clin. Nurs. Res. 2013, 19, 345–356. [Google Scholar]
- The Korean Nurses Association News. The Level of Nurse Staffing Determines Patient Safety; Urgent Need to Revise Standards for the Ratio of Patients per Nurse. 2022. Available online: http://www.nursenews.co.kr/main/ArticleDetailView.asp?sSection=57&idx=31014&intPage=1;KoreanNursingAssociation (accessed on 24 March 2023).
- Singh, R.; Lichter, M.I.; Danzo, A.; Taylor, J.; Rosenthal, T. The Adoption and Use of Health Information Technology in Rural Areas: Results of a National Survey. J. Rural Health. 2012, 28, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Alsyouf, A.; Lutfi, A.; Alsubahi, N.; Alhazmi, F.N.; Al-Mugheed, K.; Anshasi, R.J.; Alharbi, N.I.; Albugami, M. The Use of a Technology Acceptance Model (TAM) to Predict Patients’ Usage of a Personal Health Record System: The Role of Security, Privacy, and Usability. Int. J. Environ. Res. Public Health 2023, 20, 1347. [Google Scholar] [CrossRef] [PubMed]
| Authors (Year) | Antecedents (RN) | Antecedents (Work Environment) | Attributes | Facilitate NS | Consequences (Adequate NS) | Barriers to the Implementation of NS | Consequences (Inadequate NS) |
|---|---|---|---|---|---|---|---|
| Peet et al. (2022) [18] | Clinical experience, asserted nurses’ clinical knowledge, critical reflection, psychological safety, holistic facilitation | Learning culture, patient safety culture, safe, and effective ward culture | Purposeful and collaborative assessment, clinical reasoning, observing handovers, complexity, collaborating with staff, exploring alternative solutions | Collaborative relationship, person-centered relationships by both patients and staff, hourly mandated, protocolized, scripted bedside rounding, sense of harmony and teamwork, shared vision | Build safety cultures, effective safe teamwork, and nurses’ confidence | Communication hierarchies, time-pressured handover, adverse event data and workload systems, nurse leadership disengagement, rising conflict with doctors, constant negative audit feedback, time-consuming meeting, underestimating the complex environment | Clinical deterioration, frustrating team communication, and teamwork |
| Halverson and Scott (2022) [19] | Nurse certification, nurse education, nurse expertise | Organizational culture—hiring, staffing—retention, healthcare facility, and medical equipment, a culture of effective interdisciplinary communication, clinical ladder programs, support system | Systematic process, pattern recognition, the anticipation of the problem of instability, coordinated communication | Teamwork, strong clinical resources, standardized assessment, and intervention tools, coordinated communication (nurse and doctor), evidence-based handoff techniques and formal systems, good mix of nursing staff expertise | Patient safety, reduction in adverse events, nurse satisfaction, decreased nurse burnout | Abrupt communication, reporting fear of retaliation, nurse handoff of omitted and missed care, interruption and interfering nursing care | Adverse outcomes, errors, nurse burnout |
| Perry-Woodford and Marinova (2022) [20] | Understanding patients’ specific concerns, highly skilled nursing competency | Patient pathway | Quality of advice, good working relationships with patients | Protocol, patient feedback, and audit | Patient satisfaction, reducing patients’ problems improvement in patients’ perception of QoL, and confidence | Not feeling well-informed, no solutions to patients’ problems | Restriction on patients’ life |
| LeBlanc et al. (2022) [21] | Nurses’ knowledge, confidence, concerns | Competency-based education, training, simulation, creative learning strategies, nurse-to-patient ratios, adequate staffing, professional courtesy, respect, and trust | Detecting changes in condition early and providing appropriate urgent medical care and treatment, purposeful and ongoing acquisition, interpretation, and synthesis of patient data for clinical decision-making, nurse monitoring, swift and appropriate interventions | Standardized tool and handoff sheet, critical information regarding the patient’s current condition and treatment, rapid response teams | Keeping the patient safe and decreasing failure to rescue, maximizing optimal patient outcomes, professional courtesy, and trust, working in sync with each other | Lack of adherence to policies, procedures, and shortcuts with the delivery of care, and the inability to provide nursing surveillance | Medical errors |
| Christabel et al. (2022) [22] | Willing to participate in training and upgrading knowledge | Adequate designated workforce with explicitly identified duties, ample lines of communication, safe working environment | Effective prevention, detection, and control of the problem, maintaining close contact with the laboratory findings, cooperation | Staffing/less paperwork, standardized manner, user-friendly computer program, healthcare personnel-related professionalism, role boundaries, daily workflow and management, interdisciplinary collaboration, standards and protocols, and technological infrastructure | High-quality healthcare | Uncertain about the process, inactive role in the surveillance process, increased work demands and staff shortage, no computer programs available to support NS | |
| Stotts et al. (2020) [6] | Nurse education, experience, expertise, confidence, timely recognition and mitigation of clinical deterioration, collaboration | Staffing, standardized assessment, communication tools, availability of emergency services, team composition, opportunities for multidisciplinary care planning | Assessment, documentation, decision-making, intervening, communication, continuous process of acquisition, interpretation, recognition, and management of clinical deterioration and synthesis of physical, behavioral, and cognitive patient data to determine intervention and threats to health and safety during the course of nursing care | Availability of medical equipment, staffing, skill and team composition, interactions, standardized tools between people, and with technology | Increasing nursing confidence and assertion of concerns and escalation | Clinical deterioration, adverse events, high stakes, time-dependent work | |
| Halverson et al. (2022) [23] | Purposeful, ongoing acquisition, interpretation, and synthesis of patient data for clinical decision-making, follow-up rounding, systematic process, pattern recognition, effective communication, and decision-making, physiological measurements associated with deterioration, continuous monitoring | EWS, consensus-approved assessment tools, vital sign-directed protocol, pre-MET UCR | Patient safety, detection of early deterioration signs | High incidence of pre-MET activation failure | |||
| Halverson and Scott (2022) [4] | Nurse education, expertise, staffing | Organizational culture | Systematic process, pattern recognition, anticipating problems, coordinated communication, decision-making | Assessment tool: EWS, NEWS, APACHE, checklists, follow-up rounding, coordinated handoff, pre-MET | Decreases complications, adverse outcomes, and nurse burnout, increased nurse satisfaction | Reactive care, uncoordinated care, siloed round | Adverse outcomes, medical errors, nurse burnout |
| Copanitsanou and Santy-Tomlinson (2021) [24] | Education, early recognition, and diagnosis of wound infection | Given feedback on their performance, hospital surveillance policies, effective diagnostic processes | Patient safety, effectiveness, and improvement of healthcare services | Scarcity of resources, lack of trained staff, microbiology support, and information technology support | Wasted energy and money | ||
| Allen et al. (2020) [25] | Knowledge and skill set, authority and training, expression of concern | Regulations, adjusting their workflow, and collaboration with each other | Direct and continuous observation and monitoring, recognize signs, accurately assess the probability | Changing their standards of practice to reflect what they know, believe, and value | Decreased duration of mechanical restraint episodes, quality improvement | Improper staffing, mandate | Increased risk and complications |
| No. | Sex | Age | Education | Position | Total Career (Years) | Current Department | Current Department Career (Years) | Nursing Care Confidence |
|---|---|---|---|---|---|---|---|---|
| 1 | Female | 27 | BSN | General nurse | 4.92 | M | 4.92 | 8 |
| 2 | Female | 30 | BSN | General nurse | 7.25 | M | 7.25 | 7 |
| 3 | Female | 37 | MSN | General nurse | 14.42 | HRC | 2.25 | 9 |
| 4 | Female | 38 | BSN | Head nurse | 15 | M | 15 | 8 |
| 5 | Female | 32 | MSN | General nurse | 9.67 | ICU | 8.08 | 7 |
| 6 | Female | 32 | MSN | General nurse | 8.33 | M-S | 8.33 | 9 |
| 7 | Female | 49 | MSN | Charge nurse | 28.83 | S | 1.25 | 10 |
| 8 | Female | 48 | MSN | Charge nurse | 24.83 | IR | 9 | 9 |
| 9 | Female | 33 | BSN | Charge nurse | 13 | S | 3 | 6 |
| 10 | Female | 30 | BSN | General nurse | 5.75 | ICU | 5.75 | 8 |
| Antecedents (Situation) | Antecedents (RN) | Antecedents (Work Environment) | Attributes (Subcategories) | Participant Statements | Consequences (Adequate NS) | Consequences (Inadequate NS) |
|---|---|---|---|---|---|---|
| Handover, circumstances different from handover details, sudden change in patient condition after surgery or treatment, the occurrence of disease complications, urgent care, and emergencies | 3–4 years of clinical experience, nursing proficiency, knowledge of disease and nursing, passion and will to actively solve problems, nursing professionalism, responsibility, rapport formation, intuition, interest, and empathy for patients, communication skills, careful observation, self-health and emotional control | Support of auxiliary personnel, patient severity, securing time for direct nursing care, staffing according to nursing proficiency, reducing the patient-to-nurse ratio, support and encouragement from colleagues, doctor–nurse cooperative relationship and sense of fellowship, sharing of treatment plans with doctors, practical training by the department, new nurse education and adaptation training | Systematic assessment | Carefully listening to handover details, direct confirmation of handover details (V/S, hemodynamic monitoring, consciousness, appearance, existing lines and drains, catheters, medication, order, lab, video, assessment through open questions to patients and guardians, disease characteristics focus assessment, treatment, treatment, postintervention effect assessment), acquisition of problematic cues, checking of alarms, past events, patient monitoring settings 24 h before handover and trend of patient condition change, continuous monitoring of the patient condition, planned rounds, checking the effectiveness of nursing intervention and treatment | The rapid and appropriate response to emergencies, patient safety, improvement of patient care quality, rapid recovery of patients and reduction in patient length of stay, patient’s cooperation and satisfaction, nurse’s job satisfaction and pride, increasing confidence in nursing performance, and hospital awareness and rapport with patients, doctors, and colleagues, decreasing nurse burnout and turnover, and frequency of unexpected emergencies, smooth progress as if a cogwheel was being engaged, reducing patient costs, preventing unnecessary treatment, passing on experiences to junior nurse | Deterioration of patient condition, death of a patient, an accusation of patient, guardian, doctor, and colleague, increase in customer’s complaints and patient medical costs, increasing nurse’s workload, working hours, fatigue, burnout, stress, and training costs, increase in medical lawsuits, financial loss, loss of trust with patients, medical staff, colleagues, and other departments, decreasing hospital satisfaction, increasing fear of patient care, guilt, excessive treatment |
| Pattern recognition | Arranging handover details, organizing patient assessment data, integrating handover details and assessment data, interpreting the meaning of assessment data, identifying patterns by checking and comparing past and current assessment data, thinking about and finding factors that cause changes in patient conditions, recognizing patient problems to be solved during duty, treatment and nursing goals, recalling past patient experiences, evaluation of treatment and intervention effects | |||||
| Anticipation of problem | Prediction of the patient’s problem situation through past and present data, including baseline data; prioritization of problems to be solved during duty; detection of problems and prediction of them by comprehensively judging the assessment data before the patient’s condition changes; disease progression, treatment effects, comparison with past patterns, predicting disease progression and doctor’s orders, preparing patients, and providing nursing care | |||||
| Effective communication | Communicating with patients and guardians, communicating with handover nurses and duty nurses on the same shift, notifying doctors of perceived problems, patient condition, and changes after intervention | |||||
| Decision-making | Discussion and proposal of the patient treatment plan, participation in patient treatment decision-making, the suggestion of consulting with other departments | |||||
| Performing nursing practice | Carrying out nursing care according to orders or protocols, educating and preparing patients and guardians about predicted problems, symptom reduction, and problem-solving nursing, preparing for and carrying out predicted doctor’s orders, performing interventions that have to be carried out on time |
| Antecedents (Situation) | Antecedents (RN) | Antecedents (Work Environment) | Attributes | Consequences (Adequate NS) | Consequences (Inadequate NS) | |
|---|---|---|---|---|---|---|
| -Handover -A sudden change in the patient’s condition -Urgent care and emergencies | -Clinical experience -Knowledge -Expertise -Professionalism -Responsibility -Communication skills -Self-health and emotional control | -Supporting resources -Securing time for direct nursing care -Proper nurse staffing -Cooperative relationship with staff -Education and adaptation program -Organizational culture -Clear standards and guidelines | Systematic assessment | -Purposeful and collaborative assessment -Acquisition of problematic cues -Continuous monitoring of the patient’s condition -Planned round -Checking the effectiveness of nursing intervention and treatment | -Patient safety -Improvement of patient care quality -Patient’s cooperation and satisfaction -Increasing nurse’s job satisfaction, confidence, hospital awareness, and rapport with patients, doctors, and colleagues, -Preventing unnecessary treatment -Passing on experiences to junior nurse | -Deterioration of the patient’s condition -Accusation of patient, guardian, doctor, and colleague -Increasing patient medical costs, nurse’s workload, burnout, stress, and training costs -Increase in medical lawsuits, financial loss, loss of trust |
| Pattern recognition | -Organizing and synthesizing handover details and assessment data -Interpreting the meaning of assessment data -Identifying patterns by checking and comparing past and current assessment data -Recognizing patient problems to be solved during duty -Evaluating treatment and intervention effects | |||||
| Anticipation of problems | -Prioritization of problems to be solved during duty -Detection of problems and prediction by comprehensively judging the assessment data before the patient’s condition change -Progress of the disease, and the treatment effect -Comparing with past patterns, predicting disease progression, and doctor’s order -Preparing for patients and nursing care | |||||
| Effective communication | -Effective and coordinated communication with patients, guardians, handover nurses, duty nurses on the same shift, and other departments -Notifying doctors of perceived problems, patient conditions, and changes after the intervention | |||||
| Decision- making | -Participation in the decision-making for patient treatment plans -Exploring alternative solutions | |||||
| Performing nursing practice | -Performing nursing care according to orders, protocols, guidelines, and standards for clinical deterioration and problem-solving -Carrying out duty after predicting and preparing doctor’s orders -Performing interventions that have to be carried out on time | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Cho, M.-K. Concept Analysis of Nursing Surveillance Using a Hybrid Model. Healthcare 2023, 11, 1613. https://doi.org/10.3390/healthcare11111613
Kim SY, Cho M-K. Concept Analysis of Nursing Surveillance Using a Hybrid Model. Healthcare. 2023; 11(11):1613. https://doi.org/10.3390/healthcare11111613
Chicago/Turabian StyleKim, Se Young, and Mi-Kyoung Cho. 2023. "Concept Analysis of Nursing Surveillance Using a Hybrid Model" Healthcare 11, no. 11: 1613. https://doi.org/10.3390/healthcare11111613






