Prognostic Impact of Sarcopenic Obesity after Neoadjuvant Chemotherapy Followed by Surgery in Elderly Patients with Esophageal Squamous Cell Carcinoma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Neoadjuvant Chemotherapy
2.3. Evaluation of Chemotherapy-related Toxicities and Postoperative Complications
2.4. Measurement and Definitions of Body Composition
2.5. Patient Data
2.6. Nutritional Screening
2.7. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. NAC-Related Factors
3.3. Operation-Related Factors
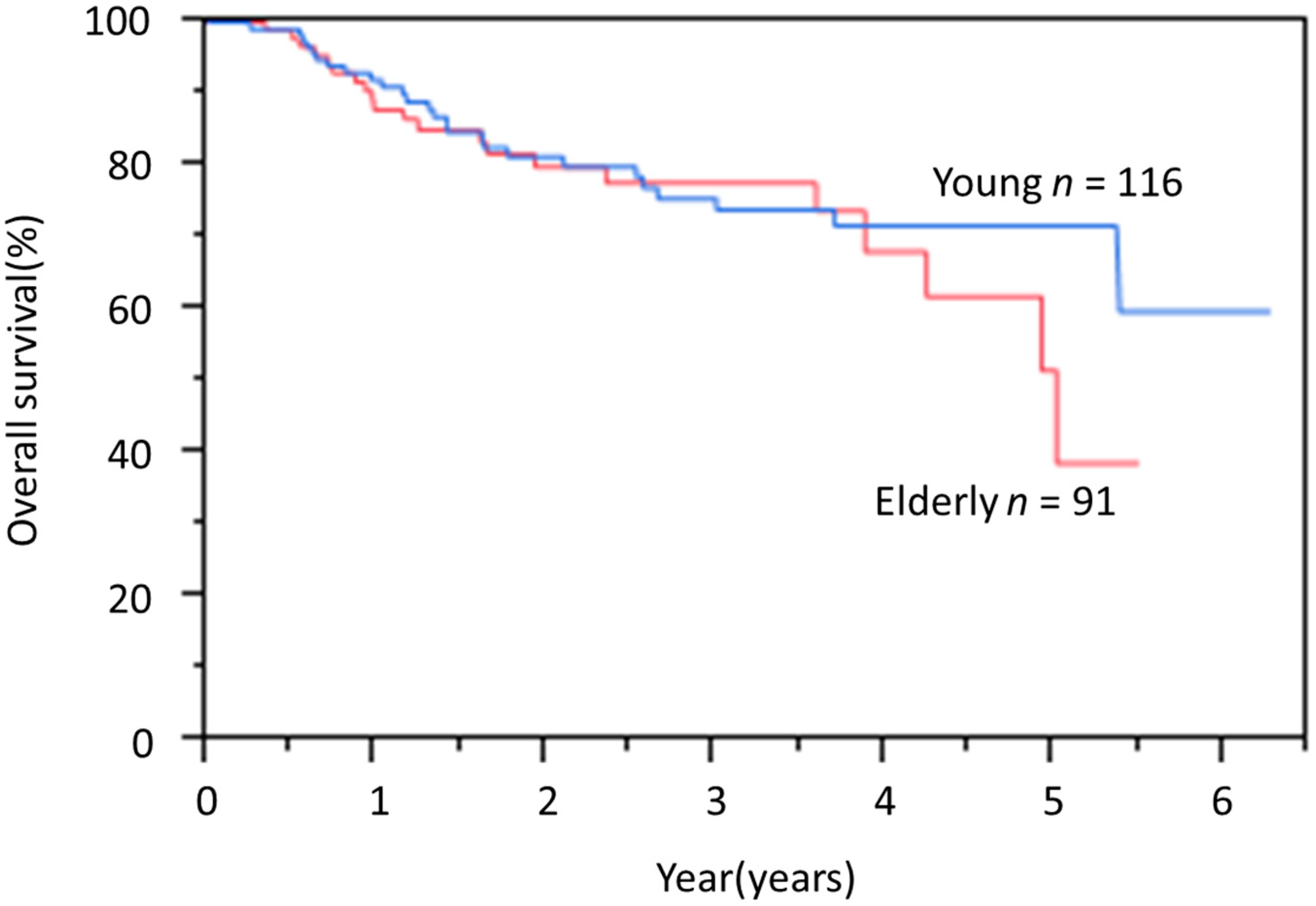
3.4. OS Rate
3.5. Prognostic Factors for OS in the Elderly Group
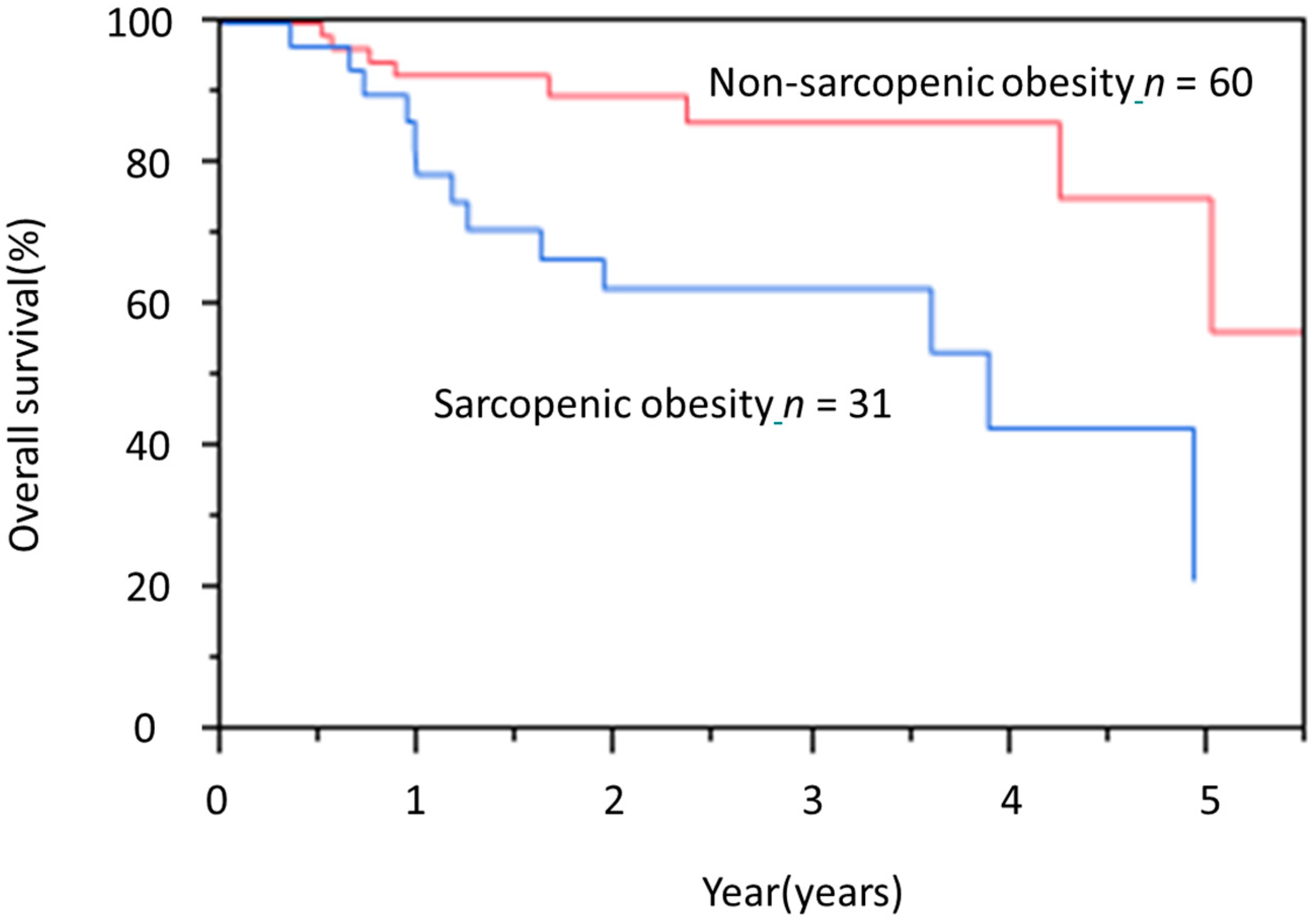
3.6. Characteristics of Sarcopenic Obesity in the Elderly Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Smyth, E.C.; Lagergren, J.; Fitzgerald, R.C.; Lordick, F.; Shah, M.A.; Lagergren, P.; Cunningham, D. Oesophageal cancer. Nat. Rev. Dis. Primers 2017, 3, 17048. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, Y.; Uno, T.; Oyama, T.; Kato, K.; Kato, H.; Kawakubo, H.; Kawamura, O.; Kusano, M.; Kuwano, H.; Takeuchi, H.; et al. Esophageal cancer practice guidelines 2017 edited by the Japan Esophageal Society: Part 1. Esophagus 2019, 16, 1–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ando, N.; Kato, H.; Igaki, H.; Shinoda, M.; Ozawa, S.; Shimizu, H.; Nakamura, T.; Yabusaki, H.; Aoyama, N.; Kurita, A.; et al. A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann. Surg. Oncol. 2012, 19, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Nishiguchi, S.; Fukutani, N.; Tanigawa, T.; Yukutake, T.; Kayama, H.; Aoyama, T.; Arai, H. Prevalence of sarcopenia in community-dwelling Japanese older adults. J. Am. Med. Dir. Assoc. 2013, 14, 911–915. [Google Scholar] [CrossRef]
- Onishi, S.; Shiraki, M.; Nishimura, K.; Hanai, T.; Moriwaki, H.; Shimizu, M. Prevalence of sarcopenia and its relationship with nutritional state and quality of life in patients with digestive diseases. J. Nutr. Sci. Vitaminol. (Tokyo) 2018, 64, 445–453. [Google Scholar] [CrossRef] [Green Version]
- Deng, H.Y.; Zha, P.; Peng, L.; Hou, L.; Huang, K.L.; Li, X.Y. Preoperative sarcopenia is a predictor of poor prognosis of esophageal cancer after esophagectomy: A comprehensive systematic review and meta-analysis. Dis. Esophagus 2019, 32, doy115. [Google Scholar] [CrossRef] [Green Version]
- Sato, S.; Kunisaki, C.; Suematsu, H.; Tanaka, Y.; Miyamoto, H.; Kosaka, T.; Yukawa, N.; Tanaka, K.; Sato, K.; Akiyama, H.; et al. Impact of sarcopenia in patients with unresectable locally advanced esophageal cancer receiving chemoradiotherapy. In Vivo 2018, 32, 603–610. [Google Scholar] [CrossRef]
- Onishi, S.; Tajika, M.; Tanaka, T.; Hirayama, Y.; Hara, K.; Mizuno, N.; Kuwahara, T.; Kuno, N.; Inaba, Y.; Kodaira, T.; et al. Prognostic significance of sarcopenia in patients with unresectable advanced esophageal cancer. J. Clin. Med. 2019, 8, 1647. [Google Scholar] [CrossRef] [Green Version]
- Rier, H.N.; Jager, A.; Sleijfer, S.; Maier, A.B.; Levin, M.D. The prevalence and prognostic value of low muscle mass in cancer patients: A review of the literature. Oncologist 2016, 21, 1396–1409. [Google Scholar] [CrossRef] [Green Version]
- Levolger, S.; van Vugt, J.L.; de Bruin, R.W.; IJzermans, J.N. Systematic review of sarcopenia in patients operated on for gastrointestinal and hepatopancreatobiliary malignancies. Br. J. Surg. 2015, 102, 1448–1458. [Google Scholar] [CrossRef]
- Pamoukdjian, F.; Bouillet, T.; Lévy, V.; Soussan, M.; Zelek, L.; Paillaud, E. Prevalence and predictive value of pre-therapeutic sarcopenia in cancer patients: A systematic review. Clin. Nutr. 2018, 37, 1101–1113. [Google Scholar] [CrossRef] [PubMed]
- Anandavadivelan, P.; Brismar, T.B.; Nilsson, M.; Johar, A.M.; Martin, L. Sarcopenic obesity: A probable risk factor for dose limiting toxicity during neo-adjuvant chemotherapy in oesophageal cancer patients. Clin. Nutr. 2016, 35, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.; Jia, C.; Rouvelas, I.; Lagergren, P. Risk factors for malnutrition after oesophageal and cardia cancer surgery. Br. J. Surg. 2008, 95, 1362–1368. [Google Scholar] [CrossRef] [PubMed]
- Prado, C.M.; Lieffers, J.R.; McCargar, L.J.; Reiman, T.; Sawyer, M.B.; Martin, L.; Baracos, V.E. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: A population-based study. Lancet Oncol. 2008, 9, 629–635. [Google Scholar] [CrossRef]
- Mourtzakis, M.; Prado, C.M.; Lieffers, J.R.; Reiman, T.; McCargar, L.J.; Baracos, V.E. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl. Physiol. Nutr. Metab. 2008, 33, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Iritani, S.; Imai, K.; Takai, K.; Hanai, T.; Ideta, T.; Miyazaki, T.; Suetsugu, A.; Shiraki, M.; Shimizu, M.; Moriwaki, H. Skeletal muscle depletion is an independent prognostic factor for hepatocellular carcinoma. J. Gastroenterol. 2015, 50, 323–332. [Google Scholar] [CrossRef]
- Imai, K.; Takai, K.; Watanabe, S.; Hanai, T.; Suetsugu, A.; Shiraki, M.; Shimizu, M. Sarcopenia impairs prognosis of patients with hepatocellular carcinoma: The role of liver functional reserve and tumor-related factors in loss of skeletal muscle volume. Nutrients 2017, 9, 1054. [Google Scholar] [CrossRef] [Green Version]
- Nishikawa, H.; Shiraki, M.; Hiramatsu, A.; Moriya, K.; Hino, K.; Nishiguchi, S. Japan Society of Hepatology guidelines for sarcopenia in liver disease (1st edition): Recommendation from the working group for creation of sarcopenia assessment criteria. Hepatol. Res. 2016, 46, 951–963. [Google Scholar] [CrossRef]
- Baker, J.P.; Detsky, A.S.; Wesson, D.E.; Wolman, S.L.; Stewart, S.; Whitewell, J.; Langer, B.; Jeejeebhoy, K.N. Nutritional assessment: A comparison of clinical judgement and objective measurements. N. Engl. J. Med. 1982, 306, 969–972. [Google Scholar] [CrossRef]
- Wakahara, T.; Shiraki, M.; Murase, K.; Fukushima, H.; Matsuura, K.; Fukao, A.; Kinoshita, S.; Kaifuku, N.; Arakawa, N.; Tamura, T.; et al. Nutritional screening with Subjective Global Assessment predicts hospital stay in patients with digestive diseases. Nutrition 2007, 23, 634–639. [Google Scholar] [CrossRef]
- Makiura, D.; Ono, R.; Inoue, J.; Kashiwa, M.; Oshikiri, T.; Nakamura, T.; Kakeji, Y.; Sakai, Y.; Miura, Y. Preoperative sarcopenia is a predictor of postoperative pulmonary complications in esophageal cancer following esophagectomy: A retrospective cohort study. J. Geriatr. Oncol. 2016, 7, 430–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reisinger, K.W.; Bosmans, J.W.; Uittenbogaart, M.; Alsoumali, A.; Poeze, M.; Sosef, M.N.; Derikx, J.P. Loss of skeletal muscle mass during neoadjuvant chemoradiotherapy predicts postoperative mortality in esophageal cancer surgery. Ann. Surg. Oncol. 2015, 22, 4445–4452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugawara, K.; Yamashita, H.; Okumura, Y.; Yagi, K.; Yoshimura, S.; Kawasaki, K.; Tanabe, A.; Aikou, S.; Seto, Y. Relationships among body composition, muscle strength, and sarcopenia in esophageal squamous cell carcinoma patients. Support. Care Cancer 2020, 28, 2797–2803. [Google Scholar] [CrossRef] [PubMed]
- Baracos, V.E.; Arribas, L. Sarcopenic obesity: Hidden muscle wasting and its impact for survival and complications of cancer therapy. Ann. Oncol. 2018, 29 (Suppl. 2), ii1–ii9. [Google Scholar] [CrossRef] [PubMed]
- Must, A.; Spadano, J.; Coakley, E.H.; Field, A.E.; Colditz, G.; Dietz, W.H. The disease burden associated with overweight and obesity. JAMA 1999, 282, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Sandini, M.; Bernasconi, D.P.; Fior, D.; Molinelli, M.; Ippolito, D.; Nespoli, L.; Caccialanza, R.; Gianotti, L. A high visceral adipose tissue-to-skeletal muscle ratio as a determinant of major complications after pancreatoduodenectomy for cancer. Nutrition 2016, 32, 1231–1237. [Google Scholar] [CrossRef]
- Nishigori, T.; Tsunoda, S.; Okabe, H.; Tanaka, E.; Hisamori, S.; Hosogi, H.; Shinohara, H.; Sakai, Y. Impact of sarcopenic obesity on surgical site infection after laparoscopic total gastrectomy. Ann. Surg. Oncol. 2016, 23, 524–531. [Google Scholar] [CrossRef]
- Srikanthan, P.; Hevener, A.L.; Karlamangla, A.S. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: Findings from the National Health and Nutrition Examination Survey III. PLoS ONE 2010, 5, e10805. [Google Scholar] [CrossRef]
- Pierpont, Y.N.; Dinh, T.P.; Salas, R.E.; Johnson, E.L.; Wright, T.G.; Robson, M.C.; Payne, W.G. Obesity and surgical wound healing: A current review. ISRN Obes. 2014, 2014, 638936. [Google Scholar] [CrossRef] [Green Version]
- Malietzis, G.; Johns, N.; Al-Hassi, H.O.; Knight, S.C.; Kennedy, R.H.; Fearon, K.C.; Aziz, O.; Jenkins, J.T. Low muscularity and myosteatosis is related to the host systemic inflammatory response in patients undergoing surgery for colorectal cancer. Ann. Surg. 2016, 263, 320–325. [Google Scholar] [CrossRef]
- Fearon, K.; Strasser, F.; Anker, S.D.; Bosaeus, I.; Bruera, E.; Fainsinger, R.L.; Jatoi, A.; Loprinzi, C.; MacDonald, N.; Mantovani, G.; et al. Definition and classification of cancer cachexia: An international consensus. Lancet Oncol. 2011, 12, 489–495. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Gonzalez, M.C.; Shen, W.; Redman, L.; Thomas, D. Weight loss composition is one-fourth fat-free mass: A critical review and critique of this widely cited rule. Obes. Rev. 2014, 15, 310–321. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, J.C.; Malik, V.; Jia, W.; Kadowaki, T.; Yajnik, C.S.; Yoon, K.-H.; Hu, F.B. Diabetes in Asia: Epidemiology, risk factors, and pathophysiology. JAMA 2009, 301, 2129–2140. [Google Scholar] [CrossRef]
| Total | Elderly | Young | ||
|---|---|---|---|---|
| Variables | (n = 207) | (n = 91) | (n = 116) | p |
| Age (years) | 68.9 ± 5.4 (60–81) | 74.1 ± 2.9 (70–81) | 64.9 ± 2.9 (60–69) | <0.01 |
| Sex (male/female) | 169/38 | 73/18 | 96/20 | 0.71 |
| ASA-PS (1/2) | 70/137 | 21/70 | 49/67 | <0.01 |
| Body mass index (kg/m2) | 21.0 ± 2.8 (13.7–30.5) | 21.1 ± 2.8 (13.7–30.5) | 20.9 ± 2.8 (14.8–27.3) | 0.81 |
| Body mass index >25 kg/m2 | 15 (7.3) | 6 (6.6) | 9 (7.7) | 0.79 |
| Visceral fat mass (cm2) | 93.9 ± 55.9 | 94.9 ± 55.9 | 93.1 ± 56.1 | 0.81 |
| Obese | 91 (44.0) | 41 (45.1) | 50 (43.1) | 0.78 |
| Albumin (g/dL) | 4.13 ± 0.37 | 4.09 ± 0.41 | 4.16 ± 0.34 | 0.14 |
| CCr | 75.9 ± 15.1 | 74.2 ± 15.1 | 77.3 ± 14.9 | 0.13 |
| ChE | 292 ± 64 | 290 ± 61 | 294 ± 66 | 0.63 |
| T-chol | 196 ± 36 | 189 ± 32 | 201 ± 39 | 0.02 |
| Hb | 13.5 ± 1.5 | 13.5 ± 1.3 | 13.6 ± 1.7 | 0.54 |
| SGA (A/B or C) | 149/58 | 53/38 | 96/20 | <0.01 |
| Body weight loss rate (%) | 3.4 ± 5.5 | 3.4 ± 5.5 | 3.3 ± 5.5 | 0.83 |
| Sarcopenia, n (%) | 142 (68.6) | 69 (75.8) | 73 (62.9) | 0.06 |
| Sarcopenic obesity, n (%) | 58 (28.0) | 31 (34.1) | 27 (23.3) | 0.08 |
| %VC | 101.4 ± 13.3 | 100.6 ± 15.1 | 102.1 ± 11.7 | 0.42 |
| %FEV1.0 | 77.2 ± 8.0 | 76.9 ± 7.8 | 77.4 ± 8.2 | 0.62 |
| Diabetes mellitus, n (%) | 32 (15.5) | 20 (21.9) | 12 (10.3) | 0.03 |
| Cardiovascular disorder, n (%) | 97 (46.9) | 49 (53.8) | 48 (41.4) | 0.09 |
| Cerebrovascular disorder, n (%) | 2 (0.9) | 2 (2.2) | 0(0) | 0.19 |
| Malignant disease, n (%) | 40 (19.3) | 25 (27.5) | 15 (12.9) | 0.01 |
| Chronic disease, n (%) | 32 (15.4) | 10 (10.9) | 22 (18.9) | 0.12 |
| Primary tumor location (Ut/Mt/Lt) | 31/109/67 | 13/48/30 | 18/61/37 | 0.93 |
| Clinical T (1/2/3) | 35/41/131 | 16/17/58 | 19/24/73 | 0.41 |
| Clinical N (0/1/2/3) | 25/109/68/5 | 12/53/26/0 | 13/56/42/5 | 0.11 |
| Clinical stage (II/III) | 68/139 | 29/62 | 39/77 | 0.88 |
| Elderly | Young | p | |
|---|---|---|---|
| Variables | (n = 91) | (n = 116) | |
| Adverse events (≥ grade 3), n (%) | |||
| Hematological | |||
| Neutropenia | 40 (46.0) | 69 (59.5) | 0.06 |
| Non-hematological adverse events | |||
| Diarrhea | 3 (3.5) | 7 (6.0) | 0.52 |
| Malaise | 8 (9.2) | 8 (6.9) | 0.6 |
| Anorexia | 8 (9.2) | 8 (6.9) | 0.6 |
| Incomplete case | 6 (6.6) | 8 (6.9) | 0.31 |
| Operation time (min) | 497.4 ± 96.3 | 478.3 ± 89.1 | 0.14 |
| Hospital stay (days) | 29.1 ± 17.9 | 27.7 ± 17.5 | 0.57 |
| Surgery-related complications (≥Grade 3), n (%) | 29 (31.9) | 42 (36.2) | 0.55 |
| Anastomotic | 4 (4.4) | 7 (6.0) | 0.75 |
| Pneumonia | 7 (7.7) | 3 (2.6) | 0.11 |
| Recurrent nerve paralysis | 2 (2.2) | 1 (0.9) | 0.58 |
| SSI | 10 (11.0) | 12 (10.3) | 1.00 |
| Chylothorax | 2 (2.2) | 2 (1.7) | 1.00 |
| Arrhythmia | 0 (0) | 1 (0.9) | 1.00 |
| Anastomosis stenosis | 15 (16.5) | 27 (23.3) | 0.30 |
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| Variables | n | HR (95%CI) | p | HR (95%CI) | p | |
| Age, years | <75 | 57 | 2.11 (0.82–6.16) | |||
| ≥75 | 34 | 1 | 0.12 | |||
| Sex | male | 73 | 2.78 (0.80–17.5) | |||
| female | 18 | 1 | 0.11 | |||
| cStage | III | 62 | 1.47 (0.57–4.49) | |||
| II | 29 | 1 | 0.43 | |||
| NAC | DCF | 24 | 1.79 (0.71–4.36) | |||
| FP | 67 | 1 | 0.21 | |||
| ASA-PS | 2 | 70 | 2.54 (0.73–16.1) | |||
| 1 | 21 | 1 | 0.16 | |||
| DM | + | 20 | 2.11 (0.77–5.38) | |||
| - | 71 | 1 | 0.14 | |||
| Cardiovascular event | + | 49 | 1.06 (0.43–2.66) | |||
| - | 42 | 1 | 0.88 | |||
| Malignant disease | + | 25 | 1.87 (0.73–4.51) | |||
| - | 66 | 1 | 0.18 | |||
| SGA | A | 53 | 1.33 (0.54–3.42) | |||
| B-C | 38 | 1 | 0.53 | |||
| Sarcopenia | + | 69 | 6.11 (1.25–111.0) | |||
| - | 22 | 1 | 0.02 | |||
| Sarcopenic obesity | + | 31 | 3.52 (1.41–9.48) | 2.72 (1.06–7.76) | ||
| - | 60 | 1 | <0.01 | 1 | 0.03 | |
| Sarcopenic Obesity | Non-Sarcopenic Obesity | ||
|---|---|---|---|
| Variables | (n = 31) | (n = 60) | p |
| Age (years) | 73.6 ± 3.1 | 74.3 ± 2.9 | 0.36 |
| Sex (male/female) | 27/4 | 46/14 | 0.28 |
| ASA-PS (1/2) | 7/24 | 14/46 | 1.00 |
| Body mass index (kg/m2) | 22.2 ± 2.3 | 20.4 ± 2.8 | <0.01 |
| Body mass index >25 kg/m2 | 3 (9.7) | 3 (5.0) | 0.40 |
| Visceral fat mass (cm²) | 134.7 ± 36.8 | 75.0 ± 53.3 | <0.01 |
| Albumin (g/dL) | 4.10 ± 0.36 | 4.05 ± 0.44 | 0.21 |
| CCr | 74.4 ± 12.5 | 74.1 ± 16.4 | 0.92 |
| ChE | 307 ± 70 | 281 ± 54 | 0.06 |
| T-chol | 188.8 ± 40.1 | 189.9 ± 28.5 | 0.88 |
| Hb | 13.8 ± 1.1 | 13.3 ± 1.3 | 0.06 |
| SGA (A/B or C) | 26/5 | 27/33 | <0.01 |
| Body weight loss rate (%) | 1.7 ± 3.2 | 4.3 ± 6.2 | 0.03 |
| %VC | 98.6 ± 16.2 | 101.6 ± 14.6 | 0.38 |
| %FEV1.0 | 77.0 ± 6.9 | 76.8 ± 8.3 | 0.90 |
| Diabetes mellitus, n (%) | 7 (22.6) | 13 (21.7) | 1.00 |
| Cardiovascular disorder, n (%) | 17 (54.8) | 32 (53.3) | 1.00 |
| Cerebrovascular disorder, n (%) | 1 (3.2) | 1 (1.7) | 1.00 |
| Malignant disease, n (%) | 9 (29.0) | 16 (26.7) | 0.81 |
| Chronic disease, n (%) | 3 (9.7) | 7 (11.6) | 1.00 |
| Sarcopenic Obesity | Non-Sarcopenic Obesity | ||
|---|---|---|---|
| Variables | (n = 31) | (n = 60) | p |
| Adverse events (≥ grade 3), n (%) | |||
| Hematological | |||
| Neutropenia | 11 (43.2) | 29 (58.3) | 0.49 |
| Non-hematological adverse events | |||
| Diarrhea | 0 (0) | 3 (3.8) | 0.54 |
| Malaise | 2 (6.8) | 6 (6.8) | 1.00 |
| Anorexia | 2 (6.8) | 6 (6.8) | 1.00 |
| Incomplete case | 2(6.5) | 4(6.7) | 1.00 |
| Operation time (min) | 522.7 ± 92.6 | 484.0 ± 96.2 | 0.06 |
| Hospital stay (days) | 33.4 ± 20.9 | 26.8 ± 15.8 | 0.09 |
| Surgery related complications (≥grade 3), n (%) | 13 (41.9) | 16 (26.7) | 0.15 |
| Anastomotic | 3 (9.7) | 1 (1.7) | 0.11 |
| Pneumonia | 5 (16.1) | 2 (3.3) | 0.04 |
| Recurrent nerve paralysis | 1 (3.2) | 1 (1.7) | 1.00 |
| SSI | 3 (9.7) | 7 (11.7) | 1.00 |
| Chylothorax | 1 (3.2) | 1 (1.7) | 1.00 |
| Arrhythmia | 0 (0) | 0 (0) | 1.00 |
| Anastomosis stenosis | 8 (25.8) | 7 (11.7) | 0.13 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Onishi, S.; Tajika, M.; Tanaka, T.; Yamada, K.; Abe, T.; Higaki, E.; Hosoi, T.; Inaba, Y.; Muro, K.; Shimizu, M.; et al. Prognostic Impact of Sarcopenic Obesity after Neoadjuvant Chemotherapy Followed by Surgery in Elderly Patients with Esophageal Squamous Cell Carcinoma. J. Clin. Med. 2020, 9, 2974. https://doi.org/10.3390/jcm9092974
Onishi S, Tajika M, Tanaka T, Yamada K, Abe T, Higaki E, Hosoi T, Inaba Y, Muro K, Shimizu M, et al. Prognostic Impact of Sarcopenic Obesity after Neoadjuvant Chemotherapy Followed by Surgery in Elderly Patients with Esophageal Squamous Cell Carcinoma. Journal of Clinical Medicine. 2020; 9(9):2974. https://doi.org/10.3390/jcm9092974
Chicago/Turabian StyleOnishi, Sachiyo, Masahiro Tajika, Tsutomu Tanaka, Keisaku Yamada, Tetsuya Abe, Eiji Higaki, Takahiro Hosoi, Yoshitaka Inaba, Kei Muro, Masahito Shimizu, and et al. 2020. "Prognostic Impact of Sarcopenic Obesity after Neoadjuvant Chemotherapy Followed by Surgery in Elderly Patients with Esophageal Squamous Cell Carcinoma" Journal of Clinical Medicine 9, no. 9: 2974. https://doi.org/10.3390/jcm9092974





