Postoperative Telephone-Based Questionnaire on Quality of Life after Robotic-Assisted Laparoscopic Hysterectomy versus Conventional Total Laparoscopic Hysterectomy
Abstract
:1. Introduction
Objective
2. Method
2.1. Design of Questionnaire
2.2. Telephone Interview
2.3. Material
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
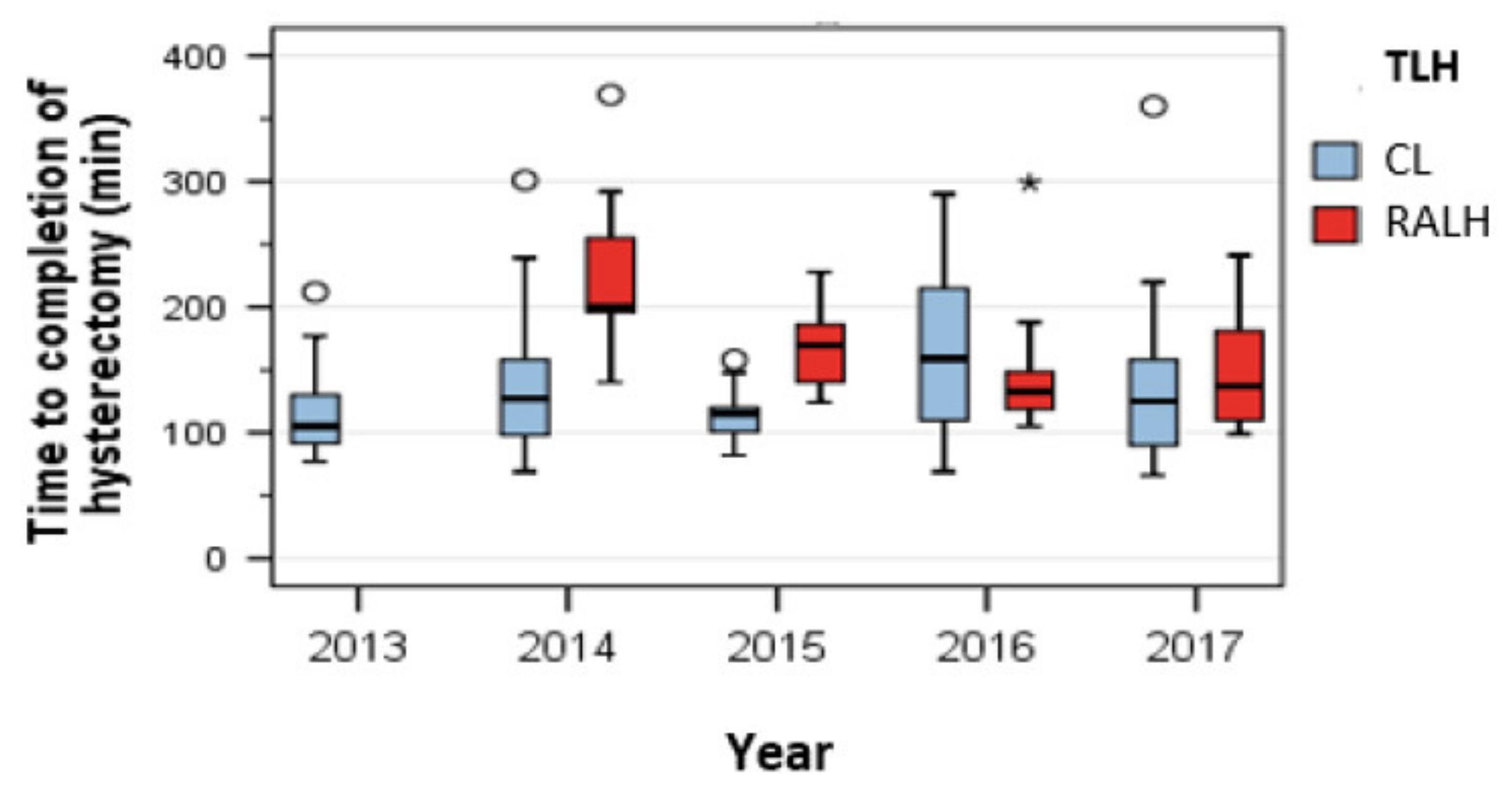
3.2. Operating Time
3.3. Learning Curve
3.4. Intra- and Postoperative Complications
3.5. Length of Hospital Stay, Pain Scores, and Postoperative Intake of Painkillers
3.6. Postoperative Satisfaction and Dissatisfaction
3.7. Dissatisfaction with the Abdominal Incision
3.8. Limitation of Sexual Intercourse
3.9. Convalescence
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| German speaking community | English speaking community |
| (1) Zum Zeitpunkt der OP waren Sie: verheiratet □ in einer festen Beziehung □ ledig □ verwitwet □? | (1) What was your relationship status at the time of the operation? Married- in a committed relationship- single- widowed |
| (2) Wie war Ihr Zustand zum Zeitpunkt der OP? Waren Sie: Noch nicht in den Wechseljahren □ in den Wechseljahren □ durch die Wechseljahre durch □? | (2) What was your hormone status at the time of the operation? Premenopausal Perimenopausal Post menopausal |
| (3) Wie lange waren Sie krankgeschrieben nach der Gebärmutterentfernung? Tage__________________ | (3) How long were you on sick leave after hysterectomy? Days: _____________________ |
| (4) Auf einer Skala von 1-6, wobei analog zum Schulnotensystem, hier 1 = sehr zufrieden/bestmögliche Zufriedenheit und 6 = sehr unzufrieden/überhaupt keine Zufriedenheit, bedeutet: Wie zufrieden sind Sie dann mit dem Behandlungsergebnis der OP insgesamt? Skala: 🙂 1 □ 2 □ 3 □ 4 □ 5 □ 6 □ 🙁 | (4) How satisfied are you with the result of the hospital treatment all in all? On a scale from 1–6, whereby analogous to the German school grading system, here 1 means = very satisfied/best possible satisfaction and 6 means = very dissatisfied/no satisfaction at all: Scale 🙂 1 □ 2 □ 3 □ 4 □ 5 □ 6 □ 🙁 |
| (5) Würden Sie diese Operation unter den gleichen Umständen weiterempfehlen? Ja □ Nein □ | (5) In the same circumstances, would you recommend this surgery to others? Yes □ No □ |
| (6) Auf einer Skala von 0–10, wobei hier 0 = keine Schmerzen, 10 = stärkste vorstellbare Schmerzen bedeutet, Wie waren die Schmerzen nach der Operation im Abstand nach: 6a) Ca. 1 Woche? Skala: 🙂 0 □ 1 □ 2 □ 3 □ 4 □ 5□ 6 □ 7 □ 8 □ 9 □ 10 □ 🙁 6b) Ca. 4 Wochen? Skala: 🙂 0 □ 1 □ 2 □ 3 □ 4 □ 5 □ 6 □ 7 □ 8 □ 9 □ 10 □ 🙁 | (6) How was the pain after surgery? On a scale of 0–10, 0 means = no pain, 10 means = strongest imaginable pain 6a) After 1 week: Scale: 🙂 0 □ 1 □ 2 □ 3 □ 4 □ 5 □ 6 □ 7 □ 8 □ 9 □ 10 □ 🙁 6b) After 4 weeks: Scale 🙂 0 □ 1 □ 2 □ 3 □ 4 □ 5 □ 6 □ 7 □ 8 □ 9 □ 10 □ 🙁 |
| (7) Wie lange haben Sie Schmerzmittel nach der OP eingenommen? In Wochen:__________________ | (7) How many weeks did you take pain medication after the operation? |
| (8) Wie schnell nach der OP sind Sie zum Alltag zurückgekehrt? Das heißt.: (8a) Wie viele Tage brauchten Sie Hilfe beim Anziehen, Waschen oder Benutzen der Toilette? (8b) Wie viele Tage waren Sie bei den tagtäglichen Beschäftigungen im Haushalt eingeschränkt? (8c) Wie viele Tage waren Sie bei Ihren Hobbys oder anderen Freizeitbeschäftigungen, inklusive Sport, eingeschränkt? | (8) How quickly did you return to everyday life after the operation? Specifically, we wanted to know: (8a) How many days did you need help getting dressed, washing or using the toilet? (8b) How many days were you restricted from daily activities in the household? (8c) How many days were you restricted in your hobbies or other leisure activities, including sports? |
| (9) Wenn Sie in einer festen Partnerschaft zum Zeitpunkt der OP waren: (9a) Nach wie vielen Tagen/Wochen hatten Sie wieder Geschlechtsverkehr? (9b) Wie viele Tage/Wochen waren Sie beim Geschlechtsverkehr, nachdem Sie wieder damit begonnen hatten, eingeschränkt? (9c) Was war am ehesten der Grund für die Einschränkung beim Geschlechtsverkehr? □ Schmerzen □ sexuelle Lust □ Lubrikation (Feuchte) □ Orgasmus □ Angst | (9) If you were in a permanent partnership at the time of the operation: (9a) After how many days/weeks did you have sexual intercourse again? (9b) How many days/weeks were you restricted in sexual intercourse after starting again? (9c) What was most likely the reason for the restriction in sexual intercourse? □ pain □ sexual pleasure □ lubrication (moisture) □ orgasm □ fear |
| (10) Sind Sie mit dem kosmetischen Ergebnis der Operation zufrieden? Ja □ Nein □ (10a) Wenn nein: Was ist am ehesten die Ursache der Unzufriedenheit? Ort der Narben □ Anzahl der Narben □ die Länge der Narben □ Beschaffenheit der Narben □ Schmerzhafte/empfindliche Narben □ | (10) Are you satisfied with the cosmetic result of the operation? Yes □ No □ (10a) If not: What is most likely cause of the dissatisfaction? Location of scars □ number of scars □ length of scars □ Nature of the scars □ Painful/sensitive scars □ |
References
- Finks, J.F.; Osborne, N.H.; Birkmeyer, J.D. Trends in Hospital Volume and Operative Mortality for High-Risk Surgery. N. Engl. J. Med. 2011, 364, 2128–2137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birkmeyer, J.D.; Siewers, A.E.; Finlayson, E.V.; Stukel, T.A.; Lucas, F.L.; Batista, I.; Welch, H.G.; Wennberg, D.E. Hospital Volume and Surgical Mortality in the United States. N. Engl. J. Med. 2002, 346, 1128–1137. [Google Scholar] [CrossRef]
- Lawrie, T.A.; Liu, H.; Lu, D.; Dowswell, T.; Song, H.; Wang, L.; Shi, G. Robot-assisted surgery in gynaecology. Cochrane Database Syst. Rev. 2019, 4, CD011422. [Google Scholar] [CrossRef] [PubMed]
- Schollmeyer, T.; Elessawy, M.; Chastamouratidhs, B.; Alkatout, I.; Meinhold-Heerlein, I.; Mettler, L.; Jonat, W.; Weigel, M.T. Hysterectomy trends over a 9-year period in an endoscopic teaching center. Int. J. Gynaecol. Obstet. 2014, 126, 45–49. [Google Scholar] [CrossRef]
- Alkatout, I.; Mettler, L.; Maass, N.; Ackermann, J. Robotic surgery in gynecology. J. Turk. Ger. Gynecol. Assoc. 2016, 17, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Alkatout, I. An atraumatic retractor for interdisciplinary use in conventional laparoscopy and robotic surgery. Minim. Invasive Ther. Allied Technol. 2018, 27, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.; Lu, D.; Wang, L.; Shi, G.; Song, H.; Clarke, J. Robotic surgery for benign gynaecological disease. Cochrane Database Syst. Rev. 2012, 2, CD008978. [Google Scholar]
- Nicklin, J. The future of robotic-assisted laparoscopic gynaecologic surgery in Australia-A time and a place for everything. Aust. N. Z. J. Obstet. Gynaecol. 2017, 57, 493–498. [Google Scholar] [CrossRef]
- Kilic, G.S.; Moore, G.; Elbatanony, A.; Radecki, C.; Phelps, J.Y.; Borahay, M.A. Comparison of Perioperative Outcomes of Total Laparoscopic and Robotically Assisted Hysterectomy for Benign Pathology during Introduction of a Robotic Program. Obstet. Gynecol. Int. 2011, 2011. [Google Scholar] [CrossRef] [Green Version]
- Paraiso, M.F.; Ridgeway, B.; Park, A.J.; Jelovsek, J.E.; Barber, M.D.; Falcone, T.; Einarsson, J.I. A randomized trial comparing conventional and robotically assisted total laparoscopic hysterectomy. Am. J. Obstet. Gynecol. 2013, 208, 368-e1-7. [Google Scholar] [CrossRef]
- Margolis, M.K.; Vats, V.; Coyne, K.S.; Kelleher, C. Establishing the content validity of the King’s Health Questionnaire in men and women with overactive bladder in the US. Patient 2011, 4, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Cabases, J.; Rabin, R. Introduction, in Self-Reported Population Health: An International Perspective Based on EQ-5D; Szende, A., Janssen, B., Cabases, J., Eds.; Springer: Dordrecht, The Netherlands, 2014; pp. 1–6. [Google Scholar]
- Gerstenberger, E.P.; Rosen, R.C.; Brewer, J.V.; Meston, C.M.; Brotto, L.A.; Wiegel, M.; Sand, M. Sexual desire and the female sexual function index (FSFI): A sexual desire cutpoint for clinical interpretation of the FSFI in women with and without hypoactive sexual desire disorder. J. Sex Med. 2010, 7, 3096–3103. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, R.H.; Turk, D.C.; Wyrwich, K.W.; Beaton, D.; Cleeland, C.S.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Kerns, R.D.; Ader, D.N.; et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J. Pain 2008, 9, 105–121. [Google Scholar] [CrossRef] [PubMed]
- Oberski, D.L.; Hagenaars, J.A.; Saris, W.E. The latent class multitrait-multimethod model. Psychol. Methods 2015, 20, 422–443. [Google Scholar] [CrossRef]
- Gunther, V.; Malchow, B.; Schubert, M.; Andresen, L.; Jochens, A.; Jonat, W.; Mundhenke, C.; Alkatout, I. Impact of radical operative treatment on the quality of life in women with vulvar cancer—A retrospective study. Eur. J. Surg. Oncol. 2014, 40, 875–882. [Google Scholar] [CrossRef]
- Bauer, M.; Bohrer, H.; Aichele, G.; Bach, A.; Martin, E. Measuring patient satisfaction with anaesthesia: Perioperative questionnaire versus standardised face-to-face interview. Acta Anaesthesiol. Scand. 2001, 45, 65–72. [Google Scholar] [CrossRef] [Green Version]
- Clavien, P.A.; Barkun, J.; De Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; De Santibanes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [Green Version]
- Rosero, E.B.; Kho, K.A.; Joshi, G.P.; Giesecke, M.; Schaffer, J.I. Comparison of robotic and laparoscopic hysterectomy for benign gynecologic disease. Obstet. Gynecol. 2013, 122, 778–786. [Google Scholar] [CrossRef] [Green Version]
- Wright, J.D.; Ananth, C.V.; Lewin, S.N.; Burke, W.M.; Lu, Y.S.; Neugut, A.I.; Herzog, T.J.; Hershman, D.L. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA 2013, 309, 689–698. [Google Scholar] [CrossRef]
- Sarlos, D.; Kots, L.A. Robotic versus laparoscopic hysterectomy: A review of recent comparative studies. Curr. Opin. Obstet. Gynecol. 2011, 23, 283–288. [Google Scholar] [CrossRef] [Green Version]
- Berlit, S.; Tuschy, B.; Wuhrer, A.; Jurgens, S.; Buchweitz, O.; Kircher, A.T.; Sutterlin, M.; Lis, S.; Hornemann, A. Sexual functioning after total versus subtotal laparoscopic hysterectomy. Arch. Gynecol. Obstet. 2018, 298, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Alkatout, I. Communicative and ethical aspects of physician-patient relationship in extreme situations. Wien. Med. Wochenschr. 2015, 165, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Ercan, O.; Ozer, A.; Kostu, B.; Bakacak, M.; Kiran, G.; Avci, F. Comparison of postoperative vaginal length and sexual function after abdominal, vaginal, and laparoscopic hysterectomy. Int. J. Gynaecol. Obstet. 2016, 132, 39–41. [Google Scholar] [CrossRef] [PubMed]
- Bastu, E.; Yasa, C.; Dural, O.; Ozgor, B.Y.; Yilmaz, G.; Ugurlucan, F.G.; Buyru, F.; Banerjee, S. Comparison of 2 Methods of Vaginal Cuff Closure at Laparoscopic Hysterectomy and Their Effect on Female Sexual Function and Vaginal Length: A Randomized Clinical Study. J. Minim. Invasive Gynecol. 2016, 23, 986–993. [Google Scholar] [CrossRef]
- De La Cruz, J.F.; Myers, E.M.; Geller, E.J. Vaginal versus robotic hysterectomy and concomitant pelvic support surgery: A comparison of postoperative vaginal length and sexual function. J. Minim. Invasive Gynecol. 2014, 21, 1010–1014. [Google Scholar] [CrossRef]
- Alkatout, I.; Mettler, L.; Peters, G.; Noe, G.; Holthaus, B.; Jonat, W.; Schollmeyer, T. Laparoscopic hysterectomy and prolapse: A multiprocedural concept. JSLS 2014, 18, 89–101. [Google Scholar] [CrossRef] [Green Version]
- Lonnerfors, C.; Reynisson, P.; Persson, J. A randomized trial comparing vaginal and laparoscopic hysterectomy vs robot-assisted hysterectomy. J. Minim. Invasive Gynecol. 2015, 22, 78–86. [Google Scholar] [CrossRef]
- Lenihan, J.P., Jr.; Kovanda, C.; Seshadri-Kreaden, U. What is the learning curve for robotic assisted gynecologic surgery? J. Minim. Invasive. Gynecol. 2008, 15, 589–594. [Google Scholar] [CrossRef]
- Rajadurai, V.A.; Tan, J.; Salfinger, S.G.; Cohen, P.A. Outcomes in women undergoing robotic-assisted laparoscopic hysterectomy compared to conventional laparoscopic hysterectomy at a tertiary hospital in Western Australia. Aust. N. Z. J. Obstet. Gynaecol. 2017. [Google Scholar] [CrossRef] [Green Version]
- Seamon, L.G.; Fowler, J.M.; Richardson, D.L.; Carlson, M.J.; Valmadre, S.; Phillips, G.S.; Cohn, D.E. A detailed analysis of the learning curve: Robotic hysterectomy and pelvic-aortic lymphadenectomy for endometrial cancer. Gynecol. Oncol. 2009, 114, 162–167. [Google Scholar] [CrossRef]
- Pitter, M.C.; Anderson, P.; Blissett, A.; Pemberton, N. Robotic-assisted gynaecological surgery-establishing training criteria; minimizing operative time and blood loss. Int. J. Med. Robot. 2008, 4, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.M.; Wechter, M.E.; Geller, E.J.; Nguyen, T.V.; Visco, A.G. Hysterectomy rates in the United States, 2003. Obstet. Gynecol. 2007, 110, 1091–1095. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | CL (n = 99) | RALH (n = 56) | p-Value |
|---|---|---|---|
| Age (years), Mean | 49,00 | 49.09 | |
| Median (range) | 47.0 (42.0–54.0) | 47.0 (43.0–52.0) | 0.907 |
| BMI (kg/m2), Mean | 27.78 | 29.53 | |
| Median (range) | 26.66 (22.65–32.42) | 27.71 (24.16–31.98) | 0.265 |
| Operative time (min.), Mean | 162.73 | 131.31 | |
| Lenghts of stay (nights), Mean | 4.44 | 4.13 | |
| Median (range) | 4.0 (3.0–5.0) | 4.0 (4.0–4.0) | 0.514 |
| Uterine weight (g), Mean | 210.14 | 185.64 | |
| Median (range) | 150.0 (86.0–262.0) | 141.0 (94.0–206.25) | 0.804 |
| Indications | |||
| benign, n (%) | 73 (73.3%) | 48 (85.7%) | 0.083 |
| leiomyomas, n (%) | 43 (43.4%) | 28 (50.0%) | 0.431 |
| gynecologic (pre)cancer, n (%) | 26 (26.3%) | 9 (16.1%) | 0.145 |
| abnormal bleeding, n (%) | 9 (9.1%) | 6 (10.7%) | 0.743 |
| endometriosis, n (%) | 17 (17.2%) | 13 (23.2%) | 0.36 |
| other indications, n (%) | 4 (4.0%) | 1 (1.8%) | 0.654 |
| Complications Number (%) | CL | RALH | p-Value |
|---|---|---|---|
| 15 (15.2%) | 12 (21.4%) | 0.322 | |
| Intraoperative | 8 (8.1%) | 5 (8.9%) | 0.999 |
| Injuries of the urinary tract, n (%) | 4 (4.0%) | 2 (3.6%) | >0.999 |
| Injuries of the gastrointestinal tract, n (%) | 3 (3.0%) | 1 (1.8%) | >0.999 |
| Vascular injuries, n (%) | 1 (1.0%) | 3 (5.4%) | 0.135 |
| Other complications, n (%) | 1 (1.0%) | 0 | >0.999 |
| Postoperative | 8 (8.1%) | 9 (16.1%) | 0.126 |
| Revision surgery, n (%) | 2 (2.0%) | 1 (1.8%) | >0.999 |
| Wound complications, n (%) | 2 (2.0%) | 2 (3.6%) | 0.62 |
| Thromboembolic complications, n (%) | 0 | 1 (1.8%) | 0.361 |
| Mortality, n (%) | 0 | 0 | >0.999 |
| Other complications, n (%) | 5 (5.1%) | 5 (8.9%) | 0.497 |
| Postoperative | CL | RALH | p-Value |
|---|---|---|---|
| Pain score at week 1 (mean) | 3.26 (SD 2.809) | 2.73 (SD 2.136) | |
| Median (range) | 3.00 (0.75–5.00) | 3.00 (1.00–4.00) | 0.519 |
| Pain score- week 4 (mean) | 1.19 (SD 1.733) | 1.11 (SD 1.385) | |
| Median (range) | 0.00 (0.00–2.00) | 1.00 (0.00–2.00) | 0.693 |
| Intake of painkillers (days) (mean) | 11.92 (SD 43.043) | 8.44 (SD 10.874) | |
| Median (range) | 4.00 (1.00–7.00) | 4.00 (2.50–7.00) | 0.471 |
| Surgical Procedure | Total | ||||
|---|---|---|---|---|---|
| CL | RALH | ||||
| Satisfaction with the outcome of treatment | 1 | Number (Percentage) | 52 (70.3%) | 29 (64.4%) | 81 (68.1%) |
| 2 | Number (Percentage) | 15 (20.3%) | 13 (28.9%) | 28 (23.5%) | |
| 3 | Number (Percentage) | 5 (6.8%) | 3 (6.7%) | 8 (6.7%) | |
| 4 | Number (Percentage) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| 5 | Number (Percentage) | 1 (1.4%) | 0 (0.0%) | 1 (0.8%) | |
| 6 | Number (Percentage) | 1 (1.4%) | 0 (0.0%) | 1 (0.8%) | |
| Total | Number (Percentage) | 74 (100.0%) | 45 (100.0%) | 119 (100.0%) | |
| Statistical test | Chi-square test | 0.823 | |||
| Surgical Procedure | Total | Statistical Test | ||||
|---|---|---|---|---|---|---|
| CL | RALH | Chi-Square Test | ||||
| Total satisfaction | Number (Percentage) | 72 (97.3%) | 36 (80.0%) | 108 (90.8%) | ||
| Main cause of cosmetic dissatisfaction | Position of the incisions | Number (Percentage) | 0 (0.0%) | 2 (4.4%) | 2 (1.7%) | 0.002 |
| Number of scars | Number (Percentage) | 0 (0.0%) | 1 (2.2%) | 1 (0.8%) | ||
| Scar | Number (Percentage) | 1 (1.4%) | 6 (13.3%) | 7 (5.9%) | ||
| Painful/sensitive scars | Number (Percentage) | 1 (1.4%) | 0 (0.0%) | 1 (0.8%) | ||
| Total | Number (Percentage) | 74 (100.0%) | 45 (100.0%) | 119 (100.0%) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elessawy, M.; Schneekloth, S.; Günther, V.; Maass, N.; Mettler, L.; Alkatout, I. Postoperative Telephone-Based Questionnaire on Quality of Life after Robotic-Assisted Laparoscopic Hysterectomy versus Conventional Total Laparoscopic Hysterectomy. J. Clin. Med. 2020, 9, 2849. https://doi.org/10.3390/jcm9092849
Elessawy M, Schneekloth S, Günther V, Maass N, Mettler L, Alkatout I. Postoperative Telephone-Based Questionnaire on Quality of Life after Robotic-Assisted Laparoscopic Hysterectomy versus Conventional Total Laparoscopic Hysterectomy. Journal of Clinical Medicine. 2020; 9(9):2849. https://doi.org/10.3390/jcm9092849
Chicago/Turabian StyleElessawy, Mohamed, Sarah Schneekloth, Veronika Günther, Nicolai Maass, Liselotte Mettler, and Ibrahim Alkatout. 2020. "Postoperative Telephone-Based Questionnaire on Quality of Life after Robotic-Assisted Laparoscopic Hysterectomy versus Conventional Total Laparoscopic Hysterectomy" Journal of Clinical Medicine 9, no. 9: 2849. https://doi.org/10.3390/jcm9092849





