Blood Pressure Abnormalities Associated with Gut Microbiota-Derived Short Chain Fatty Acids in Children with Congenital Anomalies of the Kidney and Urinary Tract
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Biochemical Analysis
2.3. Office Blood Pressure and 24 h Ambulatory Blood Pressure Monitoring (ABPM)
2.4. Gas Chromatography-Flame Ionization Detector (GC-FID)
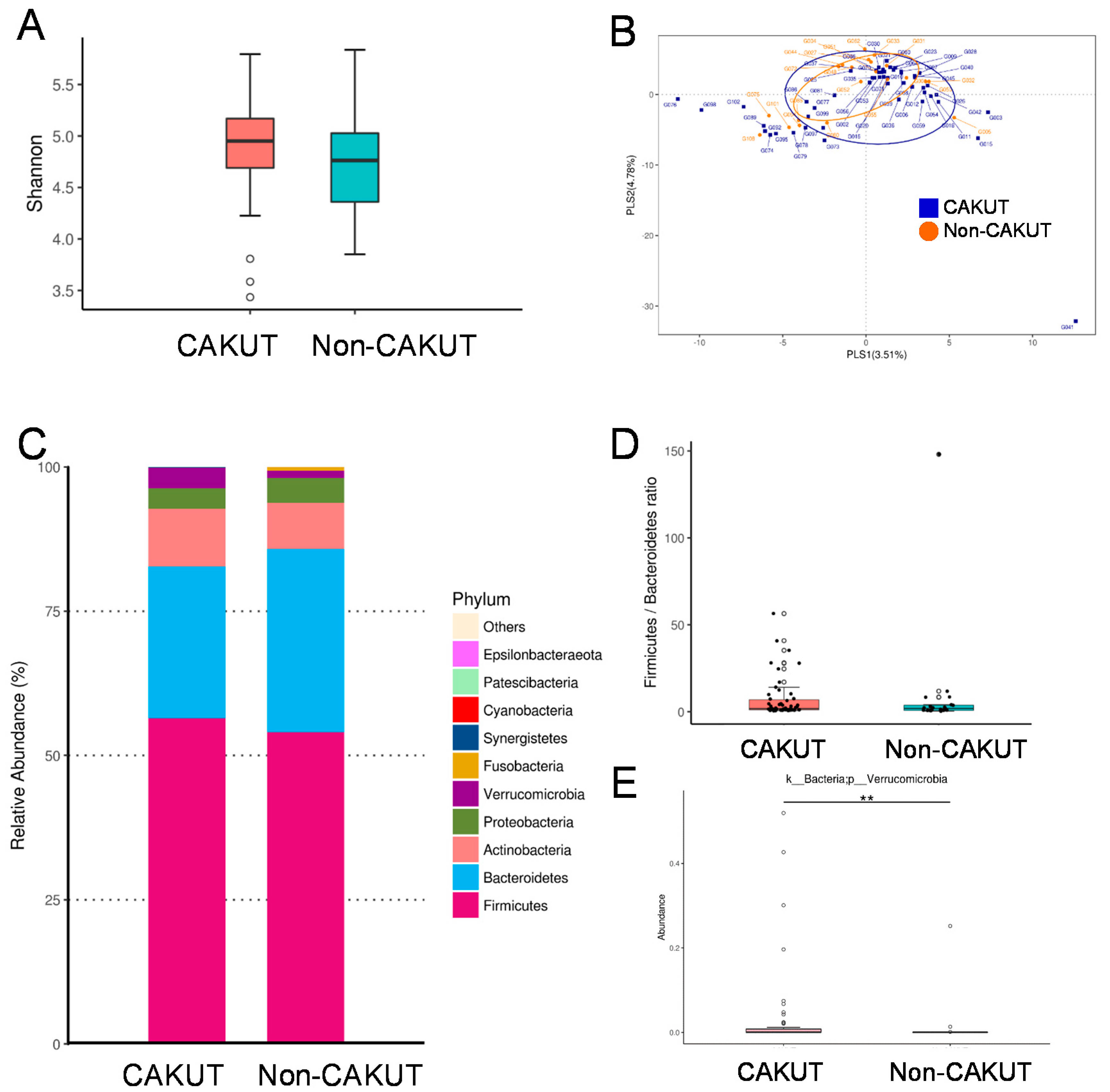
2.5. Analysis of Gut Microbiota Composition
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nicolaou, N.; Renkema, K.Y.; Bongers, E.M.; Giles, R.H.; Knoers, N.V. Genetic, environmental, and epigenetic factors involved in CAKUT. Nat. Rev. Nephrol. 2015, 11, 720–731. [Google Scholar] [CrossRef] [PubMed]
- Queisser-Luft, A.; Stolz, G.; Wiesel, A.; Schlaefer, K.; Spranger, J. Malformations in newborn: Results based on 30,940 infants and fetuses from the Mainz congenital birth defect monitoring system (1990–1998). Arch. Gynecol. Obstet. 2002, 266, 163. [Google Scholar] [CrossRef] [PubMed]
- Harambat, J.; van Stralen, K.J.; Kim, J.J.; Tizard, E.J. Epidemiology of chronic kidney disease in children. Pediatr. Nephrol. 2012, 27, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Saran, R.; Li, Y.; Robinson, B.; Ayanian, J.; Balkrishnan, R.; Bragg-Gresham, J.; Chen, J.T.; Cope, E.; Gipson, D.; He, K.; et al. US renal data system 2014 annual data report: Epidemiology of kidney disease in the United States. Am. J. Kidney Dis. 2015, 65, A7. [Google Scholar] [CrossRef] [PubMed]
- Chou, H.H.; Chiou, Y.Y.; Chiou, Y.H.; Tain, Y.L.; Wang, H.H.; Yu, M.C.; Hsu, C.C.; Lin, C.Y. Mortality Risks among Various Primary Renal Diseases in Children and Adolescents on Chronic Dialysis. J. Clin. Med. 2018, 7, 414. [Google Scholar] [CrossRef]
- Wuhl, E.; Van Stralen, K.J.; Verrina, E.; Bjerre, A.; Wanner, C.; Heaf, J.G.; Zurriaga, O.; Hoitsma, A.; Niaudet, P.; Palsson, R.; et al. Timing and outcome of renal replacement therapy in patients with congenital malformations of the kidney and urinary tract. Clin. J. Am. Soc. Nephrol. 2013, 8, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Flynn, J.T.; Mitsnefes, M.; Pierce, C.; Cole, S.R.; Parekh, R.S.; Furth, S.L.; Warady, B.A. Chronic Kidney Disease in Children Study Group: Blood pressure in children with chronic kidney disease: A report from the Chronic Kidney Disease in Children study. Hypertension 2008, 52, 631–637. [Google Scholar] [CrossRef]
- Hsu, C.N.; Lu, P.C.; Lo, M.H.; Lin, I.C.; Chang-Chien, G.P.; Lin, S.; Tain, Y.L. Gut Microbiota-Dependent Trimethylamine N-Oxide Pathway Associated with Cardiovascular Risk in Children with Early-Stage Chronic Kidney Disease. Int. J. Mol. Sci. 2018, 19, 3699. [Google Scholar] [CrossRef]
- Wühl, E.; Trivelli, A.; Picca, S.; Litwin, M.; Peco-Antic, A.; Zurowska, A.; Testa, S.; Jankauskiene, A.; Emre, S.; Caldas-Afonso, A.; et al. ESCAPE Trial Group: Strict blood-pressure control and progression of renal failure in children. N. Engl. J. Med. 2009, 361, 1639–1650. [Google Scholar]
- Mitsnefes, M.M. Cardiovascular disease in children with chronic kidney disease. J. Am. Soc Nephrol. 2012, 23, 578–585. [Google Scholar] [CrossRef]
- Urbina, E.M.; Williams, R.V.; Alpert, B.S.; Collins, R.T.; Daniels, S.R.; Hayman, L.; Jacobson, M.; Mahoney, L.; Mietus-Snyder, M.; Rocchini, A.; et al. American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young. American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young. Noninvasive assessment of subclinical atherosclerosis in children and adolescents: Recommendations for standard assessment for clinical research: A scientific statement from the American Heart Association. Hypertension 2009, 54, 919–950. [Google Scholar] [PubMed]
- Ingelfinger, J.R.; Kalantar-Zadeh, K.; Schaefer, F.; World Kidney Day Steering Committee. World Kidney Day 2016: Averting the legacy of kidney disease-focus on childhood. Pediatr. Nephrol. 2016, 31, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Tain, Y.L.; Hsu, C.N. Developmental Origins of Chronic Kidney Disease: Should We Focus on Early Life? Int. J. Mol. Sci. 2017, 18, 381. [Google Scholar] [CrossRef] [PubMed]
- Luyckx, V.A.; Bertram, J.F.; Brenner, B.M.; Fall, C.; Hoy, W.E.; Ozanne, S.E.; Vikse, B.E. Effect of fetal and child health on kidney development and long-term risk of hypertension and kidney disease. Lancet 2013, 382, 273–283. [Google Scholar] [CrossRef] [Green Version]
- Tain, Y.L.; Luh, H.; Lin, C.Y.; Hsu, C.N. Incidence and Risks of Congenital Anomalies of Kidney and Urinary Tract in Newborns: A Population-Based Case-Control Study in Taiwan. Medicine 2016, 95, e2659. [Google Scholar] [CrossRef] [PubMed]
- Jovanovich, A.; Isakova, T.; Stubbs, J. Microbiome and Cardiovascular Disease in CKD. Clin. J. Am. Soc. Nephrol. 2018, 13, 1598–1604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meijers, B.; Jouret, F.; Evenepoel, P. Linking gut microbiota to cardiovascular disease and hypertension: Lessons from chronic kidney disease. Pharmacol. Res. 2018, 133, 101–107. [Google Scholar] [CrossRef] [Green Version]
- Felizardo, R.J.F.; Watanabe, I.K.M.; Dardi, P.; Rossoni, L.V.; Câmara, N.O.S. The interplay among gut microbiota, hypertension and kidney diseases: The role of short-chain fatty acids. Pharmacol. Res. 2019, 141, 366–377. [Google Scholar] [CrossRef]
- Yang, T.; Santisteban, M.M.; Rodriguez, V.; Li, E.; Ahmari, N.; Carvajal, J.M.; Zadeh, M.; Gong, M.; Qi, Y.; Zubcevic, J.; et al. Gut dysbiosis is linked to hypertension. Hypertension 2015, 65, 1331–1340. [Google Scholar] [CrossRef]
- Al Khodor, S.; Reichert, B.; Shatat, I.F. The microbiome and blood pressure: Can microbes regulate our blood pressure? Front. Pediatr. 2017, 5, 138. [Google Scholar] [CrossRef]
- Chambers, E.S.; Preston, T.; Frost, G.; Morrison, D.J. Role of Gut Microbiota-Generated Short-Chain Fatty Acids in Metabolic and Cardiovascular Health. Curr. Nutr. Rep. 2018, 7, 198–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levin, A.; Stevens, P.E.; Bilous, R.W.; Coresh, J.; De Francisco, A.L.M.; De Jong, P.E.; Griffith, K.E.; Hemmelgarn, B.R.; Iseki, K.; Lamb, E.J. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Schwartz, G.J.; Muñoz, A.; Schneider, M.F.; Mak, R.H.; Kaskel, F.; Warady, B.A.; Furth, S.L. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 2009, 20, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Renkema, K.Y.; Winyard, P.J.; Skovorodkin, I.N.; Levtchenko, E.; Hindryckx, A.; Jeanpierre, C.; Weber, S.; Salomon, R.; Antignac, C.; Vainio, S.; et al. Novel perspectives for investigating congenital anomalies of the kidney and urinary tract (CAKUT). Nephrol. Dial. Transplant. 2011, 26, 3843–3851. [Google Scholar] [CrossRef] [PubMed]
- Lin, I.C.; Hsu, C.N.; Lo, M.H.; Chien, S.J.; Tain, Y.L. Low urinary citrulline/arginine ratio associated with blood pressure abnormalities and arterial stiffness in childhood chronic kidney disease. J. Am. Soc. Hypertens. 2016, 10, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Wuhl, E.; Witte, K.; Soergelm, M.; Mehls, O.; Schaefer, F.; German Working Group on Pediatric Hypertension. Distribution of 24-h ambulatory blood pressure in children: Normalized reference values and role of body dimensions. J. Hypertens. 2002, 20, 1995–2007. [Google Scholar] [CrossRef] [PubMed]
- Kollias, A.; Stergiou, G.S.; Dolan, E.; O’Brien, E. Ambulatory arterial stiffness index: A systematic review and meta-analysis. Atherosclerosis 2012, 224, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.N.; Lin, Y.L.; Hou, C.Y.; Tain, Y.L. Maternal Administration of Probiotic or Prebiotic Prevents Male Adult Rat Offspring against Developmental Programming of Hypertension Induced by High Fructose Consumption in Pregnancy and Lactation. Nutrients 2018, 10, 1229. [Google Scholar] [CrossRef]
- Hsu, C.N.; Chang-Chien, G.P.; Lin, S.; Lo, M.H.; Tain, Y.L. Targeting on gut microbial metabolite trimethylamine-N-oxide (TMAO) and short chain fatty acid to prevent maternal high-fructose diet-induced developmental programming of hypertension in adult male offspring. Mol. Nutr. Food Res. 2019, in press. [Google Scholar] [CrossRef]
- Fisher, R.A. The use of multiple measurements in taxonomic problems. Ann. Eugenics. 1936, 7, 179–188. [Google Scholar] [CrossRef]
- Chou, H.H.; Lin, C.Y.; Chiou, Y.H.; Tain, Y.L.; Wang, Y.F.; Wang, H.H.; Chiou, Y.Y. Clinical characteristics and prevalence of complications of chronic kidney disease in children: The Taiwan Pediatric Renal Collaborative study. Pediatr. Nephrol. 2016, 31, 1113–1120. [Google Scholar] [CrossRef] [PubMed]
- Ardissino, G.; Daccò, V.; Testa, S.; Bonaudo, R.; Claris-Appiani, A.; Taioli, E.; Marra, G.; Edefonti, A.; Fabio Sereni on Behalf of the ItalKid Project. Epidemiology of chronic renal failure in children: Data from the ItalKid project. Pediatrics 2003, 111, e382–e387. [Google Scholar] [CrossRef] [PubMed]
- Staples, A.O.; Greenbaum, L.A.; Smith, J.M.; Gipson, D.S.; Filler, G.; Warady, B.A.; Martz, K.; Wong, C.S. Association between clinical risk factors and progression of chronic kidney disease in children. Clin. J. Am. Soc. Nephrol. 2010, 5, 2172–2179. [Google Scholar] [CrossRef] [PubMed]
- Chiou, Y.Y.; Lin, C.Y.; Chen, M.J.; Chiou, Y.H.; Wang, Y.F.; Wang, H.H.; Tain, Y.L.; Chou, H.H. Etiology and pediatric chronic kidney disease progression: Taiwan Pediatric Renal Collaborative Study. J. Formos. Med. Assoc. 2016, 115, 752–763. [Google Scholar] [CrossRef] [PubMed]
- Cani, P.D.; de Vos, W.M. Next-Generation Beneficial Microbes: The Case of Akkermansia muciniphila. Front. Microbiol. 2017, 8, 1765. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhao, F.; Wang, Y.; Chen, J.; Tao, J.; Tian, G.; Wu, S.; Liu, W.; Cui, Q.; Geng, B. Gut microbiota dysbiosis contributes to the development of hypertension. Microbiome 2017, 5, 14. [Google Scholar] [CrossRef] [PubMed]
- Pluznick, J.L. Microbial short chain fatty acids and blood pressure regulation. Curr. Hypertens. Rep. 2017, 19, 25. [Google Scholar] [CrossRef]
- Pluznick, J.L.; Protzko, R.J.; Gevorgyan, H.; Peterlin, Z.; Sipos, A.; Han, J.; Brunet, I.; Wan, L.X.; Rey, F.; Wang, T.; et al. Olfactory receptor responding to gut microbiota-derived signals plays a role in renin secretion and blood pressure regulation. Proc. Natl. Acad. Sci. USA 2013, 110, 4410–4415. [Google Scholar] [CrossRef] [Green Version]
- Bier, A.; Braun, T.; Khasbab, R.; Di Segni, A.; Grossman, E.; Haberman, Y.; Leibowitz, A. A High Salt Diet Modulates the Gut Microbiota and Short Chain Fatty Acids Production in a Salt-Sensitive Hypertension Rat Model. Nutrients 2018, 10, 1154. [Google Scholar] [CrossRef]
- Reichardt, N.; Duncan, S.H.; Young, P.; Belenguer, A.; McWilliam Leitch, C.; Scott, K.P.; Flint, H.J.; Louis, P. Phylogenetic distribution of three pathways for propionate production within the human gut microbiota. ISME J. 2014, 8, 1323–1335. [Google Scholar] [CrossRef] [Green Version]
- Ríos-Covián, D.; Ruas-Madiedo, P.; Margolles, A.; Gueimonde, M.; de Los Reyes-Gavilán, C.G.; Salazar, N. Intestinal Short Chain Fatty Acids and their Link with Diet and Human Health. Front. Microbiol. 2016, 7, 185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, T.; Magee, K.L.; Colon-Perez, L.M.; Larkin, R.; Liao, Y.S.; Balazic, E.; Cowart, J.R.; Arocha, R.; Redler, T.; Febo, M.; et al. Impaired butyrate absorption in the proximal colon, low serum butyrate and diminished central effects of butyrate on blood pressure in spontaneously hypertensive rats. Acta Physiol. 2019, 226, e13256. [Google Scholar] [CrossRef] [PubMed]
- Meijers, B.; Evenepoel, P.; Anders, H.J. Intestinal microbiome and fitness in kidney disease. Nat. Rev. Nephrol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Chen, D.Q.; Chen, L.; Liu, J.R.; Vaziri, N.D.; Guo, Y.; Zhao, Y.Y. Microbiome-metabolome reveals the contribution of gut-kidney axis on kidney disease. J. Transl. Med. 2019, 17, 5. [Google Scholar] [CrossRef] [PubMed]

| Group | CAKUT | Non-CAKUT | ||
|---|---|---|---|---|
| N = 57 | N = 21 | |||
| Children | Adolescents | Children | Adolescents | |
| N = 39 | N = 18 | N = 6 | N = 15 | |
| Gender: M:F | 24:15 | 11:7 | 5:1 | 9:6 |
| CKD staging | ||||
| Stage G1 | 33 | 6 | 5 | 7 |
| Stage G2 | 3 | 9 | 0 | 5 |
| Stage G3 | 3 | 2 | 1 | 3 |
| Stage G4 | 0 | 1 | 0 | 0 |
| Age, years | 7.5 (5.5–10.3) | 15.8 (14.1–17.5) a | 10.2 (7.9–11.4) | 15.7 (13.9–16.9) a |
| Body height, percentile | 50 (15–75) | 50 (25–77.5) | 25 (3–58.8) | 25 (3–50) |
| Body weight, percentile | 25 (15–75) | 50 (12–85) | 25 (3–85) | 25 (15–85) |
| Systolic blood pressure, mmHg | 105 (101–113) | 121 (111–130) a | 114 (105–119) | 124 (112–136) |
| Diastolic blood pressure, mmHg | 69 (64–73) | 74 (71–82) a | 75 (63–82) | 70 (64–78) |
| Body mass index, kg·m−2 | 15.6 (14.7–17.7) | 20.8 (17.8–24.8) a | 18.3 (13.9–23.2) | 20.3 (18.3–23.6) |
| Hypertension (by office BP) | 12 (30%) | 6 (33%) | 5 (83%) b | 6 (40%) |
| Blood urea nitrogen, mg/dL | 13 (10–16) | 13 (12–15) | 14 (11–20) | 12 (11–15) |
| Creatinine, mg/dL | 0.5 (0.42–0.56) | 0.86 (0.64–0.97) a | 0.37 (0.19–0.75) | 0.73 (0.58–1) a |
| eGFR, mL/min/1.73 m2 | 104 (96–116) | 82 (71–101) a | 136 (103–393) b | 88 (71–113) a |
| CKD progression | 2 (5.1%) | 7 (38.9%) a | 1 (16.7%) | 5 (33.3%) |
| Urine total protein-to-creatinine ratio, mg/g | 49 (34–72) | 71 (29–172) | 2364 (709–12,293) b | 273 (51–1282) |
| Hemoglobin, g/dL | 13.4 (12.8–14) | 14.2 (12.2–16.2) | 13.4 (12.7–14.5) | 12.9 (11.9–14.2) |
| Hematocrit, % | 39.4 (37.9–41.3) | 42.2 (37.1–46.1) | 38.8 (37.2–40.3) | 38.1 (36–41.6) |
| Total cholesterol, mg/dL | 174 (155–194) | 146 (130–166) a | 239 (158–353) | 185 (132–207) |
| LDL, mg/dL | 89 (74–110) | 80 (59–99) | 140 (92–252) b | 96 (69–129) |
| Triglyceride, mg/dL | 61 (43–87) | 65 (51–106) | 98 (91–159) b | 66 (45–156) |
| Uric acid, mg/dL | 4.8 (3.9–5.4) | 5.9 (5.5–6.8) a | 7.6 (4.1–8.7) | 6.9 (5.2–9) |
| Sodium, mEq/L | 141 (139–142) | 142 (140–143) | 141 (137–142) | 140 (140–142) |
| Potassium, mEq/L | 4.4 (4.3–4.7) | 4.4 (4.2–4.6) | 4.2 (3.6–4.9) | 4.4 (4–4.7) |
| Calcium, mg/dL | 9.9 (9.7–10.1) | 9.9 (9.5–10.2) | 8.5 (7.3–9.8) b | 9.6 (9.2–9.6) |
| Phosphate, mg/dL | 5 (4.7–5.3) | 4.5 (4.1–4.9) a | 4.5 (4.1–4.7) b | 4.3 (3.9–4.4) |
| Group | CAKUT | Non-CAKUT |
|---|---|---|
| 24 h ABPM | N = 37 | N = 18 |
| Abnormal ABPM profile (with any of the following abnormalities) | 24 (65%) | 14 (78%) |
| Average 24 h BP >95th percentile | 7 (19%) | 7 (39%) |
| Average daytime BP >95th percentile | 8 (22%) | 8 (44%) |
| Average nighttime >95th percentile | 7 (19%) | 8 (44%) * |
| BP load ≥25% | 16 (43%) | 14 (78%) * |
| Nocturnal decrease of BP <10% | 20 (54%) | 9 (50%) |
| Arterial stiffness assessment | ||
| AASI | 0.35 (0.22–0.46) | 0.38 (0.25–0.49) |
| Plasma Level | CAKUT | Non-CAKUT |
|---|---|---|
| Acetate, μM | 56.4 (48.5–68.1) | 57.9 (46–83.4) |
| Propionate, μM | 1.8 (1.5–2.2) | 2.5 (1.6–3.3) * |
| Butyrate, μM | 1.4 (1.1–1.7) | 1.8 (1.2–2.2) |
| BP | n | Acetate | Propionate | Butyrate |
|---|---|---|---|---|
| 24 h BP | ||||
| Abnormal | 14 | 65.7 (49.4–73.5) | 2.4 (1.6–3.4) * | 1.9 (1.2–2.6) * |
| Normal | 40 | 56.1 (46–66.6) | 1.9 (1.5–2.2) | 1.5 (1.1–1.6) |
| Daytime BP | ||||
| Abnormal | 16 | 65.7 (47.3–77.2) | 2.4 (1.6–3.3) * | 1.8 (1.2–2.4) * |
| Normal | 38 | 56.1 (45.5–65.7) | 1.9 (1.5–2.2) | 1.4 (1.1–1.6) |
| Nighttime BP | ||||
| Abnormal | 15 | 68.1 (50.5–79.1) | 2.5 (1.6–3.5) * | 1.9 (1.2–2.5) * |
| Normal | 39 | 55.8 (45.9–65.3) | 1.8 (1.5–2.2) | 1.4 (1.1–1.6) |
| BP load | ||||
| Abnormal | 30 | 59.5 (46.1–73.5) | 2.2 (1.6–2.8) * | 1.4 (1.1–1.9) |
| Normal | 24 | 52.5 (46.2–65.2) | 1.8 (1.4–2.1) | 1.5 (1.2–1.6) |
| Night dipping | ||||
| Abnormal | 29 | 58.9 (48–75.3) | 2 (1.6–2.6) | 1.3 (0.8–1.7) |
| Normal | 25 | 55.8 (44.5–66.2) | 1.8 (1.5–2.4) | 1.5 (1.3–1.9) |
| ABPM profile | ||||
| Abnormal | 38 | 59 (46.4–68.6) | 2 (1.7–2.7) | 1.4 (1–1.8) |
| Normal | 16 | 54.2 (42.7–64.5) | 1.8 (1.3–2.2) | 1.5 (1.3–1.8) |
| Office BP | ||||
| Abnormal | 29 | 54.3 (49.4–68.6) | 2 (1.7–2.7) | 1.5 (1.2–1.9) |
| Normal | 47 | 56.9 (46.5–71.5) | 1.8 (1.5–2.2) | 1.4 (1–1.7) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, C.-N.; Lu, P.-C.; Hou, C.-Y.; Tain, Y.-L. Blood Pressure Abnormalities Associated with Gut Microbiota-Derived Short Chain Fatty Acids in Children with Congenital Anomalies of the Kidney and Urinary Tract. J. Clin. Med. 2019, 8, 1090. https://doi.org/10.3390/jcm8081090
Hsu C-N, Lu P-C, Hou C-Y, Tain Y-L. Blood Pressure Abnormalities Associated with Gut Microbiota-Derived Short Chain Fatty Acids in Children with Congenital Anomalies of the Kidney and Urinary Tract. Journal of Clinical Medicine. 2019; 8(8):1090. https://doi.org/10.3390/jcm8081090
Chicago/Turabian StyleHsu, Chien-Ning, Pei-Chen Lu, Chih-Yao Hou, and You-Lin Tain. 2019. "Blood Pressure Abnormalities Associated with Gut Microbiota-Derived Short Chain Fatty Acids in Children with Congenital Anomalies of the Kidney and Urinary Tract" Journal of Clinical Medicine 8, no. 8: 1090. https://doi.org/10.3390/jcm8081090






