A Systematic Review and Meta-Analysis of Anterolateral Thigh Flap Outcomes in High-Risk Diabetic Foot Reconstruction
Abstract
1. Introduction
- To determine the pooled flap survival rate, categorized as complete survival, partial necrosis, or total failure.
- To synthesize data on wound-healing parameters.
- To determine the pooled incidence of postoperative complications.
- To evaluate intraoperative variability and technical flap characteristics.
- To assess the long-term outcomes, such as ulcer recurrence, mortality, and return to ambulation.
- To report available data on patient-reported quality of life.
2. Materials and Methods
2.1. Study Eligibility
- Adult patients (aged ≥ 18 years) with a diagnosis of diabetes mellitus presenting with foot or ankle defects requiring surgical reconstruction.
- Evaluated the use of the anterolateral thigh free flap for reconstruction. Eligible studies included those that either:
- ○
- Directly compared the ALT free flap to other free tissue transfers.
- ○
- Reported on a single-arm case series of ALT flaps with at least five patients.
- Eligible study designs included randomized controlled trials (RCTs), prospective and retrospective cohort studies, case–control studies, and comparative or single-arm case series (as defined above).
- Reported on at least one of the predefined primary outcomes.
- Published in the English language (or had a full English translation available), with no restrictions placed on the date of publication.
- Focused on non-diabetic wound etiologies (e.g., acute trauma, malignancy) where data for the diabetic subgroup could not be isolated.
- Evaluated reconstruction with non-microvascular techniques, such as local pedicled flaps or skin grafts, microsurgical reconstruction without using the ALT flap.
- Were case reports with fewer than five patients, technical notes lacking clinical outcome data, narrative reviews, editorials, letters, or conference abstracts without a corresponding full-text publication.
- Reported on reconstructions for anatomical sites other than the lower limb.
2.2. Search Strategy
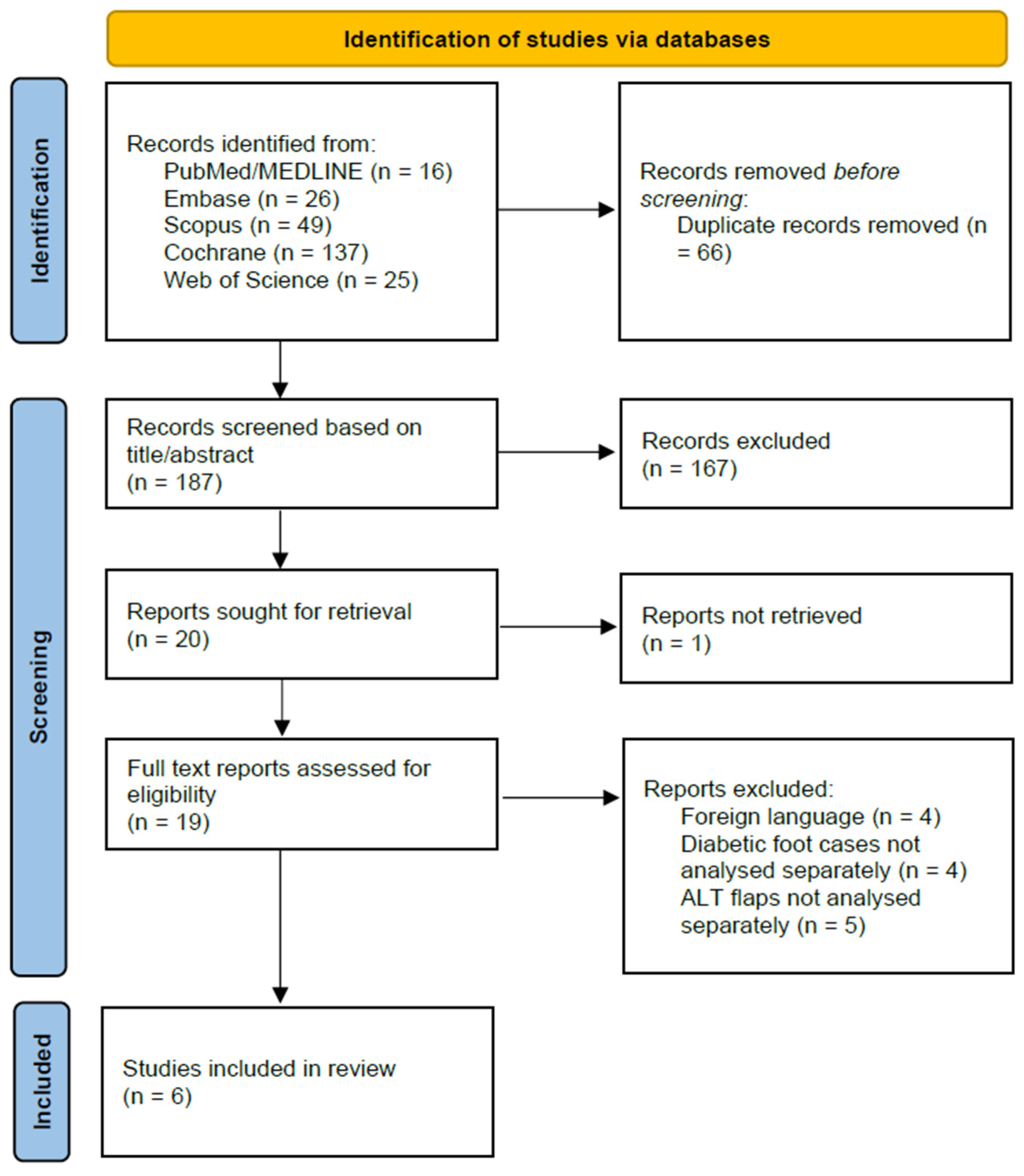
2.3. Study Selection
2.4. Data Extraction
- Study Characteristics: First author, year of publication, country of origin, study design, and total sample size.
- Population Demographics: Mean patient age, mean Glycated Hemoglobin (HbA1c), prevalence of key comorbidities (chronic heart disease, chronic kidney disease, peripheral artery disease, smoker status, osteomyelitis), and anatomical location of the defect
- Surgical Details: Mean flap size, pedicle length, number of perforators detected, type of microvascular anastomosis, and the recipient vessels used.
- Postoperative Outcomes: Rates of complete and partial flap necrosis, incidence of complications (including infection and vascular compromise), surgical revision rates, and the mean length of hospital stay.
- Long-Term Outcomes: Mean duration of follow-up, rates of ulcer recurrence and mortality, wound healing metrics (including the percentage of healed wounds and the mean time to complete healing), functional outcomes (such as the number of patients who achieved ambulation), and any patient-reported quality of life measures.
2.5. Risk of Bias Assessment
2.6. Statistical Analysis
3. Results
3.1. Study Identification
3.2. Study Characteristics
| First Author and Year of Study | Sample Size | Study Design | Inclusion Criteria | Age Mean | Outcome | Follow-Up Mean (Months) | Minors |
|---|---|---|---|---|---|---|---|
| Kim 2007 [42] | 16 | Unspecified | Diabetic feet reconstructed with free flaps | 62.8 | Complete necrosis: 6.25% Partial necrosis: 25% Necrosed area <10% of flap area in all cases of partial flap necrosis. | N/A | 7 |
| Hong 2006 [41] | 71 | Retrospective cohort | Diabetic patients with infected foot ulcers Reconstruction with the ALT free-flap | 51.4 | Complete necrosis: 1.4% Partial necrosis: 5.6% Unassisted bipedal gait: 95.7% | 11 | 7 |
| Hong 2005 [40] | 28 | Retrospective cohort | Chronic osteomyelitis of the lower extremity Reconstruction with anterolateral thigh perforator flaps. | 42.8 | Complete necrosis: 0% Partial necrosis: 7.1% | 18.2 | 9 |
| Kadam 2016 [43] | 26 | Retrospective cohort | Trophic ulcers of the insensate sole Microsurgical reconstruction with free-flaps | 44.69 | Flaps used: ALT flap (n = 18) Radial artery forearm flap (n = 4) Gracilis flap (n = 4) Complete necrosis: 0% Partial necrosis: 3.8% | 48 | 6 |
| Yang 2024 [44] | 83 | Retrospective cohort with matched controls | Inclusion Criteria for Diabetic Patients: (1) Diagnosis of Type 2 Diabetes Mellitus (2) Wagner grade ≥ 2 (3) Soft tissue defect of the foot with exposed wounds of important tissues such as bones, nerves, and tendons (4) Limb salvage patients undergoing prosthesis using flap technique Inclusion Criteria for Non-Diabetic Patients: (1) The patient’s age, defect site, defect size, and severity were similar to those of diabetic foot patients (2) Wound repair using ALT | 56.5 | Diabetic Foot Group: Complete necrosis: 5% Partial necrosis: 10% Non-Diabetic Foot Group: Complete necrosis: 0% Partial necrosis: 2.3% (p = 0.019) | 27.4 | 16 |
| Wen 2025 [45] | 48 | Retrospective cohort with matched controls | (1) Age range of 21–90 years; (2) Diagnosis of Diabetes Mellitus, either type 1 or type 2; (3) Patients exhibiting open lesions in the foot and ankle region, classified as Meggitt-Wagner grade 3 or 4. | 46.1 | Complete necrosis: 8.3% ALT group wound healing: 33.7 days Control group (sharp debridement and wound dressing) wound healing: 69.29 days (p < 0.001) | 6 | 16 |
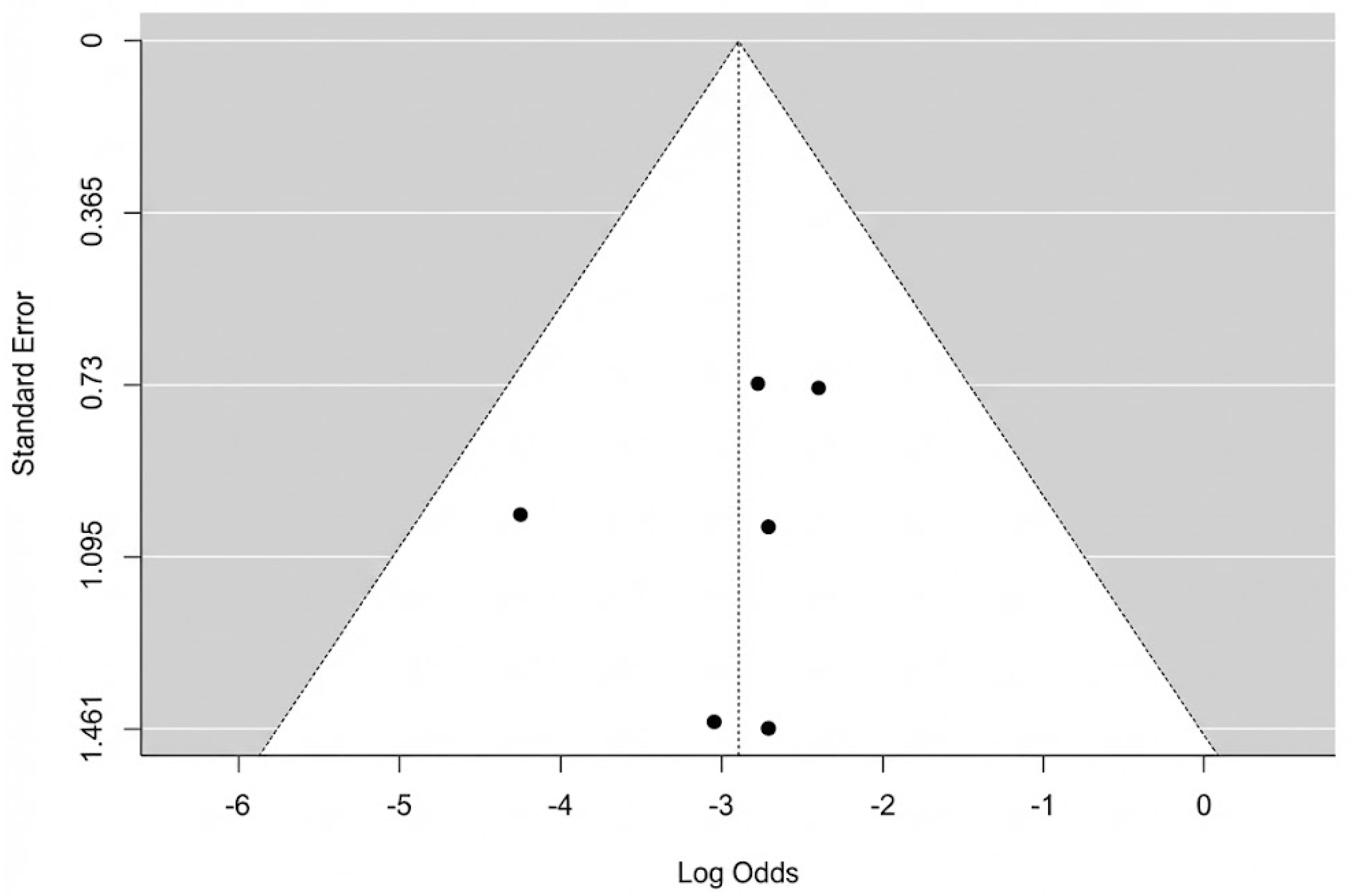
3.3. Risk of Bias
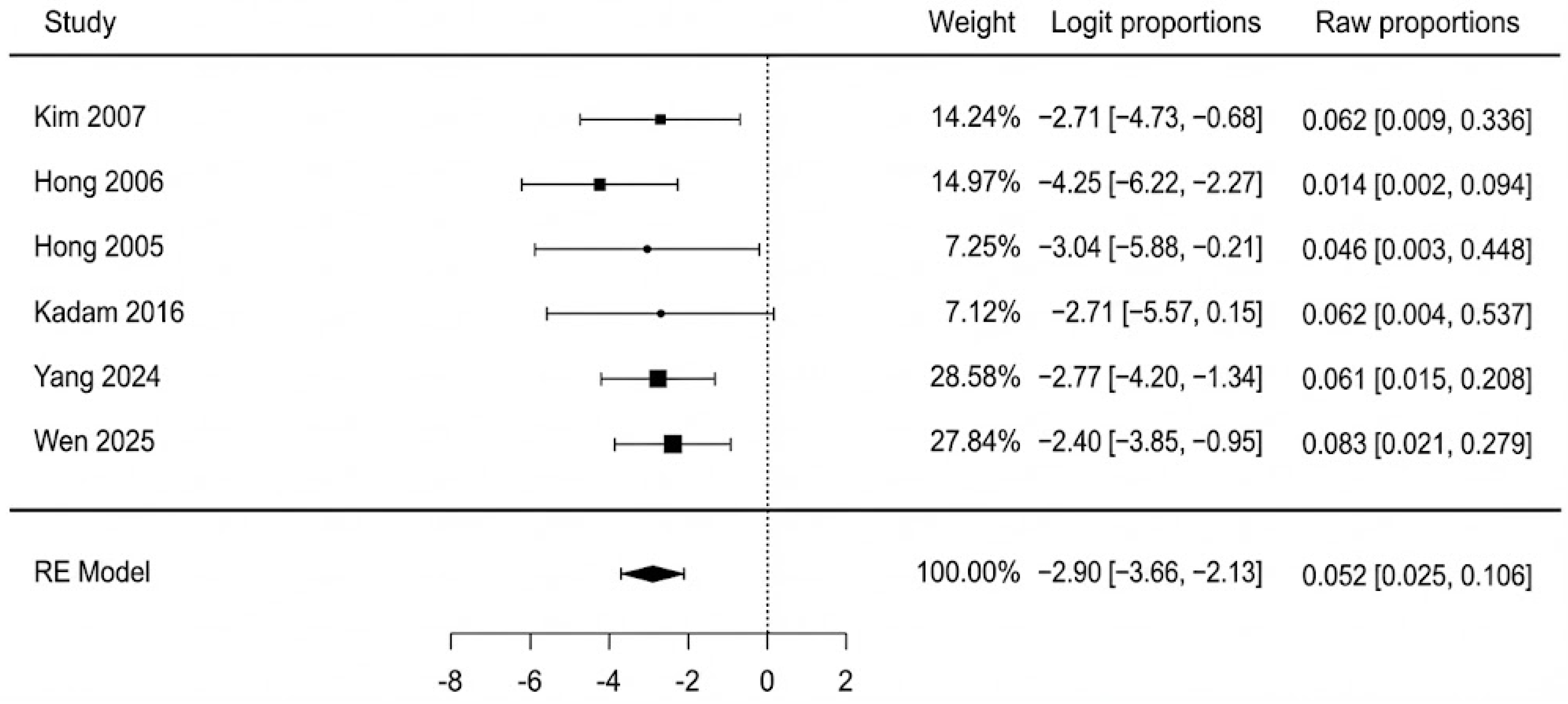
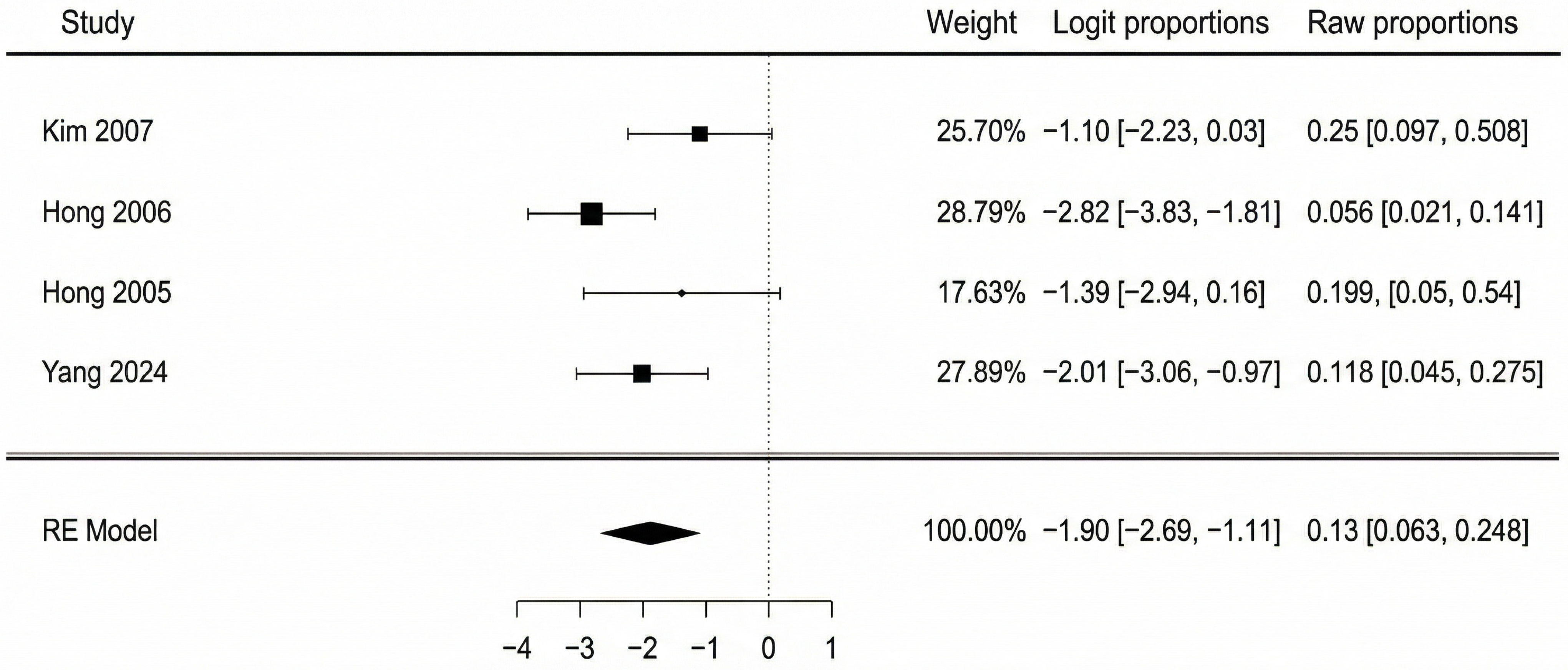
3.4. Meta-Analysis of Primary Outcome
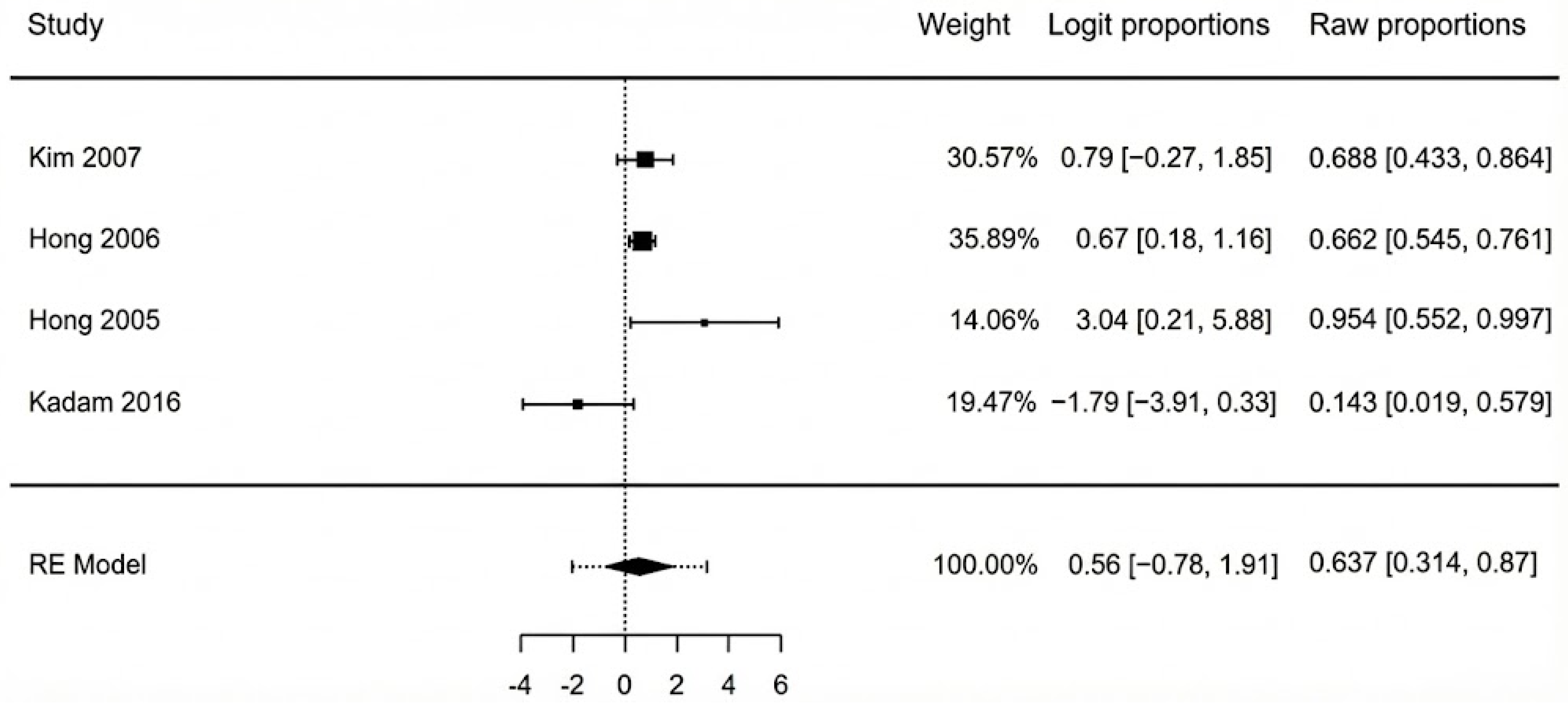
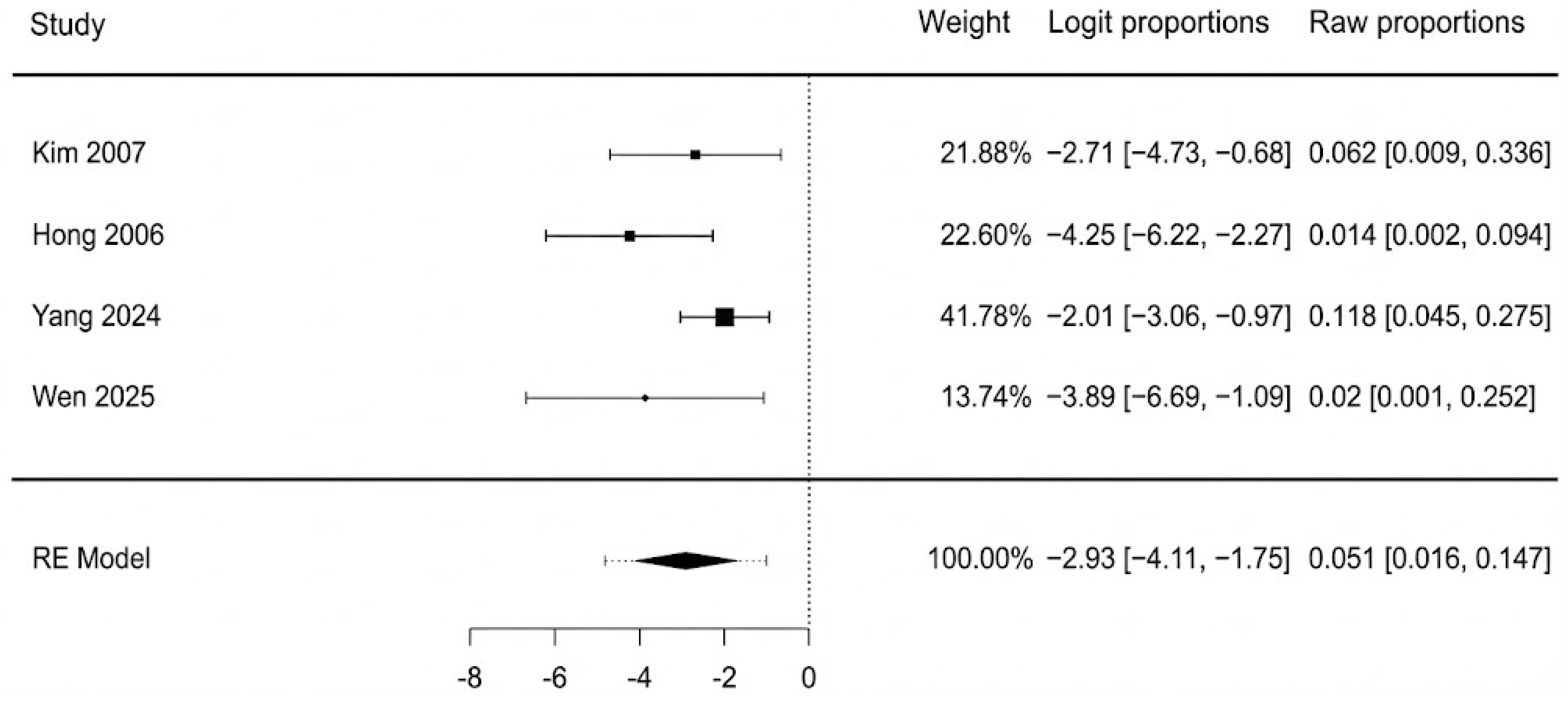
3.5. Meta-Analysis of Secondary Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AOFAS | American Orthopaedic Foot and Ankle Society |
| ALT | Anterolateral thigh |
| ASAMI | Association for the Study and Application of the Methods of Ilizarov |
| CKD | Chronic kidney disease |
| DFU | Diabetic foot ulcer |
| eGFR | Estimated glomerular filtration rate |
| HbA1c | Glycated hemoglobin |
| MeSH | Medical Subject Headings |
| MINORS | Methodological Index for Non-Randomized Studies |
| MMP | Matrix metalloproteinase |
| PAD | Peripheral arterial disease |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROM | Patient-reported outcome measure |
| RCT | Randomized controlled trial |
| RE | Random-effect |
Appendix A
- Embase
- 2.
- Scopus
- 3.
- Cochrane Library
- 4.
- Web of Science Core Collection
References
- Jang, W.; Kim, S.; Son, Y.; Kim, S.; Kim, H.J.; Jo, H.; Park, J.; Lee, K.; Lee, H.; A Tully, M.; et al. Prevalence, Awareness, Treatment, and Control of Type 2 Diabetes in South Korea (1998 to 2022): Nationwide Cross-Sectional Study. JMIR Public Health Surveill. 2024, 10, e59571. [Google Scholar] [CrossRef] [PubMed]
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Xu, Y.; Pan, X.; Xu, J.; Ding, Y.; Sun, X.; Song, X.; Ren, Y.; Shan, P.F. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci. Rep. 2020, 10, 14790. [Google Scholar] [CrossRef]
- Standl, E.; Khunti, K.; Hansen, T.B.; Schnell, O. The global epidemics of diabetes in the 21st century: Current situation and perspectives. Eur. J. Prev. Cardiol. 2019, 26 (Suppl. S2), 7–14. [Google Scholar] [CrossRef]
- Safiri, S.; Karamzad, N.; Kaufman, J.S.; Bell, A.W.; Nejadghaderi, S.A.; Sullman, M.J.M.; Moradi-Lakeh, M.; Collins, G.; Kolahi, A.-A. Prevalence, Deaths and Disability-Adjusted-Life-Years (DALYs) Due to Type 2 Diabetes and Its Attributable Risk Factors in 204 Countries and Territories, 1990-2019: Results From the Global Burden of Disease Study 2019. Front. Endocrinol. 2022, 13, 838027. [Google Scholar] [CrossRef] [PubMed]
- Edmonds, M.; Manu, C.; Vas, P. The current burden of diabetic foot disease. J. Clin. Orthop. Trauma 2021, 17, 88–93. [Google Scholar] [CrossRef]
- Wadhawan, G.; Prakash, A.; Wadhawan, M. Diabetic Foot Ulcer—A clinical study. Int. J. Multidiscip. Res. 2025, 7, 1–22. [Google Scholar] [CrossRef]
- McDermott, K.; Fang, M.; Boulton, A.J.; Selvin, E.; Hicks, C.W. Etiology, Epidemiology, and Disparities in the Burden of Diabetic Foot Ulcers. Diabetes Care 2023, 46, 209–221. [Google Scholar] [CrossRef]
- Everett, E.; Mathioudakis, N. Update on management of diabetic foot ulcers. Ann. N. Y. Acad. Sci. 2018, 1411, 153–165. [Google Scholar] [CrossRef]
- Fan, Z.; Liu, Y.; Xie, H.; Yang, Q.; Zhang, G.; Zhang, P.; Ding, H. Analysis of risk factors for foot ulcers in diabetes patients with neurovascular complications. BMC Public Health 2025, 25, 792. [Google Scholar] [CrossRef]
- Fitridge, R.; Chuter, V.; Mills, J.; Hinchliffe, R.; Azuma, N.; Behrendt, C.; Boyko, E.J.; Conte, M.S.; Humphries, M.; Kirksey, L.; et al. The intersocietal IWGDF, ESVS, SVS guidelines on peripheral artery disease in people with diabetes and a foot ulcer. Diabetes/Metabolism Res. Rev. 2024, 40, e3686. [Google Scholar] [CrossRef] [PubMed]
- Piran, N.; Farhadian, M.; Soltanian, A.R.; Borzouei, S. Diabetic foot ulcers risk prediction in patients with type 2 diabetes using classifier based on associations rule mining. Sci. Rep. 2024, 14, 635. [Google Scholar] [CrossRef]
- Chang, M.; Nguyen, T.T. Strategy for Treatment of Infected Diabetic Foot Ulcers. Accounts Chem. Res. 2021, 54, 1080–1093. [Google Scholar] [CrossRef]
- Lin, C.-W.; Hung, C.-M.; Chen, W.-J.; Chen, J.-C.; Huang, W.-Y.; Lu, C.-S.; Kuo, M.-L.; Chen, S.-G. New Horizons of Macrophage Immunomodulation in the Healing of Diabetic Foot Ulcers. Pharmaceutics 2022, 14, 2065. [Google Scholar] [CrossRef]
- Monaghan, M.G.; Borah, R.; Thomsen, C.; Browne, S. Thou shall not heal: Overcoming the non-healing behaviour of diabetic foot ulcers by engineering the inflammatory microenvironment. Adv. Drug Deliv. Rev. 2023, 203, 115120. [Google Scholar] [CrossRef] [PubMed]
- Afonso, A.C.; Oliveira, D.; Saavedra, M.J.; Borges, A.; Simões, M. Biofilms in Diabetic Foot Ulcers: Impact, Risk Factors and Control Strategies. Int. J. Mol. Sci. 2021, 22, 8278. [Google Scholar] [CrossRef] [PubMed]
- Abu-Baker, A.; Ţigăran, A.-E.; Timofan, T.; Ion, D.-E.; Gheoca-Mutu, D.-E.; Avino, A.; Marina, C.-N.; Tulin, A.D.; Raducu, L.; Jecan, R.-C. Mapping Perfusion and Predicting Success: Infrared Thermography-Guided Perforator Flaps for Lower Limb Defects. Medicina 2025, 61, 1410. [Google Scholar] [CrossRef]
- Boulton, A.J.; Armstrong, D.G.; Kirsner, R.S.; Attinger, C.E.; Lavery, L.A.; Lipsky, B.A.; Mills, J.L., Sr.; Steinberg, J.S. Diagnosis and management of diabetic foot complications. Diabetes 2018, 2018, 1–20. [Google Scholar] [CrossRef]
- Gallagher, K.A.; Mills, J.L.; Armstrong, D.G.; Conte, M.S.; Kirsner, R.S.; Minc, S.D.; Plutzky, J.; Southerland, K.W.; Tomic-Canic, M.; on behalf of the American Heart Association Council on Peripheral Vascular Disease; et al. Current Status and Principles for the Treatment and Prevention of Diabetic Foot Ulcers in the Cardiovascular Patient Population: A Scientific Statement From the American Heart Association. Circulation 2024, 149, e232–e253. [Google Scholar] [CrossRef]
- Jeffcoate, W.J.; Harding, K.G. Diabetic foot ulcers. Lancet 2003, 361, 1545–1551. [Google Scholar] [CrossRef]
- Alavi, A.; Sibbald, R.G.; Mayer, D.; Goodman, L.; Botros, M.; Armstrong, D.G.; Woo, K.; Boeni, T.; Ayello, E.A.; Kirsner, R.S. Diabetic foot ulcers. J. Am. Acad. Dermatol. 2014, 70, 21.e1–21.e24. [Google Scholar] [CrossRef]
- Jeffcoate, W.J.; Vileikyte, L.; Boyko, E.J.; Armstrong, D.G.; Boulton, A.J. Current Challenges and Opportunities in the Prevention and Management of Diabetic Foot Ulcers. Diabetes Care 2018, 41, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Bhat, S.; Chia, B.; Barry, I.P.; Panayi, A.C.; Orgill, D.P. Free Tissue Transfer in Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis. Eur. J. Vasc. Endovasc. Surg. 2023, 66, 670–677. [Google Scholar] [CrossRef] [PubMed]
- Reed, A.J.; Lim, N.T.; Yip, S.W.; Thurley, N.; Wormald, J.C.; Rodrigues, J.N.; Shirley, R.A.; Chan, J.K. Outcomes of Flap Reconstruction for Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis of Clinical Studies. Plast. Reconstr. Surg. 2024, 154, 1118–1130. [Google Scholar] [CrossRef] [PubMed]
- Nigam, M.; Zolper, E.G.B.; Sharif-Askary, B.; Abdou, S.A.; Charipova, K.B.; Bekeny, J.C.B.; Fan, K.L.; Steinberg, J.S.D.; Attinger, C.E.; Evans, K.K. Expanding Criteria for Limb Salvage in Comorbid Patients with Nonhealing Wounds: The MedStar Georgetown Protocol and Lessons Learned after 200 Lower Extremity Free Flaps. Plast. Reconstr. Surg. 2022, 150, 197–209. [Google Scholar] [CrossRef]
- Kotha, V.S.; Fan, K.L.; Schwitzer, J.A.; Youn, R.; Black, C.K.; Attinger, C.E.; Evans, K.K. Amputation versus Free Flap: Long-Term Outcomes of Microsurgical Limb Salvage and Risk Factors for Amputation in the Diabetic Population. Plast. Reconstr. Surg. 2021, 147, 742–750. [Google Scholar] [CrossRef]
- Felder, J.M.; Orr, J.; Schott, H.B.; Geraghty, P. Objective grading of peripheral vascular disease strongly predicts morbidity in microsurgical lower limb salvage. Plast. Reconstr. Surg. 2025. [Google Scholar] [CrossRef]
- Chang, C.-H.; Huang, C.-C.; Hsu, H.; Lin, C.-M.; Huang, S.-M. Editor’s Choice—Diabetic Limb Salvage with Endovascular Revascularisation and Free Tissue Transfer: Long-Term Follow up. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 527–536. [Google Scholar] [CrossRef]
- O’Connor, E.F.; Vesely, M.; Holt, P.; Jones, K.; Thompson, M.; Hinchliffe, R. A Systematic Review of Free Tissue Transfer in the Management of Non-traumatic Lower Extremity Wounds in Patients with Diabetes. Eur. J. Vasc. Endovasc. Surg. 2011, 41, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Kallio, M.; Vikatmaa, P.; Kantonen, I.; Lepäntalo, M.; Venermo, M.; Tukiainen, E. Strategies for Free Flap Transfer and Revascularisation with Long-term Outcome in the Treatment of Large Diabetic Foot Lesions. Eur. J. Vasc. Endovasc. Surg. 2015, 50, 223–230. [Google Scholar] [CrossRef]
- Kozusko, S.; Liu, X.; Riccio, C.; Chang, J.; Boyd, L.; Kokkalis, Z.; Konofaos, P. Selecting a free flap for soft tissue coverage in lower extremity reconstruction. Injury 2019, 50, S32–S39. [Google Scholar] [CrossRef]
- Hong, J.P.; Kim, E.K. Sole Reconstruction Using Anterolateral Thigh Perforator Free Flaps. Plast. Reconstr. Surg. 2007, 119, 186–193. [Google Scholar] [CrossRef]
- Lee, Y.J.; Kim, J.; Lee, C.R.; Kim, J.H.; Oh, D.Y.; Jun, Y.J.; Moon, S.-H. Anterolateral Thigh Chimeric Flap: An Alternative Reconstructive Option to Free Flaps for Large Soft Tissue Defects. J. Clin. Med. 2023, 12, 6723. [Google Scholar] [CrossRef]
- Min, K.; Hong, J.P.M.; Suh, H.P.M. Risk Factors for Partial Flap Loss in a Free Flap: A 12-Year Retrospective Study of Anterolateral Thigh Free Flaps in 303 Lower Extremity Cases. Plast. Reconstr. Surg. 2022, 150, 1071e–1081e. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef] [PubMed]
- The Jamovi Project. Jamovi, version 2.3 [Computer Software]; Jamovi: Sydney, Australia, 2025. Available online: https://www.jamovi.org (accessed on 13 September 2025).
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.P.M.; Shin, H.W.M.; Kim, J.J.M.; Wei, F.-C.M.; Chung, Y.K.M. The Use of Anterolateral Thigh Perforator Flaps in Chronic Osteomyelitis of the Lower Extremity. Plast. Reconstr. Surg. 2005, 115, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.P. Reconstruction of the Diabetic Foot Using the Anterolateral Thigh Perforator Flap. Plast. Reconstr. Surg. 2006, 117, 1599–1608. [Google Scholar] [CrossRef]
- Lee, Y.J.; Kim, J.-Y. A Study of the Survival Factors of Free Flap in Older Diabetic Patients. J. Reconstr. Microsurg. 2007, 23, 373–380. [Google Scholar] [CrossRef]
- Kadam, D. Microsurgical Reconstruction of Plantar Ulcers of the Insensate Foot. J. Reconstr. Microsurg. 2016, 32, 402–410. [Google Scholar] [CrossRef]
- Yang, Y.; Cao, Z.-M.; Sun, N.-Z.; Qing, L.-M.; Wu, P.-F.; Tang, J.-Y. Clinical effects of different types of flaps selected according to local conditions in the treatment of diabetic foot defects. J. Orthop. Surg. Res. 2024, 19, 634. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Zhou, Z.; Boey, J.; Yu, L.; Marei, A.E.; Meng, F.; Xiao, Y.; Zeng, H.; Wan, S. Clinical evaluation of orthoplastic limb salvage protocol using anterolateral femoral free flap and kickstand fixation: A retrospective case-control study. Foot 2025, 63, 102176. [Google Scholar] [CrossRef] [PubMed]
- Paley, D.; Catagni, M.A.; Argnani, F.; Villa, A.; Bijnedetti, G.B.; Cattaneo, R. Ilizarov Treatment of Tibial Nonunions with Bone Loss. Clin. Orthop. Relat. Res. 1989, 241, 146–165. [Google Scholar] [CrossRef]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical Rating Systems for the Ankle-Hindfoot, Midfoot, Hallux, and Lesser Toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef]
- Bekara, F.; Herlin, C.; Mojallal, A.; Sinna, R.; Ayestaray, B.; Letois, F.; Chavoin, J.P.; Garrido, I.; Grolleau, J.L.; Chaput, B. A Systematic Review and Meta-Analysis of Perforator-Pedicled Propeller Flaps in Lower Extremity Defects. Plast. Reconstr. Surg. 2016, 137, 314–331. [Google Scholar] [CrossRef]
- Demiri, E.; Tsimponis, A.; Pavlidis, L.; Spyropoulou, G.-A.; Foroglou, P.; Dionyssiou, D. Reverse neurocutaneous vs propeller perforator flaps in diabetic foot reconstruction. Injury 2020, 51, S16–S21. [Google Scholar] [CrossRef]
- Hutting, K.H.; de Stegge, W.B.A.; van Netten, J.J.; Cate, W.A.T.; Smeets, L.; Welten, G.M.J.M.; Scharn, D.M.; de Vries, J.-P.P.M.; van Baal, J.G. Surgical Treatment of Diabetic Foot Ulcers Complicated by Osteomyelitis with Gentamicin-Loaded Calcium Sulphate-Hydroxyapatite Biocomposite. J. Clin. Med. 2021, 10, 371. [Google Scholar] [CrossRef]
- Kavarthapu, V.; Giddie, J.; Kommalapati, V.; Casey, J.; Bates, M.; Vas, P. Evaluation of Adjuvant Antibiotic Loaded Injectable Bio-Composite Material in Diabetic Foot Osteomyelitis and Charcot Foot Reconstruction. J. Clin. Med. 2023, 12, 3239. [Google Scholar] [CrossRef]
- Burkhard, J.-P.; Pfister, J.; Giger, R.; Huber, M.; Lädrach, C.; Waser, M.; Olariu, R.; Engel, D.; Löffel, L.M.; Schaller, B.; et al. Correction to: Perioperative predictors of early surgical revision and flap-related complications after microvascular free tissue transfer in head and neck reconstructions: A retrospective observational series. Clin. Oral Investig. 2021, 25, 5551. [Google Scholar] [CrossRef]
- Toro, G.; Cecere, A.B.; Braile, A.; De Cicco, A.; Liguori, S.; Tarantino, U.; Iolascon, G. New insights in lower limb reconstruction strategies. Ther. Adv. Musculoskelet. Dis. 2023, 15, 1759720X231189008. [Google Scholar] [CrossRef]
- Yan, X.; Song, J.-F.; Zhang, L.; Li, X. Analysis of risk factors for multidrug-resistant organisms in diabetic foot infection. BMC Endocr. Disord. 2022, 22, 46. [Google Scholar] [CrossRef]
- Bonnet, J.-B.; Sultan, A. Narrative Review of the Relationship Between CKD and Diabetic Foot Ulcer. Kidney Int. Rep. 2022, 7, 381–388. [Google Scholar] [CrossRef]
- Vacaroiu, I.A.; Cuiban, E.; Geavlete, B.F.; Gheorghita, V.; David, C.; Ene, C.V.; Bulai, C.; Lupusoru, G.E.; Lupusoru, M.; Balcangiu-Stroescu, A.E.; et al. Chronic Kidney Disease—An Underestimated Risk Factor for Antimicrobial Resistance in Patients with Urinary Tract Infections. Biomedicines 2022, 10, 2368. [Google Scholar] [CrossRef] [PubMed]
- Calinoiu, A.; Guluta, E.-C.; Rusu, A.; Minca, A.; Minca, D.; Tomescu, L.; Gheorghita, V.; Minca, D.G.; Negreanu, L. Accessory renal arteries—A source of hypertension: A case report. World J. Clin. Cases 2023, 11, 1506–1512. [Google Scholar] [CrossRef]
- Otte, J.; van Netten, J.J.; Woittiez, A.-J.J. The association of chronic kidney disease and dialysis treatment with foot ulceration and major amputation. J. Vasc. Surg. 2015, 62, 406–411. [Google Scholar] [CrossRef]
- Lan, N.S.R.; Hiew, J.; Ferreira, I.; Ritter, J.C.; Manning, L.; Fegan, P.G.; Hamilton, E.J.; Dwivedi, G. The combined impact of chronic kidney disease and ulcer severity on incident cardiovascular events in patients with diabetes-related foot ulceration. Physiol. Rep. 2025, 13, e70415. [Google Scholar] [CrossRef]
- Rahma, S.; Woods, J.; Brown, S.; Nixon, J.; Russell, D. The Use of Point-of-Care Bacterial Autofluorescence Imaging in the Management of Diabetic Foot Ulcers: A Pilot Randomized Controlled Trial. Diabetes Care 2022, 45, 1601–1609. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-Y.; Lin, C.-W.; Cheng, N.-C.; Cazzell, S.M.; Chen, H.-H.; Huang, K.-F.; Tung, K.-Y.; Huang, H.-L.; Lin, P.-Y.; Perng, C.-K.; et al. Effect of a Novel Macrophage-Regulating Drug on Wound Healing in Patients With Diabetic Foot Ulcers. JAMA Netw. Open 2021, 4, e2122607. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.; Jian, Y.; Liu, C.; Prà, I.D.; Armato, U.; Chen, X.; Zhou, J.; Chen, W.; Zhang, F.; Nie, K.; et al. Combining antibiotic-loaded bone cement-based free vastus lateralis muscle-sparing flap with split-thickness skin grafts: A reliable strategy for reconstructing diabetic foot ulcers at non-weight-bearing areas. Int. Wound J. 2024, 21, e14900. [Google Scholar] [CrossRef] [PubMed]
| Kim 2007 [42] | Hong 2006 [41] | Hong 2005 [40] | Kadam 2016 [43] | Yang 2024 [44] | Wen 2025 [45] | |
|---|---|---|---|---|---|---|
| 1. A clearly stated aim | 2 | 2 | 2 | 1 | 1 | 2 |
| 2. Inclusion of consecutive patients | 2 | 1 | 2 | 2 | 2 | 1 |
| 3. Prospective collection of data | 0 | 0 | 0 | 0 | 0 | 0 |
| 4. Endpoints appropriate to the aim of the study | 1 | 1 | 1 | 1 | 2 | 2 |
| 5. Unbiased assessment of the study endpoint | 0 | 0 | 0 | 0 | 0 | 0 |
| 6. Follow-up period appropriate to the aim of the study | 2 | 1 | 2 | 0 | 2 | 2 |
| 7. Loss to follow-up less than 5% | 0 | 2 | 2 | 2 | 2 | 2 |
| 8. Prospective calculation of the study size | 0 | 0 | 0 | 0 | 0 | 0 |
| Item 9–12 only for comparative studies | ||||||
| 9. An adequate control group | 1 | 1 | ||||
| 10. Contemporary groups | 2 | 2 | ||||
| 11. Baseline equivalence of groups | 2 | 2 | ||||
| 12. Adequate statistical analyses | 2 | 2 | ||||
| TOTAL MINORS score | 7 | 7 | 9 | 6 | 16 | 16 |
| Maximum possible score | 16 | 16 | 16 | 16 | 24 | 24 |
| Outcome | No. of Studies (k) | Total Patients (N) | Pooled Estimate (95% CI) | Heterogeneity (I2) |
|---|---|---|---|---|
| Primary outcomes | ||||
| Complete flap necrosis | 6 | 162 | 5.2% [2.5%, 10.6%] | 0% |
| Partial flap necrosis | 4 | 131 | 13% [6.3%, 24.8%] | 46.8% |
| Patient characteristics | ||||
| Age (years) | 5 | 91 | 54.9 [49.7, 60.2] | 90.1% |
| Prevalence of osteomyelitis | 4 | 104 | 63.7% [31.4%, 87%] | 76.5% |
| Glycated Hemoglobin (%) | 2 | 40 | 9.9% [8.5%, 11.5%] | 75.3% |
| Peripheral arterial disease | 2 | 50 | 54.3% [−35%, 144%] | 99.1% |
| Chronic kidney failure | 2 | 41 | 16.9% [5.5%, 28.2%] | 0% |
| Chronic heart failure | 1 | 34 | 14.7% | N/A |
| Tobacco consumption | 1 | 34 | 41.1% | N/A |
| Defect location | ||||
| Foot plantar surface | 4 | 81 | 38.6% [28.6%, 49.8%] | 0% |
| Dorsum of foot | 3 | 74 | 40.9% [20.8%, 64.5%] | 71.99% |
| Heel | 3 | 57 | 27% [8%, 61.2%] | 75.79% |
| Ankle | 3 | 74 | 15.6% [4.3%, 42.9%] | 70.11% |
| Calf | 2 | 50 | 3.7% [−4%, 11.6%] | 0% |
| Flap characteristics | ||||
| Area (cm2) | 5 | 138 | 103 [50, 155] | 97.6% |
| End-to-end anastomosis | 2 | 23 | 11.4% [−16%, 38.8%] | 68.7% |
| End-to-side anastomosis | 2 | 23 | 88.6% [61.2%, 116%] | 68.7% |
| Anterior tibial artery as receiving vessel | 3 | 57 | 42.2% [24.4%, 62.3%] | 45.2% |
| Posterior tibial artery as receiving vessel | 3 | 57 | 55.6% [30.4%, 78.3%] | 65.17% |
| Peroneal artery as receiving vessel | 1 | 16 | 0% | N/A |
| Mean pedicle length (cm) | 1 | 16 | 14.1 | N/A |
| Number of perforators/flaps | 1 | 16 | 1.125 | N/A |
| Outcomes | ||||
| Flap infection | 4 | 145 | 5.1% [1.6%, 14.7%] | 40.2% |
| Vascular insufficiency | 3 | 74 | 6.9% [2.9%, 15.4%] | 0% |
| Ulcer recurrence | 2 | 78 | 1.7% [−2.6%, 6.1%] | 0% |
| Revision rate | 2 | 87 | 7.7% [1.5%, 13.9%] | 0% |
| Wound healing success rate | 1 | 24 | 100% | N/A |
| Time to complete wound healing (weeks) | 2 | 58 | 7.2 [2.3, 12.1] | 95.1% |
| Mean follow-up (weeks) | 2 | 44 | 119 [114, 125] | 0% |
| Mean length of stay (weeks) | 1 | 71 | 3.5 | N/A |
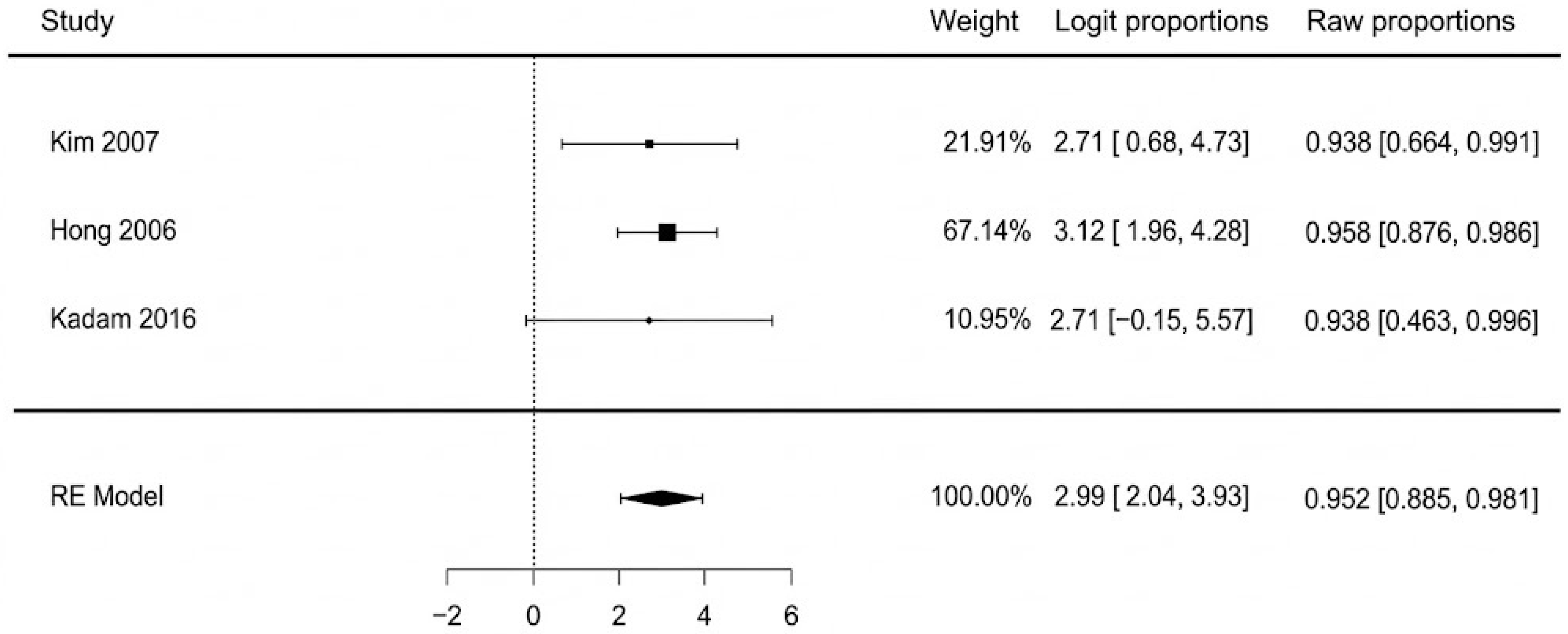
| Gait return | 3 | 94 | 95.2% [88.5%, 98.1%] | 0% |
| Mortality | 1 | 16 | 6.20% | N/A |
| ASAMI Functional Results | Number of Patients |
|---|---|
| Excellent | 8 |
| Good | 13 |
| Fair | 7 |
| Poor | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abu-Baker, A.; Ţigăran, A.-E.; Timofan, T.; Ion, D.-E.; Gheoca-Mutu, D.-E.; Avino, A.; Tulin, A.D.; Raducu, L.; Jecan, C.-R. A Systematic Review and Meta-Analysis of Anterolateral Thigh Flap Outcomes in High-Risk Diabetic Foot Reconstruction. J. Clin. Med. 2025, 14, 8481. https://doi.org/10.3390/jcm14238481
Abu-Baker A, Ţigăran A-E, Timofan T, Ion D-E, Gheoca-Mutu D-E, Avino A, Tulin AD, Raducu L, Jecan C-R. A Systematic Review and Meta-Analysis of Anterolateral Thigh Flap Outcomes in High-Risk Diabetic Foot Reconstruction. Journal of Clinical Medicine. 2025; 14(23):8481. https://doi.org/10.3390/jcm14238481
Chicago/Turabian StyleAbu-Baker, Abdalah, Andrada-Elena Ţigăran, Teodora Timofan, Daniela-Elena Ion, Daniela-Elena Gheoca-Mutu, Adelaida Avino, Adrian Daniel Tulin, Laura Raducu, and Cristian-Radu Jecan. 2025. "A Systematic Review and Meta-Analysis of Anterolateral Thigh Flap Outcomes in High-Risk Diabetic Foot Reconstruction" Journal of Clinical Medicine 14, no. 23: 8481. https://doi.org/10.3390/jcm14238481
APA StyleAbu-Baker, A., Ţigăran, A.-E., Timofan, T., Ion, D.-E., Gheoca-Mutu, D.-E., Avino, A., Tulin, A. D., Raducu, L., & Jecan, C.-R. (2025). A Systematic Review and Meta-Analysis of Anterolateral Thigh Flap Outcomes in High-Risk Diabetic Foot Reconstruction. Journal of Clinical Medicine, 14(23), 8481. https://doi.org/10.3390/jcm14238481