Are There Benefits of Total Hip Arthroplasty with Dual-Mobility Cups Compared to Bipolar Hemiarthroplasty for Femoral Neck Fractures in the Geriatric Population? A Systematic Review and Meta-Analysis of Comparative Studies
Abstract
1. Introduction
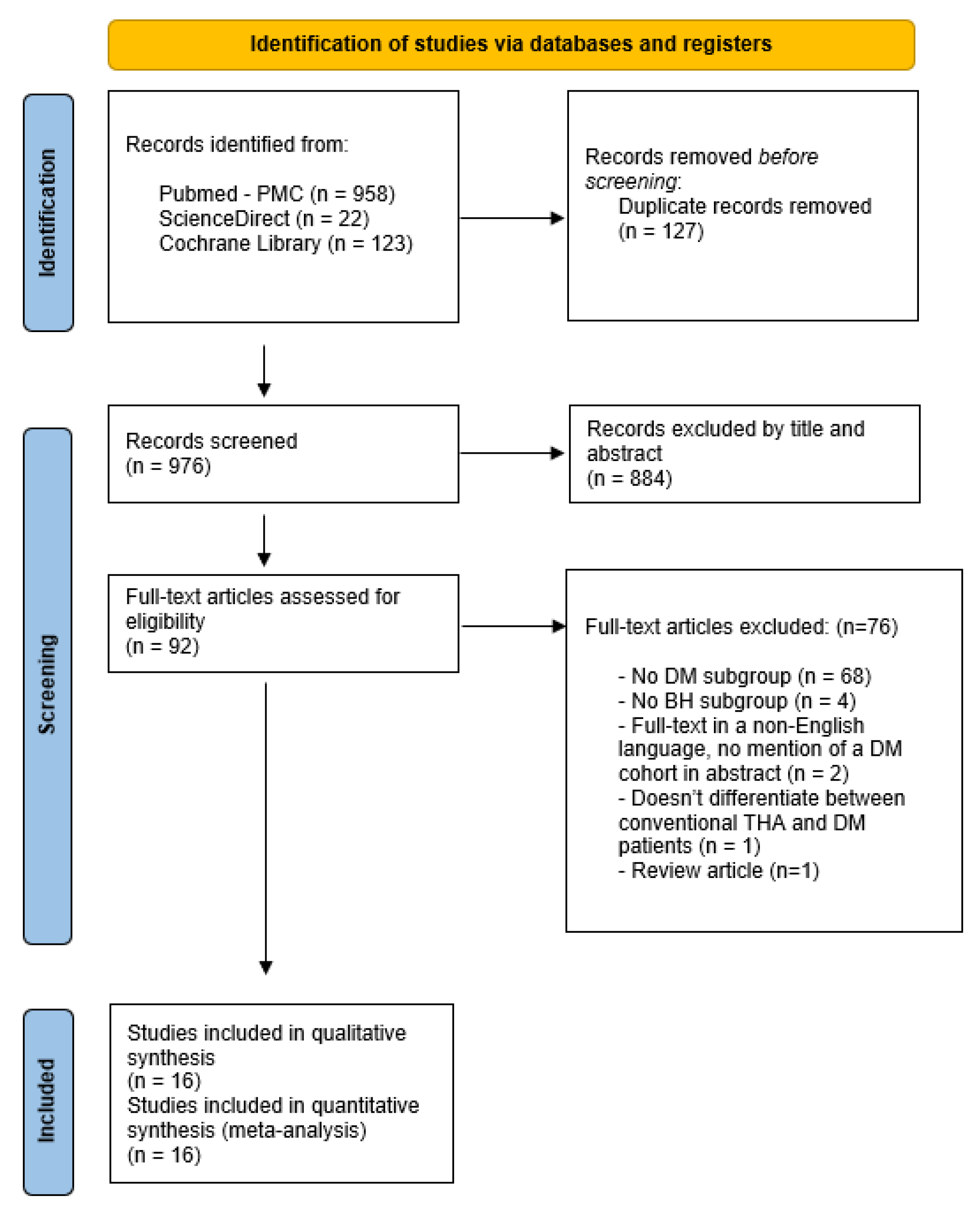
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Risk of Bias and Study Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Search Results
3.2. Included Studies Design and Patient Demographics
3.3. Studied Outcomes and Follow-Up
3.4. Operative and Implant Characteristics
3.5. Cognitive and Neuromuscular Status of Patients in the Included Studies
3.6. Outcomes
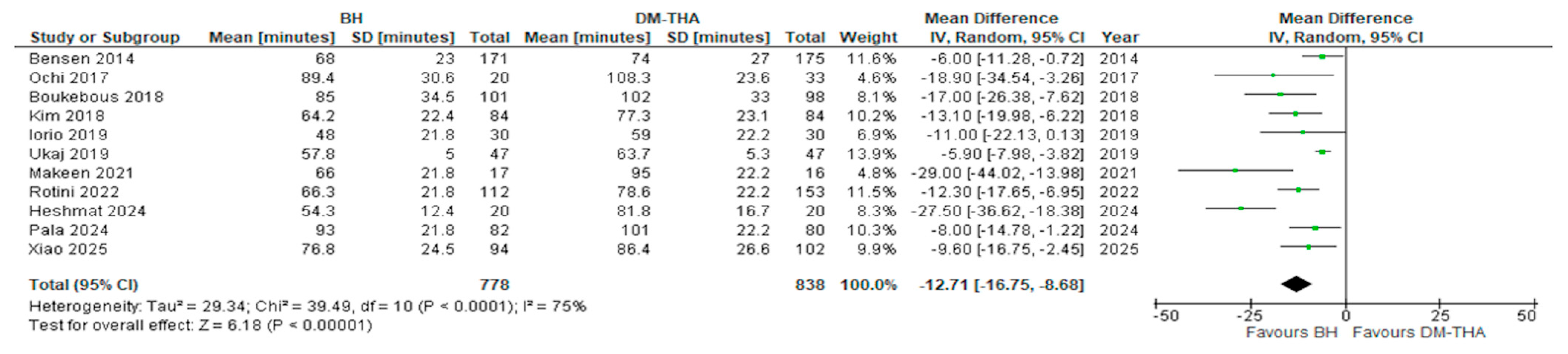
- (i)
- Operative time
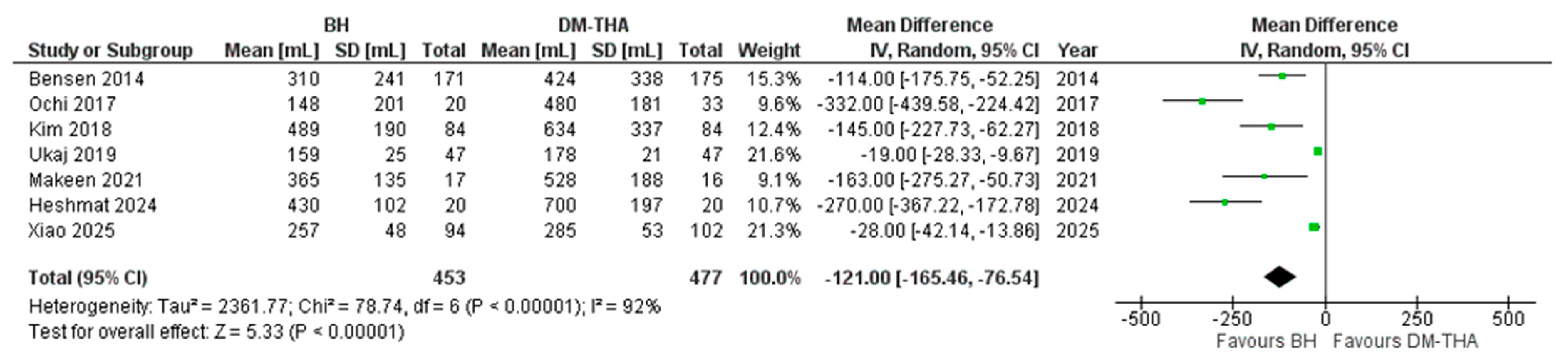
- (ii)
- Estimated blood loss
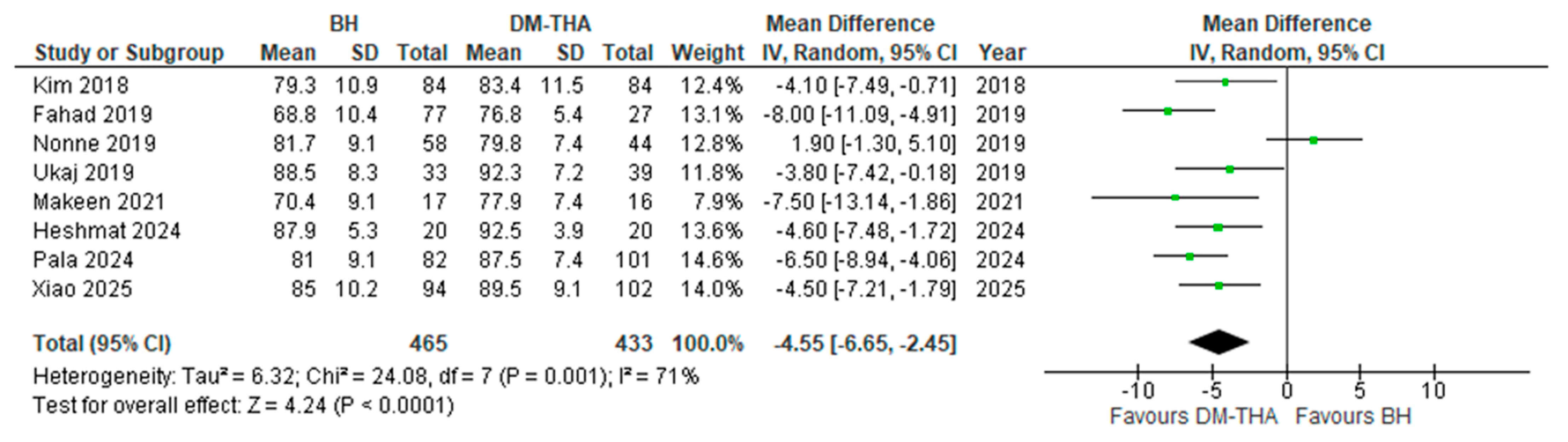
- (iii)
- Postoperative Harris Hip Score (HHS)
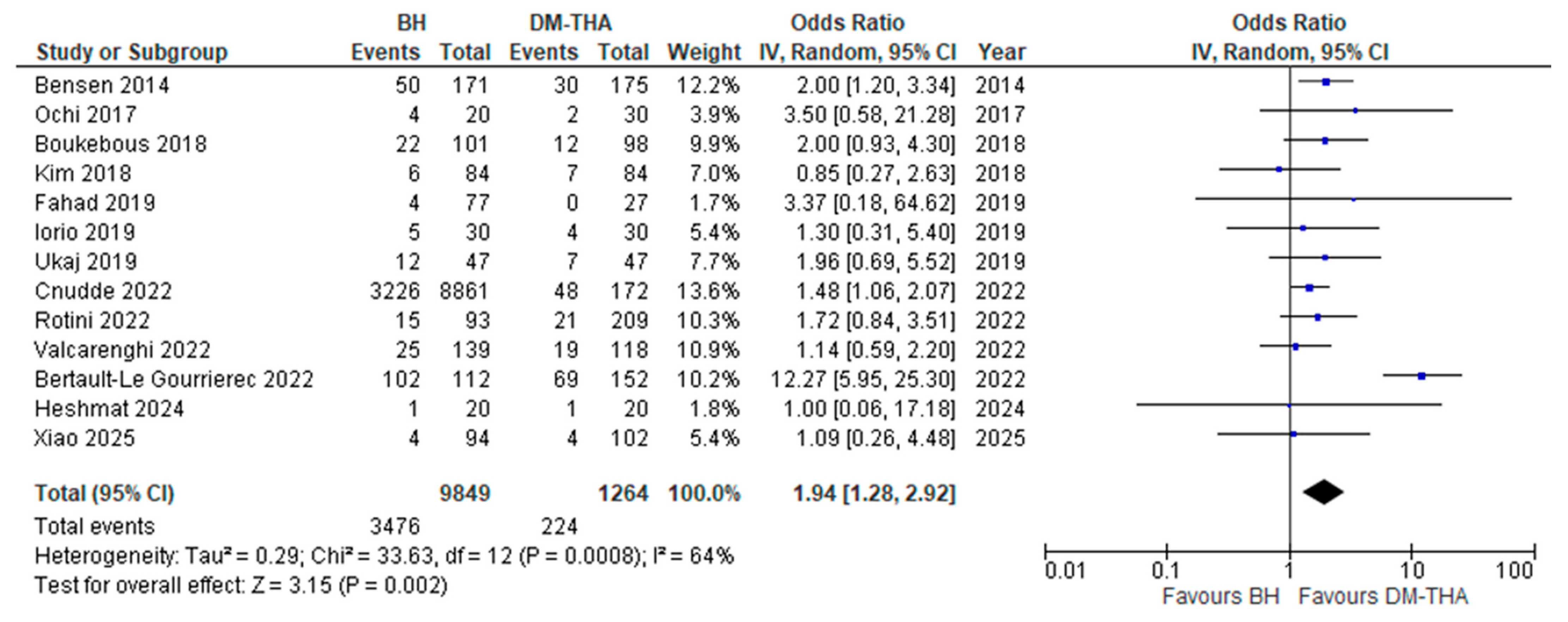
- (iv)
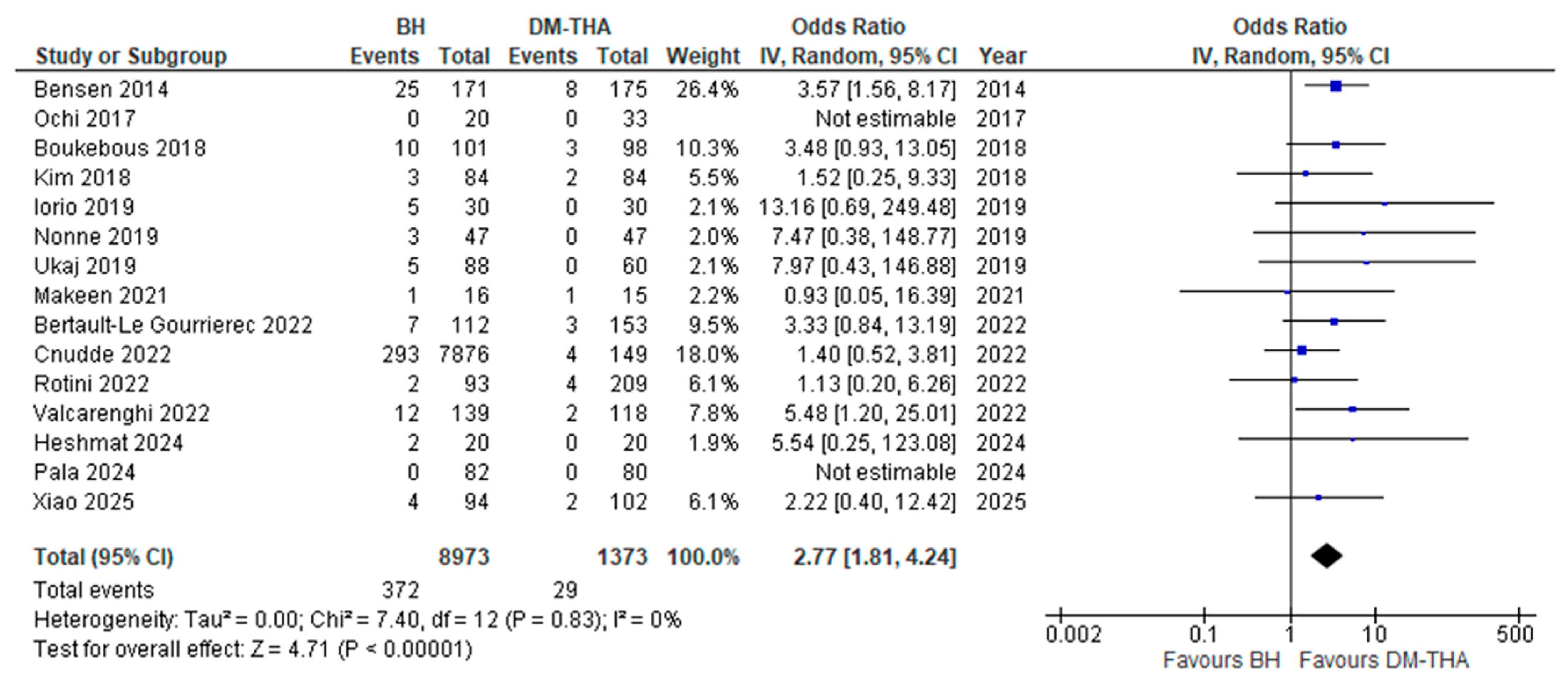
- Dislocation rate
- (v)
- Reoperation rate
- (vi)
- Mortality rate
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| FNF | Femoral Neck Fracture |
| HA | Hip Hemiarthroplasty |
| THA | Total Hip Arthroplasty |
| DM | Dual Mobility |
| BH | Bipolar Hip Hemiarthroplasty |
| DM-THA | Dual Mobility Total Hip Arthroplasty |
| PROMs | Patient Reported Outcome Measures |
| RCT | Randomised Controlled Trials |
| RoB2 | Cochrane Risk of Bias 2 assessment tool |
| NOS | Newcastle-Ottawa Scale |
| CI | Confidence Interval |
| OR | Odds Ratio |
| HHS | Harris Hip Score |
References
- Xu, D.-F.; Bi, F.-G.; Ma, C.-Y.; Wen, Z.-F.; Cai, X.-Z. A Systematic Review of Undisplaced Femoral Neck Fracture Treatments for Patients over 65 Years of Age, with a Focus on Union Rates and Avascular Necrosis. J. Orthop. Surg. Res. 2017, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, H.Q.; Hossain, F.S.; Aqil, A.; Akinbamijo, B.; Mushtaq, V.; Kapoor, H. A Comprehensive Analysis of the Causes and Predictors of 30-Day Mortality Following Hip Fracture Surgery. Clin. Orthop. Surg. 2017, 9, 10. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F.; Moldovan, L. A Modeling Study for Hip Fracture Rates in Romania. J. Clin. Med. 2025, 14, 3162. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; She, G.; Luo, S.; Wu, W.; Zhuang, T.; Huan, S.; Liu, N.; Zha, Z. Hemiarthroplasty Compared with Internal Fixation for Treatment of Nondisplaced Femoral Neck Fractures in Elderly Patients: A Retrospective Study. Injury 2020, 51, 1021–1024. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp-Chalifour, P.; Pelet, S.; Belhumeur, V.; Angers-Goulet, M.; Bédard, L.; Belzile, E.L. Should We Use Bipolar Hemiarthroplasty in Patients ≥70 Years Old with a Femoral Neck Fracture? A Review of Literature and Meta-Analysis of Randomized Controlled Trials. J. Arthroplast. 2022, 37, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Filippo, M.; Driessen, A.; Colarossi, G.; Quack, V.; Tingart, M.; Eschweiler, J. Bipolar versus Monopolar Hemiarthroplasty for Displaced Femur Neck Fractures: A Meta-Analysis Study. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Imam, M.A.; Shehata, M.; Abdallah, A.R.; Ahmed, H.; Kader, N.; Ernstbrunner, L.; Narvani, A.A.; Kambouroglou, G.; Mcnamara, I.; Sallam, A.A. Unipolar versus Bipolar Hemiarthroplasty for Displaced Femoral Neck Fractures: A Pooled Analysis of 30,250 Participants Data. Injury 2019, 50, 1694–1708. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.-I.; Jang, S.-Y.; Cha, Y.; Choy, W.-S.; Koo, K.-H. Comparison of Mortality, Length of Hospital Stay and Transfusion between Hemiarthroplasty and Total Hip Arthroplasty in Octo- and Nonagenarian Patients with Femoral Neck Fracture: A Nationwide Study in Korea. J. Korean Med. Sci. 2021, 36, e300. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Bi, N.; Zheng, J.; Xi, N. Does Total Hip Arthroplasty Provide Better Outcomes than Hemiarthroplasty for the Femoral Neck Fracture? A Systematic Review and Meta-Analysis. Chin. J. Traumatol. 2020, 23, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Bhattacharyya, T. Outcomes of Hemiarthroplasty and Total Hip Arthroplasty for Femoral Neck Fracture: A Medicare Cohort Study. J. Orthop. Trauma 2017, 31, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Patil, N.; Deshmane, P.; Deshmukh, A.; Mow, C. Dual Mobility in Total Hip Arthroplasty: Biomechanics, Indications and Complications–Current Concepts. Indian J. Orthop. IJOO 2021, 55, 1202–1207. [Google Scholar] [CrossRef] [PubMed]
- Castiello, E.; Moghnie, A.; Tigani, D.; Affatato, S. Dual Mobility Cup in Hip Arthroplasty: An In-depth Analysis of Joint Registries. Artif. Organs 2022, 46, 804–812. [Google Scholar] [CrossRef] [PubMed]
- De Martino, I.; Triantafyllopoulos, G.K.; Sculco, P.K.; Sculco, T.P. Dual Mobility Cups in Total Hip Arthroplasty. World J. Orthop. WJO 2014, 5, 180. [Google Scholar] [CrossRef] [PubMed]
- Heckmann, N.; Weitzman, D.S.; Jaffri, H.; Berry, D.J.; Springer, B.D.; Lieberman, J.R. Trends in the Use of Dual Mobility Bearings in Hip Arthroplasty. Bone Jt. J. 2020, 102-B, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Santiago, M.S.; Akbarpoor, F.; Aidar, F.J.; Neto, J.M.S.; De Matos Pereira Silva, M.V.V.; Darwish, S.; Khokar, M.A.; Ahmed, Z.; Zamora, F.V.; Madruga, R.E.T.T.; et al. Outcomes of Dual Mobility versus Conventional Total Hip Arthroplasty for Patients with Femoral Neck Fractures: A Systematic Review and Meta-Analysis Including Registry Data. J. Orthop. Surg. Res. 2025, 20, 405. [Google Scholar] [CrossRef] [PubMed]
- Bloemheuvel, E.M.; van Steenbergen, L.N.; Swierstra, B.A.; Schreurs, B.W. Revision Risk of Unipolar and Bipolar Hemiarthroplasties in the Dutch Arthroplasty Register. J. Arthroplast. 2024, 39, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Ravi, B.; Pincus, D.; Khan, H.; Wasserstein, D.; Jenkinson, R.; Kreder, H.J. Comparing Complications and Costs of Total Hip Arthroplasty and Hemiarthroplasty for Femoral Neck Fractures: A Propensity Score-Matched, Population-Based Study. J. Bone Jt. Surg. 2019, 101, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Burgers, P.T.P.W.; Hoogendoorn, M.; Van Woensel, E.A.C.; Poolman, R.W.; Bhandari, M.; Patka, P.; Van Lieshout, E.M.M. Total Medical Costs of Treating Femoral Neck Fracture Patients with Hemi- or Total Hip Arthroplasty: A Cost Analysis of a Multicenter Prospective Study. Osteoporos. Int. 2016, 27, 1999–2008. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.-H.; Chou, T.-F.A.; Pai, F.-Y.; Tsai, S.-W.; Chen, C.-F.; Wu, P.-K.; Chen, W.-M. Outcomes of Dual-Mobility Total Hip Arthroplasty versus Bipolar Hemiarthroplasty for Patients with Femoral Neck Fractures: A Systematic Review and Meta-Analysis. J. Orthop. Surg. Res. 2021, 16, 152. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Wang, D.; Liu, Y.; Chen, J.; Zhou, Z.; Li, P.; Ning, N. The Comparison between Total Hip Arthroplasty and Hemiarthroplasty in Patients with Femoral Neck Fractures: A Systematic Review and Meta-Analysis Based on 25 Randomized Controlled Trials. J. Orthop. Surg. Res. 2020, 15, 596. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Corporation for Digital Scholarship. Zotero, version 6.0.26, [Software] (Original Work Published 2006); Corporation for Digital Scholarship: Vienna, VA, USA, 2023. Available online: https://www.zotero.org/ (accessed on 15 June 2025).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Ottawa Hospital Research Institute. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 15 June 2025).
- RevMan. Available online: https://revman.cochrane.org/myReviews (accessed on 22 June 2025).
- Bensen, A.S.; Jakobsen, T.; Krarup, N. Dual Mobility Cup Reduces Dislocation and Re-Operation When Used to Treat Displaced Femoral Neck Fractures. Int. Orthop. SICOT 2014, 38, 1241–1245. [Google Scholar] [CrossRef] [PubMed]
- Ochi, H.; Baba, T.; Homma, Y.; Matsumoto, M.; Watari, T.; Ozaki, Y.; Kobayashi, H.; Kaneko, K. Total Hip Arthroplasty via the Direct Anterior Approach with a Dual Mobility Cup for Displaced Femoral Neck Fracture in Patients with a High Risk of Dislocation. SICOT-J. 2017, 3, 56. [Google Scholar] [CrossRef] [PubMed]
- Boukebous, B.; Boutroux, P.; Zahi, R.; Azmy, C.; Guillon, P. Comparison of Dual Mobility Total Hip Arthroplasty and Bipolar Arthroplasty for Femoral Neck Fractures: A Retrospective Case-Control Study of 199 Hips. Orthop. Traumatol. Surg. Res. 2018, 104, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.T.; Yoo, J.-H.; Kim, M.K.; Kim, S.; Hwang, J. Dual Mobility Hip Arthroplasty Provides Better Outcomes Compared to Hemiarthroplasty for Displaced Femoral Neck Fractures: A Retrospective Comparative Clinical Study. Int. Orthop. SICOT 2018, 42, 1241–1246. [Google Scholar] [CrossRef] [PubMed]
- Fahad, S.; Nawaz Khan, M.Z.; Aqueel, T.; Hashmi, P. Comparison of Bipolar Hemiarthroplasty and Total Hip Arthroplasty with Dual Mobility Cup in the Treatment of Old Active Patients with Displaced Neck of Femur Fracture: A Retrospective Cohort Study. Ann. Med. Surg. 2019, 45, 62–65. [Google Scholar] [CrossRef]
- Iorio, R.; Iannotti, F.; Mazza, D.; Speranza, A.; Massafra, C.; Guzzini, M.; D’Arrigo, C.; Ferretti, A. Is Dual Cup Mobility Better than Hemiarthroplasty in Patients with Dementia and Femoral Neck Fracture? A Randomized Controlled Trial. SICOT-J. 2019, 5, 38. [Google Scholar] [CrossRef] [PubMed]
- Ukaj, S.; Zhuri, O.; Ukaj, F.; Podvorica, V.; Grezda, K.; Caton, J.; Prudhon, J.L.; Krasniqi, S. Dual Mobility Acetabular Cup Versus Hemiarthroplasty in Treatment of Displaced Femoral Neck Fractures in Elderly Patients: Comparative Study and Results at Minimum 3-Year Follow-Up. Geriatr. Orthop. Surg. Rehabil. 2019, 10, 2151459319848610. [Google Scholar] [CrossRef] [PubMed]
- Nonne, D.; Sanna, F.; Bardelli, A.; Milano, P.; Rivera, F. Use of a Dual Mobility Cup to Prevent Hip Early Arthroplasty Dislocation in Patients at High Falls Risk. Injury 2019, 50, S26–S29. [Google Scholar] [CrossRef] [PubMed]
- Makeen, T.M.; Abdelazim Mohamed, H.; Mohasseb, A.M.; Elshabrawy, W.E.S.A.E.; Ashoub, M.M.; El Ganzoury, I.M. Functional Outcome after Dual Mobility Cups Total Hip Replacement versus Bipolar Hemiarthroplasty in Femoral Neck Fractures in Active Elderly Patients: A Randomized Controlled Trial. Curr. Orthop. Pract. 2021, 32, 468–473. [Google Scholar] [CrossRef]
- Bertault-Le Gourrierec, J.; Cavaignac, E.; Berard, E.; Moretti, F.; Marot, V.; Chiron, P.; Reina, N. Comparative Study of Total Hip Arthroplasties with Dual Mobility Cups versus Hemiarthroplasties in Management of Femoral Neck Fractures: Survival and Dislocation Rate at 5 Years of Follow-Up? Orthop. Traumatol. Surg. Res. 2022, 108, 103098. [Google Scholar] [CrossRef] [PubMed]
- Cnudde, P.H.J.; Nåtman, J.; Hailer, N.P.; Rogmark, C. Total, Hemi, or Dual-Mobility Arthroplasty for the Treatment of Femoral Neck Fractures in Patients with Neurological Disease: Analysis of 9,638 Patients from the Swedish Hip Arthroplasty Register. Bone Jt. J. 2022, 104-B, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Rotini, M.; Farinelli, L.; Natalini, L.; De Rosa, F.; Politano, R.; Cianforlini, M.; Pacetti, E.; Procaccini, R.; Magrini Pasquinelli, F.; Gigante, A. Is Dual Mobility Total Hip Arthroplasty Surgery More Aggressive than Hemiarthroplasty When Treating Femoral Neck Fracture in the Elderly? A Multicentric Retrospective Study on 302 Hips. Geriatr. Orthop. Surg. Rehabil. 2022, 13, 21514593221081375. [Google Scholar] [CrossRef] [PubMed]
- Valcarenghi, J.; Martinov, S.; Chahidi, E.; Jennart, H.; Bui Quoc, E.; Dimanche, M.C.; Hupez, A.; Bhogal, H.; Hafez, K.; Callewier, A.; et al. Hip Fractures Re-Operation Compared with Death at Two Year in Elderly Patients: Lowest Risk of Revision with Dual Mobility Total Hip Arthroplasty than with Bipolar Hemiarthroplasty or Internal Fixation of Garden I and II. Int. Orthop. SICOT 2022, 46, 1945–1953. [Google Scholar] [CrossRef] [PubMed]
- Pala, E.; Canapeti, J.; Trovarelli, G.; Berizzi, A.; Cerchiaro, M.C.; Zanarella, S.; Ruggieri, P. Dual Mobility Cup in Hip Fracture: Indications and Clinical Results Compared with Bipolar Hip Arthroplasty. Injury 2024, 55, 111483. [Google Scholar] [CrossRef] [PubMed]
- Heshmat, H.; Samir, W.; Abdel-Moneim, M.; Zakaria, Z.M. Management of Fracture Neck Femur in Elderly Patients Using Dual Mobility Cup Arthroplasty versus Bipolar Hemiarthroplasty. QJM Int. J. Med. 2024, 117, hcae175.670. [Google Scholar] [CrossRef]
- Xiao, K.; Liu, S.; Liang, B.; Li, S.; Liu, X.; Chen, J. Clinical Efficacy of THA with Dual Mobility Cup vs. Hemiarthroplasty in Elderly Patients with Femoral Neck Fracture: A Retrospective Study. Front. Surg. 2025, 12, 1507068. [Google Scholar] [CrossRef] [PubMed]
- Harris, T.; Segovia, N.; Koltsov, J.; Gardner, M. Association between Operative Duration and Adverse Outcomes after Hip Fracture Surgery: A NSQIP Matched Cohort Study. Injury 2024, 55, 111635. [Google Scholar] [CrossRef] [PubMed]
- Duchman, K.R.; Pugely, A.J.; Martin, C.T.; Gao, Y.; Bedard, N.A.; Callaghan, J.J. Operative Time Affects Short-Term Complications in Total Joint Arthroplasty. J. Arthroplast. 2017, 32, 1285–1291. [Google Scholar] [CrossRef] [PubMed]
- Surace, P.; Sultan, A.A.; George, J.; Samuel, L.T.; Khlopas, A.; Molloy, R.M.; Stearns, K.L.; Mont, M.A. The Association Between Operative Time and Short-Term Complications in Total Hip Arthroplasty: An Analysis of 89,802 Surgeries. J. Arthroplast. 2019, 34, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.L.; Park, J.-H.; Han, S.-B.; Cho, I.Y.; Jang, K.-M. Allogeneic Blood Transfusion Is a Significant Risk Factor for Surgical-Site Infection Following Total Hip and Knee Arthroplasty: A Meta-Analysis. J. Arthroplast. 2017, 32, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Foss, N.B.; Kristensen, M.T.; Kehlet, H. Anaemia Impedes Functional Mobility after Hip Fracture Surgery. Age Ageing 2008, 37, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Guyen, O. Hemiarthroplasty or Total Hip Arthroplasty in Recent Femoral Neck Fractures? Orthop. Traumatol. Surg. Res. 2019, 105, S95–S101. [Google Scholar] [CrossRef] [PubMed]
- Foote, C.J.; Soni, C.; Patel, S.P.; Moore, D.; Szatkowski, J. Factors That Influence Surgical Decision-Making for Geriatric Displaced Femoral Neck Fractures: Bullet Health Analysis (BHA) I: Worldwide Orthopaedic Research Collaboration: Leveraging Big Data (WORLD) I. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 3005–3013. [Google Scholar] [CrossRef] [PubMed]
- Woon, C.Y.L.; Moretti, V.M.; Schwartz, B.E.; Goldberg, B.A. Total Hip Arthroplasty and Hemiarthroplasty: US National Trends in the Treatment of Femoral Neck Fractures. Am. J. Orthop. 2017, 46, E474–E478. [Google Scholar] [PubMed]
- Stronach, B.M.; Bergin, P.F.; Perez, J.L.; Watson, S.; Jones, L.C.; McGwin, G.; Ponce, B.A. The Rising Use of Total Hip Arthroplasty for Femoral Neck Fractures in the United States. HIP Int. 2020, 30, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Zhang, H.; Zhang, Z.; Ma, C.; Feng, X. Comparison of Bipolar Hemiarthroplasty and Total Hip Arthroplasty for Displaced Femoral Neck Fractures in the Healthy Elderly: A Meta-Analysis. BMC Musculoskelet. Disord. 2015, 16, 229. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Luo, J. Hemiarthroplasty Compared to Total Hip Arthroplasty for the Treatment of Femoral Neck Fractures: A Systematic Review and Meta-Analysis. J. Orthop. Surg. Res. 2021, 16, 172. [Google Scholar] [CrossRef] [PubMed]
- Wek, C.; Reichert, I.; Gee, M.; Foley, R.; Ahluwalia, R. Have Advances in Surgical Implants and Techniques in Hemiarthroplasty for Intracapsular Hip Fractures Improved Patient Outcomes Compared to THA? A Systematic Review and Meta-Analysis of the Evidence. The Surgeon 2022, 20, e344–e354. [Google Scholar] [CrossRef] [PubMed]
- Goru, P.; Haque, S.; Verma, G.G.; Mustafa, A.; Hamed, M.; Ismail, M.; Shah, S. Dislocation of Total Hip Replacement in Femoral Neck Fracture: Do Surgical Approach and Dual Mobility Implant Matter? Cureus 2022, 14, e21031. [Google Scholar] [CrossRef] [PubMed]
- Kamimura, T.; Kobayashi, Y.; Tamaki, S.; Koinuma, M. Impact of Prefracture Cognitive Impairment and Postoperative Delirium on Recovery after Hip Fracture Surgery. J. Am. Med. Dir. Assoc. 2024, 25, 104961. [Google Scholar] [CrossRef] [PubMed]
- Pieterse, A.J.; Luttikhold, T.B.; De Laat, K.; Bloem, B.R.; Van Engelen, B.G.; Munneke, M. Falls in Patients with Neuromuscular Disorders. J. Neurol. Sci. 2006, 251, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Ryu, H.-G.; Roh, Y.J.; Oh, K.-J.; Hwang, J.-H.; Kim, Y.; Cho, H.-W.; Kim, S.-M. Dual Mobility Articulation Total Hip Arthroplasty for Displaced Neck Fracture in Elderly with Neuromuscular Disorder. Injury 2021, 52, 1480–1486. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yao, Z.; Shi, P.; Wang, C.; Liu, J.; Yang, Y.; Zhang, C. Morphological Risk Factors Associated with Dislocation after Bipolar Hemiarthroplasty of the Hip in Patients with Femoral Neck Fractures—A Nested Case-Control Study. J. Orthop. Surg. Res. 2019, 14, 395. [Google Scholar] [CrossRef] [PubMed]
- Zanna, L.; Innocenti, M.; Secci, G.; Cipolleschi, L.; Carulli, C.; Civinini, R. Acetabular Morphology Predicts the Risk of Dislocation Following Hemiarthroplasty for Femoral Neck Fractures in the Elderly. J. Arthroplast. 2023, 38, 1773–1778. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.B.; Ang, C.L.; Pang, H.N. Acetabular Prosthetic Protrusio after Bipolar Hemi-Arthroplasty of the Hip: Case Report and Review of the Literature. J. Orthop. Case Rep. 2016, 6, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Zi-Sheng, A.; You-Shui, G.; Zhi-Zhen, J.; Ting, Y.; Chang-Qing, Z. Hemiarthroplasty vs. Primary Total Hip Arthroplasty for Displaced Fractures of the Femoral Neck in the Elderly. J. Arthroplast. 2012, 27, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Guo, Z.; Wang, T.; Xing, K.; Wang, W.; Liu, Y.; Xing, J.; Xiang, H.; Wang, J.; Chen, B.; et al. Treatment Trade-Offs and Choices for Femoral Fractures: A Systematic Review and Meta-Analysis. Orthop. Surg. 2025, 17, 1298–1313. [Google Scholar] [CrossRef] [PubMed]
| Authors | Year, Country | Study Type | Total Number of Patients (BH/DM) | Time of Surgery | Age at Surgery * (Years) (BH/DM) | Follow up * (Months) (BH/DM) | Sex (BH/DM) (Men–Women) | Studied Outcomes |
|---|---|---|---|---|---|---|---|---|
| Bensen et al [26]. | 2014, Denmark | RCS | 346 | 2007–2010 | 84.1/75.9 | 25.3/21.7 | 40–131/52–123 | BL, Disl, R & M |
| (171/175) | ||||||||
| Ochi et al. [27] | 2017, Japan | RCS | 53 | 2009–2015 | 80/75.4 | 28.2/15.8 | 4–16/7–26 | BL, Disl, R & M |
| (20/33) | ||||||||
| Boukebous et al. [28] | 2018, France | RCS | 199 | 2010–2015 | 83.3/77.8 | 25.8/24.2 | 28–73/28–70 | Disl, R & M |
| (101/98) | ||||||||
| Kim et al. [29] | 2018, South Korea | RCS | 168 | 2007–2016 | 72.9/73.1 | 22.1/21.7 | 27–57/26–58 | BL, Disl & M, HHS |
| (84/84) | ||||||||
| Fahad et al. [30] | 2019, Pakistan | RCS | 104 | 2015–2017 | 71.1/69.3 | 20.6/10.9 | 31–46/13–14 | M, HHS |
| (77/27) | ||||||||
| Iorio et al. [31] | 2019, Italy | RCT | 60 | 2015–2017 | 83/82 | 12/12 | 13–17/12–18 | Disl, R & M |
| (30/30) | ||||||||
| Ukaj et al. [32] | 2019, Kosovo | RCT | 94 | 2008–2014 | 77.6/78.1 | 36/36 | 32–15/23–24 | BL, Disl, R & M, HHS |
| (47/47) | ||||||||
| Nonne et al. [33] | 2019, Italy | RCS | 148 | 2013–2017 | 86.1/87.6 | 28.3 | 22–66/15–45 | Disl & R |
| (88/60) | ||||||||
| Makeen et al. [34] | 2021, Egypt | RCT | 33 | 2018–2020 | 71.1/70.4 | 24 | 10–7/7–9 | BL, HHS Disl |
| (17/16) | ||||||||
| Bertault-Le Gourrierec et al. [35] | 2022, France | RCS | 265 | 2010–2013 | 85.4/78.5 | 62 | 28–84/42–111 | Disl, R & M |
| (112/153) | ||||||||
| Cnudde et al. [36] | 2022, Sweeden | RCS | 9033 | 2005–2014 | 83.3/77.9 | ≥36 | 2941–5920/70–102 | Disl, R & M |
| (8861/172) | ||||||||
| Rotini et al. [37] | 2022, Italy | RCS | 302 | 2018–2019 | 87/84.8 | ≥6 | 31–62/54–155 | Disl & M |
| (93/209) | ||||||||
| Valcarenghi et al. [38] | 2022, Belgium | RCS | 257 | 2015–2019 | 85/81 | 17.6/18.1 | 26–113/21–97 | Disl, R & M |
| (139/118) | ||||||||
| Pala et al. [39] | 2024, Italy | RCS | 162 | 2020–2022 | 78/74 | 10.3/14.5 | 20–62/19–61 | BL, HHS Disl &R |
| (82/80) | ||||||||
| Heshmat et al. [40] | 2024, Egypt | RCT | 40 | 2018–2021 | 72.5/69 | ≥24 | 9–11/5–15 | BL, HHS Disl & M |
| (20/20) | ||||||||
| Xiao et al. [41] | 2025, China | RCS | 196 | 2017–2021 | 69.1/68.7 | ≥36 | 42–52/43–59 | BL, HHS Disl, R & M |
| (94/102) |
| Authors | Outcomes | ||||
|---|---|---|---|---|---|
| Estimated Blood Loss * (mL) | Dislocation Rate ** | Reoperation Rate ** | Mortality Rate *** | HHS ** | |
| BH–DM | BH–DM | BH–DM | BH–DM | BH–DM | |
| Bensen et al. [26] | 310–424 | 25/171–8/175 | 32/171–16/175 | 50/171–30/175 | N/A |
| Ochi et al. [27] | 148–480 | 0/20–0/33 | 2/20–0/33 | 4/20–2/30 | N/A |
| Boukebous et al. [28] | N/A | 10/101–3/98 | 9/101–7/98 | 22/101–12/98 | N/A |
| Kim et al. [29] | 489–634 | 3/84–2/84 | N/A | 6/84–7/84 | 79.3–83.4 |
| Fahad et al. [30] | N/A | N/A | N/A | 4/77–0/27 | 68.8–76.8 |
| Iorio et al. [31] | N/A | 5/30–0/30 | 1/30–0/30 | 5/30–4/30 | N/A |
| Ukaj et al. [32] | 159–178 | 3/47–0/47 | 4/47–0/47 | 12/47–7/47 | 88.3–92.5 |
| Nonne et al. [33] | N/A | 5/88–0/60 | 4/88–1/60 | N/A | 81.7–79.8 |
| Makeen et al. [34] | 365–528 | 1/16–1/15 | N/A | N/A | 70.4–77.9 |
| Bertault-Le Gourrierec et al. [35] | N/A | 7/112–3/153 | 10/35–9/97 | 102/112–69/152 a | N/A |
| Cnudde et al. [36] | N/A | 293/7876–4/149 | N/A | 36.4–27.9% | N/A |
| Rotini et al. [37] | N/A | 2/93–4/209 | N/A | 15/93–21/209 b | N/A |
| Valcarenghi et al. [38] | N/A | 12/139–2/118 | 26/139–10/118 | 25/139–19/118 | N/A |
| Pala et al. [39] | N/A | 0/82–0/80 | 0/82–3/80 | N/A | 81–87.5 |
| Heshmat et al. [40] | 700–430 | 2/20–0/– | N/A | 1/20–1/20 c | 88–92.5 |
| Xiao et al. [41] | 257–285 | 4/94–2/102 | 1/92–0/102 | 4/94–4/102 | 85–89.5 |
| Author | Surgical Approach (BH/DM) | Operative Time * (minutes) (BH/DM) | Fixation Type ** (%) (BH/DM) | Type of Implants (BH/DM) | Other Technical Considerations | Criteria for Allocation to Either BH, DM |
|---|---|---|---|---|---|---|
| Bensen et al. [26] | PL | 68/74 | US: 94.4/94.6 UC: 98.3 | Stems: Corail/Corail, ANCA-FIT™, Cups: Saturne | PC and SER repair, Limited DM previous experience, MS | Preexisting OA: (DM), SP, Time period: (2007–8: BH, 2009–10:DM) |
| Ochi et al. [27] | DAA | 89.4/108.3 | US: 100 UC: 100 | Stems: Profemur TL, AccoladeTMZF, TriLock Cups: Trident, MDM | Fluoroscopy use, additional cups screws in osteoporotic bone, MS | Time period: (2009–13: BH, 2013–15: DM) |
| Boukebous et al. [28] | PL | 85/102 | US: 22/ 55 UC: 70 | Stems: Sem3 (CS), Louxor (UC), Cups: Galliléa (CC), Evora (UC) | MS | Time period: (2010–13: BHA, 2013–15: DM) |
| Kim et al. [29] | PL | 64.2/77.3 | US: 100 UC: 100 | Stems: Accolade TMZF Cups: Trident PSL MDM | PC and SER repair, fluoroscopy use, SS | Time period: (2007–13: BH 2013–16: DM) |
| Fahad et al. [30] | DL, PL | N/A | US: 100 UC: 100 | Stems: porous coated Cups: titanium alloy with HY coating | Cups stabilisation with two pegs and a screw, MS | N/A |
| Iorio et al. [31] | DL | 48/59 | US: 100 UC: 100 | Stems: Excia/Pavi Cups: Quattro | N/A | -Randomisation |
| Ukaj et al. [32] | PL | 57.8/63.7 | US: 34.4 UC: 100 | Stems: Pavi Cups: Quattro | PC repair, Cups stabilisation with six fins & four spikes, SS | -Randomisation |
| Nonne et al. [33] | PL | N/A | US: 85.2 UC: 96.7 | Stems: S-Taper, Korus Cups: Dualis | N/A | N/A |
| Makeen et al. [34] | PL | 66/95 | US: N/A UC: 100 | Stems: Exception, CPT/Exception Cups: Serf NOVAE Evolution | -PC and SER repair | -Randomisation |
| Bertault-Le Gourrierec et al. [35] | PL | N/A | US: 25 /85 UC: 92 | Stems: N/A/ Cups: Liberty ATF, Novae SERF, others | MS | SP, Patient factors |
| Cnudde et al. [36] | DL:65.3%, PL:34.7%/ DL:40.1%, PL:59.9% | N/A | US: 0 UC: N/A | N/A | MS and institutions | Institution dependent |
| Rotini et al. [37] | PL | 66.3/78.6 | Both US & CS, (%N/A) Both UC & CC, (%N/A) | Stems: CCA, MS-30, SL/PolarStem, Taperloc, Hype, Apta Fix, Exeter, ABG, Accolade, Apta Cups: PolarCups, Avantage, Novae Stick, Trident, Novae | MS and institutions | SP, Patient factors |
| Valcarenghi et al. [38] | PL | N/A | US: most cases, (%N/A) UC: 100 | N/A | PC and SER repair, MS | Preexisting OA: (DM-THA) SP |
| Pala et al. [39] | DA:4.9%, PL:3.6%, AL: 91.5%/ DA: 27.5%, PL:12.5%, AL:60% | 85/101 | US: 26.8 UC: 100 | Stems: H-max, CL-trauma /Hype Cups: NOVAE SunFit | MS | Patient factors |
| Heshmat et al. [40] | DL | 54.3/81.6 | US: 0 UC: 40 | Stems: N/A Cups: Avantage | MS | -Randomisation |
| Xiao et al. [41] | N/A | 76.8/86.4 | N/A | N/A | N/A | N/A |
| Author | Cognitive Impairment % (BH/DM) | Neuromuscular Deficit % (BH/DM) |
|---|---|---|
| Bensen et al. [26] | N/A | N/A |
| Ochi et al. [27] | N/A | 10/24.2 |
| Boukebous et al. [28] | 50/25 | N/A |
| Kim et al. [29] | 0 * | 0 * |
| Fahad et al. [30] | N/A | N/A |
| Iorio et al. [31] | 100 ** | 0 ** |
| Ukaj et al. [32] | 0 | 0 |
| Nonne et al. [33] | 100 *** | |
| Makeen et al. [34] | N/A | N/A |
| Bertault-Le Gourrierec et al. [35] | 27.2 | 5.8 |
| Cnudde et al. [36] | 100 *** | |
| Rotini et al. [37] | N/A | N/A |
| Valcarenghi et al. [38] | 32/40 | N/A |
| Pala et al. [39] | 0 * | 0 * |
| Heshmat et al. [40] | N/A | N/A |
| Xiao et al. [41] | 0 * | 0 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grammatikopoulos, D.; Pegios, V.F.; Tsotsolis, S.; Kenanidis, E.; Tsiridis, E. Are There Benefits of Total Hip Arthroplasty with Dual-Mobility Cups Compared to Bipolar Hemiarthroplasty for Femoral Neck Fractures in the Geriatric Population? A Systematic Review and Meta-Analysis of Comparative Studies. J. Clin. Med. 2025, 14, 5076. https://doi.org/10.3390/jcm14145076
Grammatikopoulos D, Pegios VF, Tsotsolis S, Kenanidis E, Tsiridis E. Are There Benefits of Total Hip Arthroplasty with Dual-Mobility Cups Compared to Bipolar Hemiarthroplasty for Femoral Neck Fractures in the Geriatric Population? A Systematic Review and Meta-Analysis of Comparative Studies. Journal of Clinical Medicine. 2025; 14(14):5076. https://doi.org/10.3390/jcm14145076
Chicago/Turabian StyleGrammatikopoulos, Dimitrios, Vasileios F. Pegios, Stavros Tsotsolis, Eustathios Kenanidis, and Eleftherios Tsiridis. 2025. "Are There Benefits of Total Hip Arthroplasty with Dual-Mobility Cups Compared to Bipolar Hemiarthroplasty for Femoral Neck Fractures in the Geriatric Population? A Systematic Review and Meta-Analysis of Comparative Studies" Journal of Clinical Medicine 14, no. 14: 5076. https://doi.org/10.3390/jcm14145076
APA StyleGrammatikopoulos, D., Pegios, V. F., Tsotsolis, S., Kenanidis, E., & Tsiridis, E. (2025). Are There Benefits of Total Hip Arthroplasty with Dual-Mobility Cups Compared to Bipolar Hemiarthroplasty for Femoral Neck Fractures in the Geriatric Population? A Systematic Review and Meta-Analysis of Comparative Studies. Journal of Clinical Medicine, 14(14), 5076. https://doi.org/10.3390/jcm14145076