Effectiveness and Safety of Recombinant Zoster Vaccine in Rheumatic Diseases: Real-World Evidence from a Single-Centre Italian Cohort
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Aims and Endpoints
- (1)
- Collect additional safety data on RZV in a large cohort with adequate representation of the main rheumatologic diagnoses and to characterize adverse events reported as adverse events following immunization (AEFI).
- (2)
- Identify potential predictive factors of AEFI among demographic and clinical variables.
2.3. Statistical Analysis
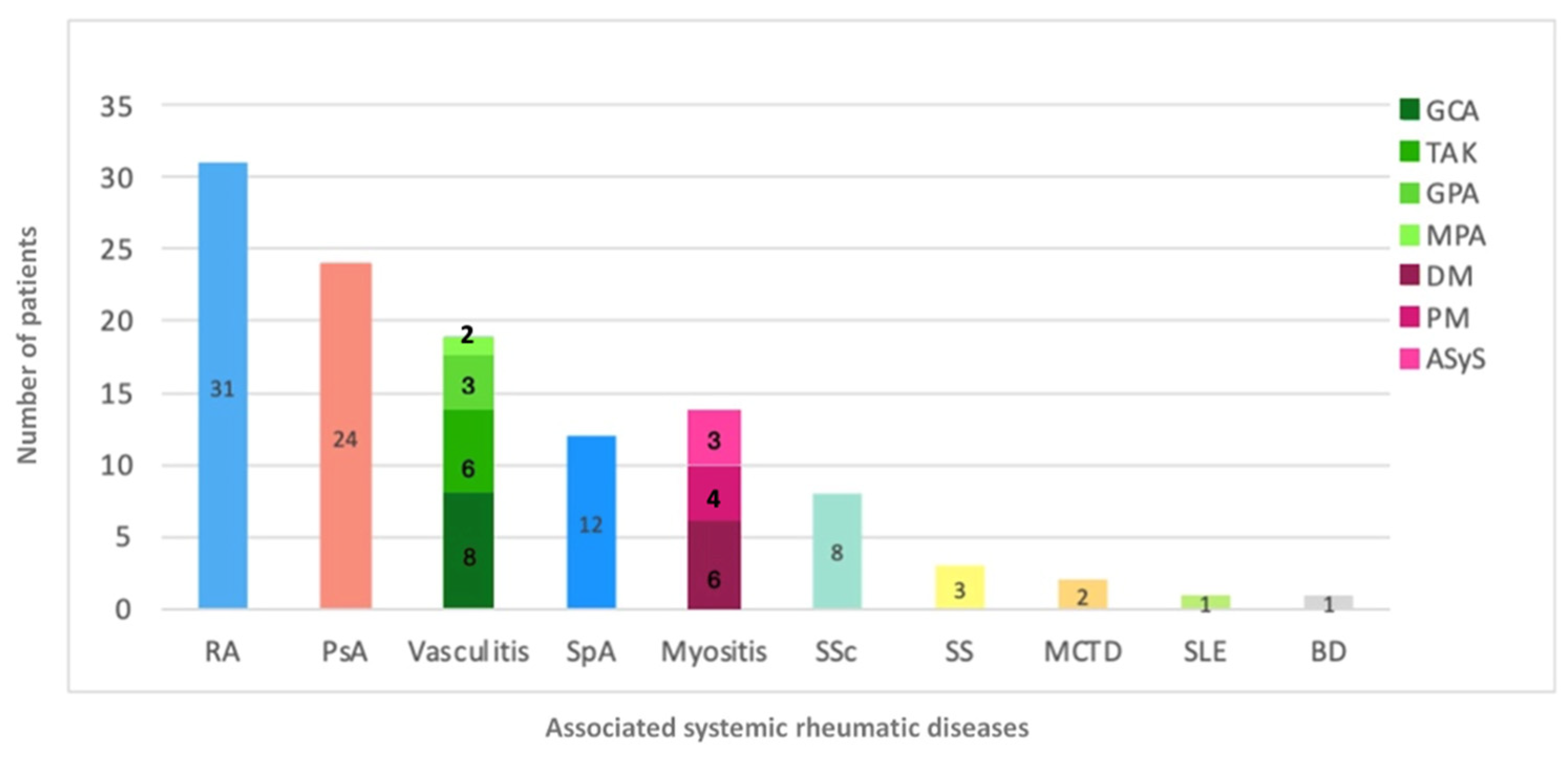
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AEFI | Adverse events following immunization |
| HZ | Herpes Zoster |
| RMDs | Rheumatic Diseases |
| RZV | Recombinant Zoster Vaccine |
References
- Van Oorschot, D. A systematic literature review of herpes zoster incidence worldwide. Hum. Vaccines Immunother. 2021, 17, 1714–1732. [Google Scholar] [CrossRef]
- Marra, F.; Parhar, K.; Huang, B.; Vadlamudi, N. Risk Factors for Herpes Zoster Infection: A Meta-Analysis. Open Forum Infect. Dis. 2020, 7, ofaa005. [Google Scholar] [CrossRef]
- Fan, L.; Wang, Y.; Liu, X.; Guan, X. Association between statin use and herpes zoster: Systematic review and meta-analysis. BMJ Open 2019, 9, e022897. [Google Scholar] [CrossRef]
- Duque, S.; Marinho, A.; Almeida, P.; Marques Pereira, R.; Buzaco, R. Expanding the coverage of herpes zoster vaccination recommendations in European countries: The example of Portugal. Drugs Ther. Perspect. 2025, 41, 34–43. [Google Scholar] [CrossRef]
- Mehta, B.; Pedro, S.; Ozen, G.; Kalil, A.; Wolfe, F.; Mikuls, T.; Michaud, K. Serious infection risk in rheumatoid arthritis compared with non-inflammatory rheumatic and musculoskeletal diseases: A US national cohort study. RMD Open 2019, 5, e000935. [Google Scholar] [CrossRef] [PubMed]
- Germano, V.; Cattaruzza, M.S.; Osborn, J.; Tarantino, A.; Di Rosa, R.; Salemi, S.; D’amelio, R. Infection risk in rheumatoid arthritis and spondyloarthropathy patients under treatment with DMARDs, corticosteroids and TNF-α antagonists. J. Transl. Med. 2014, 12, 77. [Google Scholar] [CrossRef] [PubMed]
- González, C.O.S.; González, J.C.N. JAK kinase inhibitors and varicella zoster virus infection in patients with rheumatoid arthritis. Systematic review of the literature. Reumatol. Clín. (Engl. Ed.) 2022, 18, 453–458. [Google Scholar]
- Furer, V.; Rondaan, C.; Heijstek, M.W.; Agmon-Levin, N.; Van Assen, S.; Bijl, M.; Breedveld, F.C.; D”Amelio, R.; Dougados, M.; Kapetanovic, M.C.; et al. 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann. Rheum. Dis. 2020, 79, 39–52. [Google Scholar] [CrossRef]
- Bass, A.R.; Chakravarty, E.; Akl, E.A.; Bingham, C.O.; Calabrese, L.; Cappelli, L.C.; Johnson, S.R.; Imundo, L.F.; Winthrop, K.L.; Arasaratnam, R.J.; et al. 2022 American College of Rheumatology guideline for vaccinations in patients with rheumatic and musculoskeletal diseases. Arthritis Care Res. 2023, 75, 449–464. [Google Scholar] [CrossRef]
- Harbecke, R.; Cohen, J.I.; Oxman, M.N. Herpes zoster vaccines. J. Infect. Dis. 2021, 224, S429–S442. [Google Scholar] [CrossRef]
- McGirr, A.; Widenmaier, R.; Curran, D.; Espié, E.; Mrkvan, T.; Oostvogels, L.; Simone, B.; McElhaney, J.E.; Burnett, H.; Haeussler, K.; et al. The comparative efficacy and safety of herpes zoster vaccines: A network meta-analysis. Vaccine 2019, 37, 2896–2909. [Google Scholar] [CrossRef]
- Lal, H.; Cunningham, A.L.; Godeaux, O.; Chlibek, R.; Diez-Domingo, J.; Hwang, S.-J.; Levin, M.J.; McElhaney, J.E.; Poder, A.; Puig-Barberà, J.; et al. Efficacy of an adjuvanted herpes zoster subunit vaccine in older adults. N. Engl. J. Med. 2015, 372, 2087–2096. [Google Scholar] [CrossRef]
- Cunningham, A.L.; Lal, H.; Kovac, M.; Chlibek, R.; Hwang, S.-J.; Díez-Domingo, J.; Godeaux, O.; Levin, M.J.; McElhaney, J.E.; Puig-Barberà, J.; et al. Efficacy of the herpes zoster subunit vaccine in adults 70 years of age or older. N. Engl. J. Med. 2016, 375, 1019–1032. [Google Scholar] [CrossRef]
- Dagnew, A.F.; Rausch, D.; Herve, C.; Zahaf, T.; Levin, M.J.; Schuind, A. Efficacy and serious adverse events profile of the adjuvanted recombinant zoster vaccine in adults with pre-existing potential immune-mediated diseases: A pooled post hoc analysis on two parallel randomized trials. Rheumatology 2021, 60, 1226–1233. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.; Zhang, X.; Zhang, L.; Fu, C. Efficacy, effectiveness, and safety of herpes zoster vaccine in the immunocompetent and immunocompromised subjects: A systematic review and network meta-analysis. Front. Immunol. 2022, 13, 978203. [Google Scholar] [CrossRef] [PubMed]
- Lenfant, T.; Jin, Y.; Kirchner, E.; Hajj-Ali, R.A.; Calabrese, L.H.; Calabrese, C. Safety of recombinant zoster vaccine: A retrospective study of 622 rheumatology patients. Rheumatology 2021, 60, 5149–5157. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Amill-Rosario, A.; Johnson, A.; Lee, H.; Spence, O.; Oraichi, D.; Seifert, H.; Franck, V.; Gamble, S.; Yun, H.; et al. Risk of incident gout following exposure to recombinant zoster vaccine in US adults aged ≥ 65 years. Semin. Arthritis Rheum. 2024, 68, 152515. [Google Scholar] [CrossRef]
- Cito, A.; Fornaro, M.; Carenza, A.; Anelli, M.G.; Scioscia, C.; Iannone, F.; Lopalco, G. Turning the tide against herpes zoster in rheumatoid arthritis patients treated with JAK inhibitors. J. Clin. Med. 2024, 13, 4423. [Google Scholar] [CrossRef]
- Chen, P.-K.; Chang, S.-H.; Chen, Y.-M.; Chen, H.-H.; Huang, P.-H.; Huang, C.-C.; Yeo, K.-J.; Lan, J.-L.; Chen, D.-Y. Prior herpes zoster occurrence and high-dose corticosteroids increase herpes zoster risk in rheumatoid arthritis patients receiving janus kinase inhibitors in a retrospective and observational study. Clin. Rheumatol. 2024, 43, 2503–2511. [Google Scholar] [CrossRef]
- Vink, P.; Ramon Torrell, J.M.; Sanchez Fructuoso, A.; Kim, S.-J.; Kim, S.; Zaltzman, J.; Ortiz, F.; Plana, J.M.C.; Rodriguez, A.M.F.; Rodrigo, H.R.; et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in chronically immunosuppressed adults following renal transplant: A phase 3, randomized clinical trial. Clin. Infect. Dis. 2020, 70, 181–190. [Google Scholar] [CrossRef]
- Dagnew, A.F.; Ilhan, O.; Lee, W.-S.; Woszczyk, D.; Kwak, J.-Y.; Bowcock, S.; Sohn, S.K.; Macías, G.R.; Chiou, T.-J.; Quiel, D.; et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in adults with haematological malignancies: A phase 3, randomised, clinical trial and post-hoc efficacy analysis. Lancet Infect. Dis. 2019, 19, 988–1000. [Google Scholar] [CrossRef] [PubMed]
- Pier, M.; Wolbink, G.; Boekel, L. Time to talk to adults with rheumatic diseases about herpes zoster vaccination. Lancet Rheumatol. 2024, 6, e247–e251. [Google Scholar] [CrossRef]
- Nagata, S.; Yokogawa, N. Breakthrough herpes zoster following recombinant zoster vaccinations in a rheumatoid arthritis patient receiving a Janus kinase inhibitor: A case report and literature review. Mod. Rheumatol. Case Rep. 2025, 9, rxaf012. [Google Scholar] [CrossRef]
- Stevens, E.; Weinblatt, M.E.; Massarotti, E.; Griffin, F.; Emani, S.; Desai, S. Safety of the zoster vaccine recombinant adjuvanted in rheumatoid arthritis and other systemic rheumatic disease patients: A single center’s experience with 400 patients. ACR Open Rheumatol. 2020, 2, 357–361. [Google Scholar] [CrossRef]
- Källmark, H.; Bergström, T.; Nagel, J.; Gullstrand, B.; Einarsson, J.T.; A Bengtsson, A.; Kapetanovic, M.C. Serologic immunogenicity and safety of herpes zoster subunit vaccine in patients with rheumatoid arthritis receiving Janus kinase inhibitors. Rheumatology 2024, 63, 2024–2033. [Google Scholar] [CrossRef] [PubMed]
- Pons-Bas, A.; Rosas, J.; Pons-Canet, L.; Senabre-Gallego, J.; Soler, G.S.; Bernal, J.; Cortés-Quiroz, J.C.; Raya-Santos, C.; Gallego-Campuzano, R.; Betoret, M.L. AB1774-HPR safety of the recombinant herpes zoster vaccine in patients with rheumatoid arthritis treated with jaki drugs. Ann. Rheum. Dis. 2023, 82, 2121. [Google Scholar] [CrossRef]
- Kojima, S.; Iwamoto, T.; Kobayashi, Y.; Kato, M.; Takizawa, F.; Ida, T.; Suzuki, J.; Toda, Y.; Miyachi, K.; Iwata, A.; et al. Immunogenicity and influence on disease activity of recombinant zoster vaccine in patients with rheumatoid arthritis treated with DMARDs. RMD Open 2024, 10, e003902. [Google Scholar] [CrossRef] [PubMed]
- Raza, S.; Acharya, S.; Howard, G.; Pattanaik, D. Safety of Recombinant Zoster Vaccine in Rheumatology Patients. South. Med. J. 2022, 115, 125–128. [Google Scholar] [CrossRef]
- Venerito, V.; Stefanizzi, P.; Cantarini, L.; Lavista, M.; Galeone, M.G.; Di Lorenzo, A.; Iannone, F.; Tafuri, S.; Lopalco, G. Immunogenicity and safety of adjuvanted recombinant zoster vaccine in rheumatoid arthritis patients on anti-cellular biologic agents or JAK inhibitors: A prospective observational study. Int. J. Mol. Sci. 2023, 24, 6967. [Google Scholar] [CrossRef] [PubMed]
- Curtis, J.R.; Conrad, D.M.; Krueger, W.S.; Gara, A.P.; Winthrop, K.L. Real-world data on the use of the Shingrix vaccine among patients with inflammatory arthritis and risk of cardiovascular events following herpes zoster. Arthritis Res. Ther. 2025, 27, 108. [Google Scholar] [CrossRef]
- Stefanizzi, P.; Moscara, L.; Palmieri, C.; Martinelli, A.; Di Lorenzo, A.; Venerito, V.; Germinario, C.A.; Tafuri, S. Safety profile of recombinant adjuvanted anti-herpes zoster vaccine (RZV) in high-risk groups: Data from active surveillance program. Puglia (Italy), 2021–2023. Vaccine 2024, 42, 2966–2974. [Google Scholar] [CrossRef]
- Esteban-Vazquez, A.; Steiner, M.; Castañeda, E.; Andreu-Vazquez, C.; Thiussard, I.J.; Somodevilla, A.; Gracia-Martínez, M.; Sánchez-Diaz, R.; García-Yubero, C.; Paredes-Romero, M.B.; et al. The real-world study of immunogenicity and safety of the adjuvant recombinant vaccine against varicella zoster virus in patients with immune-mediated inflammatory diseases treated with Janus kinase inhibitors. Vaccines 2023, 11, 1610. [Google Scholar] [CrossRef] [PubMed]
- Sieiro Santos, C.; Herrero, J.G.; Ordas Martínez, J.; Álvarez Castro, C.; López Robles, A.; Colindres, R.; Martín, E.R.; Sahagun, A.M.; de Morales, J.G.R. Immunogenicity to Herpes Zoster recombinant subunit vaccine in immune-mediated rheumatic patients under treatment with JAK inhibitors. Rheumatology 2025, 64, 2442–2450. [Google Scholar] [CrossRef]
- Winthrop, K.L.; Silverfield, J.; Racewicz, A.; Neal, J.; Lee, E.B.; Hrycaj, P.; Gomez-Reino, J.; Soma, K.; Mebus, C.; Wilkinson, B.; et al. The effect of tofacitinib on pneumococcal and influenza vaccine responses in rheumatoid arthritis. Ann. Rheum. Dis. 2016, 75, 687–695. [Google Scholar] [CrossRef]
- Friedman, M.A.; Curtis, J.R.; Winthrop, K.L. Impact of disease-modifying antirheumatic drugs on vaccine immunogenicity in patients with inflammatory rheumatic and musculoskeletal diseases. Ann. Rheum. Dis. 2021, 80, 1255–1265. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, R.; Fujii, H.; Imai, T.; Furusawa, Y.; Katsushima, M.; Fukumoto, K.; Yamada, Y.; Mamoto, K.; Okano, T.; Yamada, S.; et al. Immune Response to an Adjuvanted Recombinant Zoster Vaccine in Japanese Patients with Rheumatoid Arthritis Receiving Upadacitinib (End Zoster-J Study): Study Protocol for an Exploratory Parallel Triple-Arm Prospective Trial. J. Clin. Med. 2024, 13, 7321. [Google Scholar] [CrossRef]
- Takanashi, S.; Ohmura, K.; Misaki, K.; Ihata, A.; Matsui, T.; Tohma, S.; Saegusa, J.; Sato, S.; Matsubara, T.; Yamaoka, K.; et al. Optimal timing of recombinant herpes zoster virus vaccination for a JAK inhibitor treatment in rheumatoid arthritis: A multicentre, open-label, randomised comparative study (STOP-HZ study): Study protocol. BMJ Open 2024, 14, e090668. [Google Scholar] [CrossRef] [PubMed]
- Kupa, L.V.K.; Medeiros-Ribeiro, A.C.; Aikawa, N.E.; Pasoto, S.G.; Borba, E.F.; Assad, A.P.L.; Carla, C.G.S.; Yuki, E.F.N.; Seguro, L.P.C.; Danieli, A.; et al. Disease Safety, Immunogenicity, and Efficacy of Recombinant Herpes Zoster Vaccine (RZV or Shingrix) in Autoimmune Rheumatic Diseases: Launching a Randomized Phase 4 Study. JCR J. Clin. Rheumatol. 2025, 31, e104–e111. [Google Scholar] [CrossRef]
| Characteristics | Rheumatologic Patients | General Care |
|---|---|---|
| Values, % (n) | Values, % (n) | |
| Total Number | 63.7% (114) | 36.3% (65) |
| Period of observation after first dose of vaccine (years) | 1.9 ± 0.93 | - |
| Period of follow up pre-RZV (years) | 5.69 ± 7.83 | - |
| Mean age ± SD (years) | 61.0 ± 14.3 | 77.0 ± 6.8 |
| Female (n, %) | 71.1% (81) | 44.6% (29) |
| Comorbidities (n, %) | 62.3% (71) | 54.4% (62) |
| Previous malignancies | 1.7% (2) | 12.3% (8) |
| Other inflammatory/autoimmune disorder a | 18.4% (21) | 21.5% (14) |
| Osteoporosis | 16.7% (19) | 0% (0) |
| Fibromyalgia | 4.4% (5) | 0% (0) |
| Previous HZ, % (n) | 34.2% (39) | 50.8% (33) |
| 0, % (n) | 65.8% (75) | 49.2% (32) |
| 1, % (n) | 22.8% (26) | 36.9% (24) |
| 2, % (n) | 7.9% (9) | 10.8% (7) |
| 3, % (n) | 1.7% (2) | 1.7% (2) |
| 4, % (n) | 1.7% (2) | 0% (0) |
| cDMARDs monotherapy, % (n) | 9.6% * (11) | - |
| MTX | 5.3% * (6) | - |
| HCQ | 2.6% * (3) | - |
| LFN | 0.9% * (1) | - |
| APR | 0.9% * (1) | - |
| bDMARDs monotherapy, % (n) | ||
| ADA | 8.8% * (10) | - |
| CZP | 0.9% * (1) | - |
| ETN | 3.5% * (4) | - |
| IFX | 0.9% * (1) | - |
| IXE | 0.9% * (1) | - |
| RTX | 7.0% * (8) | - |
| SEC | 1.7% * (2) | - |
| TCZ | 9.6% * (11) | - |
| JAKi monotherapy, % (n) | 28.1% * (32) | - |
| UPA | 12.3% * (14) | - |
| BARI | 11.4% * (13) | - |
| TOFA | 3.5% * (4) | - |
| FILGO | 0.9% * (1) | - |
| Mycophenolate mofetil, % (n) | 7.9% * (9) | - |
| bDMARDs + MTX, % (n) | 9.6% * (11) | - |
| bDMARDs + other cDMARDs, % (n) | 3.5% * (4) | - |
| JAKi+ MTX | 4.4% * (5) | - |
| JAK i+ other cDMARDs, % (n) | 0.9% * (1) | - |
| Oral GC | 28.1% * (32) | - |
| AEFI * | First Dose | Second Dose | ||||||
|---|---|---|---|---|---|---|---|---|
| Patients | General Care Group | Patients | General Care Gorup | |||||
| n | % | n | % | n | % | n | % | |
| Any reaction | 94 | 82 | 51 | 78.5 | 97 | 85.1 | 53 | 81.5 |
| General disorders | ||||||||
| Injection site reaction | 5 | 4.4 | 2 | 3.1 | 5 | 4.4 | 2 | 3.1 |
| Injection site rash | 0 | 0 | 2 | 3.1 | 0 | 0 | 0 | 0 |
| Fever | 10 | 8.8 | 8 | 12.3 | 7 | 6.1 | 8 | 12.3 |
| Flu-like syndrome | 1 | 0.9 | 0 | 0 | 2 | 1.8 | 0 | 0 |
| Nervous system disorders | ||||||||
| Headache | 1 | 0.9 | 0 | 0 | 1 | 0.9 | 0 | 0 |
| MSK and CTD | ||||||||
| Myalgia | 2 | 1.6 | 1 | 1.5 | 2 | 1.7 | 1 | 1.5 |
| Arthralgia | 1 | 0.9 | 1 | 1.5 | 0 | 0 | 1 | 1.5 |
| Variable | p-Value | Odd Ratio | C.I. |
|---|---|---|---|
| Groups a | 0.326 | 2.028 | 0.495–8.300 |
| Number of attacks before 1st dose of VZV vaccine b | 0.524 | 0.780 | 0.362–1.677 |
| Comorbidities | 0.239 | 0.585 | 0.239–1.429 |
| Advance treatments c | 0.311 | 1.941 | 0.510–7.380 |
| PDN or equivalent | 0.264 | 0.504 | 0.151–1.680 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valentini, S.; Sota, J.; Fineschi, I.; Conticini, E.; Garcia-Gonzalez, E.; D’Ignazio, E.; Bardelli, M.; Gentileschi, S.; Fabbroni, M.; Bellisai, F.; et al. Effectiveness and Safety of Recombinant Zoster Vaccine in Rheumatic Diseases: Real-World Evidence from a Single-Centre Italian Cohort. Vaccines 2025, 13, 1227. https://doi.org/10.3390/vaccines13121227
Valentini S, Sota J, Fineschi I, Conticini E, Garcia-Gonzalez E, D’Ignazio E, Bardelli M, Gentileschi S, Fabbroni M, Bellisai F, et al. Effectiveness and Safety of Recombinant Zoster Vaccine in Rheumatic Diseases: Real-World Evidence from a Single-Centre Italian Cohort. Vaccines. 2025; 13(12):1227. https://doi.org/10.3390/vaccines13121227
Chicago/Turabian StyleValentini, Silvia, Jurgen Sota, Irene Fineschi, Edoardo Conticini, Estrella Garcia-Gonzalez, Emilio D’Ignazio, Marco Bardelli, Stefano Gentileschi, Marta Fabbroni, Francesca Bellisai, and et al. 2025. "Effectiveness and Safety of Recombinant Zoster Vaccine in Rheumatic Diseases: Real-World Evidence from a Single-Centre Italian Cohort" Vaccines 13, no. 12: 1227. https://doi.org/10.3390/vaccines13121227
APA StyleValentini, S., Sota, J., Fineschi, I., Conticini, E., Garcia-Gonzalez, E., D’Ignazio, E., Bardelli, M., Gentileschi, S., Fabbroni, M., Bellisai, F., Falsetti, P., Selvi, E., Cantarini, L., Frediani, B., & Baldi, C. (2025). Effectiveness and Safety of Recombinant Zoster Vaccine in Rheumatic Diseases: Real-World Evidence from a Single-Centre Italian Cohort. Vaccines, 13(12), 1227. https://doi.org/10.3390/vaccines13121227







