Optimized MALDI TOF Mass Spectrometry Identification of Francisella tularensis Subsp. holarctica
Abstract
:1. Introduction
2. Materials and Methods
2.1. Bacterial Strains
2.2. Bacterial Cultures
2.3. Bacterial Inactivation and Protein Extraction
2.4. MALDI TOF ms Procedure
2.5. MALDI TOF ms Francisella Database Building
2.6. MALDI TOF ms Francisella Database Evaluation
3. Results
3.1. F. tularensis LVS Strain Inactivation and MALDI TOF ms Analysis
3.2. F. tularensis LVS Culture Optimization
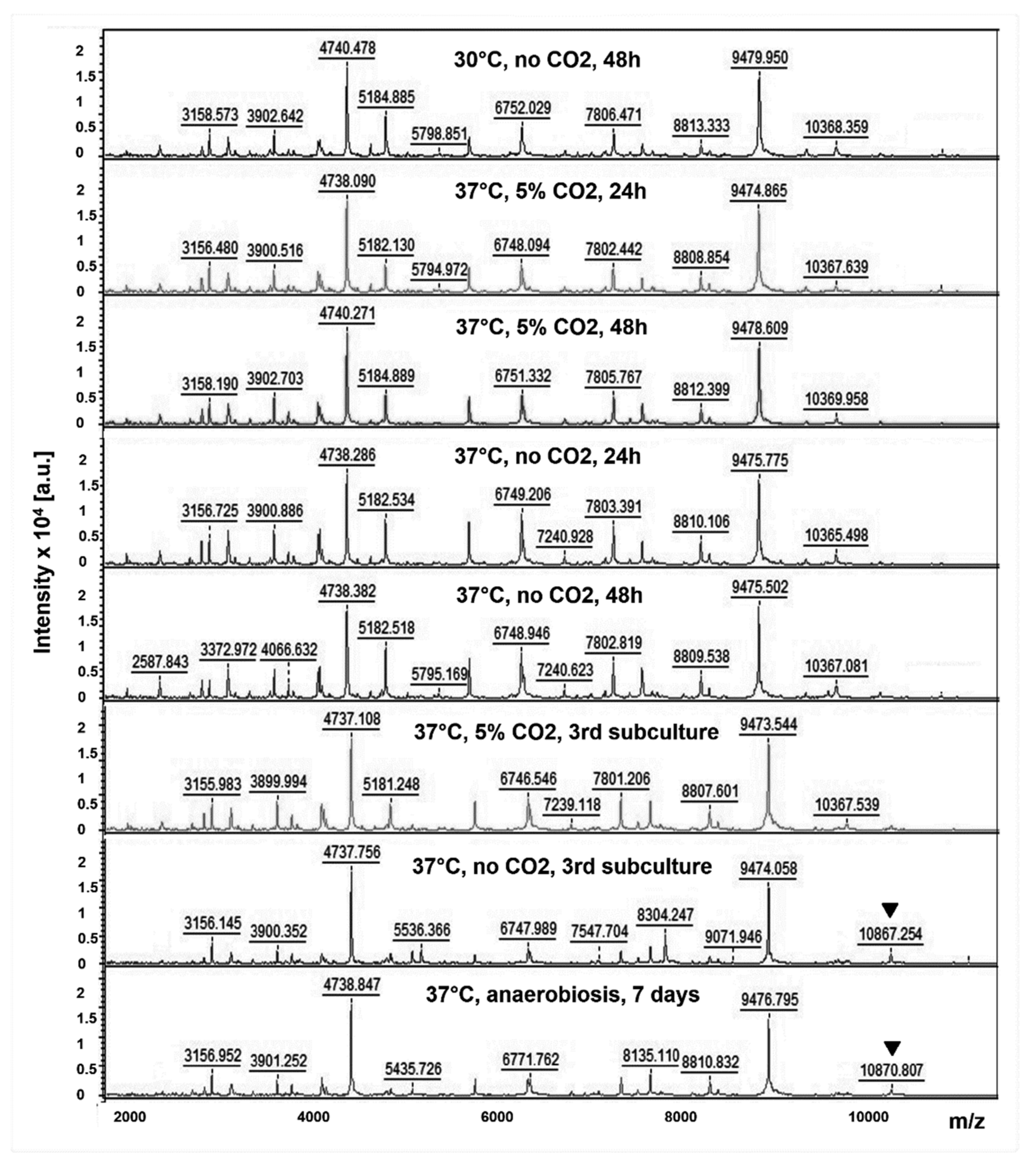
3.3. F. tularensis LVS MALDI TOF Mass Spectra According to Culture Conditions
3.4. Identification of Francisella Strains Using the MBT IVD Database
3.5. Analytical Sensitivity Evaluation of the FNRCT Database
3.6. Analytical Specificity Evaluation of the FNRCT Database
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Maurin, M.; Gyuranecz, M. Tularaemia: Clinical aspects in Europe. Lancet Infect. Dis. 2016, 16, 113–124. [Google Scholar] [CrossRef]
- Maurin, M. Francisella tularensis as a potential agent of bioterrorism? Expert Rev. Anti Infect. Ther. 2015, 13, 141–144. [Google Scholar] [CrossRef]
- Dennis, D.T.; Inglesby, T.V.; Henderson, D.A.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Friedlander, A.M.; Hauer, J.; Layton, M.; et al. Tularemia as a biological weapon: Medical and public health management. JAMA 2001, 285, 2763–2773. [Google Scholar] [CrossRef]
- Aravena-Román, M.; Merritt, A.; Inglis, T.J.J. First case of Francisella bacteraemia in Western Australia. New Microbes New Infect. 2015, 8, 75–77. [Google Scholar] [CrossRef] [Green Version]
- Timofeev, V.; Bakhteeva, I.; Titareva, G.; Kopylov, P.; Christiany, D.; Mokrievich, A.; Dyatlov, I.; Vergnaud, G. Russian isolates enlarge the known geographic diversity of Francisella tularensis subsp. mediasiatica. PLoS ONE 2017, 12, e0183714. [Google Scholar] [CrossRef] [Green Version]
- Brett, M.; Doppalapudi, A.; Respicio-Kingry, L.B.; Myers, D.; Husband, B.; Pollard, K.; Mead, P.; Petersen, J.M.; Whitener, C.J. Francisella novicida bacteremia after a near-drowning accident. J. Clin. Microbiol. 2012, 50, 2826–2829. [Google Scholar] [CrossRef] [Green Version]
- Afset, J.E.; Larssen, K.W.; Bergh, K.; Larkeryd, A.; Sjodin, A.; Johansson, A.; Forsman, M. Phylogeographical pattern of Francisella tularensis in a nationwide outbreak of tularaemia in Norway, 2011. Eurosurveillance 2015, 20, 9–14. [Google Scholar] [CrossRef] [Green Version]
- Johansson, A.; Lärkeryd, A.; Widerström, M.; Mörtberg, S.; Myrtännäs, K.; Ohrman, C.; Birdsell, D.; Keim, P.; Wagner, D.M.; Forsman, M.; et al. An Outbreak of Respiratory Tularemia Caused by Diverse Clones of Francisella tularensis. Clin. Infect. Dis. 2014, 59, 1546–1553. [Google Scholar] [CrossRef] [Green Version]
- Aktas, D.; Celebi, B.; Isik, M.E.; Tutus, C.; Ozturk, H.; Temel, F.; Kizilaslan, M.; Zhu, B.-P. Oropharyngeal Tularemia Outbreak Associated with Drinking Contaminated Tap Water, Turkey, July-September 2013. Emerg. Infect. Dis. 2015, 21, 2194–2196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez-Castrillón, J.L.; Bachiller-Luque, P.; Martín-Luquero, M.; Mena-Martín, F.J.; Herreros, V. Tularemia epidemic in northwestern Spain: Clinical description and therapeutic response. Clin. Infect. Dis. 2001, 33, 573–576. [Google Scholar] [CrossRef]
- Mailles, A.; Vaillant, V. 10 years of surveillance of human tularaemia in France. Eurosurveillance 2014, 19, 20956. [Google Scholar] [CrossRef] [PubMed]
- Hepburn, M.J.; Simpson, A.J.H. Tularemia: Current diagnosis and treatment options. Expert Rev. Anti Infect. Ther. 2008, 6, 231–240. [Google Scholar] [CrossRef] [Green Version]
- Tärnvik, A.; Chu, M.C. New approaches to diagnosis and therapy of tularemia. Ann. N. Y. Acad. Sci. 2007, 1105, 378–404. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Tularaemia; WHO Press: Geneva, Switzerland, 2007. [Google Scholar]
- Shapiro, D.S.; Schwartz, D.R. Exposure of laboratory workers to Francisella tularensis despite a bioterrorism procedure. J. Clin. Microbiol. 2002, 40, 2278–2281. [Google Scholar] [CrossRef] [Green Version]
- Van den Beld, M.J.C.; Reinders, E.; Notermans, D.W.; Reubsaet, F.A.G. Possible misidentification of species in the Pseudomonas fluorescens lineage as Burkholderia pseudomallei and Francisella tularensis, and emended descriptions of Pseudomonas brenneri, Pseudomonas gessardii and Pseudomonas proteolytica. Int. J. Syst. Evol. Microbiol. 2016, 66, 3420–3425. [Google Scholar] [CrossRef]
- Rudrik, J.T.; Soehnlen, M.K.; Perry, M.J.; Sullivan, M.M.; Reiter-Kintz, W.; Lee, P.A.; Pettit, D.; Tran, A.; Swaney, E. Safety and Accuracy of Matrix-Assisted Laser Desorption Ionization-Time of Flight Mass Spectrometry for Identification of Highly Pathogenic Organisms. J. Clin. Microbiol. 2017, 55, 3513–3529. [Google Scholar] [CrossRef] [Green Version]
- Grunow, R.; Splettstoesser, W.; McDonald, S.; Otterbein, C.; O’Brien, T.; Morgan, C.; Aldrich, J.; Hofer, E.; Finke, E.J.; Meyer, H. Detection of Francisella tularensis in biological specimens using a capture enzyme-linked immunosorbent assay, an immunochromatographic handheld assay, and a PCR. Clin. Diagn. Lab. Immunol. 2000, 7, 86–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Splettstoesser, W.D.; Tomaso, H.; Al Dahouk, S.; Neubauer, H.; Schuff-Werner, P. Diagnostic procedures in tularaemia with special focus on molecular and immunological techniques. J. Vet. Med. B Infect. Dis. Vet. Public Health 2005, 52, 249–261. [Google Scholar] [CrossRef]
- Larson, M.A.; Sayood, K.; Bartling, A.M.; Meyer, J.R.; Starr, C.; Baldwin, J.; Dempsey, M.P. Differentiation of Francisella tularensis Subspecies and Subtypes. J. Clin. Microbiol. 2020, 58, e01495-19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birdsell, D.N.; Vogler, A.J.; Buchhagen, J.; Clare, A.; Kaufman, E.; Naumann, A.; Driebe, E.; Wagner, D.M.; Keim, P.S. TaqMan real-time PCR assays for single-nucleotide polymorphisms which identify Francisella tularensis and its subspecies and subpopulations. PLoS ONE 2014, 9, e107964. [Google Scholar] [CrossRef]
- Hou, T.-Y.; Chiang-Ni, C.; Teng, S.-H. Current status of MALDI-TOF mass spectrometry in clinical microbiology. J. Food Drug Anal. 2019, 27, 404–414. [Google Scholar] [CrossRef] [PubMed]
- Angeletti, S.; Ciccozzi, M. Matrix-assisted laser desorption ionization time-of-flight mass spectrometry in clinical microbiology: An updating review. Infect. Genet. Evol. 2019, 76, 104063. [Google Scholar] [CrossRef] [PubMed]
- Schubert, S.; Kostrzewa, M. MALDI-TOF MS in the Microbiology Laboratory: Current Trends. Curr. Issues Mol. Biol. 2017, 23, 17–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Broekhuijsen, M.; Larsson, P.; Johansson, A.; Byström, M.; Eriksson, U.; Larsson, E.; Prior, R.G.; Sjöstedt, A.; Titball, R.W.; Forsman, M. Genome-wide DNA microarray analysis of Francisella tularensis strains demonstrates extensive genetic conservation within the species but identifies regions that are unique to the highly virulent F. tularensis subsp. tularensis. J. Clin. Microbiol. 2003, 41, 2924–2931. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunningham, S.A.; Patel, R. Standard Matrix-Assisted Laser Desorption Ionization-Time of Flight Mass Spectrometry Reagents May Inactivate Potentially Hazardous Bacteria. J. Clin. Microbiol. 2015, 53, 2788–2789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larsson, P.; Svensson, K.; Karlsson, L.; Guala, D.; Granberg, M.; Forsman, M.; Johanssont, A. Canonical insertion-deletion markers for rapid DNA typing of Francisella tularensis. Emerg. Infect. Dis. 2007, 13, 1725–1732. [Google Scholar] [CrossRef]
- Kreitmann, L.; Terriou, L.; Launay, D.; Caspar, Y.; Courcol, R.; Maurin, M.; Lemaître, N. Disseminated Infection Caused by Francisella philomiragia, France. Emerg. Infect. Dis. 2015, 21, 2260–2261. [Google Scholar] [CrossRef]
- Fukuchi, T.; Yanagihara, N.; Imaoka, K.; Sugawara, H. Imported Brucellosis In The Era Of Dramatically Increasing Immigrants And Foreign Travelers From Endemic Areas: Occupational Hazards Of Secondary Infection Among Laboratory Technicians In A Nonendemic Country. Int. Med. Case Rep. J. 2019, 12, 313–317. [Google Scholar] [CrossRef] [Green Version]
- Kostrzewa, M.; Nagy, E.; Schröttner, P.; Pranada, A.B. How MALDI-TOF mass spectrometry can aid the diagnosis of hard-to-identify pathogenic bacteria—The rare and the unknown. Expert Rev. Mol. Diagn. 2019, 19, 667–682. [Google Scholar] [CrossRef]
- Karatuna, O.; Celebi, B.; Can, S.; Akyar, I.; Kilic, S. The use of Matrix-assisted laser desorption ionization-time of flight mass spectrometry in the identification of Francisella tularensis. Bosn. J. Basic Med. Sci. 2016, 16, 132–138. [Google Scholar] [CrossRef]
- Seibold, E.; Maier, T.; Kostrzewa, M.; Zeman, E.; Splettstoesser, W. Identification of Francisella tularensis by whole-cell matrix-assisted laser desorption ionization-time of flight mass spectrometry: Fast, reliable, robust, and cost-effective differentiation on species and subspecies levels. J. Clin. Microbiol. 2010, 48, 1061–1069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lundquist, M.; Caspersen, M.B.; Wikström, P.; Forsman, M. Discrimination of Francisella tularensis subspecies using surface enhanced laser desorption ionization mass spectrometry and multivariate data analysis. FEMS Microbiol. Lett. 2005, 243, 303–310. [Google Scholar] [CrossRef] [Green Version]
- Seibold, E.; Bogumil, R.; Vorderwülbecke, S.; Al Dahouk, S.; Buckendahl, A.; Tomaso, H.; Splettstoesser, W. Optimized application of surface-enhanced laser desorption/ionization time-of-flight MS to differentiate Francisella tularensis at the level of subspecies and individual strains. FEMS Immunol. Med. Microbiol. 2007, 49, 364–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hennebique, A.; Boisset, S.; Maurin, M. Tularemia as a waterborne disease: A review. Emerg. Microbes Infect. 2019, 8, 1027–1042. [Google Scholar] [CrossRef] [PubMed]
| Species | Species |
|---|---|
| Francisella tularensis subsp. holarctica (68 clinical strains) | |
| Francisella tularensis subsp. holarctica LVS | Haemophilus influenzae |
| F. novicida U112 | Haemophilus parainfluenzae |
| F. philomiragia ATCC 25015 | Hafnia alvei |
| Acidovorax temperans | Kingella kingae |
| Acinetobacter baumannii | Klebsiella pneumoniae |
| Acinetobacter pittii | Klebsiella variicola |
| Actinomyces odontolyticus | Lactobacillus rhamnosus |
| Aggregatibacter actinomycetemcomitans | Morganella morganii |
| Aggregatibacter aphrophilus | Neisseria subflava |
| Bacillus subtilis | Neisseria flavescens |
| Bacteroides fragilis | Paenibacillus amylolyticus |
| Bacteroides ovatus | Pediococcus acidilactici |
| Bacteroides thetaiotaomicron | Propionibacterium acnes |
| Bacteroides vulgatus | Proteus mirabilis |
| Brucella melitensis | Pseudomonas aeruginosa |
| Campylobacter jejuni | Serratia ureilytica |
| Capnocytophaga sp. | Sphingomonas paucimobilis |
| Citrobacter amalonaticus | Sphingomonas sp |
| Citrobacter braakii | Staphylococcus aureus |
| Citrobacter freundii | Staphylococcus epidermidis |
| Citrobacter koseri | Staphylococcus haemolyticus |
| Citrobacter sedlakii | Staphylococcus hominis |
| Corynebacterium simulans | Staphylococcus lugdunensis |
| Eikenella corrodens | Staphylococcus pasteuri |
| Enterobacter aerogenes | Staphylococcus warneri |
| Enterobacter asburiae | Streptococcus agalactiae |
| Enterobacter cloacae | Streptococcus constellatus |
| Enterococcus casseliflavus | Streptococcus gallolyticus |
| Enterococcus faecalis | Streptococcus pyogenes |
| Enterococcus faecium | Streptococcus mitis |
| Escherichia coli | Streptococcus oralis |
| Gemella haemolysans | Turicella otitidis |
| Species (Strain) | MBT IVD Score | MBT IVD 2nd Proposal Score | FNRCT Database Score |
|---|---|---|---|
| Haemophilus influenzae | 2.44 | NA | F. tul. novicida, 0.79 |
| Haemophilus influenzae | 2.3 | NA | F. tul. holarctica, 0.49 |
| H. parainfluenzae (1) | 2.51 | H. parainfluenzae, 2.33 | F. tul. holarctica, 0.88 |
| H. parainfluenzae (2) | 2.49 | Pasteurella canis, 1.64 | F. tul. holarctica, 0.9 |
| H. parainfluenzae (3) | 2.28 | H. haemolyticus, 1.6 | F. philomiragia, 0.74 |
| H. parainfluenzae (4) | 2.2 | H. haemolyticus, 1.67 | F. tul. holarctica, 0.7 |
| H. parainfluenzae (5) | 2.01 | Neisseria gonorrheae, 1.39 | F. philomiragia, 0.65 |
| A. actinomycetemcomitans (1) | 2.36 | Sphingomonas yabuuchiae, 1.42 | F. tul. holarctica, 0.72 |
| A. actinomycetemcomitans (2) | 2.27 | Sphingomonas aquatilis, 1.57 | F. tul. holarctica, 0.69 |
| A. actinomycetemcomitans (3) | 2.44 | H. parainfluenzae, 1.41 | F. philomiragia, 0.19 |
| A. actinomycetemcomitans (4) | 2.41 | A. aphrophilus, 1.45 | F. philomiragia, 0.6 |
| A. actinomycetemcomitans (5) | 2.39 | H. influenza, 1.35 | F. tul. holarctica, 0.7 |
| A. aphrophilus (1) | 2.37 | H. haemolyticus, 1.83 | F. tul. holarctica, 0.32 |
| A. aphrophilus (2) | 2.23 | H. haemolyticus, 1.64 | F. philomiragia, 0.51 |
| A. aphrophilus (3) | 2.08 | H. haemolyticus, 1.68 | F. philomiragia, 0.81 |
| A. aphrophilus (4) | 2.05 | A. actinomycetemcomitans, 1.47 | F. tul. holarctica, 0.7 |
| A. aphrophilus (5) | 2.02 | Streptococcus intermedius, 1.61 | F. tul. holarctica, 0.71 |
| Capnocytophaga sp. (1) | 2.21 | Hafnia alvei, 1.35 | F. tul. holarctica, 0.4 |
| Capnocytophaga sp. (2) | 2.09 | Agromyces rhizospherae, 1.35 | F. tul. holarctica, 0.68 |
| Capnocytophaga sp. (3) | 2.01 | Pseudomonas asplenii, 1.39 | F. tul. holarctica, 0.83 |
| Capnocytophaga sp. (4) | 1.97 | Branhamella catarrhalis, 1.39 | F. tul. holarctica, 0.55 |
| C. sputigena | 2.49 | Capnocytophaga ochracea, 1.81 | F. tul. novicida, 0.22 |
| E. corrodens (1) | 2.29 | Burkholderia anthina, 1.51 | F. tul. holarctica, 0.62 |
| E. corrodens (2) | 2.27 | Burkholderia anthina, 1.37 | F. tul. holarctica, 0.4 |
| E. corrodens (3) | 2.13 | Burkholderia cepacia, 1.41 | F. tul. novicida, 0.39 |
| E. corrodens (4) | 2.09 | Neisseria meningitides, 1.41 | LVS, 0.33 |
| E. corrodens (5) | 2.01 | Pseudomonas koreensis, 1.38 | LVS, 0.52 |
| K. kingae (1) | 2.6 | Kingella kingae, 2.43 | F. tul. holarctica, 0.89 |
| K. kingae (2) | 2.46 | Jonesia denitrificans, 1.31 | F. tul. holarctica, 1.2 |
| K. kingae (3) | 2.6 | Kingella kingae, 2.43 | F. tul. holarctica, 1.05 |
| K. kingae (4) | 2.45 | Pseudomonas monteilii, 1.41 | F. tul. holarctica, 0.9 |
| K. kingae (5) | 2.5 | Kingella kingae, 2.5 | F. tul. holarctica, 0.86 |
| B. melitensis M16 | 2.38 | Clostridium botulinum, 0.97, or Bacillus anthracis (0.91–1.09) | F. philomiragia, 0.31–0.59 |
| Species (Number of Strains) | MBT IVD Database Score | Database Score Against One or Several of the Following Francisella Species | ||
|---|---|---|---|---|
| F. tul. holactia | F. tul. novicida | F. philomiragia | ||
| Acidovorax temperans | 2.23 | 0.47 | ||
| Acinetobacter baumannii | 2.35 | 0.16 | ||
| Acinetobacter pittii | 2.3 | 0.52 | ||
| Actinomyces odontolyticus | 2.05 | 0.63 | ||
| Enterobacter cloacae | 2.31 | 0.40 | ||
| Bacteroides fragilis (2) | 2.33 | 0.14 | 0.41 | |
| Bacteroides ovatus | 2.17 | 0.17 | ||
| Bacillus subtilis | 1.93 | 1.06 | ||
| Bacteroides thetaiotaomicron | 2.35 | 0.32 | ||
| Bacteroides vulgatus | 2.62 | 0.33 | ||
| Campylobacter jejuni | 2.11 | |||
| Citrobacter amalonaticus | 2.31 | 0.74 | ||
| Citrobacter braakii | 2.17 | 0.83 | ||
| Citrobacter freundii (4) | 2.07–2.43 | 0.71–0.98 | ||
| Citrobacter koseri | 2.39 | 0.25 | ||
| Citrobacter sedlakii | 2.41 | 0.69 | ||
| Corynebacterium simulans | 2.08 | 0.37 | ||
| Enterobacter aerogenes | 2.25 | 1.01–1.11 | ||
| Enterobacter asburiae | 2.38 | 0.49 | ||
| Enterobacter cloacae (4) | 2.29–2.41 | 0.35–0.59 | 0.13–0.5 | |
| Enterococcus casseliflavus | 2.16–2.22 | 0.69–0.91 | ||
| Enterococcus faecalis (5) | 2.34–2.41 | 0.6 | ||
| Enterococcus faecium (2) | 2.42 | 0.58 | 0.49 | |
| Gemella haemolysans | 2.06 | 0.55 | ||
| Escherichia coli (7) | 2.36–2.55 | 0.56–0.78 | ||
| Hafnia alvei (6) | 2.26–2.6 | 0.37–0.72 | 0.76 | |
| klebsiella pneumoniae (9) | 2.16–2.54 | 0.43–0.92 | ||
| Klebsiella variicola | 2.48 | 0.74 | ||
| Lactobacillus rhamnosus | 2.38 | 0.70 | ||
| Morganella morganii (8) | 2.42–2.6 | 0.57–0.95 | ||
| Neisseria flavescens | 2.14 | 0.25 | ||
| Neisseria subflava | 2.7 | 0.27 | ||
| Paenibacillus amylolyticus | 2.14 | 0.56 | ||
| Pediococcus acidilactici | 2.25 | 0.65 | ||
| Propionibacterium acnes | 2.47 | 0.39 | ||
| Proteus mirabilis (3) | 2.4–2.46 | 0.86–1.07 | ||
| Pseudomonas aeruginosa (10) | 2.05–2.51 | 0.22–0.46 | 0.13–0.76 | 0.47–0.60 |
| Serratia ureilytica | 2.32 | 0.47 | ||
| Sphingomonas paucimobilis | 2.48 | 1.03 | ||
| Staphylococcus aureus (12) | 2.26–2.5 | 0.27–0.60 | 0.33–0.6 | |
| Staphylococcus epidermidis (13) | 2.04–2.23 | 0.1–0.7 | ||
| Staphylococcus haemolyticus (2) | 2.13–2.33 | 0.58–0.59 | ||
| Staphylococcus hominis | 2.21 | 0.54 | ||
| Staphylococcus lugdunensis (3) | 2.06–2.25 | 0.45 | 0.74 | |
| Staphylococcus pasteuri | 2.12 | 0.47 | ||
| Staphylococcus warneri (2) | 2.09–2.1 | 0.54–0.73 | ||
| Streptococcus agalactiae | 2.35 | 0.34 | ||
| Streptococcus anginosus | 2.06 | 0.90 | ||
| Streptococcus constellatus (2) | 2.13–2.24 | 1.11–1.13 | ||
| Streptococcus gallolyticus | 2.25 | 0.73 | ||
| Streptococcus mitis | 2.01 | 0.92 | ||
| Streptococcus oralis | 2.14 | 0.68 | ||
| Streptococcus pyogenes (2) | 2.42–2.44 | 0.78–0.98 | ||
| Turicella otitidis | 2.07 | 0.35 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Regoui, S.; Hennebique, A.; Girard, T.; Boisset, S.; Caspar, Y.; Maurin, M. Optimized MALDI TOF Mass Spectrometry Identification of Francisella tularensis Subsp. holarctica. Microorganisms 2020, 8, 1143. https://doi.org/10.3390/microorganisms8081143
Regoui S, Hennebique A, Girard T, Boisset S, Caspar Y, Maurin M. Optimized MALDI TOF Mass Spectrometry Identification of Francisella tularensis Subsp. holarctica. Microorganisms. 2020; 8(8):1143. https://doi.org/10.3390/microorganisms8081143
Chicago/Turabian StyleRegoui, Sofiane, Aurélie Hennebique, Thomas Girard, Sandrine Boisset, Yvan Caspar, and Max Maurin. 2020. "Optimized MALDI TOF Mass Spectrometry Identification of Francisella tularensis Subsp. holarctica" Microorganisms 8, no. 8: 1143. https://doi.org/10.3390/microorganisms8081143
APA StyleRegoui, S., Hennebique, A., Girard, T., Boisset, S., Caspar, Y., & Maurin, M. (2020). Optimized MALDI TOF Mass Spectrometry Identification of Francisella tularensis Subsp. holarctica. Microorganisms, 8(8), 1143. https://doi.org/10.3390/microorganisms8081143






