Acromio-Humeral Distance Is Associated with Shoulder External Strength in National Elite Badminton Players—A Preliminary Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
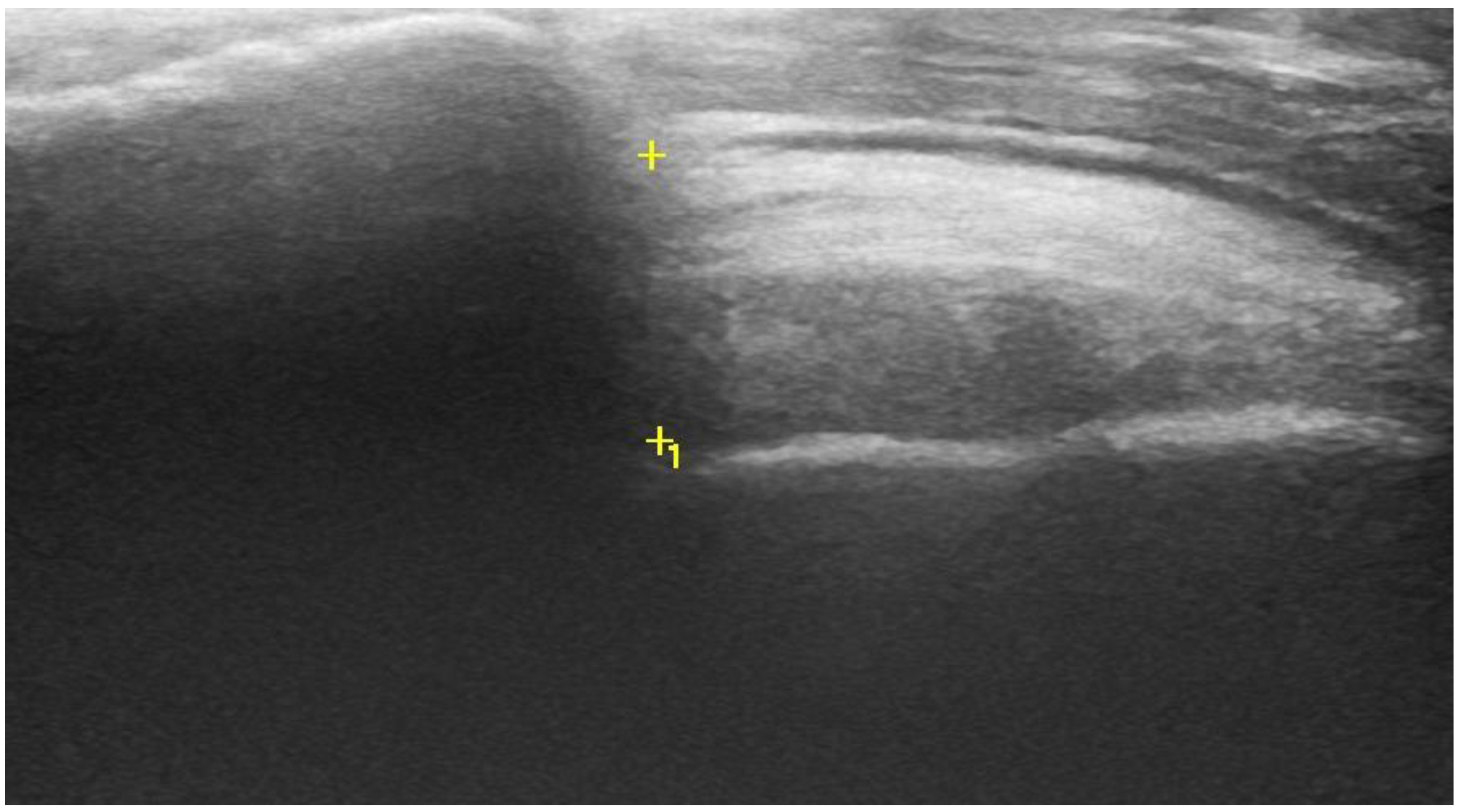
2.2. Acromiohumeral Distance (AHD)
2.3. Shoulder Rotational Strength
2.4. Statistical Analysis
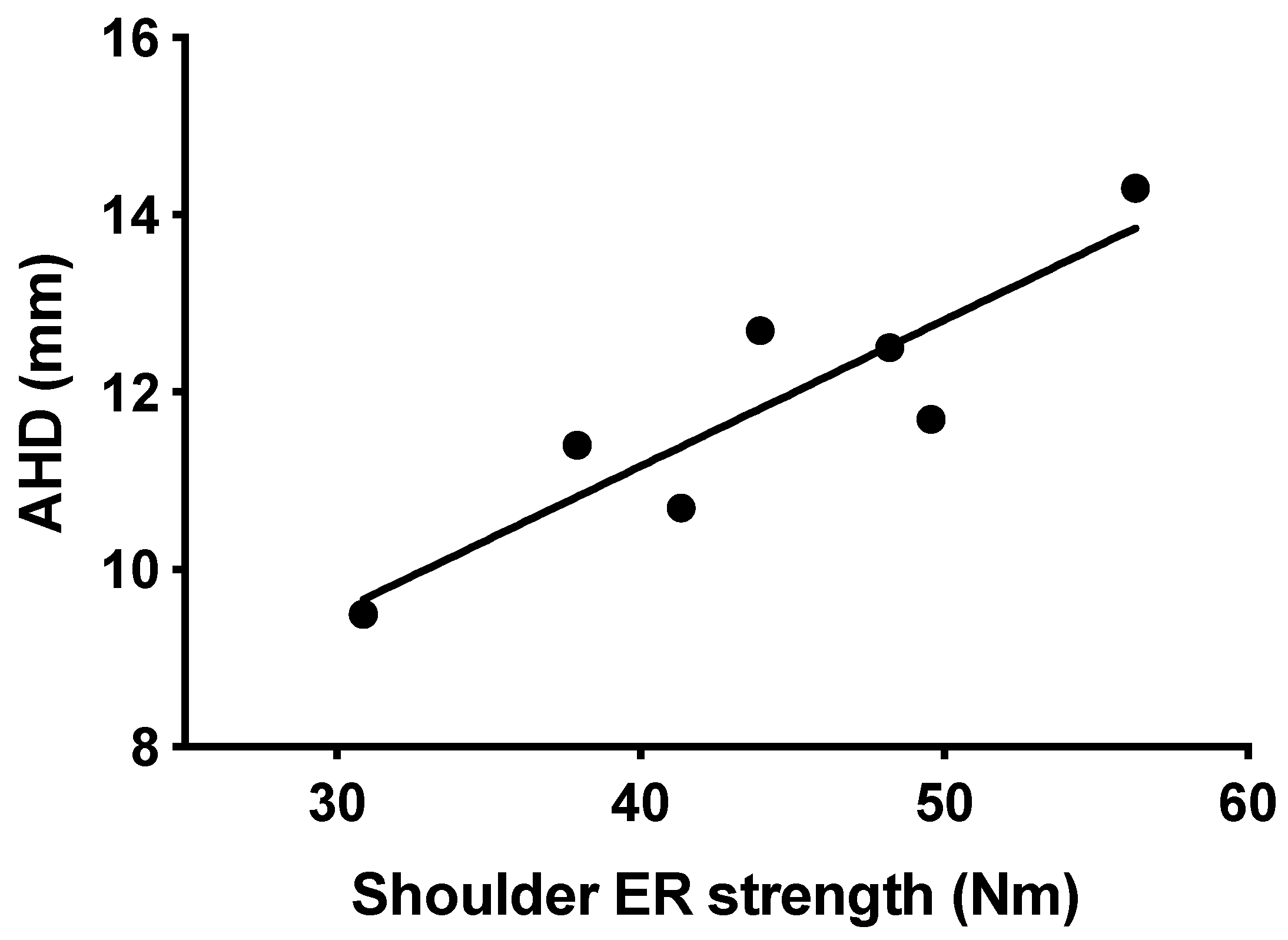
3. Results
4. Discussion
4.1. AHD
4.2. Shoulder Rotational Strength Profile
4.3. Correlation between AHD and ER Strength
4.4. Limitations
4.5. Practical Applications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jørgensen, U.; Winge, S. Epidemiology of Badminton Injuries. Int. J. Sports Med. 1987, 8, 379–382. [Google Scholar] [CrossRef]
- Fahlstrom, M.; Yeap, J.S.; Alfredson, H.; Soderman, K. Shoulder pain—A common problem in world-class badminton players. Scand. J. Med. Sci. Sports 2006, 16, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Fahlström, M.; Söderman, K. Decreased shoulder function and pain common in recreational badminton players. Scand. J. Med. Sci. Sports 2006, 17, 246–251. [Google Scholar] [CrossRef]
- Urwin, M.; Symmons, D.; Allison, T.; Brammah, T.; Busby, H.; Roxby, M.; Simmons, A.W.G. Estimating the burden of muskuloskeletal disorders in the community: The comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann. Rheum. Dis. 1998, 57, 649–655. [Google Scholar] [CrossRef]
- Meister, K. Injuries to the shoulder in the throwing athlete. Part one: Biomechanics/pathophysiology/classification of injury. Am. J. Sport Med. 2000, 28, 265–275. [Google Scholar] [CrossRef]
- Donatelli, R.; Ellenbecker, T.S.; Ekedahl, S.R.; Wilkes, J.S.; Kocher, K.A.J. Assessment of shoulder strength in professional baseball pitchers. J. Orthop. Sport Phys. Ther. 2000, 30, 544–551. [Google Scholar] [CrossRef] [PubMed]
- Leong, H.-T.; Tsui, S.; Ying, M.; Leung, V.Y.-F.; Fu, S.N. Ultrasound measurements on acromio-humeral distance and supraspinatus tendon thickness: Test–retest reliability and correlations with shoulder rotational strengths. J. Sci. Med. Sport 2012, 15, 284–291. [Google Scholar] [CrossRef]
- Ng, G.Y.; Lam, P.C. A Study of antagonist/agonist isokinetic work ratios of shoulder rotators in men who play badminton. J. Orthop. Sports Phys. Ther. 2002, 32, 399–404. [Google Scholar] [CrossRef] [Green Version]
- Couppé, C.; Thorborg, K.; Hansen, M.; Fahlström, M.; Bjordal, J.M.; Nielsen, D.; Baun, M.; Storgaard, M.; Magnusson, S.P. Shoulder rotational profiles in young healthy elite female and male badminton players. Scand. J. Med. Sci. Sports 2012, 24, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Byram, I.R.; Bushnell, B.D.; Dugger, K.; Charron, K.; Harrell, F.E.; Noonan, T.J. Preseason shoulder strength measurements in professional baseball pitchers. Am. J. Sports Med. 2010, 38, 1375–1382. [Google Scholar] [CrossRef]
- Clarsen, B.; Bahr, R.; Andersson, S.H.; Munk, R.; Myklebust, G. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: A prospective cohort study. Br. J. Sports Med. 2014, 48, 1327–1333. [Google Scholar] [CrossRef] [PubMed]
- Møller, M.; Nielsen, O.R.; Attermann, J.; Wedderkopp, N.; Lind, M.; Sørensen, H.; Myklebust, G. Handball load and shoulder injury rate: A 31-week cohort study of 679 elite youth handball players. Br. J. Sports Med. 2017, 51, 231–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cools, A.M.; Michener, A.L. Shoulder pain: Can one label satisfy everyone and everything? Br. J. Sports Med. 2016, 51, 416–417. [Google Scholar] [CrossRef]
- Belley, A.F.; Gagnon, D.H.; Routhier, F.; Roy, J.-S. Ultrasonographic measures of the acromiohumeral distance and supraspinatus tendon thickness in manual wheelchair users with spinal cord injury. Arch. Phys. Med. Rehabil. 2017, 98, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Saupe, N.; Pfirrmann, C.W.A.; Schmid, M.R.; Jost, B.; Werner, C.M.L.; Zanetti, M. Association between rotator cuff abnormalities and reduced acromiohumeral distance. Am. J. Roentgenol. 2006, 187, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Cholewinski, J.J.; Kusz, D.J.; Wojciechowski, P.; Cielinski, L.S.; Zoladz, M.P. Ultrasound measurement of rotator cuff thickness and acromio-humeral distance in the diagnosis of subacromial impingement syndrome of the shoulder. Knee Surg. Sports Traumatol. Arthrosc. 2007, 16, 408–414. [Google Scholar] [CrossRef]
- Maenhout, A.; Van Eessel, V.; Van Dyck, L.; Vanraes, A.; Cools, A. Quantifying acromiohumeral distance in overhead athletes with glenohumeral internal rotation loss and the influence of a stretching program. Am. J. Sports Med. 2012, 40, 2105–2112. [Google Scholar] [CrossRef]
- Harput, G.; Guney, H.; Toprak, U.; Kaya, T.; Colakoglu, F.F.; Baltaci, G. Shoulder-rotator strength, range of motion, and acromiohumeral distance in asymptomatic adolescent volleyball attackers. J. Athl. Train. 2016, 51, 733–738. [Google Scholar] [CrossRef] [Green Version]
- Silva, R.T.; Hartmann, L.G.; Laurino, C.F.D.S.; Bilo, J.P.R. Clinical and ultrasonographic correlation between scapular dyskinesia and subacromial space measurement among junior elite tennis players. Br. J. Sports Med. 2010, 44, 407–410. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.-K.; Lin, J.-J.; Pan, S.-L.; Wang, T.-G. Sonographic evaluations in elite college baseball athletes. Scand. J. Med. Sci. Sports 2005, 15, 29–35. [Google Scholar] [CrossRef]
- Maenhout, A.; Van Cingel, R.; De Mey, K.; Van Herzeele, M.; Dhooge, F.; Cools, A. Sonographic evaluation of the acromiohumeral distance in elite and recreational female overhead athletes. Clin. J. Sport Med. 2013, 23, 178–183. [Google Scholar] [CrossRef]
- Couppé, C.; Kongsgaard, M.; Aagaard, P.; Hansen, P.; Bojsen-Moller, J.; Kjaer, M.; Magnusson, S.P. Habitual loading results in tendon hypertrophy and increased stiffness of the human patellar tendon. J. Appl. Physiol. 2008, 105, 805–810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kongsgaard, M.; Reitelseder, S.; Pedersen, T.G.; Holm, L.; Aagaard, P.; Kjaer, M.; Magnusson, S.P. Region specific patellar tendon hypertrophy in humans following resistance training. Acta Physiol. 2007, 191, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Wiesinger, H.-P.; Rieder, F.; Kösters, A.; Müller, E.; Seynnes, O.R. Are sport-specific profiles of tendon stiffness and cross-sectional area determined by structural or functional integrity? PLoS ONE 2016, 11, e0158441. [Google Scholar] [CrossRef] [Green Version]
- Magnusson, S.P.; Kjaer, M. The impact of loading, unloading, ageing and injury on the human tendon. J. Physiol. 2019, 597, 1283–1298. [Google Scholar] [CrossRef] [Green Version]
- Arampatzis, A.; Karamanidis, K.; Albracht, K. Adaptational responses of the human Achilles tendon by modulation of the applied cyclic strain magnitude. J. Exp. Biol. 2007, 210, 2743–2753. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCreesh, K.M.; Purtill, H.; Donnelly, A.E.; Lewis, J.S. Increased supraspinatus tendon thickness following fatigue loading in rotator cuff tendinopathy: Potential implications for exercise therapy. BMJ Open Sport Exerc. Med. 2017, 3, e000279. [Google Scholar] [CrossRef] [Green Version]
- Desmeules, F.; Minville, L.; Riederer, B.; Côté, C.H.; Frémont, P. Acromio-humeral distance variation measured by ultrasonography and its association with the outcome of rehabilitation for shoulder impingement syndrome. Clin. J. Sport Med. 2004, 14, 197–205. [Google Scholar] [CrossRef]
- Tyler, T.F.; Nahow, R.C.; Nicholas, S.J.; McHugh, M.P. Quantifying shoulder rotation weakness in patients with shoulder impingement. J. Shoulder Elb. Surg. 2005, 14, 570–574. [Google Scholar] [CrossRef]
- Joensen, J.; Couppe, C.; Bjordal, J.M. Increased palpation tenderness and muscle strength deficit in the prediction of tendon hypertrophy in symptomatic unilateral shoulder tendinopathy: An ultrasonographic study. Physiotherapy 2009, 95, 83–93. [Google Scholar] [CrossRef]
- Couppé, C.; Kongsgaard, M.; Aagaard, P.; Vinther, A.; Boesen, M.; Kjaer, M.; Magnusson, S.P. Differences in tendon properties in elite badminton players with or without patellar tendinopathy. Scand. J. Med. Sci. Sports 2012, 23, e89–e95. [Google Scholar] [CrossRef]
- Ocguder, D.A.; Tosun, O.; Bektaser, B.; Cicek, N.; Ipek, A.; Bozkurt, M. Ultrasonographic evaluation of the shoulder in asymptomatic overhead athletes. Acta Orthop. Belg. 2010, 76, 456–461. [Google Scholar] [PubMed]
- Langberg, H.; Skovgaard, D.; Petersen, L.J.; Bülow, J.; Kjaer, M. Type I collagen synthesis and degradation in peritendinous tissue after exercise determined by microdialysis in humans. J. Physiol. 1999, 521, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Gumucio, J.P.; Phan, A.C.; Ruehlmann, D.G.; Noah, A.C.; Mendias, C.L. Synergist ablation induces rapid tendon growth through the synthesis of a neotendon matrix. J. Appl. Physiol. 2014, 117, 1287–1291. [Google Scholar] [CrossRef] [Green Version]
- Tyler, T.F.; Mullaney, M.J.; Mirabella, M.R.; Nicholas, S.J.; McHugh, M.P. Risk factors for shoulder and elbow injuries in high school baseball pitchers. Am. J. Sports Med. 2014, 42, 1993–1999. [Google Scholar] [CrossRef] [PubMed]
- Daghir, A.A.; Sookur, P.A.; Shah, S.; Watson, M. Dynamic ultrasound of the subacromial–subdeltoid bursa in patients with shoulder impingement: A comparison with normal volunteers. Skelet. Radiol. 2012, 41, 1047–1053. [Google Scholar] [CrossRef]
- Ohya, N.; Yamada, T.; Satoh, Y.; Kawamura, H. Relative and absolute reliability of ultrasound measurements for the thickness of the soft tissue around the shoulder joint of young normal subjects. J. Phys. Ther. Sci. 2017, 29, 754–759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maenhout, A.; Dhooge, F.; Van Herzeele, M.; Palmans, T.; Cools, A. Acromiohumeral distance and 3-dimensional scapular position change after overhead muscle fatigue. J. Athl. Train. 2015, 50, 281–288. [Google Scholar] [CrossRef] [Green Version]

| Characteristics | National Badminton Players (n = 7) | |||||||
|---|---|---|---|---|---|---|---|---|
| Male (n = 5) | Female (n = 2) | |||||||
| Player 1 | Player 2 | Player 3 | Player 4 | Player 5 | Player 1 | Player 2 | Mean ± SD | |
| Age (years) | 28 | 20 | 31 | 22 | 23 | 21 | 22 | 24 ± 4 |
| Weight (kg) | 75 | 87 | 78 | 71 | 85 | 69 | 75 | 77 ± 7 |
| Height (m) | 1.82 | 1.95 | 1.81 | 1.85 | 1.89 | 1.73 | 1.83 | 1.84 ± 0.07 |
| BMI (kg/m2) | 23 | 23 | 23 | 21 | 24 | 23 | 23 | 23 ± 1 |
| Forearm length (m) | 0.26 | 0.28 | 0.26 | 0.26 | 0.27 | 0.24 | 0.25 | 0.26 ± 0.01 |
| Measurements | National Badminton Players (n = 7) | |||||||
|---|---|---|---|---|---|---|---|---|
| Male (n = 5) | Female (n = 2) | |||||||
| Player 1 | Player 2 | Player 3 | Player 4 | Player 5 | Player 1 | Player 2 | Mean ± SEM | |
| AHD (mm) | ||||||||
| Dominant | 13 | 12 | 14 | 11 | 13 | 11 | 10 | 11.8 ± 0.6 * |
| Nondominant | 10 | 11 | 11 | 10 | 9 | 10 | 9 | 10 ± 0.4 |
| ER strength (Nm) | ||||||||
| Dominant | 44 | 50 | 56 | 41 | 48 | 38 | 31 | 44 ± 3 |
| Nondominant | 38 | 52 | 57 | 47 | 49 | 32 | 32 | 44 ± 4 |
| IR strength (Nm) | ||||||||
| Dominant | 56 | 70 | 50 | 53 | 58 | 43 | 46 | 54 ± 3 # |
| Nondominant | 50 | 57 | 53 | 50 | 55 | 39 | 34 | 48 ± 3 |
| ER/IR strength-ratio | ||||||||
| Dominant | 0.78 | 0.70 | 1.12 | 0.78 | 0.84 | 0.89 | 0.67 | 0.83 ± 0.06 |
| Nondominant | 0.77 | 0.92 | 1.06 | 0.94 | 0.89 | 0.83 | 0.97 | 0.91 ± 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmidt, S.V.; Engelhardt, J.A.; Cools, A.; Magnusson, S.P.; Couppé, C. Acromio-Humeral Distance Is Associated with Shoulder External Strength in National Elite Badminton Players—A Preliminary Study. Sports 2021, 9, 48. https://doi.org/10.3390/sports9040048
Schmidt SV, Engelhardt JA, Cools A, Magnusson SP, Couppé C. Acromio-Humeral Distance Is Associated with Shoulder External Strength in National Elite Badminton Players—A Preliminary Study. Sports. 2021; 9(4):48. https://doi.org/10.3390/sports9040048
Chicago/Turabian StyleSchmidt, Simon Vadstrup, Jannik Andersen Engelhardt, Ann Cools, Stig Peter Magnusson, and Christian Couppé. 2021. "Acromio-Humeral Distance Is Associated with Shoulder External Strength in National Elite Badminton Players—A Preliminary Study" Sports 9, no. 4: 48. https://doi.org/10.3390/sports9040048






