Turbans vs. Helmets: A Systematic Narrative Review of the Literature on Head Injuries and Impact Loci of Cranial Trauma in Several Recreational Outdoor Sports
Abstract
:1. Introduction
Social Relevance of the Narrative Review
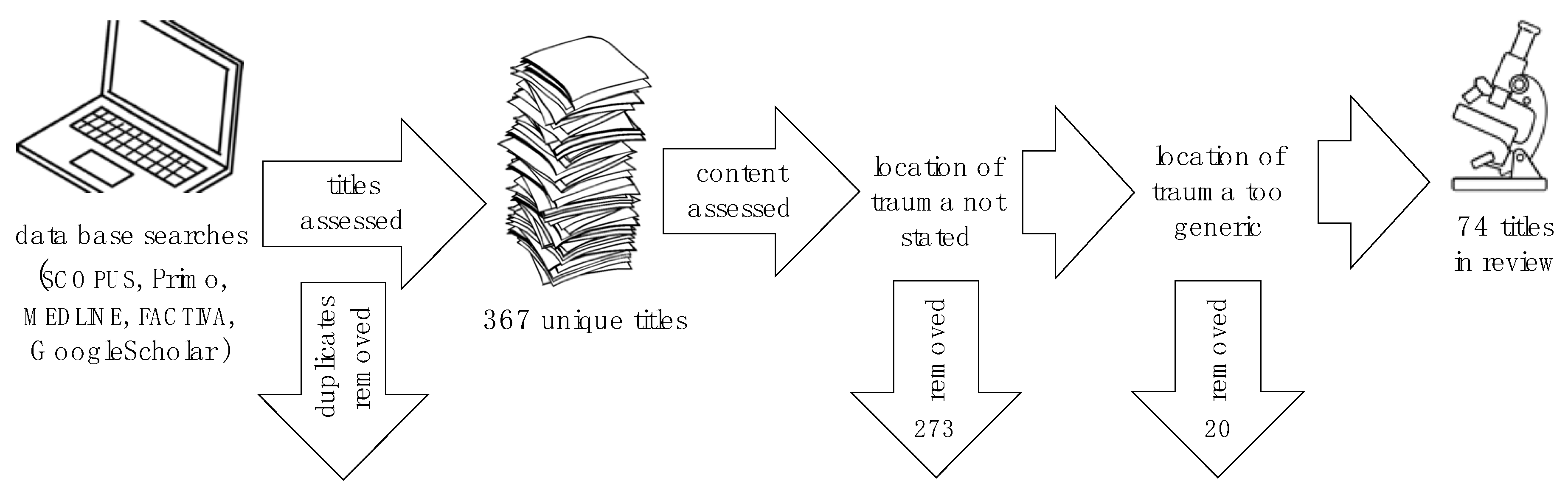
2. Methodology
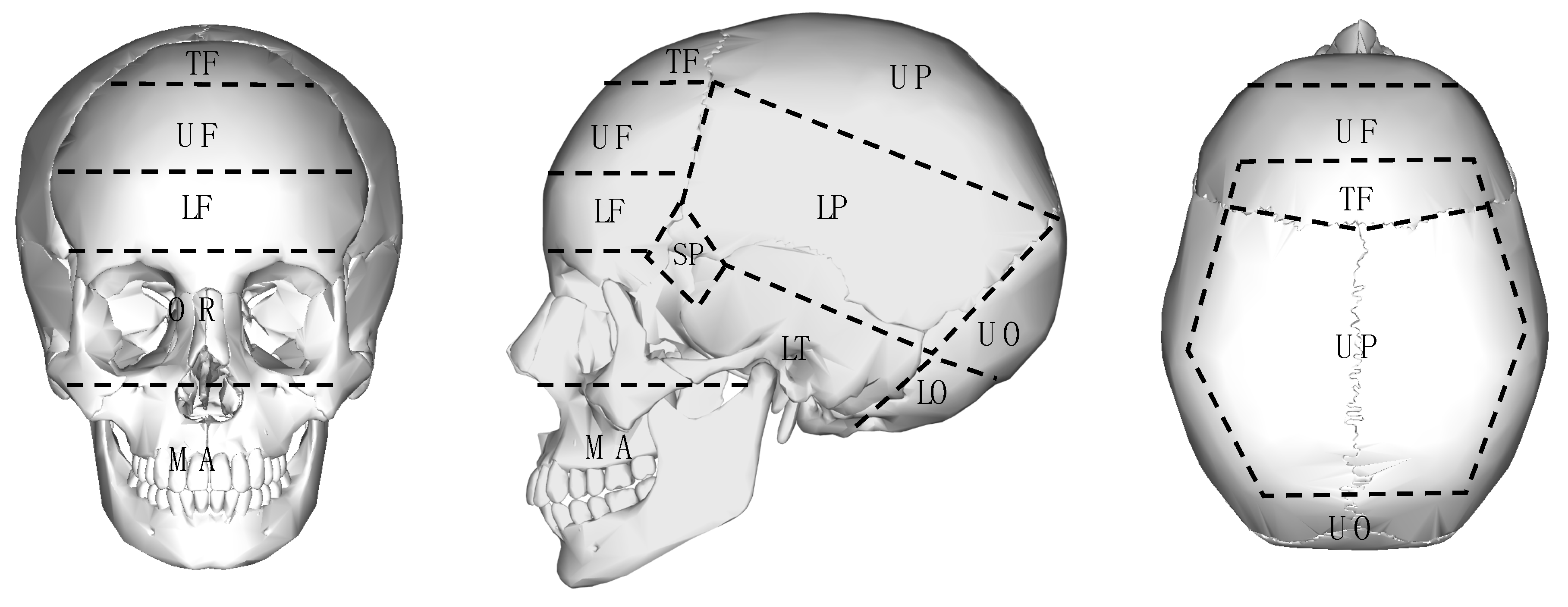
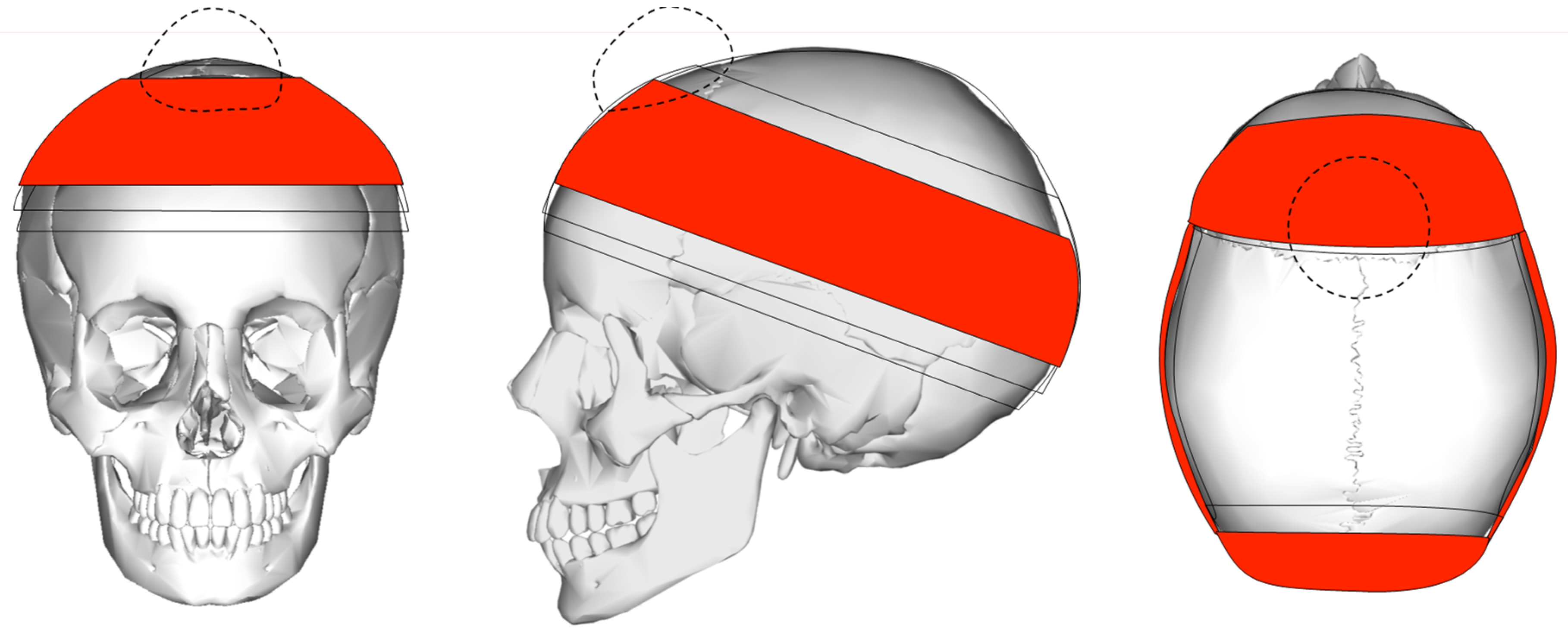
2.1. Injury Locus Classification
2.2. Impact Attenuation
3. Results: Traumatic Head Injuries in Various Outdoor Sports
3.1. Rock and Ice Climbing
3.2. Wheeled Sports
3.2.1. Mountain and Trail Biking
3.2.2. Scooters
3.2.3. Skateboarding
3.2.4. Skating
3.3. Aerial Sports
3.3.1. Hang-Gliding and Paragliding
3.3.2. Sky-Diving
3.3.3. BASE Jumping
3.4. Winter Sports
3.4.1. Downhill Skiing
3.4.2. Cross-Country Skiing
3.4.3. Snowboarding
3.4.4. Sledding
3.4.5. Curling
3.5. Water Sports
3.5.1. Surfing
3.5.2. Wind and Kitesurfing
3.5.3. White-Water Kayaking and Rafting
3.6. Animal-Based Sports
Equestrian
4. Discussion
Protective Potential of Turbans
5. Future Research
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spennemann, D.H.R. Would turbans provide protection against cranial trauma in the construction industry? A review. J. Punjab Acad. Forensic Med. Toxicol. 2020, 21. in press. [Google Scholar]
- Spennemann, D.H.R. Do turbans provide protection against cranial trauma in two-wheeler accidents? A review of the Indian medical literature. Indian J. Forensic Med. Toxicol. 2020, 14, 938–944. [Google Scholar]
- Sood, S. Survey of factors influencing injury among riders involved in motorized two-wheeler accidents in India: A prospective study of 302 cases. J. Trauma 1988, 28, 530–534. [Google Scholar] [CrossRef]
- McLeod, W.H. The Five Ks of the Khalsa Sikhs. J. Am. Orient. Soc. 2008, 128, 325–331. [Google Scholar]
- Spennemann, D.H.R. Turbans vs. Helmets: The conflict between the mandatory wearing of protective head-gear and the freedom of religious expression. Sikh Form. 2020, 17, 207–244. [Google Scholar] [CrossRef]
- McLeod, W.H. Punjabis in New Zealand. A History of Punjabi Migration 1890–1940; Guru Nanak Dev University: Amritsar, India, 1986; Volume 199, p. 9. [Google Scholar]
- Judge, P.S. Social construction of identity in a multicultural state: Sikhs in Canada. Econ. Political Wkly. 2003, 38, 1725–1731. [Google Scholar]
- Spennemann, D.H.R. Slamming the door shut: Patterns of Punjabi immigration to Victoria (Australia) during the late nineteenth and early twentieth century. South Asian Diaspora 2020, 13, 129–142. [Google Scholar] [CrossRef]
- Spennemann, D.H.R. Patterns of late nineteenth and early twentieth century land use by Punjabi hawkers in Southern New South Wales, Australia. J. Sikh Punjāb Stud. 2018, 25, 225–273. [Google Scholar]
- Australian Bureau of Statistics. 2071.0—Census of Population and Housing: Reflecting Australia—Stories from the Census, 2016; Australian Bureau of Statistics: Canberra, Australia, 2018. [Google Scholar]
- Australian Bureau of Statistics. Census TableBuilder 206, 2011, 2016; Australian Bureau of Statistics: Canberra, Australia, 2021. [Google Scholar]
- Williams, I.R.; Rose, L.M.; Raniti, M.B.; Waloszek, J.; Dudgeon, P.; Olsson, C.A.; Patton, G.C.; Allen, N.B. The impact of an outdoor adventure program on positive adolescent development: A controlled crossover trial. J. Outdoor Environ. Educ. 2018, 21, 207–236. [Google Scholar] [CrossRef]
- Davidson, L. Qualitative research and making meaning from adventure: A case study of boys’ experiences of outdoor education at school. J. Adventure Educ. Outdoor Learn. 2001, 1, 11–20. [Google Scholar] [CrossRef] [Green Version]
- Passy, R.; Bentsen, P.; Gray, T.; Ho, S. Integrating outdoor learning into the curriculum: An exploration in four nations. Curric. Perspect. 2019, 39, 73–78. [Google Scholar] [CrossRef]
- Wohlin, C. Guidelines for snowballing in systematic literature studies and a replication in software engineering. In Proceedings of the 18th International Conference on Evaluation and Assessment in Software Engineering, London, UK, 13–14 May 2014; ACM: New York, NY, USA, 2014; pp. 38–42. [Google Scholar]
- Atkinson, R.; Flint, J. Accessing hidden and hard-to-reach populations: Snowball research strategies. Soc. Res. Update 2001, 33, 1–4. [Google Scholar]
- Greenhalgh, T.; Peacock, R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: Audit of primary sources. Br. Med. J. 2005, 331, 1064–1065. [Google Scholar] [CrossRef] [Green Version]
- Tominaga, G.T.; Schaffer, K.B.; Dandan, I.S.; Coufal, F.J.; Kraus, J.F. Head injuries in hospital-admitted adolescents and adults with skateboard-related trauma. Brain Inj. 2015, 29, 1044–1050. [Google Scholar] [CrossRef]
- Nelson, N.G.; McKenzie, L.B. Rock climbing injuries treated in emergency departments in the US, 1990–2007. Am. J. Prev. Med. 2009, 37, 195–200. [Google Scholar] [CrossRef]
- Addiss, D.G.; Baker, S.P. Mountaineering and rock-climbing injuries in US national parks. Ann. Emerg. Med. 1989, 18, 975–979. [Google Scholar] [CrossRef]
- Rauch, S.; Wallner, B.; Ströhle, M.; Dal Cappello, T.; Brodmann Maeder, M. Climbing Accidents—Prospective Data Analysis from the International Alpine Trauma Registry and Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2020, 17, 203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wyatt, J.P.; McNaughton, G.W.; Grant, P.T. A prospective study of rock climbing injuries. Br. J. Sports Med. 1996, 30, 148–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McLennan, J.G.; Ungersma, J. Mountaineering accidents in the Sierra Nevada. Am. J. Sports Med. 1983, 11, 160–163. [Google Scholar] [CrossRef]
- Bowie, W.S.; Hunt, T.K.; Allen, H.A., Jr. Rock-climbing injuries in Yosemite National Park. West. J. Med. 1988, 149, 172. [Google Scholar] [PubMed]
- Richardson, G.D.; Spano, S.J. Death on the Dome: Epidemiology of recreational deaths on Half Dome in Yosemite National Park. Wilderness Environ. Med. 2018, 29, 338–342. [Google Scholar] [CrossRef]
- Runer, A.; Lampl, K.; Neunhäuserer, D.; Runer, F.; Frick, N.; Seitlinger, G.; Resch, H.; Moroder, P. A 1-year prospective analysis of ice climbing injuries. Clin. J. Sport Med. 2017, 27, 161–167. [Google Scholar] [CrossRef]
- Wasserman, R.C.; Waller, J.A.; Monty, M.J.; Emery, A.B.; Robinson, D.R. Bicyclists, helmets and head injuries: A rider-based study of helmet use and effectiveness. Am. J. Public Health 1988, 78, 1220–1221. [Google Scholar] [CrossRef] [Green Version]
- Zentner, J.; Franken, H.; Löbbecke, G. Head injuries from bicycle accidents. Clin. Neurol. Neurosurg. 1996, 98, 281–285. [Google Scholar] [CrossRef]
- Thompson, R.S.; Rivara, F.P.; Thompson, D.C. A case-control study of the effectiveness of bicycle safety helmets. N. Engl. J. Med. 1989, 320, 1361–1367. [Google Scholar] [CrossRef] [PubMed]
- Kotlyar, S. Cycling injuries in Southwest Colorado: A comparison of road vs trail riding injury patterns. Wilderness Environ. Med. 2016, 27, 316–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hurst, H.T.; Atkins, S.; Dickinson, B.D. The magnitude of translational and rotational head accelerations experienced by riders during downhill mountain biking. J. Sci. Med. Sport 2018, 21, 1256–1261. [Google Scholar] [CrossRef] [PubMed]
- Chow, T.K.; Corbett, S.W.; Farstad, D.J. Do conventional bicycle helmets provide adequate protection in mountain biking? Wilderness Environ. Med. 1995, 6, 385–390. [Google Scholar] [CrossRef]
- Bürgi, N.; Clijsen, R.; Taeymans, J.; Cabri, J. Akute Mountainbike-Verletzungen–ein Review. Sportverletz. Sportschaden 2010, 24, 77–81. [Google Scholar] [CrossRef] [Green Version]
- Chow, T.K.; Bracker, M.; Patrick, K. Acute injuries from mountain biking. West. J. Med. 1993, 159, 145. [Google Scholar]
- Pfeiffer, R. Off-road bicycle racing injuries--the NORBA Pro/Elite category. Care and prevention. Clin. Sports Med. 1994, 13, 207–218. [Google Scholar] [CrossRef]
- Gaulrapp, H.; Weber, A.; Rosemeyer, B. Injuries in mountain biking. Knee Surg. Sports Traumatol. Arthrosc. 2001, 9, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Carmont, M.R. Mountain biking injuries: A review. Br. Med. Bull. 2008, 85, 101–112. [Google Scholar] [CrossRef] [Green Version]
- Illingworth, C.M. BMX compared with ordinary bicycle accidents. Arch. Dis. Child. 1985, 60, 461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gassner, R.J.; Hackl, W.; Tuli, T.; Fink, C.; Waldhart, E. Differential profile of facial injuries among mountainbikers compared with bicyclists. J. Trauma Acute Care Surg. 1999, 47, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Gassner, R.; Tuli, T.; Emshoff, R.; Waldhart, E. Mountainbiking–a dangerous sport: Comparison with bicycling on oral and maxillofacial trauma. Int. J. Oral Maxillofac. Surg. 1999, 28, 188–191. [Google Scholar] [CrossRef]
- Chapman, S.; Webber, C.; O’Meara, M. Scooter injuries in children. J. Paediatr. Child Health 2001, 37, 567–570. [Google Scholar] [CrossRef]
- Isichei, M.W.; Ale, A.F.; Misauno, M.A.; Brown, P.; Soulakis, N.D. Unpowered Scooter-Related Injuries among Adolescents and Adults in the United States 2007–2017. Open J. Emerg. Med. 2020, 8, 13–20. [Google Scholar] [CrossRef] [Green Version]
- Levine, D.A.; Platt, S.L.; Foltin, G.L. Scooter injuries in children. Pediatrics 2001, 107, e64. [Google Scholar] [CrossRef] [Green Version]
- Alwani, M.; Jones, A.; Morgan, S.; Lancaster, B.; Sim, M.; Ting, J. Facing Facts: Facial Injuries from Stand-up Electric Scooters. Cureus 2020, 12, e6663. [Google Scholar] [CrossRef] [Green Version]
- Beck, S.; Barker, L.; Chan, A.; Stanbridge, S. Emergency department impact following the introduction of an electric scooter sharing service. Emerg. Med. Australas. 2020, 32, 409–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, C.; Coimbra, R.; Hoyt, D.B.; Chan, T.C. Severe traumatic brain injury from unmotorized scooter. J. Emerg. Med. 2001, 21, 133–136. [Google Scholar] [CrossRef]
- Kubiak, R.; Slongo, T. Unpowered scooter injuries in children. Acta Paediatr. 2003, 92, 50–54. [Google Scholar] [CrossRef]
- Rethnam, U.; Yesupalan, R.S.; Sinha, A. Skateboards: Are they really perilous? A retrospective study from a district hospital. BMC Res. Notes 2008, 1, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schieber, R.A.; Branche-Dorsey, C.M.; Ryan, G.W. Comparison of In-line Skating Injuries With Rollerskating and Skateboarding Injuries. JAMA 1994, 271, 1856–1858. [Google Scholar] [CrossRef] [PubMed]
- Bandzar, S.; Funsch, D.G.; Hermansen, R.; Gupta, S.; Bandzar, A. Pediatric Hoverboard and Skateboard Injuries. Pediatrics 2018, 141, e20171253. [Google Scholar] [CrossRef]
- Veith, L.; Neunteufel, E.; Brunnader, L.; Krifter, R.M. Skateboard—New Olympic Sports in Sports Orthopaedics. Sports Orthop. Traumatol. 2020, 36, 12–19. [Google Scholar] [CrossRef]
- Russell, K.W.; Katz, M.G.; Short, S.S.; Scaife, E.R.; Fenton, S.J. Longboard injuries treated at a level 1 pediatric trauma center. J. Pediatric Surg. 2018, 54, 569–571. [Google Scholar] [CrossRef]
- Sherker, S.; Cassell, E. Preventing In-Line Skating Injuries. Sports Med. 1999, 28, 325–335. [Google Scholar] [CrossRef]
- Mitts, K.G.; Hennrikus, W.L. In-Line Skating Fractures in Children. J. Pediatric Orthop. 1996, 16, 640–643. [Google Scholar] [CrossRef]
- Knox, C.L.; Comstock, R.D.; McGeehan, J.; Smith, G.A. Differences in the Risk Associated With Head Injury for Pediatric Ice Skaters, Roller Skaters, and In-Line Skaters. Pediatrics 2006, 118, 549. [Google Scholar] [CrossRef] [PubMed]
- Ostermann, R.C.; Hofbauer, M.; Tiefenböck, T.M.; Pumberger, M.; Tiefenböck, M.; Platzer, P.; Aldrian, S. Injury severity in ice skating: An epidemiologic analysis using a standardised injury classification system. Int. Orthop. 2015, 39, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Knox, C.L.; Comstock, R.D. Video analysis of falls experienced by paediatric iceskaters and roller/inline skaters. Br. J. Sports Med. 2006, 40, 268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGeehan, J.; Shields, B.J.; Smith, G.A. Children Should Wear Helmets While Ice-Skating: A Comparison of Skating-Related Injuries. Pediatrics 2004, 114, 124. [Google Scholar] [CrossRef]
- Ivins, B.J.; Schwab, K.A.; Warden, D.; Harvey, L.T.C.S.; Hoilien, M.A.J.M.; Powell, C.O.L.J.; Johnson, C.S.M.E.W.; Salazar, A.M. Traumatic Brain Injury in U.S. Army Paratroopers: Prevalence and Character. J. Trauma Acute Care Surg. 2003, 55, 617–621. [Google Scholar] [CrossRef]
- Binns, J.H.; Potter, J.M. Head injuries in military parachutists. Injury 1972, 3, 133–134. [Google Scholar] [CrossRef]
- Monasterio, E.; Mulder, R.; Frampton, C.; Mei-Dan, O. Personality Characteristics of BASE Jumpers. J. Appl. Sport Psychol. 2012, 24, 391–400. [Google Scholar] [CrossRef]
- Federiuk, C.S.; Schlueter, J.L.; Adams, A.L. Skiing, snowboarding, and sledding injuries in a northwestern state. Wilderness Environ. Med. 2002, 13, 245–249. [Google Scholar] [CrossRef] [Green Version]
- Niedermeier, M.; Gatterer, H.; Pocecco, E.; Frühauf, A.; Faulhaber, M.; Menz, V.; Burtscher, J.; Posch, M.; Ruedl, G.; Burtscher, M. Mortality in Different Mountain Sports Activities Primarily Practiced in the Winter Season—A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 259. [Google Scholar] [CrossRef] [Green Version]
- Bailly, N.; Afquir, S.; Laporte, J.-D.; Melot, A.; Savary, D.; Seigneuret, E.; Delay, J.-B.; Donnadieu, T.; Masson, C.; Arnoux, P.-J. Analysis of Injury Mechanisms in Head Injuries in Skiers and Snowboarders. Med. Sci. Sports Exerc. 2017, 49, 1–20. [Google Scholar] [CrossRef]
- Ruedl, G.; Bilek, H.; Ebner, H.; Gabl, K.; Kopp, M.; Burtscher, M. Fatalities on Austrian Ski Slopes During a 5-year period. Wilderness Environ. Med. 2011, 22, 326–328. [Google Scholar] [CrossRef] [Green Version]
- Chaze, B.; McDonald, P. Head Injuries in Winter Sports: Downhill Skiing, Snowboarding, Sledding, Snowmobiling, Ice Skating and Ice Hockey. Phys. Med. Rehabil. Clin. North Am. 2009, 20, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Rust, D.A.; Gilmore, C.J.; Treme, G. Injury patterns at a large Western United States ski resort with and without snowboarders: The Taos experience. Am. J. Sports Med. 2013, 41, 652–656. [Google Scholar] [CrossRef] [PubMed]
- Costa-Scorse, B.A.; Hopkins, W.G.; Cronin, J.; Bressel, E. New Zealand Snow Sports Injury Trends Over Five Winter Seasons 2010–2014. In Snow Sports Trauma and Safety; Springer: Cham, Switzerland, 2017; pp. 17–28. [Google Scholar]
- Wasden, C.C.; McIntosh, S.E.; Keith, D.S.; McCowan, C. An Analysis of Skiing and Snowboarding Injuries on Utah Slopes. J. Trauma Acute Care Surg. 2009, 67, 1022–1026. [Google Scholar] [CrossRef]
- Brooks, M.A.; Evans, M.D.; Rivara, F.P. Evaluation of skiing and snowboarding injuries sustained in terrain parks versus traditional slopes. Inj. Prev. 2010, 16, 119. [Google Scholar] [CrossRef]
- Costa-Scorse, B.A.; Hopkins, W.G.; Cronin, J.; Bressel, E. The Utility of Two National Injury Databases to Evaluate Snow-Sports Injuries in New Zealand. In Snow Sports Trauma and Safety; Springer: Cham, Switzerland, 2017; pp. 41–49. [Google Scholar]
- Xiang, H.; Kelleher, K.; Shields, B.J.; Brown, K.J.; Smith, G.A. Skiing- and Snowboarding-Related Injuries Treated in U.S. Emergency Departments, 2002. J. Trauma Acute Care Surg. 2005, 58, 112–118. [Google Scholar] [CrossRef]
- Siu, T.L.T.; Chandran, K.N.; Newcombe, R.L.; Fuller, J.W.; Pik, J.H.T. Snow sports related head and spinal injuries: An eight-year survey from the neurotrauma centre for the Snowy Mountains, Australia. J. Clin. Neurosci. 2004, 11, 236–242. [Google Scholar] [CrossRef]
- Fukuda, O.; Takaba, M.; Saito, T.; Endo, S. Head Injuries in Snowboarders Compared with Head Injuries in Skiers: A Prospective Analysis of 1076 patients from 1994 to 1999 in Niigata, Japan. Am. J. Sports Med. 2001, 29, 437–440. [Google Scholar] [CrossRef] [PubMed]
- Nakaguchi, H.; Fujimaki, T.; Ueki, K.; Takahashi, M.; Yoshida, H.; Kirino, T. Snowboard Head Injury: Prospective Study in Chino, Nagano, for Two Seasons from 1995 to 1997. J. Trauma Acute Care Surg. 1999, 46, 1066–1069. [Google Scholar] [CrossRef] [PubMed]
- Renstrom, P.; Johnson, R.J. Cross-Country Skiing Injuries and Biomechanics. Sports Med. 1989, 8, 346–370. [Google Scholar] [CrossRef]
- Gannon, D.M.; Derse, A.R.; Bronkema, P.J.; Primley, D.M. The emergency care network of a ski marathon. Am. J. Sports Med. 1985, 13, 316–320. [Google Scholar] [CrossRef]
- Sadeghian, H.; Nguyen, B.; Huynh, N.; Rouch, J.; Lee, S.L.; Bazargan-Hejazi, S. Factors Influencing Helmet Use, Head Injury, and Hospitalization Among Children Involved in Skateboarding and Snowboarding Accidents. Perm. J. 2017, 21, 16–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Made, C.; Elmqvist, L.G. A 10-year study of snowboard injuries in Lapland Sweden. Scand. J. Med. Sci. Sports 2004, 14, 128–133. [Google Scholar] [CrossRef]
- Fukuda, O.; Hirashima, Y.; Origasa, H.; Endo, S. Characteristics of Helmet or Knit Cap Use in Head Injury of Snowboarders—Analysis of 1190 Consecutive Patients. Neurol. Med. -Chir. 2007, 47, 491–494. [Google Scholar] [CrossRef] [Green Version]
- Voaklander, D.C.; Kelly, K.D.; Sukrani, N.; Sher, A.; Rowe, B.H. Sledding Injuries in Patients Presenting to the Emergency Department in a Northern City. Acad. Emerg. Med. 2001, 8, 629–635. [Google Scholar] [CrossRef] [Green Version]
- Skarbek-Borowska, S.; Amanullah, S.; Mello, M.J.; Linakis, J.G. Emergency Department Visits for Sledding Injuries in Children in the United States in 2001/2002. Acad. Emerg. Med. 2006, 13, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Ting, D.K.; Brison, R.J. Injuries in recreational curling include head injuries and may be prevented by using proper footwear. Health Promot. Chronic Dis. Prev. Can. Res. Policy Pract. 2015, 35, 29–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carmont, M.R. Sailing and Yachting. In Adventure and Extreme Sports Injuries: Epidemiology, Treatment, Rehabilitation and Prevention; Mei-Dan, O., Carmont, M.R., Eds.; Springer: London, UK, 2013; pp. 203–223. [Google Scholar] [CrossRef]
- Dimmick, S.; Gillett, M.; Buchan, C.; Sheehan, P.; Franks, M.; Ratchford, A.; Porges, K.; Day, R.; Milne, T.; Anderson, S. Prospective analysis of surfing and bodyboard injuries. Trauma 2018, 21, 113–120. [Google Scholar] [CrossRef]
- Ulkestad, G.-E.; Drogset, J.O. Surfing Injuries in Norwegian Arctic Waters. Open Sports Sci. J. 2016, 9, 153–161. [Google Scholar] [CrossRef]
- Woodacre, T.; Waydia, S.E.; Wienand-Barnett, S. Aetiology of injuries and the need for protective equipment for surfers in the UK. Injury 2015, 46, 162–165. [Google Scholar] [CrossRef] [PubMed]
- Hay, C.S.M.; Barton, S.; Sulkin, T. Recreational Surfing Injuries in Cornwall, United Kingdom. Wilderness Environ. Med. 2009, 20, 335–338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dimmick, S.; Gillett, M.; Sheehan, P.; Sutton, C.; Anderson, S.E. Acute injuries and chronic pathology of the head and face sustained while surf board riding. Trauma 2014, 16, 195–201. [Google Scholar] [CrossRef]
- Dimmick, S.; Sheehan, P.; Brazier, D.; Anderson, S.E. Injuries sustained while surfboard riding. Skelet. Radiol. 2013, 42, 463–465. [Google Scholar] [CrossRef] [Green Version]
- Dimmick, S.; Brazier, D.; Wilson, P.; Anderson, S.E. Injuries of the Head and Spine sustained while Surf Board Riding. In Proceedings of the European Congress of Radiology-RANZCR-AOCR, Sydney, Australia, 30 August–2 September 2012. [Google Scholar]
- Nathanson, A.T.; Haynes, P.; Galanis, D. Surfing injuries. Am. J. Emerg. Med. 2002, 20, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.M.; Bennett, D.; Carter, M.; Garewal, D.; Finch, C.F. Acute injury and chronic disability resulting from surfboard riding. J. Sci. Med. Sport 2004, 7, 429–437. [Google Scholar] [CrossRef]
- Jubbal, K.T.; Chen, C.; Costantini, T.; Herrera, F.; Dobke, M.; Suliman, A. Analysis of surfing injuries presenting in the acute trauma setting. Ann. Plast. Surg. 2017, 78, S233–S237. [Google Scholar] [CrossRef]
- Swinney, C. Assessing the Prevalence of Traumatic Head Injury amongst Recreational Surfers in the United States. Hawai’i J. Med. Public Health A J. Asia Pac. Med. Public Health 2015, 74, 403–405. [Google Scholar]
- Goodship, J.; Roberts, H.; Caldow, D.; Aldred, M. ‘Board’ out of my skull: Penetrating skull fracture from a surfboard nose. BMJ Case Rep. 2018, 11, 227678. [Google Scholar] [CrossRef]
- Morvan, J.-B.; Rivière, D.; Vatin, L.; Joubert, C.; Bousquet, F.; Cathelinaud, O. Kitesurfing and Cranial Trauma with Frontal Sinus Fracture. Curr. Sports Med. Rep. 2018, 17, 23–25. [Google Scholar] [CrossRef]
- Durnford, A.J.; Harrisson, S.E.; Eynon, C.A. Kitesports: A new source of major trauma? Report of four cases and literature review. Trauma 2013, 16, 23–26. [Google Scholar] [CrossRef]
- Fiore, D.C. Injuries associated with whitewater rafting and kayaking. Wilderness Environ. Med. 2003, 14, 255–260. [Google Scholar] [CrossRef]
- Attarian, A.; Siderelis, C. Injuries in Commercial Whitewater Rafting on the New and Gauley Rivers of West Virginia. Wilderness Environ. Med. 2013, 24, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Whisman, S.A.; Hollenhorst, S.J. Injuries in commercial whitewater rafting. Clin. J. Sport Med. 1999, 9, 18–23. [Google Scholar] [CrossRef]
- O’Hare, D.; Chalmers, D.; Arnold, N.A.; Williams, F. Mortality and morbidity in white water rafting in New Zealand. Inj. Control Saf. Promot. 2002, 9, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Burns, R.; Smaldone, D. Injuries in West Virginia Commercial Whitewater Rafting (2011–2016); Prepared for the West Virginia Division of Natural Resources on behalf of the West Virginia Whitewater Commission; Recreation, Parks, & Tourism Resources Program, School of Natural Resources, West Virginia University: Morgantown, WV, USA, 2018. [Google Scholar]
- Folland, J.P.; Strachan, K. Whitewater Canoeing and Rafting. In Adventure and Extreme Sports Injuries: Epidemiology, Treatment, Rehabilitation and Prevention, Mei-Dan, O., Carmont, M.R., Eds.; Springer: London, UK, 2013; pp. 113–141. [Google Scholar] [CrossRef]
- Worley, G.H. Promoting the use of equestrian helmets: Another opportunity for injury prevention. J. Emerg. Nurs. 2010, 36, 263–264. [Google Scholar] [CrossRef] [PubMed]
- Barber, H.M. Horse-play: Survey of accidents with horses. Br. Med. J. 1973, 3, 532–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chitnavis, J.; Gibbons, C.; Hirigoyen, M.; Parry, J.L.; Simpson, A. Accidents with horses: What has changed in 20 years? Injury 1996, 27, 103–105. [Google Scholar] [CrossRef]
- Buckley, S.M.; Chalmers, D.J.; Langley, J.D. Injuries due to falls from horses. Aust. J. Public Health 1993, 17, 269–271. [Google Scholar] [CrossRef]
- Shahan, C.P.; Emmett, K.; Zarzaur, B.L. Large animal-related injury requiring hospital admission: Injury pattern disparities. Injury 2012, 43, 1898–1902. [Google Scholar] [CrossRef] [PubMed]
- Meredith, L.; Ekman, R.; Thomson, R. Horse-related incidents and factors for predicting injuries to the head. BMJ Open Sport Exerc. Med. 2018, 4, e000398. [Google Scholar] [CrossRef] [Green Version]
- Lim, J.; Puttaswamy, V.; Gizzi, M.; Christie, L.; Croker, W.; Crowe, P. Pattern of equestrian injuries presenting to a Sydney teaching hospital. ANZ J. Surg. 2003, 73, 567–571. [Google Scholar] [CrossRef] [PubMed]
- Bourdet, N.; Willinger, R. Head impact conditions in case of equestrian accident. In Proceedings of the IRCOBI Conference, Lyon, France, 9–11 September 2015; pp. 156–167. [Google Scholar]
- Palomar, M.; Belda, R.; Giner, E. Effect of different helmet shell configurations on the protection against head trauma. J. Strain Anal. Eng. Des. 2019, 54, 408–415. [Google Scholar] [CrossRef]
- Sepulveda-Lopez, D.; Antona-Makoshi, J.; Rubio, I.; Rodríguez-Millán, M. Numerical Analysis of Bicycle Helmet under Blunt Behavior. Appl. Sci. 2020, 10, 3692. [Google Scholar] [CrossRef]
- Cummings, P.; Rivara, F.P.; Thompson, D.C.; Thompson, R.S. Misconceptions regarding case-control studies of bicycle helmets and head injury. Accid. Anal. Prev. 2006, 38, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Haider, A.H.; Saleem, T.; Bilaniuk, J.W.; Barraco, R.D.; Eastern Association for the Surgery of Trauma Injury ControlViolence Prevention, C. An evidence-based review: Efficacy of safety helmets in the reduction of head injuries in recreational skiers and snowboarders. J. Trauma Acute Care Surg. 2012, 73, 1340–1347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spennemann, D.H.R. The protective effects of turbans against cranial trauma: A call for systematic epidemiological studies in the Punjab. J. Punjab Acad. Forensic Med. Toxicol. 2020, 20, 190–191. [Google Scholar] [CrossRef]
| Fall Direction | Differentially Preferred Broad Locus of Head Injury | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sport | For-Ward | Side-Ways | Back-Ward | Down-Ward | Facial | Frontal | Parietal | Temporal | Occipital |
| Climbing | ✓ | ✓ | X * | ||||||
| Wheeled sports | |||||||||
| Mountain/Trail Biking | ✓ | dom | dom | occ | occ | ||||
| Scooters | ✓ | ✓ | dom | dom | occ | occ | occ | ||
| Skateboarding | ✓ | ✓ | dom | dom | occ | dom | |||
| Skating | ✓ | ✓ | freq | freq | freq | ||||
| Aerial sports | |||||||||
| Hang-Gliding & Paragliding | ✓ | ✓ | ✓ | ✓ | |||||
| Skydiving | ✓ | dom | |||||||
| BASE jumping | ✓ | ✓ | ✓ | ✓ | |||||
| Winter sports | |||||||||
| Downhill skiing | ✓ | ✓ | ✓ | freq | dom | dom | |||
| Cross-country skiing | ✓ | freq | freq | ||||||
| Snowboarding | ✓ | ✓ | freq | freq | freq | ||||
| Sledding | ✓ | ✓ | freq | freq | freq | ||||
| Curling | freq | freq | |||||||
| Water sports | |||||||||
| Surfing | ✓ | dom | dom | ||||||
| Wind and Kitesurfing | ✓ | dom | dom | ||||||
| White-water kayaking and rafting | ✓ | dom | freq | ||||||
| Animal-based sports | |||||||||
| Equestrian | ✓ | ✓ | dom | dom | freq | occ | |||
| Studies Excluding Facial | Studies in Including Facial | |||||
|---|---|---|---|---|---|---|
| Activity | Turbaned | Unprotected | Turbaned | Unprotected | Facial | Reference |
| Skateboarding | 92.2% | 7.8% | [18] | |||
| Skiing | 91.7% | 8.3% | [73] | |||
| Skiing | 96.2% | 3.8% | [74] | |||
| Skiing | 95.6% | 4.8% | [75] | |||
| Skiing | (86.9%) | (13.1%) | 63.7% | 9.6% | 26.7% | [64] |
| Snowboarding | 92.5% | 7.5% | [75] | |||
| Snowboarding | 98.8% | 1.2% | [74] | |||
| Snowboarding | (89.3%) | (10.7%) | 63.1% | 7.6% | 29.1% | [64] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spennemann, D.H.R. Turbans vs. Helmets: A Systematic Narrative Review of the Literature on Head Injuries and Impact Loci of Cranial Trauma in Several Recreational Outdoor Sports. Sports 2021, 9, 172. https://doi.org/10.3390/sports9120172
Spennemann DHR. Turbans vs. Helmets: A Systematic Narrative Review of the Literature on Head Injuries and Impact Loci of Cranial Trauma in Several Recreational Outdoor Sports. Sports. 2021; 9(12):172. https://doi.org/10.3390/sports9120172
Chicago/Turabian StyleSpennemann, Dirk H. R. 2021. "Turbans vs. Helmets: A Systematic Narrative Review of the Literature on Head Injuries and Impact Loci of Cranial Trauma in Several Recreational Outdoor Sports" Sports 9, no. 12: 172. https://doi.org/10.3390/sports9120172






