Presenting Health Status in Children Using a Radar Plot
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
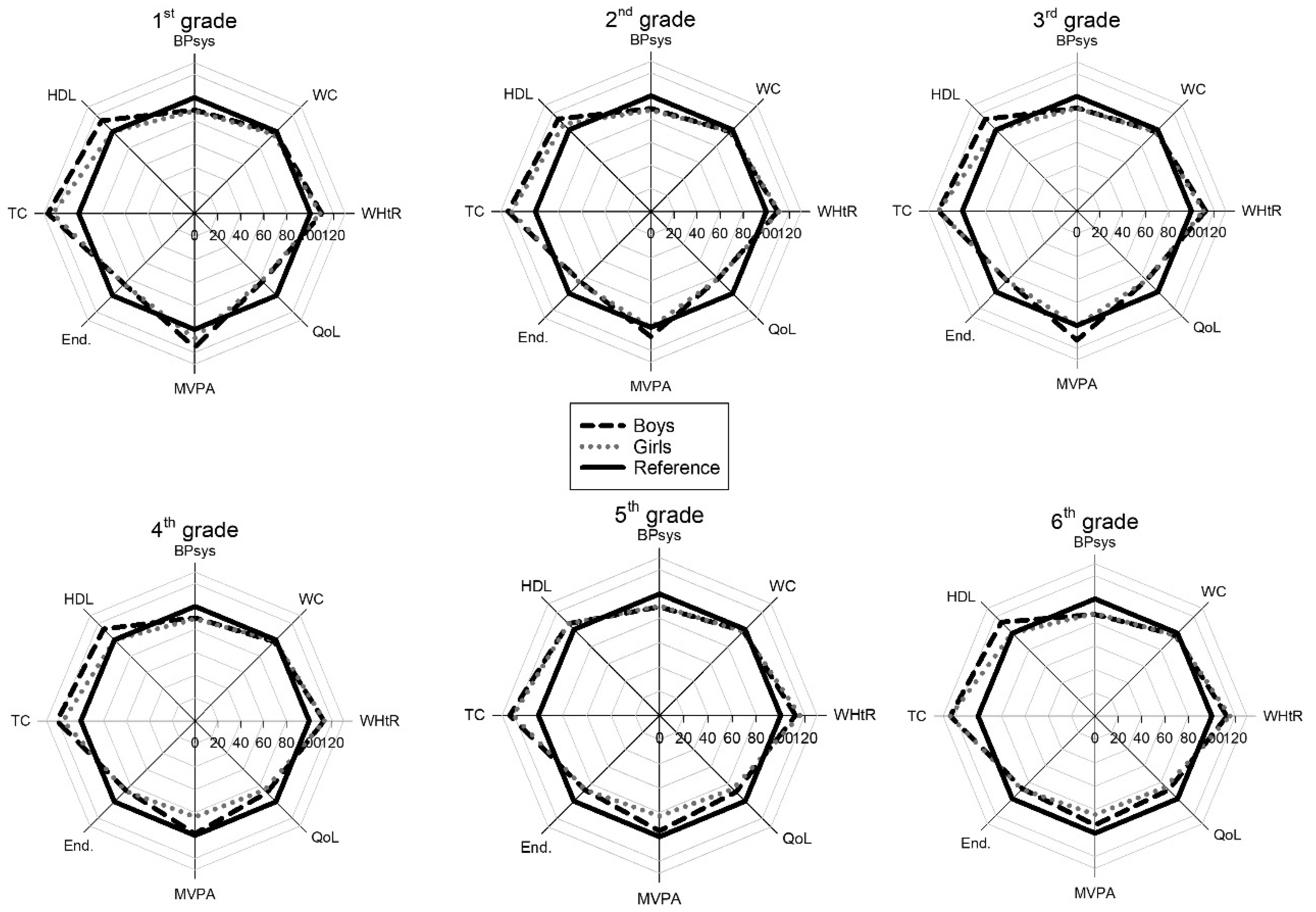
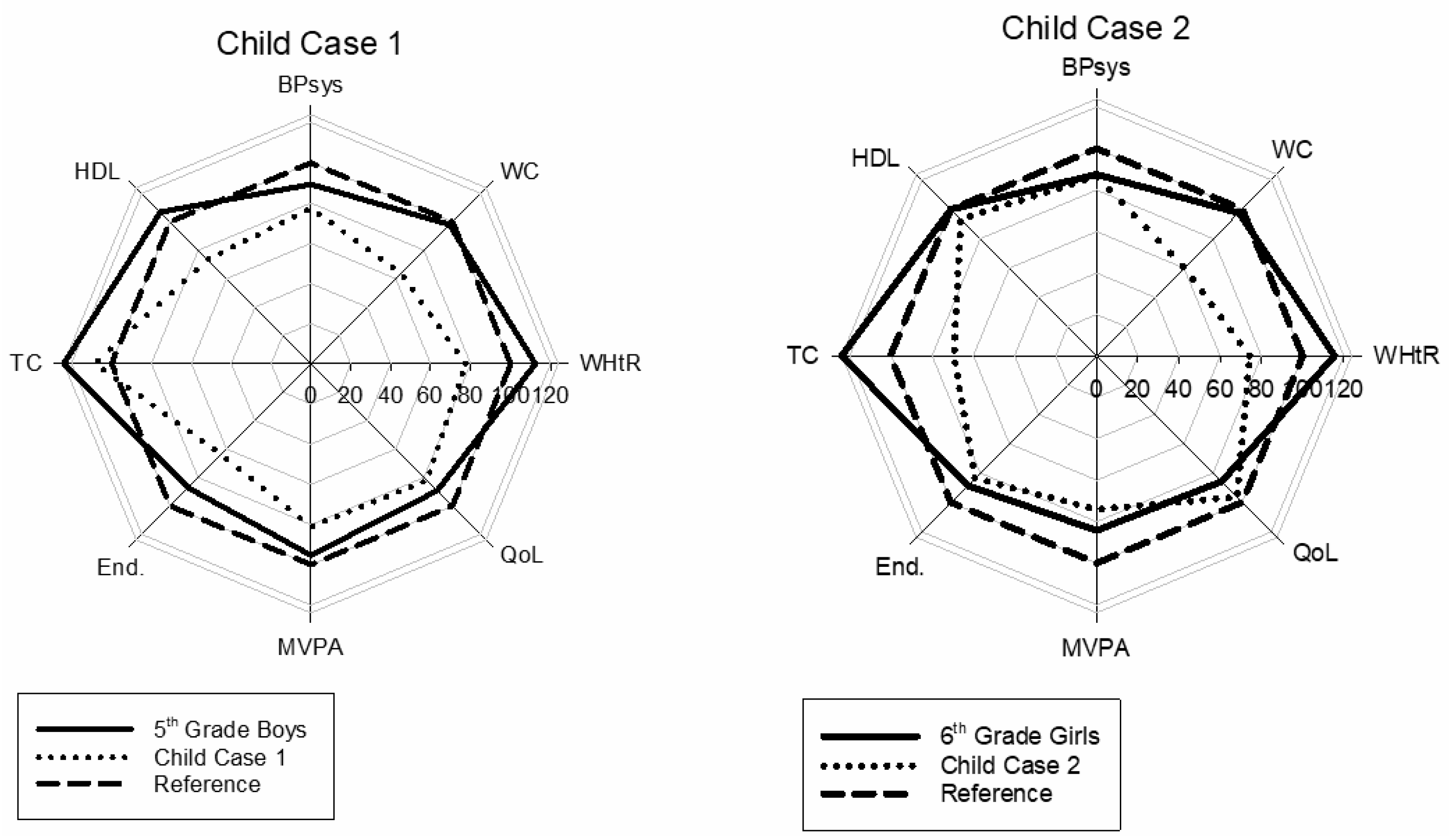
2.2. The Radar Plot
2.3. Measurements
2.3.1. Blood Pressure
2.3.2. Waist Circumference
2.3.3. Waist to Height Ratio (WHtR)
2.3.4. Quality of Life (QoL)
2.3.5. Blood Samples
2.3.6. Serum Cholesterol
2.3.7. High Density Lipoprotein (HDL)
2.3.8. Physical Activity (PA)
2.3.9. Endurance Test
2.4. Statistics
3. Results
Basic Results
4. Discussion
4.1. Main Findings
4.2. Choice of Variables
4.3. Anthropometric Variables
4.4. Medical Variables
4.4.1. HDL
4.4.2. Total Cholesterol
4.5. Activity Level
MVPA
4.6. Endurance Performance
4.7. Quality of Life
4.8. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Berenson, G.S.; Wattigney, W.A.; Tracy, R.E.; Newman, W.P.; Srinivasan, S.R.; Webber, L.S.; Dalferes, E.R.; Strong, J.P. Atherosclerosis of the aorta and coronary arteries and cardiovascular risk factors in persons aged 6 to 30 years and studied at necropsy (the Bogalusa Heart Study). Am. J. Cardiol. 1992, 70, 851–858. [Google Scholar] [CrossRef]
- Kopf, E.W. Florence Nightingale as Statistician. Publ. Am. Stat. Assoc. 1916, 15, 388–404. [Google Scholar] [CrossRef]
- Friendly, M.; Denis, D.J. Milestones in the History of Thematic Cartography, Statistica l Graphics, and Data Visualization. Available online: https://www.researchgate.net/publication/240118128_Milestones_in_the_history_of_thematic_cartography_statistica_l_graphics_and_data_visualization (accessed on 11 April 2020).
- Noirhomme-Fraiture, M. Visualization of Large Data Sets: The Zoom Star Solution. Available online: https://www.semanticscholar.org/paper/Visualization-of-Large-Data-Sets%3A-The-Zoom-Star-Noirhomme-Fraiture/2d9240bde13b1707b20b02759eb0726e4b409fcd (accessed on 14 April 2020).
- Radar Chart—Minnesota Department of Health. Available online: https://www.health.state.mn.us/communities/practice/resources/phqitoolbox/radarchart.html#sources (accessed on 14 April 2020).
- Ordóñez, P.; desJardins, M.; Lombardi, M.; Lehmann, C.U.; Fackler, J.C. An animated multivariate visualization for physiological and clinical data in the ICU. In Proceedings of the IHI; ACM: Arlington, VA, USA, 2010. [Google Scholar]
- Aasland, O.G. Alkohol og EU—fri flyt? Alcohol and EU—free flow? Tidsskr. Den. Nor. Legeforening 2003, 123, 188–189. [Google Scholar]
- Fredriksen, P.M.; Hjelle, O.P.; Mamen, A.; Meza, T.J.; Westerberg, A.C. The health Oriented pedagogical project (HOPP)—A controlled longitudinal school-based physical activity intervention program. BMC Public Health 2017, 17, 370. [Google Scholar] [CrossRef] [Green Version]
- Norsk Barnelegeforening Pediatriveiledere fra Norsk barnelegeforening Pediatric Guidence from Norwegian Pediatrician Association in Norwegian. Available online: /pediatriveiledere?key=181604&menuitemkeylev1=6747&menuitemkeylev2=6507 (accessed on 18 March 2020).
- WHO. WHO | Waist Circumference and Waist–Hip Ratio; World Health Organization: Geneva, Switzerland, 2008; p. 47. [Google Scholar]
- Janssen, I.; Katzmarzyk, P.T.; Ross, R. Waist circumference and not body mass index explains obesity-related health risk. Am. J. Clin. Nutr. 2004, 79, 379–384. [Google Scholar] [CrossRef] [Green Version]
- Bays, H.E.; Toth, P.P.; Kris-Etherton, P.M.; Abate, N.; Aronne, L.J.; Brown, W.V.; Gonzalez-Campoy, J.M.; Jones, S.R.; Kumar, R.; La Forge, R.; et al. Obesity, adiposity, and dyslipidemia: A consensus statement from the National Lipid Association. J. Clin. Lipidol. 2013, 7, 304–383. [Google Scholar] [CrossRef] [Green Version]
- International Diabetes Federation. The IDF Consensus Definition of the Metabolic Syndrome in Children and Asolescents; International Diabetes Federation: Brussels, Belgium, 2007; p. 24. [Google Scholar]
- Seo, J.-Y.; Kim, J.H. Validation of surrogate markers for metabolic syndrome and cardiometabolic risk factor clustering in children and adolescents: A nationwide population-based study. PLoS ONE 2017, 12. [Google Scholar] [CrossRef]
- Ashwell, M.; Hsieh, S.D. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int. J. Food Sci. Nutr. 2005, 56, 303–307. [Google Scholar] [CrossRef]
- Browning, L.M.; Hsieh, S.D.; Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr. Res. Rev. 2010, 23, 247–269. [Google Scholar] [CrossRef] [Green Version]
- Swainson, M.G.; Batterham, A.M.; Tsakirides, C.; Rutherford, Z.H.; Hind, K. Prediction of whole-body fat percentage and visceral adipose tissue mass from five anthropometric variables. PLoS ONE 2017, 12, e0177175. [Google Scholar] [CrossRef]
- Högrefe Psykologiförlaget Inventory of Life Quality in Children and Adolescents. Available online: https://www.hogrefe.no/Klinisk-psykologi/Personlighetstester/ILC/ (accessed on 5 August 2019).
- Kristiansen, H.; Hove, P. Måleegenskaper ved den norske versjonen av The Inventory of Life Quality in children and adolescents (ILC) [Measurement properties of the Norwegian version of …]. PsykTestBarn 2013, 1, 1–9. [Google Scholar] [CrossRef]
- American Academy of Pediatrics, Committee on Nutrition. Cholesterol in childhood. Pediatrics 2011, 128, S213–S256. [Google Scholar] [CrossRef] [Green Version]
- Deng, W.H.; Fredriksen, P.M. Objectively assessed moderate-to-vigorous physical activity levels among primary school children in Norway: The Health Oriented Pedagogical Project (HOPP). Scand. J. Public Health 2018, 46, 38–47. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics. Committee on Nutrition American Academy of Pediatrics. Committee on Nutrition. Cholesterol in childhood. Pediatrics 1998, 101, 141–147. [Google Scholar]
- Paffenbarger, R.S.; Hyde, R.T.; Wing, A.L.; Hsieh, C.C. Physical activity, all-cause mortality, and longevity of college alumni. N. Engl. J. Med. 1986, 314, 605–613. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.; Harro, M.; Sardinha, L.; Froberg, K.; Ekelund, U.; Brage, S.; Anderssen, S. Physical activity and clustered cardiovascular risk in children: A cross-sectional study (The European Youth Heart Study). Lancet Lond. Engl. 2006, 368, 299–304. [Google Scholar] [CrossRef]
- Andersen, L.B.; Andersen, T.E.; Andersen, E.; Anderssen, S.A. An intermittent running test to estimate maximal oxygen uptake: The Andersen test. J. Sports Med. Phys. Fit. 2008, 48, 434–437. [Google Scholar]
- Aadland, E.; Kvalheim, O.M.; Anderssen, S.A.; Resaland, G.K.; Andersen, L.B. The multivariate physical activity signature associated with metabolic health in children. Int. J. Behav. Nutr. Phys. Act. 2018. [Google Scholar] [CrossRef]
- Brambilla, P.; Lissau, I.; Flodmark, C.-E.; Moreno, L.A.; Widhalm, K.; Wabitsch, M.; Pietrobelli, A. Metabolic risk-factor clustering estimation in children: To draw a line across pediatric metabolic syndrome. Int. J. Obes. 2007, 31, 591–600. [Google Scholar] [CrossRef] [Green Version]
- Morrison, J.A.; Friedman, L.A.; Wang, P.; Glueck, C.J. Metabolic Syndrome in Childhood Predicts Adult Metabolic Syndrome and Type 2 Diabetes Mellitus 25 to 30 Years Later. J. Pediatr. 2008, 152, 201–206. [Google Scholar] [CrossRef]
- Skår, A.; Meza, T.J.; Fredriksen, P.M. Development of weight and height in Norwegian children: The Health Oriented Pedagogical Project (HOPP). Scand. J. Public Health 2018, 46, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.; Yang, M.; Yuan, Z.-P.; Zhang, D.-D.; Liang, L.; Wang, C.-L.; Zhang, S.; Zhu, H.-H.; Lai, M.-D.; Zhu, Y.-M. Waist-to-Height Ratio: A simple, effective and practical screening tool for childhood obesity and metabolic syndrome. Prev. Med. 2014, 67, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Lehto, R.; Ray, C.; Lahti-Koski, M.; Roos, E. Health behaviors, waist circumference and waist-to-height ratio in children. Eur. J. Clin. Nutr. 2011, 65, 841–848. [Google Scholar] [CrossRef]
- Sardinha, L.B.; Santos, D.A.; Silva, A.M.; Grøntvedt, A.; Andersen, L.B.; Ekelund, U. A comparison between BMI, waist circumference, and waist-to-height ratio for identifying cardio-metabolic risk in children and adolescents. PLoS ONE 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keefer, D.J.; Caputo, J.L.; Tseh, W. Waist-to-Height Ratio and Body Mass Index as Indicators of Cardiovascular Risk in Youth. J. Sch. Health 2013, 83, 805–809. [Google Scholar] [CrossRef] [PubMed]
- St. Olavs Hospital, B.- og ungdomspsykiatrisk klinikk Hva_er_normalt_blodtrykk_hos_barn? What’s Normal Blood Pressure for Children? Available online: http://onlinelibrary.wiley.com.ezproxy.hio.no/doi/10.1111/j.1600-0838.2009.01028.x/abstract (accessed on 9 January 2020).
- Twisk, J.W.; Kemper, H.C.; Van, W.M. Tracking of activity and fitness and the relationship with cardiovascular disease risk factors. Med. Sci. Sports Exerc. 2000, 32, 1455–1461. [Google Scholar] [CrossRef]
- Cote, A.T.; Harris, K.C.; Panagiotopoulos, C.; Sandor, G.G.S.; Devlin, A.M. Childhood Obesity and Cardiovascular Dysfunction. J. Am. Coll. Cardiol. 2013, 62, 1309–1319. [Google Scholar] [CrossRef] [Green Version]
- Strand, M.F.; Fredriksen, P.M.; Hjelle, O.P.; Lindberg, M. Reference intervals for serum lipids and prevalence of dyslipidaemia in 6–12-year-old children: The Health Oriented Pedagogical Project (HOPP). Scand. J. Public Health 2018, 46, 21–27. [Google Scholar] [CrossRef]
- Skinner, A.C.; Steiner, M.J.; Chung, A.E.; Perrin, E.M. Cholesterol Curves to Identify Population Norms by Age and Sex in Healthy Weight Children. Clin. Pediatr. 2012, 51, 233–237. [Google Scholar] [CrossRef] [Green Version]
- Telama, R.; Yang, X.; Leskinen, E.; Kankaanpää, A.; Hirvensalo, M.; Tammelin, T.; Viikari, J.; Raitakari, O. Tracking of Physical Activity from Early Childhood through Youth into Adulthood. Med. Sci. Sports Exerc. 2014, 46, 955–962. [Google Scholar] [CrossRef]
- Arvidsson, D.; Fridolfsson, J.; Buck, C.; Ekblom, Ö.; Ekblom-Bak, E.; Lissner, L.; Hunsberger, M.; Börjesson, M. Reexamination of Accelerometer Calibration with Energy Expenditure as Criterion: VO2net Instead of MET for Age-Equivalent Physical Activity Intensity. Sensors 2019, 19, 3377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | Unit | Reference Value | Presentation |
|---|---|---|---|
| Systolic Blood Pressure | mmHg | 90th percentile | Inverted † |
| Waist Circumference | cm | 90th percentile | Inverted |
| Waist to Height Ratio | - | 0.50 | Inverted |
| Quality of Life | % | 100 | Normal |
| Moderate to Vigorous Physical Activity | Average/min/day | 90 | Normal |
| Endurance Test | m | 90th percentile | Normal |
| Total Cholesterol | mmol/L | 5.2 | Inverted |
| High Density Lipoprotein Concentration | mmol/L | 1.5 | Normal |
| Girls | |||||||
|---|---|---|---|---|---|---|---|
| Grade | 1 | 2 | 3 | 4 | 5 | 6 | |
| Height (m) | mean | 1.24 | 1.29 | 1.34 | 1.40 | 1.47 | 1.53 |
| SD | 0.06 | 0.06 | 0.06 | 0.07 | 0.08 | 0.08 | |
| 10th percentile | 1.16 | 1.22 | 1.27 | 1.31 | 1.37 | 1.42 | |
| 90th percentile | 1.30 | 1.37 | 1.42 | 1.48 | 1.57 | 1.62 | |
| Body Mass (kg) | mean | 24.3 | 26.8 | 30.2 | 33.7 | 38.3 | 43.0 |
| SD | 4.8 | 5.3 | 6.0 | 8.0 | 8.7 | 9.8 | |
| 10th percentile | 19.2 | 21.5 | 23.1 | 25.8 | 29.3 | 32.3 | |
| 90th percentile | 30.0 | 33.5 | 37.1 | 44.0 | 50.2 | 56.2 | |
| WHtR | mean | 0.47 | 0.46 | 0.46 | 0.45 | 0.45 | 0.44 |
| SD | 0.04 | 0.04 | 0.04 | 0.05 | 0.05 | 0.06 | |
| 90th percentile | 0.42 | 0.42 | 0.41 | 0.39 | 0.40 | 0.39 | |
| 10th percentile | 0.53 | 0.52 | 0.51 | 0.50 | 0.51 | 0.52 | |
| WC (cm) | mean | 57.8 | 59.3 | 61.5 | 63.0 | 65.5 | 67.7 |
| SD | 6.2 | 5.9 | 6.6 | 8.6 | 8.1 | 9.0 | |
| 90th percentile | 51.1 | 54.0 | 54.0 | 54.0 | 57.6 | 59.0 | |
| 10th percentile | 66.0 | 67.1 | 70.0 | 72.7 | 75.5 | 79.0 | |
| SBP (mmHg) | mean | 104 | 106 | 107 | 108 | 111 | 112 |
| SD | 10 | 11 | 10 | 11 | 10 | 11 | |
| 90th percentile | 92 | 92 | 96 | 96 | 100 | 98.3 | |
| 10th percentile | 117 | 119 | 121 | 122 | 123 | 125.0 | |
| HDL (mmol/L) | mean | 1.54 | 1.63 | 1.56 | 1.56 | 1.59 | 1.57 |
| SD | 0.33 | 0.36 | 0.33 | 0.33 | 0.34 | 0.32 | |
| 10th percentile | 1.10 | 1.1 | 1.20 | 1.20 | 1.16 | 1.20 | |
| 90th percentile | 2.03 | 2.1 | 2.00 | 2.00 | 2.00 | 2.00 | |
| Tot Chol (mmol/L) | mean | 4.31 | 4.27 | 4.33 | 4.55 | 4.38 | 4.26 |
| SD | 0.64 | 0.66 | 0.71 | 0.69 | 0.69 | 0.64 | |
| 90th percentile | 3.60 | 3.50 | 3.50 | 3.60 | 3.50 | 3.50 | |
| 10th percentile | 5.10 | 5.20 | 5.19 | 5.53 | 5.30 | 5.20 | |
| Andersen Test (m) | mean | 779 | 855 | 934 | 934 | 975 | 1022 |
| SD | 121 | 104 | 127 | 116 | 101 | 112 | |
| 10th percentile | 610 | 715 | 790 | 797 | 843 | 890 | |
| 90th percentile | 949 | 982 | 1085 | 1078 | 1125 | 1155 | |
| MVPA (min) | mean | 98 | 91 | 91 | 79 | 79 | 78 |
| SD | 26 | 26 | 26 | 25 | 28 | 24 | |
| 10th percentile | 64 | 57 | 60 | 50.2 | 46 | 47 | |
| 90th percentile | 132 | 126 | 128 | 113 | 120 | 113 | |
| QoL (%) | mean | 80.8 | 81.7 | 83.3 | 84.2 | 85.4 | 85.3 |
| SD | 11.8 | 10.2 | 11.5 | 9.2 | 9.5 | 10.7 | |
| 10th percentile | 64.3 | 67.9 | 67.9 | 71.4 | 71.4 | 71.4 | |
| 90th percentile | 96.4 | 96.4 | 96.4 | 96.4 | 96.4 | 96.4 | |
| Boys | |||||||
| Grade | 1 | 2 | 3 | 4 | 5 | 6 | |
| Height (m) | mean | 1.24 | 1.30 | 1.36 | 1.41 | 1.47 | 1.53 |
| SD | 0.06 | 0.06 | 0.06 | 0.06 | 0.08 | 0.08 | |
| 10th percentile | 1.16 | 1.23 | 1.29 | 1.33 | 1.37 | 1.42 | |
| 90th percentile | 1.31 | 1.38 | 1.44 | 1.49 | 1.57 | 1.62 | |
| Body Mass (kg) | mean | 23.8 | 27.3 | 31.1 | 35.0 | 39.0 | 42.5 |
| SD | 4.3 | 4.1 | 5.8 | 6.9 | 8.0 | 8.5 | |
| 10th percentile | 19.4 | 22.7 | 25.0 | 27.3 | 30.9 | 33.3 | |
| 90th percentile | 29.4 | 33.1 | 37.6 | 45.2 | 49.8 | 54.2 | |
| WHtR | mean | 0.46 | 0.46 | 0.45 | 0.46 | 0.46 | 0.45 |
| SD | 0.03 | 0.04 | 0.04 | 0.04 | 0.06 | 0.05 | |
| 90th percentile | 0.42 | 0.43 | 0.41 | 0.39 | 0.41 | 0.40 | |
| 10th percentile | 0.50 | 0.51 | 0.52 | 0.50 | 0.54 | 0.51 | |
| WC (cm) | mean | 56.9 | 59.9 | 61.5 | 64.5 | 67.1 | 68.8 |
| SD | 5.0 | 5.3 | 6.6 | 7.4 | 8.4 | 8.0 | |
| 90th percentile | 51.1 | 54.5 | 54.0 | 56.5 | 59.0 | 60.0 | |
| 10th percentile | 63.0 | 67.0 | 70.0 | 75.0 | 79.0 | 80.0 | |
| SBP (mmHg) | mean | 104 | 107 | 110 | 109 | 112 | 113 |
| SD | 9 | 10 | 9 | 10 | 9 | 11 | |
| 90th percentile | 93 | 95 | 98 | 98 | 100 | 98 | |
| 10th percentile | 116 | 118 | 122 | 120 | 123 | 127 | |
| HDL (mmol/L) | mean | 1.67 | 1.71 | 1.71 | 1.70 | 1.62 | 1.66 |
| SD | 0.39 | 0.35 | 0.37 | 0.33 | 0.36 | 0.35 | |
| 10th percentile | 1.25 | 1.24 | 1.20 | 1.30 | 1.20 | 1.20 | |
| 90th percentile | 2.25 | 2.10 | 2.30 | 2.10 | 2.10 | 2.10 | |
| Tot Chol (mmol/L) | mean | 4.31 | 4.24 | 4.33 | 4.30 | 4.30 | 4.24 |
| SD | 0.66 | 0.59 | 0.71 | 0.65 | 0.586 | 0.634 | |
| 90th percentile | 3.40 | 3.60 | 3.50 | 3.46 | 3.60 | 3.50 | |
| 10th percentile | 4.90 | 5.06 | 5.19 | 5.04 | 5.20 | 5.00 | |
| Andersen Test (m) | mean | 806 | 870 | 966 | 995 | 1009 | 1063 |
| SD | 112 | 118 | 126 | 132 | 120 | 111 | |
| 10th percentile | 641 | 740 | 790 | 849 | 840 | 915 | |
| 90th percentile | 949 | 1014 | 1116 | 1160 | 1160 | 1215 | |
| MVPA (min) | mean | 106 | 98 | 102 | 92 | 89 | 88 |
| SD | 26 | 26 | 28 | 29 | 30 | 28 | |
| 10th percentile | 73 | 65 | 67 | 76 | 54 | 57 | |
| 90th percentile | 136 | 135 | 139 | 135 | 130 | 128 | |
| QoL (%) | mean | 81.0 | 81.1 | 83.7 | 86.0 | 86.0 | 86.0 |
| SD | 13.08 | 13.0 | 9.9 | 9.3 | 9.3 | 9.3 | |
| 10th percentile | 62.93 | 64.3 | 70.4 | 75.0 | 75.0 | 75.0 | |
| 90th percentile | 97.9 | 96.4 | 96.4 | 96.4 | 96.4 | 96.4 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mamen, A.; Braaum, L.E.; Fredriksen, P.M. Presenting Health Status in Children Using a Radar Plot. Sports 2020, 8, 53. https://doi.org/10.3390/sports8040053
Mamen A, Braaum LE, Fredriksen PM. Presenting Health Status in Children Using a Radar Plot. Sports. 2020; 8(4):53. https://doi.org/10.3390/sports8040053
Chicago/Turabian StyleMamen, Asgeir, Lars Erik Braaum, and Per Morten Fredriksen. 2020. "Presenting Health Status in Children Using a Radar Plot" Sports 8, no. 4: 53. https://doi.org/10.3390/sports8040053





