Prognostic Role of Androgen Receptor in Triple Negative Breast Cancer: A Multi-Institutional Study
Abstract
:1. Introduction
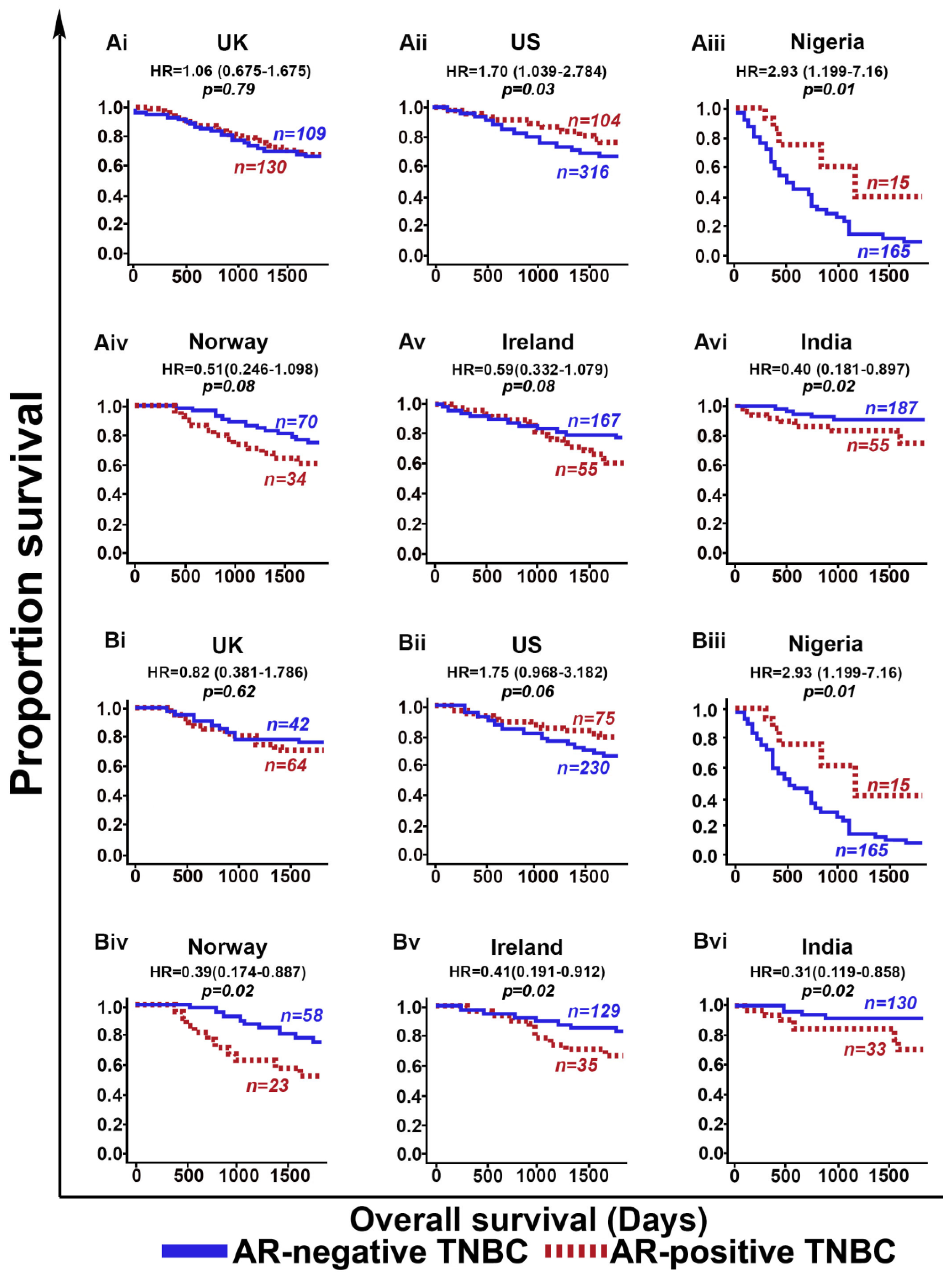
2. Results and Discussion
3. Materials and Methods
3.1. Study Cohorts and Samples
3.2. Immunohistochemistry (IHC)
3.3. Assessment of IHC Staining
3.4. Statistical Analyses
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature 2012, 490, 61–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bianchini, G.; Balko, J.M.; Mayer, I.A.; Sanders, M.E.; Gianni, L. Triple-negative breast cancer: Challenges and opportunities of a heterogeneous disease. Nat. Rev. Clin. Oncol. 2016, 13, 674–690. [Google Scholar] [CrossRef] [PubMed]
- Burstein, M.D.; Tsimelzon, A.; Poage, G.M.; Covington, K.R.; Contreras, A.; Fuqua, S.A.; Savage, M.I.; Osborne, C.K.; Hilsenbeck, S.G.; Chang, J.C.; et al. Comprehensive genomic analysis identifies novel subtypes and targets of triple-negative breast cancer. Clin. Cancer Res. 2015, 21, 1688–1698. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, B.D.; Bauer, J.A.; Chen, X.; Sanders, M.E.; Chakravarthy, A.B.; Shyr, Y.; Pietenpol, J.A. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J. Clin. Investig. 2011, 121, 2750–2767. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robinson, J.L.; Macarthur, S.; Ross-Innes, C.S.; Tilley, W.D.; Neal, D.E.; Mills, I.G.; Carroll, J.S. Androgen receptor driven transcription in molecular apocrine breast cancer is mediated by FoxA1. EMBO J. 2011, 30, 3019–3027. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sutton, L.M.; Cao, D.; Sarode, V.; Molberg, K.H.; Torgbe, K.; Haley, B.; Peng, Y. Decreased androgen receptor expression is associated with distant metastases in patients with androgen receptor-expressing triple-negative breast carcinoma. Am. J. Clin. Pathol. 2012, 138, 511–516. [Google Scholar] [CrossRef]
- Tang, D.; Xu, S.; Zhang, Q.; Zhao, W. The expression and clinical significance of the androgen receptor and E-cadherin in triple-negative breast cancer. Med. Oncol. 2012, 29, 526–533. [Google Scholar] [CrossRef]
- Masuda, H.; Baggerly, K.A.; Wang, Y.; Zhang, Y.; Gonzalez-Angulo, A.M.; Meric-Bernstam, F.; Valero, V.; Lehmann, B.D.; Pietenpol, J.A.; Hortobagyi, G.N.; et al. Differential response to neoadjuvant chemotherapy among 7 triple-negative breast cancer molecular subtypes. Clin. Cancer Res. 2013, 19, 5533–5540. [Google Scholar] [CrossRef]
- Santonja, A.; Sanchez-Munoz, A.; Lluch, A.; Chica-Parrado, M.R.; Albanell, J.; Chacon, J.I.; Antolin, S.; Jerez, J.M.; De la Haba, J.; De Luque, V.; et al. Triple negative breast cancer subtypes and pathologic complete response rate to neoadjuvant chemotherapy. Oncotarget 2018, 9, 26406–26416. [Google Scholar] [CrossRef] [Green Version]
- Cochrane, D.R.; Bernales, S.; Jacobsen, B.M.; Cittelly, D.M.; Howe, E.N.; D‘Amato, N.C.; Spoelstra, N.S.; Edgerton, S.M.; Jean, A.; Guerrero, J.; et al. Role of the androgen receptor in breast cancer and preclinical analysis of enzalutamide. Breast Cancer Res. Bcr 2014, 16, R7. [Google Scholar] [CrossRef]
- Diana, A.; Franzese, E.; Centonze, S.; Carlino, F.; Della Corte, C.M.; Ventriglia, J.; Petrillo, A.; De Vita, F.; Alfano, R.; Ciardiello, F.; et al. Triple-Negative Breast Cancers: Systematic Review of the Literature on Molecular and Clinical Features with a Focus on Treatment with Innovative Drugs. Curr. Oncol. Rep. 2018, 20, 76. [Google Scholar] [CrossRef]
- Gerratana, L.; Basile, D.; Buono, G.; De Placido, S.; Giuliano, M.; Minichillo, S.; Coinu, A.; Martorana, F.; De Santo, I.; Del Mastro, L.; et al. Androgen receptor in triple negative breast cancer: A potential target for the targetless subtype. Cancer Treat. Rev. 2018, 68, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Asano, Y.; Kashiwagi, S.; Goto, W.; Tanaka, S.; Morisaki, T.; Takashima, T.; Noda, S.; Onoda, N.; Ohsawa, M.; Hirakawa, K.; et al. Expression and Clinical Significance of Androgen Receptor in Triple-Negative Breast Cancer. Cancers 2017, 9. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Peng, R.; Yuan, Z.; Wang, S.; Peng, J.; Lin, G.; Jiang, X.; Qin, T. Prognostic value of androgen receptor expression in operable triple-negative breast cancer: A retrospective analysis based on a tissue microarray. Med. Oncol. 2012, 29, 406–410. [Google Scholar] [CrossRef] [PubMed]
- McGhan, L.J.; McCullough, A.E.; Protheroe, C.A.; Dueck, A.C.; Lee, J.J.; Nunez-Nateras, R.; Castle, E.P.; Gray, R.J.; Wasif, N.; Goetz, M.P.; et al. Androgen receptor-positive triple negative breast cancer: A unique breast cancer subtype. Ann. Surg. Oncol. 2014, 21, 361–367. [Google Scholar] [CrossRef]
- Mrklic, I.; Pogorelic, Z.; Capkun, V.; Tomic, S. Expression of androgen receptors in triple negative breast carcinomas. Acta Histochem. 2013, 115, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Barton, V.N.; Christenson, J.L.; Gordon, M.A.; Greene, L.I.; Rogers, T.J.; Butterfield, K.; Babbs, B.; Spoelstra, N.S.; D‘Amato, N.C.; Elias, A.; et al. Androgen Receptor Supports an Anchorage-Independent, Cancer Stem Cell-like Population in Triple-Negative Breast Cancer. Cancer Res. 2017, 77, 3455–3466. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Yang, F.; Zhang, W.; Song, W.; Liu, Y.; Guan, X. The Androgen Receptor Promotes Cellular Proliferation by Suppression of G-Protein Coupled Estrogen Receptor Signaling in Triple-Negative Breast Cancer. Cell. Physiol. Biochem. 2017, 43, 2047–2061. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.; Tripathi, S.; Hughley, R.; He, Q.; Bae, S.; Karanam, B.; Martini, R.; Newman, L.; Colomb, W.; Grizzle, W.; et al. AR negative triple negative or "quadruple negative" breast cancers in African American women have an enriched basal and immune signature. PLoS ONE 2018, 13, e0196909. [Google Scholar] [CrossRef]
- Lehmann-Che, J.; Hamy, A.S.; Porcher, R.; Barritault, M.; Bouhidel, F.; Habuellelah, H.; Leman-Detours, S.; De Roquancourt, A.; Cahen-Doidy, L.; Bourstyn, E.; et al. Molecular apocrine breast cancers are aggressive estrogen receptor negative tumors overexpressing either HER2 or GCDFP15. Breast Cancer Res. 2013, 15, R37. [Google Scholar] [CrossRef]
- Zhu, J.J.; Jiao, D.C.; Qiao, J.H.; Wang, L.N.; Ma, Y.Z.; Lu, Z.D.; Liu, Z.Z. Analysis of predictive effect of Androgen receptor on the response to neoadjuvant chemotherapy in breast cancer patients. Zhonghua Yi Xue Za Zhi 2018, 98, 601–605. [Google Scholar] [CrossRef] [PubMed]

| Multivariate Cox Regression Analysis of Common Clinicopathological Variables and AR | |||||
|---|---|---|---|---|---|
| Variables | US and Nigeria Study Cohorts | Norway, Ireland and India Study Cohorts | |||
| Hazard Ratio (95% CI) | p-value | Hazard Ratio (95% CI) | p-value | ||
| Overall Survival | |||||
| Age | <50 vs. ≥50 | 1.00 (0.99–1.01) | 0.3934 | 1.03 (1.01–1.05) | <0.001 |
| Grade | 2 | 0.77 (0.86–8.84) | 0.085 | 0.25 (0.05–1.17) | 0.0801 |
| Grade | 3 | 3.63 (1.15–11.44) | 0.0275 | 0.37 (0.09–1.56) | 0.1777 |
| Adjuvant Chemotherapy | treated vs. non-treated | 0.72 (0.39–1.32) | 0.2877 | 0.91 (0.56–1.47) | 0.7026 |
| Population | AA | 1.82 (1.30–2.53) | 0.0004 | - | - |
| Population | African | 11.22 (8.11–15.51) | <0.0001 | - | - |
| Population | Indian | - | - | 0.49 (0.27–0.89) | 0.0201 |
| Population | Irish | - | - | 0.79 (0.48–1.28) | 0.3462 |
| AR | AR-positive vs. AR-negative | 1.70 (1.10–2.61) | 0.0157 | 0.58 (0.37–0.90) | 0.0154 |
| Clinicopathological Variables of Study Cohorts | ||||||
|---|---|---|---|---|---|---|
| Variables | UK | Norway | Ireland | US | Nigeria | India |
| n = 239 | n = 104 | n = 222 | n = 420 | n = 180 | n = 242 | |
| Age | ||||||
| <50 | 128 (53.55) | 45 (43.3) | 55 (24.8) | 129 (30.7) | 97 (53.9) | 122 (50.4) |
| ≥50 | 111 (46.45) | 59 (56.7) | 167 (75.2) | 291 (69.3) | 83 (46.1) | 120 (49.6) |
| Clinical stage | ||||||
| I/II | 212 (88.7) | 91 (87.5) | 177 (79.7) | 320 (76.2) | NA | NA |
| III/IV | 26 (10.9) | 11 (10.6) | 34 (15.3) | 84 (20) | NA | NA |
| Missing | 1 (0.4) | 2 (1.9) | 11 (5.0) | 16 (3.8) | NA | NA |
| Grade | ||||||
| 1 | 5 (2.1) | 1 (1.0) | 2 (0.9) | 11 (2.6) | 7 (3.9) | 0 (0) |
| 2 | 12 (5.0) | 15 (14.4) | 31 (14) | 79 (18.8) | 68 (37.8) | 13 (5.4) |
| 3 | 221 (92.5) | 83 (79.8) | 189 (85.1) | 322 (76.7) | 101 (56.1) | 228 (94.2) |
| Missing | 1 (0.4) | 5 (4.8) | 0 (0) | 8 (1.9) | 4 (2.2) | 1 (0.4) |
| Chemotherapy | ||||||
| Treated | 106 (44.4) | 81 (77.9) | 164 (73.9) | 305 (72.6) | 180 (100) | 163 (67.4) |
| Untreated | 110 (46) | 20 (19.2) | 58 (26.1) | 56 (13.3) | 0 (0) | 46 (19.2) |
| Missing | 23 (9.6) | 3 (2.9) | 0 (0) | 59 (14.1) | 0 (0) | 33 (13.4) |
| Vital status | ||||||
| Dead | 112 (46.9) | 44 (42.3) | 56 (25.2) | 131 (31.2) | 139 (77.2) | 28 (11.6) |
| Alive | 127 (53.1) | 60 (57.7) | 166 (74.8) | 289 (68.8) | 41 (22.8) | 214 (88.4) |
| Androgen Receptor | ||||||
| Positive | 130 (54.9) | 34 (32.7) | 55 (24.77) | 104 (24.8) | 15 (8.3) | 55 (22.7) |
| Negative | 109 (45.1) | 70 (67.3) | 167 (75.3) | 316 (75.2) | 165 (91.7) | 187 (77.3) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bhattarai, S.; Klimov, S.; Mittal, K.; Krishnamurti, U.; Li, X.; Oprea-Ilies, G.; Wetherilt, C.S.; Riaz, A.; Aleskandarany, M.A.; Green, A.R.; et al. Prognostic Role of Androgen Receptor in Triple Negative Breast Cancer: A Multi-Institutional Study. Cancers 2019, 11, 995. https://doi.org/10.3390/cancers11070995
Bhattarai S, Klimov S, Mittal K, Krishnamurti U, Li X, Oprea-Ilies G, Wetherilt CS, Riaz A, Aleskandarany MA, Green AR, et al. Prognostic Role of Androgen Receptor in Triple Negative Breast Cancer: A Multi-Institutional Study. Cancers. 2019; 11(7):995. https://doi.org/10.3390/cancers11070995
Chicago/Turabian StyleBhattarai, Shristi, Sergey Klimov, Karuna Mittal, Uma Krishnamurti, Xiaoxian (Bill) Li, Gabriela Oprea-Ilies, Ceyda Sonmez Wetherilt, Ansa Riaz, Mohammed A. Aleskandarany, Andrew R. Green, and et al. 2019. "Prognostic Role of Androgen Receptor in Triple Negative Breast Cancer: A Multi-Institutional Study" Cancers 11, no. 7: 995. https://doi.org/10.3390/cancers11070995






