1. Introduction
Increasing rates of overweight and obesity across adult populations globally pose an important challenge for public health authorities [
1]. A high body mass index (BMI) is associated with increased risk of cardiovascular disease, type 2 diabetes, several types of cancer, and many other disorders which add to the global burden of chronic disabilities [
2,
3]. Moreover, these conditions or their precursors are more likely to affect young people who are overweight or obese [
4]. Currently in England around 60% of all adults and one in three young people between the age of 16 and 24 years are obese or overweight [
5], with more recent cohorts of young adults having a steeper increase in BMI than their predecessors [
6,
7].
The observed trends in excess body weight in young adulthood may be explained by the prevalence of risk behaviours for overweight and obesity between the ages of 18 and 25 years [
8]. Among other factors, high alcohol intake may play an important role in weight gain during this period [
9]. The potential relationship between alcohol intake and body weight arises from both biological and behavioural pathways. Biologically, alcohol contributes to increased fat stores in the body. Its metabolism inhibits lipid oxidation as one of its main metabolites, acetate, represents a readily available energy source that is used by the body in preference to fat; a phenomenon which is more pronounced with diets that are already high in fat and energy [
10]. It has also been suggested that unhealthy food choices are more likely to be made during and directly after a period of alcohol consumption [
11] which could, at least in part, be due to the disinhibiting effect of alcohol as a psychoactive substance that can alter usual behaviour [
12]; or also because of the appetite enhancing effect of alcohol [
13].
Behaviourally, alcohol consumption is typically accompanied by diets higher in fat and other risk factors for elevated adiposity, such as smoking and sedentary activities [
14].
Evidence from epidemiological studies of the relationship between alcohol intake and body weight in adults is mixed. Whereas most studies have found an inverse relationship between overweight/obesity and more frequent drinking, evidence regarding the relationship with the amount of alcohol consumed is less clear [
15,
16,
17,
18,
19]. At the same time, non-drinkers have been found to have higher BMI or obesity risk compared to drinkers, suggesting a non-linear relationship between alcohol and obesity [
20,
21,
22]. So far, however, few studies have looked at the relationship between alcohol consumption and obesity in young adults, a point in the life course at which the relationship between BMI and alcohol intake may be less affected by reverse causation. For example, in older adults it may be difficult to know if alcohol consumption increases likelihood of being obese or being obese leads to high alcohol intake.
The type of alcoholic drink may show different relationships with BMI. Studies looking at adult populations (>18 years) have generally found no association between wine consumption and BMI and positive associations for beer and spirits, particularly in men [
23], possibly reflecting broader lifestyle patterns for which spirits or beer are the preferred alcoholic beverages [
19,
24]. In the UK, wine is less popular than “white” spirits (e.g., vodka, gin, white rum and tequila) with 18 to 24 year-olds, and these spirits are more popular in this age group than with any other age group of consumers [
24]. This preference may influence the shape of the BMI-alcohol intake association in young adults.
The relationship of alcohol consumption to body weight varies between men and women because of different cultural norms around alcohol [
19,
24] and because of differences by sex in alcohol metabolism that reflect differences in body fat between men and women [
9]. In the following study, young adults were defined as individuals between 18 to 25 years of age. This age group has the heaviest concentration of acute alcohol harms such as accidents and assaults, in part because of social and environmental factors encouraging patterns of excessive drinking during this period [
25,
26]. Notably, these patterns of excessive drinking have the potential to set individuals onto drinking and overweight trajectories that persist into the rest of adult life [
26,
27,
28]. Understanding the relationship between alcohol intake and BMI in young adults is therefore important to inform the wider debate on the effects of alcohol on young individuals’ health and well-being.
The aim of this study was to determine the relationship between alcohol intake, expressed as percentage of the gender-specific recommended dietary allowance (RDA) of energy (% RDA Energy) from alcoholic beverages (excluding mixers) on the heaviest drinking day in the last seven days, and BMI in young adults. Expressing alcoholic beverage intake as a proportion of energy and standardising as a proportion of gender specific recommendations for energy illustrates the consumption that could contribute to obesity.
4. Discussion
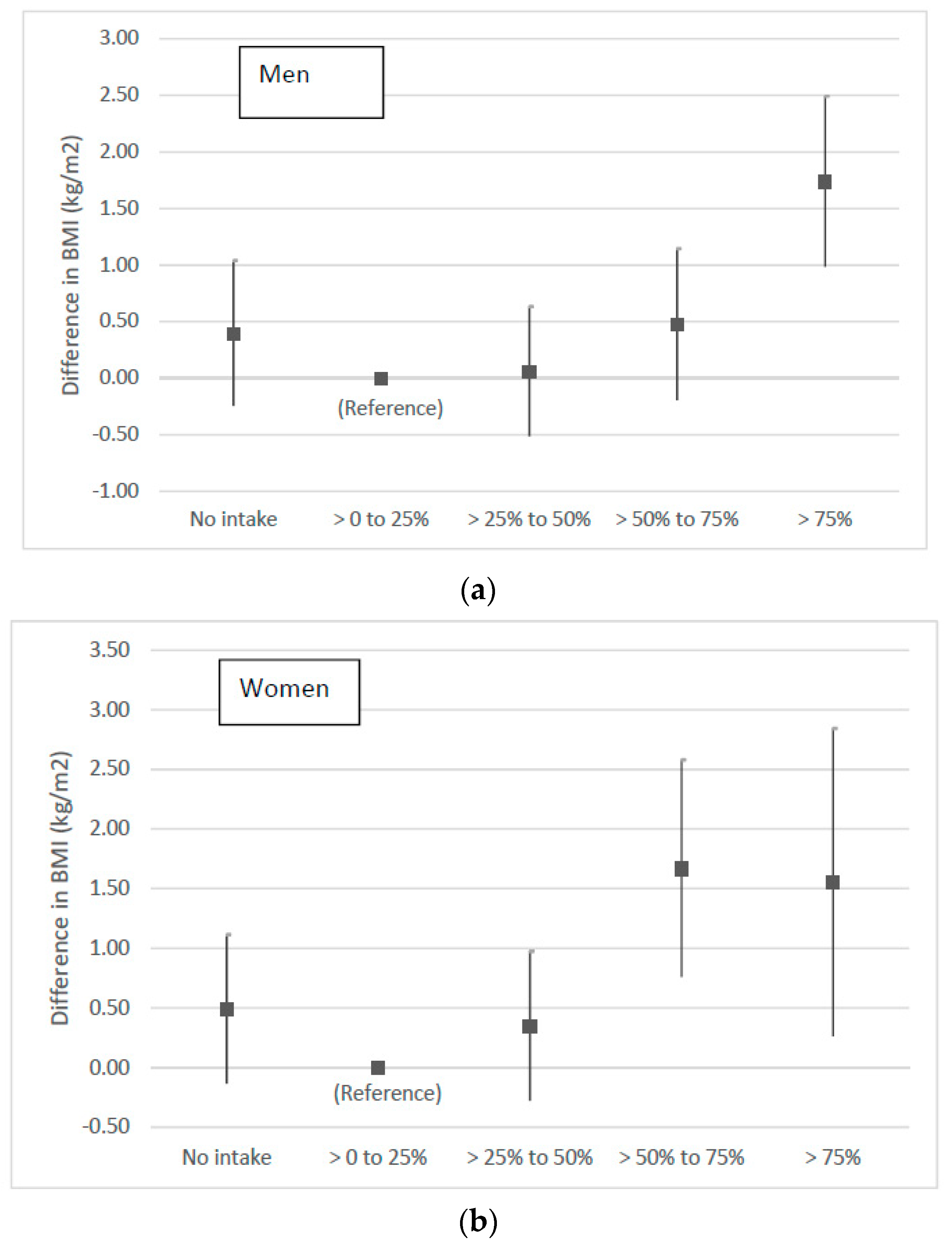
This study used large national samples from the Health Survey for England and the Scottish Health Survey to explore the relationship between BMI and the contribution to total energy from alcoholic beverage consumption on the heaviest drinking day as a percentage of the recommended daily allowance (RDA) for energy in 18 to 25 year-olds. This measure was used to emphasise the large contribution that alcoholic beverages can make to the gender specific energy RDA and the potential for excessive energy intake on heavy drinking days. Many other studies have used frequency or the average amount of alcohol consumed over a period of a week, but in the study described here the energy consumed in the single heaviest drinking session in the past week was used. This is because a single session potentially has more impact on fat stores as alcohol metabolism inhibits lipid oxidation [
9]. Results showed a trend towards a non-linear J-shaped relationship of alcohol intake with BMI, with a significant positive association between alcohol consumption and BMI observed only at Very High levels of intake (>75% RDA Energy) in men and High to Very High intakes (>50% RDA Energy energy) in women. At the same time, in both men and women, the observed relationship between consumption of different types of alcoholic beverages and BMI was similar, The only exception was for beer and women where there was no significant association for any category of % RDA Energy.
The main results on the relationship between % RDA Energy from alcoholic beverages and BMI found in men are consistent with broader findings in the literature on the association between the amount of alcohol consumed and excess body weight: namely that the amount of alcohol consumed is positively associated with BMI, but that it is higher levels of drinking (excluding alcohol dependence) that significantly influence excess body weight [
11,
19,
20,
33,
38]. In the case of women, findings of an inverse relationship or a U-shaped relationship between alcohol intake and BMI have been observed more often than in men, possibly driven by higher number of non-drinkers in women generally [
15,
20,
39]. Our results instead showed a positive relationship with alcohol intake that flattened out at High and Very High levels of consumption (>50% RDA Energy),
It has been suggested that a positive relationship between BMI with high alcohol intake may exist because individuals who consume high levels of alcohol may fail to compensate for the energy intake from alcohol by consuming fewer kcals from food. The evidence for this, however, is stronger for the consumption of spirits and beer than for wine [
33,
38]. Differences in the relationship between alcohol intake and BMI for different types of drink may be related to differences in dietary and lifestyle patterns associated with consumption of wine, spirits and beer. Wine consumers have been found to eat more fruit and vegetables, and less meat, fried foods, ready-meals, butter, margarine, and eggs, than individuals who mainly drink spirits and beer [
40,
41,
42]. However, our study showed an association with higher BMI for both greater wine and spirits intake, in both men and women, and a positive association with beer intake in men, but not in women. This may be due to the fewer women in the sample drinking a lot of beer, reflecting trends in gender preferences for this alcoholic drink [
23,
24]. It may also reflect more complex associations between BMI and alcohol intake in women than in men, due to metabolic differences between the sexes [
43].
A wealth of epidemiological evidence suggests that non-drinkers have higher BMIs than drinkers [
44]. In terms of dietary habits, non-drinkers have been found to consume more energy from carbohydrates than drinkers, which could account for additional differences in body weight [
38]. Recent evidence on excess body weight differences between drinkers and abstainers suggests, however, that this effect may be driven by differences in BMI between drinkers and ex-drinkers rather than between drinkers and abstainers as a whole [
16]. This is because some ex-drinkers stop consuming alcohol in response to health problems that may affect or be a consequence of high BMI. Results for this study refer to the amount of alcohol consumption controlling for frequency of intake, which implies that this effect may have been attenuated in our results. In fact, in the analyses for the current study no statistically significant differences were found between None and the Low category (the reference level of % RDA Energy). The relatively low proportion of ex-drinkers in the 18 to 25 year group may also have made it difficult to detect any important differences in BMI by level of alcohol intake; only 2% of men 18 to 25 years and 4% of women 18 to 25 years reported being ex-drinkers compared to 6% and 7% for the overall (>18 years) adult sample in the combined HSE and SHeS data.
Both BMI level and alcohol intake may be related to a number of other lifestyle and environmental variables that influence individuals’ weight and alcohol outcomes. An important strength of this study was the ability to take into account a wide range of potential confounders of this relationship, including physical activity, limiting longstanding illness and sociodemographic characteristics of respondents. However, it was not possible to account for food intake associated with alcoholic beverage consumption on the heaviest day of drinking as these data were not collected. It is established that unhealthy food choices are more likely to be made during and directly after a period of excessive alcohol consumption [
11]. A further limitation arises from the fact that alcohol intake is likely to be underreported, a phenomena that is has been seen to be more pronounced amongst young males [
45]. In addition the data used to calculate energy intakes from alcoholic beverages was obtained from an organisation largely funded by UK alcohol producers, retailers and supermarkets which was chosen as the most suitable available at the time. We have since cross-checked this data with the summarised energy and nutrients supplied to the Living Costs and Food Survey by the Department of Health and Public Health England based on that used for the National Diet and Nutrition Survey. The energy values are compatible with those provided by the organisation [
32].
Given the sample size, a limitation of the study was the impossibility of analysing the relationship between alcohol intake and BMI by levels of body overweight. This might have shown stronger associations of BMI with different levels of alcohol intake as some studies suggest that individuals that are already overweight are more prone to weight gain from increased levels of alcohol consumption [
10,
46]. Moreover, we cannot exclude the possibility that the relationships observed between alcohol consumption and BMI were influenced by confounding from unobserved time-invariant factors related to both drinking and body weight that introduce bias in estimates of associations from cross-sectional analyses. As with other studies in the area, the ability to fully explore the relationship between BMI and the amount of alcohol consumed may have been limited by the low participation of individuals with very high levels of alcohol consumption in health surveys [
38]. In addition, the HSE and SHeS response rates for eligible adults range between 59% and 55%, but disaggregated response rates by age groups are not reported, so it is possible that young men and women who are very high alcohol consumers had lower response rates in the survey samples.
The present study provides greater understanding of the likely contribution of alcohol consumption to BMI. Findings show a positive association between BMI and alcohol intake on the heaviest day of drinking but only High and Very High levels of intake (>50% of RDA Energy except for wine in women) are likely to be associated with changes in BMI. Patterns of the relationship of BMI and alcohol intake are similar for consumption of beer, wine, and spirits with slight variations by sex. More longitudinal studies are necessary to confirm these results and elaborate on causal mechanisms at the population level to better explain how alcohol intake impacts BMI. Future work may benefit from including other socio-psychological variables such as personality traits, [
47] cultural factors, and policies (e.g., licensing hours) that may predispose to excessive calorie and alcohol consumption.
The findings have several important policy and practice implications. Firstly, for advocacy organisations concerned with alcohol-related harm, or obesity, there may be synergies and opportunities in collaborating. This study further demonstrates that the two problems are interrelated, and it is well-recognised that the policy solutions most likely to be effective-increasing the price of unhealthy commodities, reducing their availability and regulating and reducing marketing exposure–also overlap. Similarly, the political challenges inherent in achieving policy change in these areas may be similar, as action on both is heavily opposed by powerful industry interests. Secondly, for governments developing strategies to reduce obesity and alcohol-related harm, this evidence presents a strong case for such policies to be integrated, or at least strongly cross-referenced. In many countries alcohol policy is combined with policy for illicit drugs, or tobacco, whereas the potential arguments for and synergies from linking alcohol and obesity policy may be (at least) equally strong.