Fully Immersive Virtual Reality-Based Cognitive Remediation for Adults with Psychosocial Disabilities: A Systematic Scoping Review of Methods Intervention Gaps and Meta-Analysis of Published Effectiveness Studies
Abstract
:1. Introduction
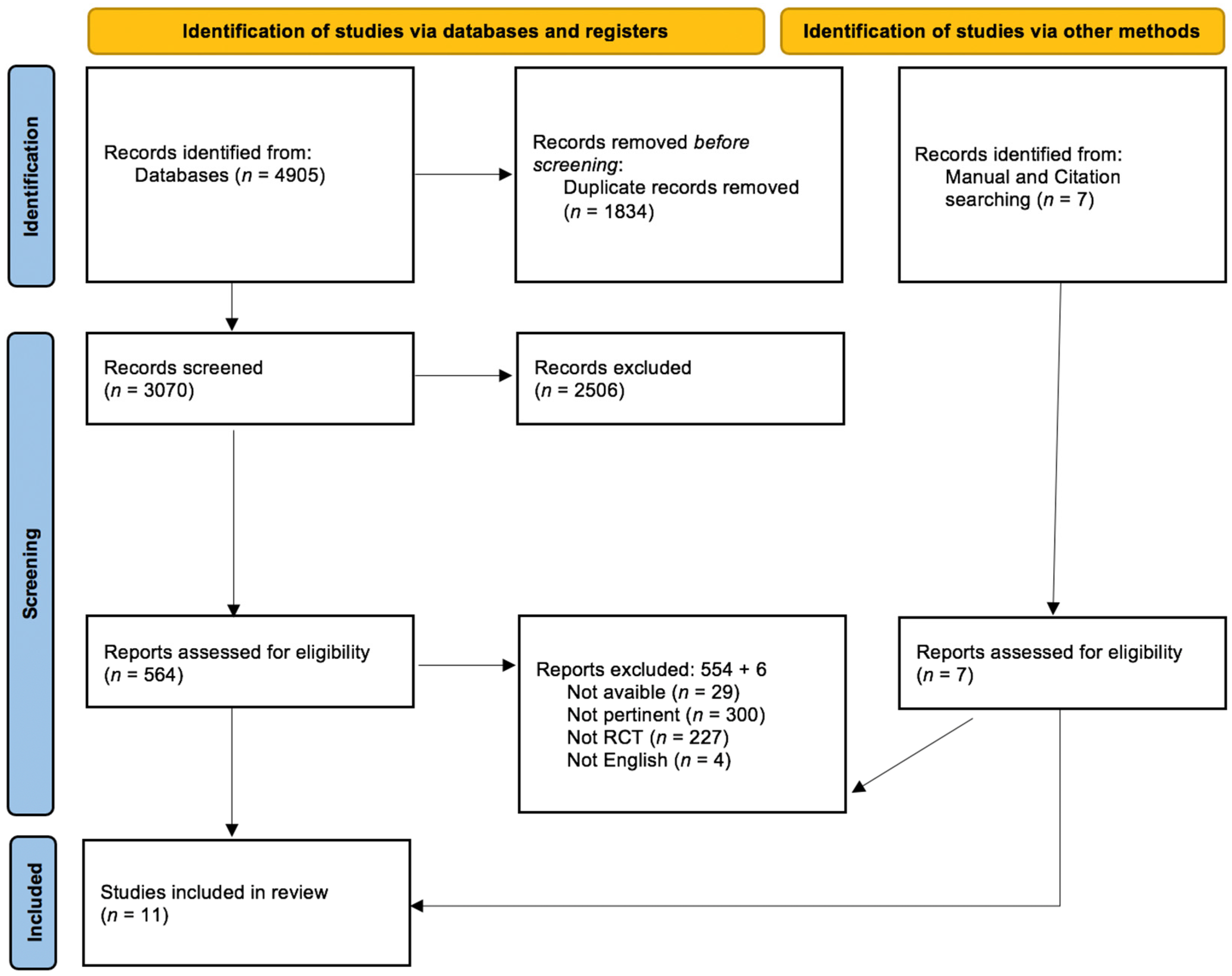
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria and Data Extraction
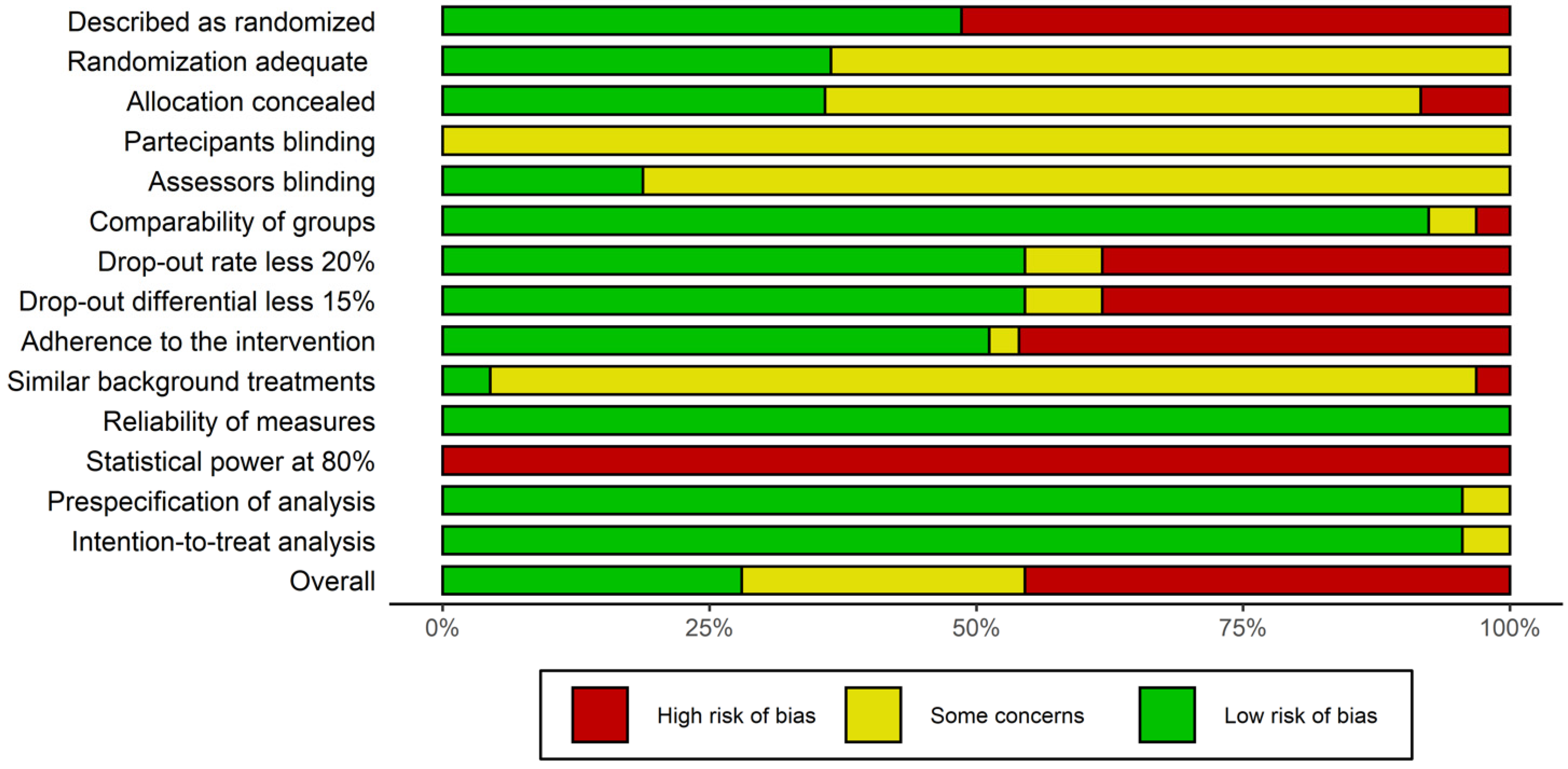
2.3. Quality Assessment of the Studies
2.4. Meta Analysis
3. Results
3.1. Search Results and Study Selection
3.2. Descriptions of Studies
3.3. Assessment of the Risk of Bias
3.4. Synthesis of the Meta-Analysis
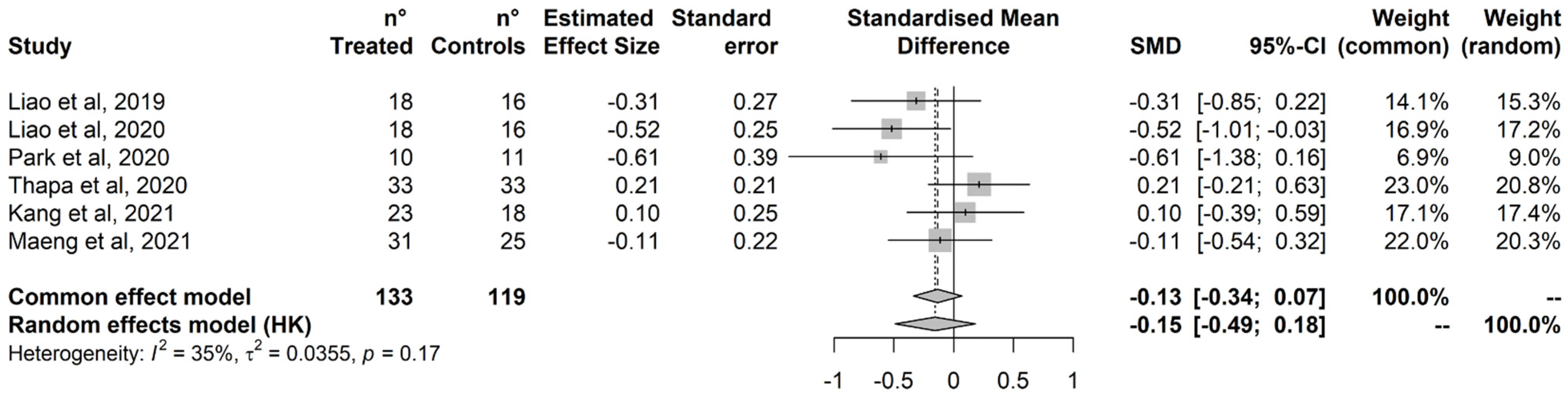
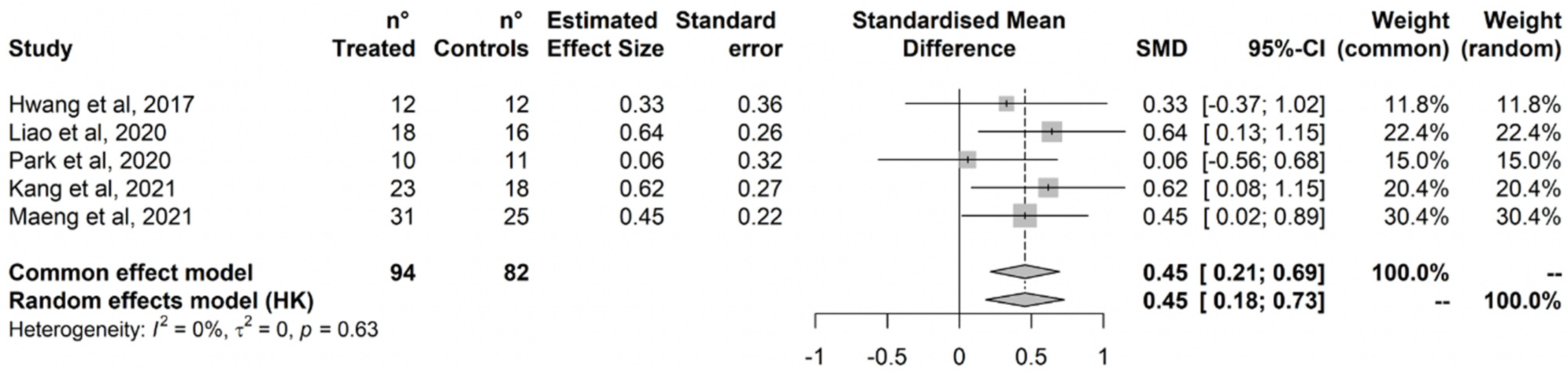
3.4.1. Executive Functions
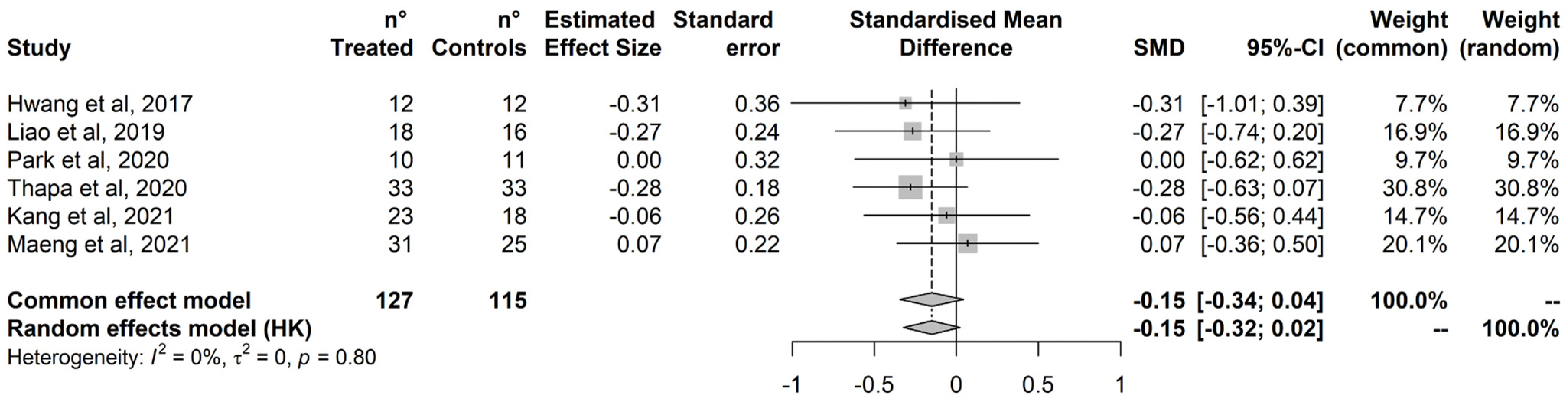
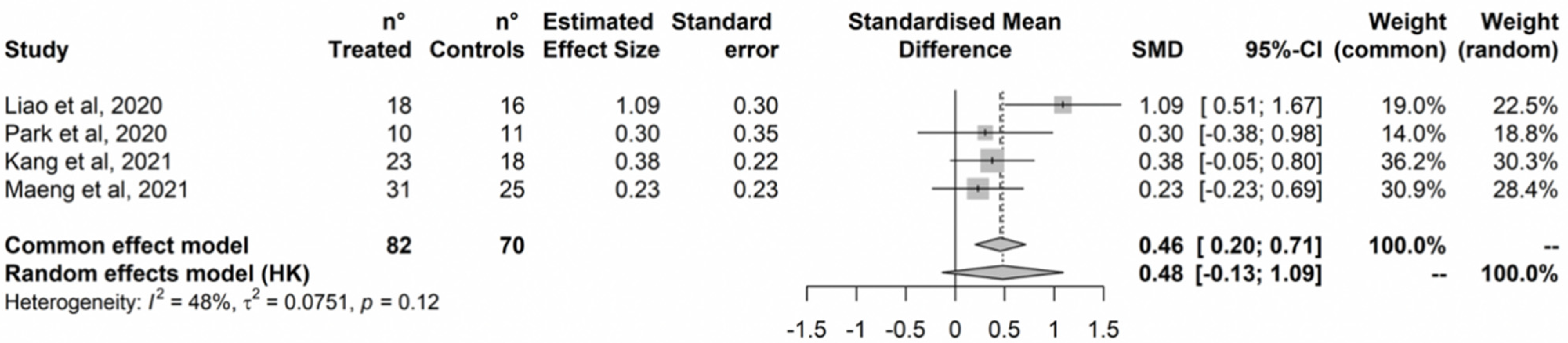
3.4.2. Attention
3.4.3. Memory
3.4.4. Language
3.4.5. Global Cognition
4. Discussion
4.1. Implication for Research and Clinics
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. The World Health Report 2001: Mental Health: New Understanding, New Hope; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Saxena, S.; Setoya, Y. World Health Organization’s Comprehensive Mental Health Action Plan 2013-2020. Psychiatry Clin. Neurosci. 2014, 68, 585–586. [Google Scholar] [CrossRef] [PubMed]
- Vigo, D.; Thornicroft, G.; Atun, R. Estimating the true global burden of mental illness. Lancet Psychiatry 2016, 3, 171–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts, N.L.; Mountjoy-Venning, W.C.; Anjomshoa, M.; Banoub, J.A.M.; Yasin, Y.J. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [Green Version]
- Harvey, P.D. What is the evidence for changes in cognition and functioning over the lifespan in patients with schizophrenia? J. Clin. Psychiatry 2014, 75 (Suppl. 2), 34–38. [Google Scholar] [CrossRef]
- Vita, A.; Barlati, S.; Ceraso, A.; Nibbio, G.; Ariu, C.; Deste, G.; Wykes, T. Effectiveness, Core Elements, and Moderators of Response of Cognitive Remediation for Schizophrenia: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Psychiatry 2021, 78, 848–858. [Google Scholar] [CrossRef] [PubMed]
- Sharma, T.; Antonova, L. Cognitive function in schizophrenia. Deficits, functional consequences, and future treatment. Psychiatr. Clin. N. Am. 2003, 26, 25–40. [Google Scholar] [CrossRef] [PubMed]
- Gold, A.K.; Montana, R.E.; Sylvia, L.G.; Nierenberg, A.A.; Deckersbach, T. Cognitive Remediation and Bias Modification Strategies in Mood and Anxiety Disorders. Curr. Behav. Neurosci. Rep. 2016, 3, 340–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tchanturia, K.; Davies, H.; Campbell, I.C. Cognitive remediation therapy for patients with anorexia nervosa: Preliminary findings. Ann. Gen. Psychiatry 2007, 6, 14. [Google Scholar] [CrossRef] [Green Version]
- Douglas, K.M.; Gallagher, P.; Robinson, L.J.; Carter, J.D.; McIntosh, V.V.; Frampton, C.M.; Watson, S.; Young, A.H.; Ferrier, I.N.; Porter, R.J. Prevalence of cognitive impairment in major depression and bipolar disorder. Bipolar Disord. 2018, 20, 260–274. [Google Scholar] [CrossRef]
- Vita, A.; Deste, G.; Barlati, S.; Poli, R.; Cacciani, P.; De Peri, L.; Sacchetti, E. Feasibility and effectiveness of cognitive remediation in the treatment of borderline personality disorder. Neuropsychol. Rehabil. 2018, 28, 416–428. [Google Scholar] [CrossRef]
- Peyroux, E.; Franck, N. RC2S: A Cognitive Remediation Program to Improve Social Cognition in Schizophrenia and Related Disorders. Front. Hum. Neurosci. 2014, 8, 400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Solé, B.; Jiménez, E.; Torrent, C.; Reinares, M.; Bonnin, C.; Torres, I.; Varo, C.; Grande, I.; Valls, E.; Salagre, E.; et al. Cognitive Impairment in Bipolar Disorder: Treatment and Prevention Strategies. Int. J. Neuropsychopharmacol. 2017, 20, 670–680. [Google Scholar] [CrossRef] [PubMed]
- Carta, M.G.; Ouali, U.; Perra, A.; Ben Cheikh Ahmed, A.; Boe, L.; Aissa, A.; Lorrai, S.; Cossu, G.; Aresti, A.; Preti, A.; et al. Living With Bipolar Disorder in the Time of COVID-19: Biorhythms During the Severe Lockdown in Cagliari, Italy, and the Moderate Lockdown in Tunis, Tunisia. Front. Psychiatry 2021, 12, 634765. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, J.; Giangrande, E.; Weinberger, D.R.; Dickinson, D. The global cognitive impairment in schizophrenia: Consistent over decades and around the world. Schizophr. Res. 2013, 150, 42–50. [Google Scholar] [CrossRef] [Green Version]
- Keefe, R.S.; Fox, K.H.; Harvey, P.D.; Cucchiaro, J.; Siu, C.; Loebel, A. Characteristics of the MATRICS Consensus Cognitive Battery in a 29-site antipsychotic schizophrenia clinical trial. Schizophr. Res. 2011, 125, 161–168. [Google Scholar] [CrossRef]
- Shamsi, S.; Lau, A.; Lencz, T.; Burdick, K.E.; DeRosse, P.; Brenner, R.; Lindenmayer, J.P.; Malhotra, A.K. Cognitive and symptomatic predictors of functional disability in schizophrenia. Schizophr. Res. 2011, 126, 257–264. [Google Scholar] [CrossRef] [Green Version]
- Brissos, S.; Dias, V.V.; Kapczinski, F. Cognitive performance and quality of life in bipolar disorder. Can. J. Psychiatry 2008, 53, 517–524. [Google Scholar] [CrossRef] [Green Version]
- McGurk, S.; Twamley, E.; Sitzer, D.; McHugo, G.; Mueser, K. A meta analysis of cognitive remediation in schizophrenia. Am. J. Psychiatry 2007, 164, 1791–1802. [Google Scholar] [CrossRef] [Green Version]
- Piras, M.; Perra, A.; Gureje, O.; Preti, A.; Carta, M.G. The Current Quality of Web-Based Information on the Treatment of Bipolar Disorder: A Systematic Search. J. Clin. Med. 2022, 11, 5427. [Google Scholar] [CrossRef]
- Thérond, A.; Pezzoli, P.; Abbas, M.; Howard, A.; Bowie, C.R.; Guimond, S. The Efficacy of Cognitive Remediation in Depression: A Systematic Literature Review and Meta-Analysis. J. Affect. Disord. 2021, 284, 238–246. [Google Scholar] [CrossRef]
- Dandil, Y.; Smith, K.; Kinnaird, E.; Toloza, C.; Tchanturia, K. Cognitive Remediation Interventions in Autism Spectrum Condition: A Systematic Review. Front. Psychiatry 2020, 11, 722. [Google Scholar] [CrossRef] [PubMed]
- Firth, J.; Stubbs, B.; Rosenbaum, S.; Vancampfort, D.; Malchow, B.; Schuch, F.; Elliott, R.; Nuechterlein, K.H.; Yung, A.R. Aerobic Exercise Improves Cognitive Functioning in People with Schizophrenia: A Systematic Review and Meta-Analysis. Schizophr. Bull. 2017, 43, 546–556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brasure, M.; Desai, P.; Davila, H.; Nelson, V.A.; Calvert, C.; Jutkowitz, E.; Butler, M.; Fink, H.A.; Ratner, E.; Hemmy, L.S.; et al. Physical Activity Interventions in Preventing Cognitive Decline and Alzheimer-Type Dementia: A Systematic Review. Ann. Intern. Med. 2018, 168, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Montemagni, C.; Del Favero, E.; Riccardi, C.; Canta, L.; Toye, M.; Zanalda, E.; Rocca, P. Effects of Cognitive Remediation on Cognition, Metacognition, and Social Cognition in Patients with Schizophrenia. Front. Psychiatry 2021, 12, 649737. [Google Scholar] [CrossRef] [PubMed]
- Sancassiani, F.; Cocco, A.; Cossu, G.; Lorrai, S.; Trincas, G.; Floris, F.; Mellino, G.; Machado, S.; Nardi, A.E.; Fabrici, E.P.; et al. “VelaMente?!”—Sailin in a Crew to Improve Self-Efficacy in People with Psychosocial Disabilities: A Randomized Controlled Trial. Clin. Pract. Epidemiol. Ment. Health CP EMH 2017, 13, 200–212. [Google Scholar] [CrossRef] [Green Version]
- Sancassiani, F.; Lorrai, S.; Cossu, G.; Cocco, A.; Trincas, G.; Floris, F.; Mellino, G.; Machado, S.; Nardi, A.E.; Fabrici, E.P.; et al. The Effects of “VelaMente?!” Project on Social Functioning of People with Severe Psychosocial Disabilities. Clin. Pract. Epidemiol. Ment. Health CP EMH 2017, 13, 220–232. [Google Scholar] [CrossRef]
- Carta, M.G.; Cossu, G.; Pintus, E.; Zoccheddu, R.; Callia, O.; Conti, G.; Pintus, M.; Gonzalez, C.; Massidda, M.V.; Mura, G.; et al. Active elderly and health-can moderate exercise improve health and wellbeing in older adults? Protocol for a randomized controlled trial. Trials 2021, 22, 331. [Google Scholar] [CrossRef]
- Carta, M.G.; Cossu, G.; Pintus, E.; Zaccheddu, R.; Callia, O.; Conti, G.; Pintus, M.; Aviles Gonzalez, C.I.; Massidda, M.V.; Mura, G.; et al. Moderate Exercise Improves Cognitive Function in Healthy Elderly People: Results of a Randomized Controlled Trial. Clin. Pract. Epidemiol. Ment. Health CP EMH 2021, 17, 75–80. [Google Scholar] [CrossRef]
- Young, J.; Angevaren, M.; Rusted, J.; Tabet, N. Aerobic exercise to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst. Rev. 2015, 4, CD005381. [Google Scholar] [CrossRef]
- Wykes, T.; Spaulding, W.D. Thinking about the future cognitive remediation therapy—What works and could we do better? Schizophr. Bull. 2011, 37 (Suppl. 2), S80–S90. [Google Scholar] [CrossRef]
- Elgamal, S.; McKinnon, M.C.; Ramakrishnan, K.; Joffe, R.T.; MacQueen, G. Successful computer-assisted cognitive remediation therapy in patients with unipolar depression: A proof of principle study. Psychol. Med. 2007, 37, 1229–1238. [Google Scholar] [CrossRef] [PubMed]
- Bellani, M.; Biagianti, B.; Zovetti, N.; Rossetti, M.G.; Bressi, C.; Perlini, C.; Brambilla, P. The effects of cognitive remediation on cognitive abilities and real-world functioning among people with bipolar disorder: A systematic review: Special Section on “Translational and Neuroscience Studies in Affective Disorders”. Section Editor, Maria Nobile MD, PhD. This Section of JAD focuses on the relevance of translational and neuroscience studies in providing a better understanding of the neural basis of affective disorders. The main aim is to briefly summaries relevant research findings in clinical neuroscience with particular regards to specific innovative topics in mood and anxiety disorders. J. Affect. Disord. 2019, 257, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Medalia, A. Factors associated with a positive response to cognitive remediation in a community psychiatric sample. Psychiatr. Serv. 2005, 56, 602–604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cella, M.; Preti, A.; Edwards, C.; Dow, T.; Wykes, T. Cognitive remediation for negative symptoms of schizophrenia: A network meta-analysis. Clin. Psychol. Rev. 2017, 52, 43–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grynszpan, O.; Perbal, S.; Pelissolo, A.; Fossati, P.; Jouvent, R.; Dubal, S.; Perez-Diaz, F. Efficacy and specificity of computer-assisted cognitive remediation in schizophrenia: A meta-analytical study. Psychol. Med. 2011, 41, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Alves, J.; Magalhães, R.; Machado, A.; Gonçalves, O.F.; Sampaio, A.; Petrosyan, A. Non-pharmacological cognitive intervention for aging and dementia: Current perspectives. World J. Clin. Cases 2013, 1, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Rodakowski, J.; Saghafi, E.; Butters, M.A.; Skidmore, E.R. Non-pharmacological interventions for adults with mild cognitive impairment and early stage dementia: An updated scoping review. Mol. Asp. Med. 2015, 43–44, 38–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Velligan, D.I.; Kern, R.S.; Gold, J.M. Cognitive rehabilitation for schizophrenia and the putative role of motivation and expectancies. Schizophr. Bull. 2006, 32, 474–485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freeman, D.; Reeve, S.; Robinson, A.; Ehlers, A.; Clark, D.; Spanlang, B.; Slater, M. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol. Med. 2017, 47, 2393–2400. [Google Scholar] [CrossRef] [Green Version]
- Valmaggia, L.R.; Latif, L.; Kempton, M.J.; Rus-Calafell, M. Virtual reality in the psychological treatment for mental health problems: An systematic review of recent evidence. Psychiatry Res. 2016, 236, 189–195. [Google Scholar] [CrossRef]
- Mesa-Gresa, P.; Gil-Gómez, H.; Lozano-Quilis, J.A.; Gil-Gómez, J.A. Effectiveness of Virtual Reality for Children and Adolescents with Autism Spectrum Disorder: An Evidence-Based Systematic Review. Sensors 2018, 18, 2486. [Google Scholar] [CrossRef] [Green Version]
- Parsons, T.D.; Courtney, C.G.; Arizmendi, B.; Dawson, M. Virtual Reality Stroop Task for neurocognitive assessment. Stud. Health Technol. Inform. 2011, 163, 433–439. [Google Scholar] [PubMed]
- Seidel, R.J.; Chatelier, P.R. (Eds.) Virtual Reality, Training’s Future?: Perspectives on Virtual Reality and Related Emerging Technologies; Springer Science & Business Media: Berlin/Heidelberg, Germany, 1997; Volume 6. [Google Scholar]
- Slater, M. Presence and emotions. Cyberpsychology Behav. Impact Internet Multimed. Virtual Real. Behav. Soc. 2004, 7, 121–123. [Google Scholar] [CrossRef] [PubMed]
- Skivington, K.; Matthews, L.; Simpson, S.A.; Craig, P.; Baird, J.; Blazeby, J.M.; Boyd, K.A.; Craig, N.; French, D.P.; McIntosh, E.; et al. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. BMJ (Clin. Res. Ed.) 2021, 374, n2061. [Google Scholar] [CrossRef] [PubMed]
- Bird, M.L.; Cannell, J.; Jovic, E.; Rathjen, A.; Lane, K.; Tyson, A.; Callisaya, M.; Smith, S. A randomized controlled trial investigating the efficacy of virtual reality in inpatient stroke rehabilitation. Arch. Phys. Med. Rehabil. 2017, 98, e27. [Google Scholar] [CrossRef]
- Albiol-Pérez, S.; Gil-Gómez, J.A.; Muñoz-Tomás, M.T.; Gil-Gómez, H.; Vial-Escolano, R.; Lozano-Quilis, J.A. The Effect of Balance Training on Postural Control in Patients with Parkinson’s Disease Using a Virtual Rehabilitation System. Methods Inf. Med. 2017, 56, 138–144. [Google Scholar] [CrossRef] [Green Version]
- Riva, G.; Wiederhold, B.K.; Mantovani, F. Neuroscience of Virtual Reality: From Virtual Exposure to Embodied Medicine. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 82–96. [Google Scholar] [CrossRef]
- Adams, R.; Finn, P.; Moes, E.; Flannery, K.; Rizzo, A.S. Distractibility in Attention/Deficit/ Hyperactivity Disorder (ADHD): The virtual reality classroom. Child Neuropsychol. J. Norm. Abnorm. Dev. Child. Adolesc. 2009, 15, 120–135. [Google Scholar] [CrossRef]
- Elkind, J.S.; Rubin, E.; Rosenthal, S.; Skoff, B.; Prather, P. A simulated reality scenario compared with the computerized Wisconsin card sorting test: An analysis of preliminary results. Cyberpsychol. Behav. Impact Internet Multimed. Virtual Real. Behav. Soc. 2001, 4, 489–496. [Google Scholar] [CrossRef]
- Iriarte, Y.; Diaz-Orueta, U.; Cueto, E.; Irazustabarrena, P.; Banterla, F.; Climent, G. AULA-Advanced Virtual Reality Tool for the Assessment of Attention: Normative Study in Spain. J. Atten. Disord. 2016, 20, 542–568. [Google Scholar] [CrossRef]
- Liu, Y.; Tan, W.; Chen, C.; Liu, C.; Yang, J.; Zhang, Y. A Review of the Application of Virtual Reality Technology in the Diagnosis and Treatment of Cognitive Impairment. Front. Aging Neurosci. 2019, 11, 280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perra, A.; De Lorenzo, V.; Zaccheddu, R.; Locci, A.; Piludu, F.; Preti, A.; Di Natale, L.; Galetti, A.; Nardi, A.E.; Cossu, G.; et al. Cognitive Remediation Virtual Reality Tool a Recovery-Oriented Project for People with Bipolar Disorder: Protocol of a feasibility randomized clinical trial. Clin. Pract. Epidemiol. Ment. Health CP EMH 2022, 18. [Google Scholar] [CrossRef]
- Jahn, F.S.; Skovbye, M.; Obenhausen, K.; Jespersen, A.E.; Miskowiak, K.W. Cognitive training with fully immersive virtual reality in patients with neurological and psychiatric disorders: A systematic review of randomized controlled trials. Psychiatry Res. 2021, 300, 113928. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Mancuso, V.; Cavedoni, S.; Stramba-Badiale, C. Virtual reality in neurorehabilitation: A review of its effects on multiple cognitive domains. Expert Rev. Med. Devices 2020, 17, 1035–1061. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; McDonough, D.J.; Gao, Z. The Effectiveness of Virtual Reality Exercise on Individual’s Physiological, Psychological and Rehabilitative Outcomes: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 4133. [Google Scholar] [CrossRef] [PubMed]
- Sayma, M.; Tuijt, R.; Cooper, C.; Walters, K. Are We There Yet? Immersive Virtual Reality to Improve Cognitive Function in Dementia and Mild Cognitive Impairment. Gerontologist 2020, 60, e502–e512. [Google Scholar] [CrossRef]
- Rotenberg, M.; Anderson, K.K.; McKenzie, K. Social capital and psychosis: A scoping review. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 659–671. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (Clin. Res. Ed.) 2021, 372, n71. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMAScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467. [Google Scholar] [CrossRef]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 129 (25 Suppl. 2), S49–S73. [Google Scholar] [CrossRef] [Green Version]
- McGuinness, L.A. Robvis: An R Package and Web Application for Visualising Risk-of-Bias Assessments. 2019. Available online: https://github.com/mcguinlu/robvis (accessed on 30 September 2022).
- Morris, S.B. Estimating effect sizes from pretest-posttest-control group designs. Organ. Res. Methods 2008, 11, 364–386. [Google Scholar] [CrossRef]
- Hedges, L.V.; Olkin, I. Statistical Methods for Meta-Analysis; Academic Press: Cambridge, MA, USA, 2014. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Cooper, H.M.; Hedges, L.V.; Valentine, J.C. The Handbook of Research Synthesis and Meta-Analysis, 2nd ed.; Russell Sage Foundation: New York, NY, USA, 2009. [Google Scholar]
- Huedo-Medina, T.B.; Sánchez-Meca, J.; Marín-Martínez, F.; Botella, J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol. Methods 2006, 11, 193–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ (Clin. Res. Ed.) 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin. Res. Ed.) 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Galbraith, R.F. Some applications of radial plots. J. Am. Stat. Assoc. 1994, 89, 1232–1242. [Google Scholar] [CrossRef]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 30 September 2022).
- Kim, H.; Hong, J.P.; Kang, J.M.; Kim, W.H.; Maeng, S.; Cho, S.E.; Na, K.S.; Oh, S.H.; Park, J.W.; Cho, S.J.; et al. Cognitive reserve and the effects of virtual reality-based cognitive training on elderly individuals with mild cognitive impairment and normal cognition. Psychogeriatr. Off. J. Jpn. Psychogeriatr. Soc. 2021, 21, 552–559. [Google Scholar] [CrossRef]
- Kang, J.M.; Kim, N.; Lee, S.Y.; Woo, S.K.; Park, G.; Yeon, B.K.; Park, J.W.; Youn, J.H.; Ryu, S.H.; Lee, J.Y.; et al. Effect of Cognitive Training in Fully Immersive Virtual Reality on Visuospatial Function and Frontal-Occipital Functional Connectivity in Predementia: Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e24526. [Google Scholar] [CrossRef]
- Maeng, S.; Hong, J.P.; Kim, W.H.; Kim, H.; Cho, S.E.; Kang, J.M.; Na, K.S.; Oh, S.H.; Park, J.W.; Bae, J.N.; et al. Effects of Virtual Reality-Based Cognitive Training in the Elderly with and without Mild Cognitive Impairment. Psychiatry Investig. 2021, 18, 619–627. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.Y.; Chen, I.H.; Lin, Y.J.; Chen, Y.; Hsu, W.C. Effects of Virtual Reality-Based Physical and Cognitive Training on Executive Function and Dual-Task Gait Performance in Older Adults with Mild Cognitive Impairment: A Randomized Control Trial. Front. Aging Neurosci. 2019, 11, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thapa, N.; Park, H.J.; Yang, J.G.; Son, H.; Jang, M.; Lee, J.; Kang, S.W.; Park, K.W.; Park, H. The Effect of a Virtual Reality-Based Intervention Program on Cognition in Older Adults with Mild Cognitive Impairment: A Randomized Control Trial. J. Clin. Med. 2020, 9, 1283. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.Y.; Tseng, H.Y.; Lin, Y.J.; Wang, C.J.; Hsu, W.C. Using virtual reality-based training to improve cognitive function, instrumental activities of daily living and neural efficiency in older adults with mild cognitive impairment. Eur. J. Phys. Rehabil. Med. 2020, 56, 47–57. [Google Scholar] [CrossRef]
- Hwang, J.; Lee, S. The effect of virtual reality program on the cognitive function and balance of the people with mild cognitive impairment. J. Phys. Ther. Sci. 2017, 29, 1283–1286. [Google Scholar] [CrossRef] [Green Version]
- Kwan, R.; Liu, J.; Fong, K.; Qin, J.; Leung, P.K.; Sin, O.; Hon, P.Y.; Suen, L.W.; Tse, M.K.; Lai, C.K. Feasibility and Effects of Virtual Reality Motor-Cognitive Training in Community-Dwelling Older People with Cognitive Frailty: Pilot Randomized Controlled Trial. JMIR Serious Games 2021, 9, e28400. [Google Scholar] [CrossRef]
- Park, J.H.; Liao, Y.; Kim, D.R.; Song, S.; Lim, J.H.; Park, H.; Lee, Y.; Park, K.W. Feasibility and Tolerability of a Culture-Based Virtual Reality (VR) Training Program in Patients with Mild Cognitive Impairment: A Randomized Controlled Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 3030. [Google Scholar] [CrossRef]
- Zając-Lamparska, L.; Wiłkość-Dębczyńska, M.; Wojciechowski, A.; Podhorecka, M.; Polak-Szabela, A.; Warchoł, Ł.; Kędziora-Kornatowska, K.; Araszkiewicz, A.; Izdebski, P. Effects of virtual reality-based cognitive training in older adults living without and with mild dementia: A pretest-posttest design pilot study. BMC Res. Notes 2019, 12, 776. [Google Scholar] [CrossRef]
- La Paglia, F.; La Cascia, C.; Rizzo, R.; Sanna, M.; Cangialosi, F.; Sideli, L.; Francomano, A.; Riva, G.; La Barbera, D. Virtual reality environments to rehabilitation attention deficits in schizophrenic patients. Annu. Reviwe Cyber Ther. Telemed. 2016, 14, 143–148. [Google Scholar]
- Tulliani, N.; Bissett, M.; Fahey, P.; Bye, R.; Liu, K.P.Y. Efficacy of cognitive remediation on activities of daily living in individuals with mild cognitive impairment or early-stage dementia: A systematic review and meta-analysis. Syst. Rev. 2022, 11, 156. [Google Scholar] [CrossRef]
- Simon, S.S.; Yokomizo, J.E.; Bottino, C.M. Cognitive intervention in amnestic Mild Cognitive Impairment: A systematic review. Neurosci. Biobehav. Rev. 2012, 36, 1163–1178. [Google Scholar] [CrossRef] [PubMed]
- Petrigna, L.; Musumeci, G. The Metaverse: A New Challenge for the Healthcare System: A Scoping Review. J. Funct. Morphol. Kinesiol. 2022, 7, 63. [Google Scholar] [CrossRef] [PubMed]

| Database searched | Pubmed | |
| Embase | ||
| Cochrane | ||
| Limits | Language: English only. | |
| Years: last 12 years (2022–2010) | ||
| Geographic: no limits | ||
| PICOS | Population | People (adult, any gender) with psychosocial disabilities, specifically all the psychiatric diagnosis such as anxiety, psychotic, mood disorder, bipolar disorder etc. and neurocognitive disease such as mild cognitive impairment/Alzheimer’s disease and dementia |
| Intervention | Studies that used cognitive remediation program in fully immersive virtual reality | |
| Comparison | No restrictions | |
| Outcome | Cognitive and clinical effectiveness, methods used | |
| Study Type | Only randomized clinical trials | |
| Exclusion | Duplicates, not randomized clinical trials, articles not in English or not available, not cognitive remediation in fully immersive virtual reality program and not adult population with mental diseases | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perra, A.; Riccardo, C.L.; De Lorenzo, V.; De Marco, E.; Di Natale, L.; Kurotschka, P.K.; Preti, A.; Carta, M.G. Fully Immersive Virtual Reality-Based Cognitive Remediation for Adults with Psychosocial Disabilities: A Systematic Scoping Review of Methods Intervention Gaps and Meta-Analysis of Published Effectiveness Studies. Int. J. Environ. Res. Public Health 2023, 20, 1527. https://doi.org/10.3390/ijerph20021527
Perra A, Riccardo CL, De Lorenzo V, De Marco E, Di Natale L, Kurotschka PK, Preti A, Carta MG. Fully Immersive Virtual Reality-Based Cognitive Remediation for Adults with Psychosocial Disabilities: A Systematic Scoping Review of Methods Intervention Gaps and Meta-Analysis of Published Effectiveness Studies. International Journal of Environmental Research and Public Health. 2023; 20(2):1527. https://doi.org/10.3390/ijerph20021527
Chicago/Turabian StylePerra, Alessandra, Chiara Laura Riccardo, Valerio De Lorenzo, Erika De Marco, Lorenzo Di Natale, Peter Konstantin Kurotschka, Antonio Preti, and Mauro Giovanni Carta. 2023. "Fully Immersive Virtual Reality-Based Cognitive Remediation for Adults with Psychosocial Disabilities: A Systematic Scoping Review of Methods Intervention Gaps and Meta-Analysis of Published Effectiveness Studies" International Journal of Environmental Research and Public Health 20, no. 2: 1527. https://doi.org/10.3390/ijerph20021527





