Development and Characterization of a Semi-Solid Dosage Form of Meglumine Antimoniate for Topical Treatment of Cutaneous Leishmaniasis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of the Gel
2.3. Physicochemical Characterization of the MA Gel
2.3.1. Morphological Analysis
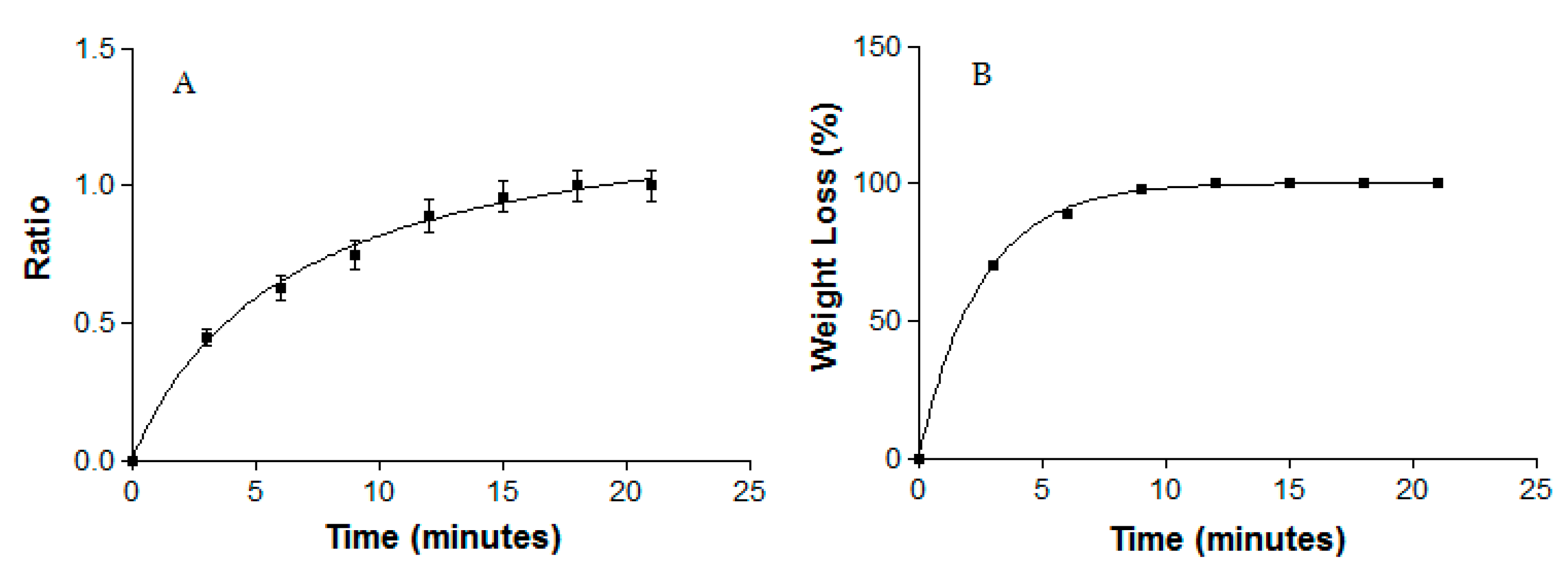
2.3.2. Swelling and Degradation Tests
2.3.3. Water Loss Due to Drying
2.3.4. Porosity Study
2.4. Stability Studies
2.5. Rheological Studies
2.6. Spreadability Test
2.7. In Vitro Release Studies
2.8. Ex Vivo Permeation Studies
2.9. In Vivo Tolerance Study
2.10. Parasite Strains and Cultures
2.11. In Vitro Cytotoxicity Assay
2.12. In Vitro Anti-Leishmanial Activity against Promastigotes
2.13. In Vitro Anti-Leishmanial Activity against Intracellular Amastigotes
2.14. Statistical Analysis
3. Results
3.1. Physicochemical Characterization of the MA Gel
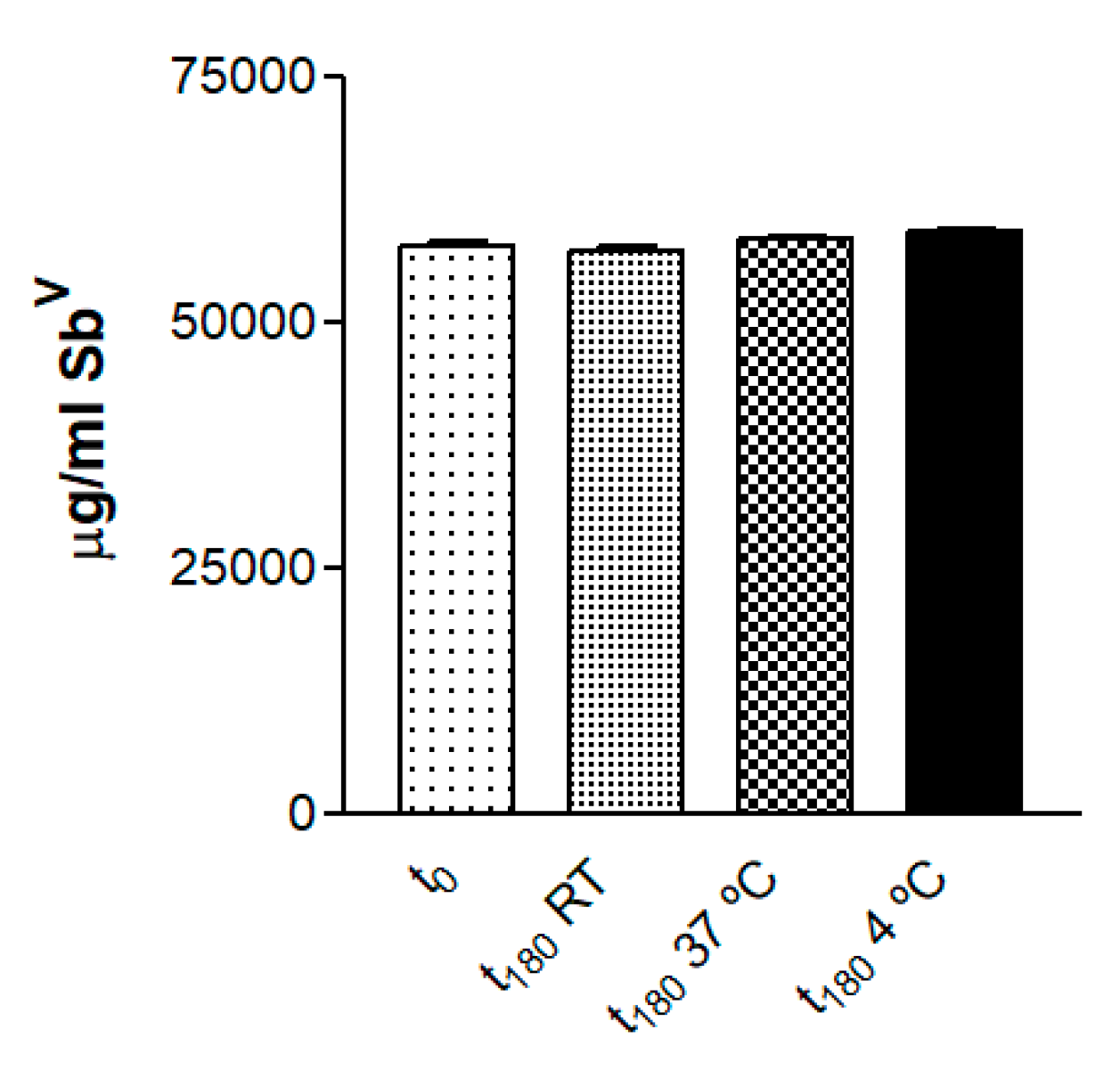
3.2. Drug Quantification and Stability Studies
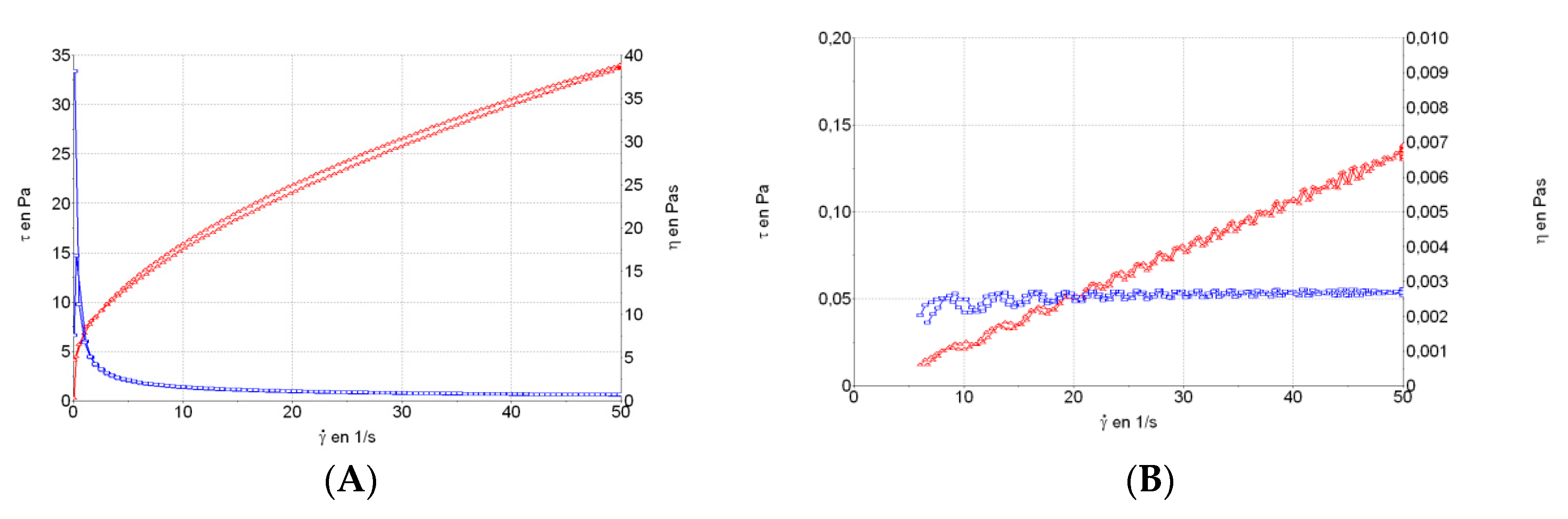
3.3. Rheological Studies
3.4. Spreadability Test
3.5. In Vitro Release Studies
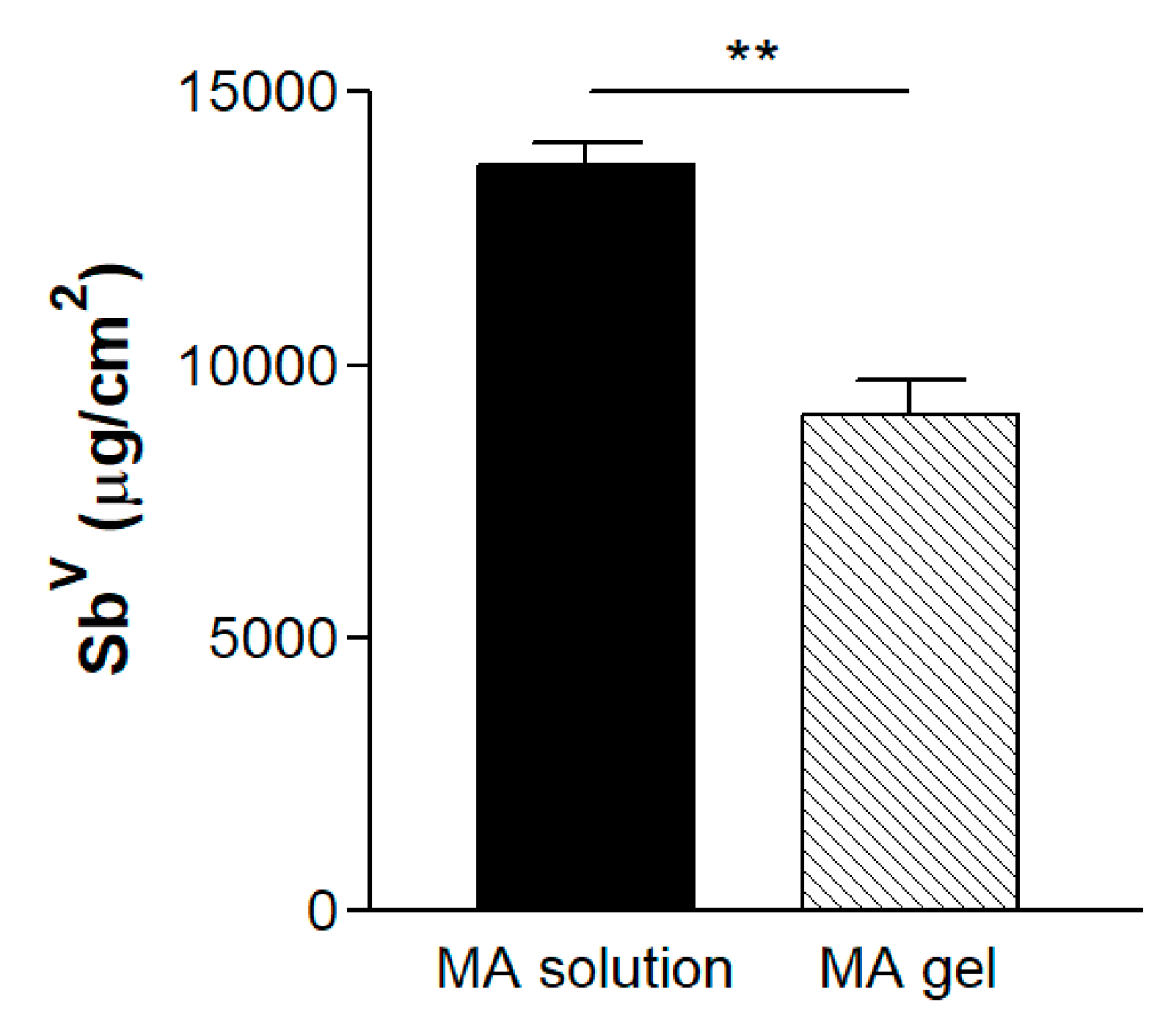
3.6. Ex Vivo Permeation Studies
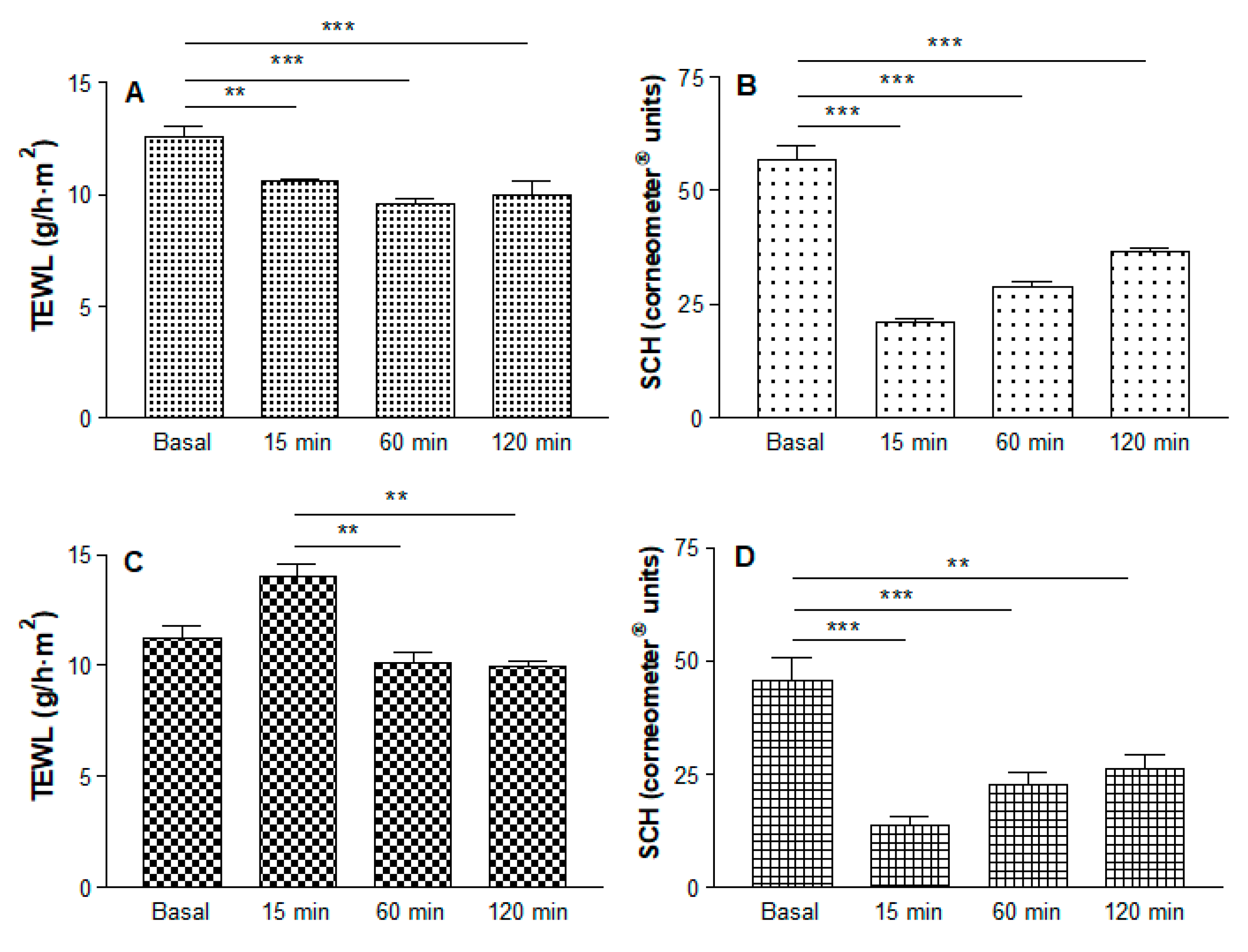
3.7. In Vivo Tolerance Study
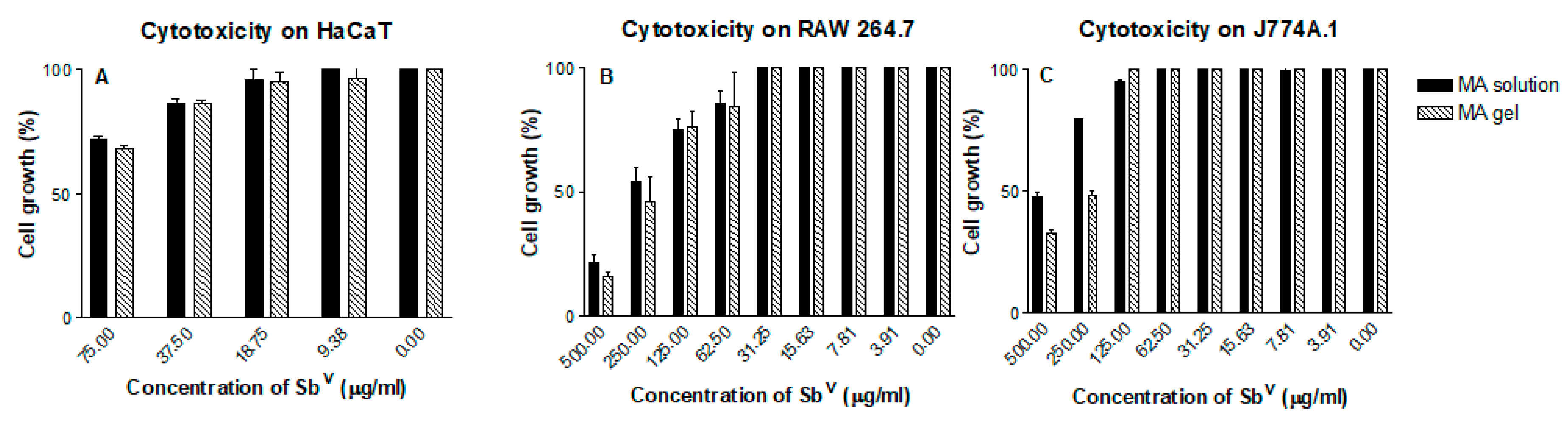
3.8. In Vitro Cytotoxicity Assay
3.9. Anti-Leishmanial In Vitro Activity against Promastigotes
3.10. Anti-Leishmanial In Vitro Activity against Intracellular Amastigotes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Weng, H.B.; Chen, H.X.; Wang, M.W. Innovation in neglected tropical disease drug discovery and development. Infect. Dis. Poverty 2018, 7, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Alvar, J.; Vélez, I.D.; Bern, C.; Herrero, M.; Desjeux, P.; Cano, J.; Janin, J.; den Boer, M.; WHO Leishmaniasis Control Team. Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE 2012, 7, e35671. [Google Scholar] [CrossRef] [PubMed]
- Alcover, M.M.; Rocamora, V.; Guillén, M.C.; Berenguer, D.; Cuadrado, M.; Riera, C.; Fisa, R. Case Report: Diffuse Cutaneous Leishmaniasis by Leishmania infantum in a Patient Undergoing Immunosuppressive Therapy: Risk Status in an Endemic Mediterranean Area. Am. J. Trop. Med. Hyg. 2018, 98, 1313–1316. [Google Scholar] [CrossRef] [PubMed]
- Rajni, E.; Ghiya, B.C.; Singh, S.; Shankar, P.; Swami, T.; Jadon, D.S.; Negi, S.R.; Malik, M.; Khatri, P.K. Cutaneous leishmaniasis in Bikaner, India: Clinicoepidemiological profile; parasite identification using conventional, molecular methods and CL DetectTM rapid test, a new Food and Drug Administration-approved test. Trop. Parasitol. 2019, 9, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Olliaro, P.; Vaillant, M.; Arana, B.; Grogl, M.; Modabber, F.; Magill, A.; Lapujade, O.; Buffet, P.; Alvar, J. Methodology of Clinical Trials Aimed at Assessing Interventions for Cutaneous Leishmaniasis. PLoS Negl. Trop. Dis. 2013, 7, e2130. [Google Scholar] [CrossRef] [PubMed]
- Jaafari, M.R.; Bavarsad, N.; Fazly-Bazzaz, B.S.; Samiei, A.; Soroush, D.; Ghorbani, S.; Lotfi-Heravi, M.M.; Khamesipour, A. Effect of Topical Liposomes Containing Paromomycin Sulfate in the Course of Leishmania major Infection in Susceptible BALB/c Mice. Antimicrob. Agents Chemother. 2009, 53, 2259–2265. [Google Scholar] [CrossRef]
- Royal Society of Chemistry. Available online: https://doi.org/10.1039/9781788010177-00001 (accessed on 9 October 2019).
- Trinconi, C.T.; Reimao, J.Q.; Bonano, V.I.; Espada, C.R.; Miguel, D.C.; Yokoyama-Yasunaka, J.K.U.; Uliana, S.R.B. Topical tamoxifen in the therapy of cutaneous leishmaniasis. Parasitology 2018, 145, 490–496. [Google Scholar] [CrossRef]
- Alexandrino-Junior, F.; Silva, K.G.H.E.; Freire, M.C.L.C.; Lione, V.O.F.; Cardoso, E.A.; Marcelina, H.R.; Genre, J.; Oliveira, A.G.; Egito, E.S.T.D. A Functional Wound Dressing as a Potential Treatment for Cutaneous Leishmaniasis. Pharmaceutics 2019, 11, 200. [Google Scholar] [CrossRef]
- Garnier, T.; Croft, S.L. Topical treatment for cutaneous leishmaniasis. Curr. Opin. Investig. Drugs 2002, 3, 538–544. [Google Scholar]
- Zur, E. Topical Treatment of Cutaneous Leishmaniasis in Israel, Part 1. Int. J. Pharm. Compd. 2019, 23, 200–207. [Google Scholar]
- El-On, J.; Livshin, R.; Even-Paz, Z.; Hamburger, D.; Weinrauch, L. Topical treatment of cutaneous leishmaniasis. J. Investig. Dermatol. 1986, 87, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Ben Salah, A.; Ben Messaoud, N.; Guedri, E.; Zaatour, A.; Ben Alaya, N.; Bettaieb, J.; Gharbi, A.; Belhadj Hamida, N.; Boukthir, A.; Chlif, S.; et al. Topical paromomycin with or without gentamicin for cutaneous leishmaniasis. N. Engl. J. Med. 2013, 368, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Sosa, N.; Pascale, J.M.; Jiménez, A.I.; Norwood, J.A.; Kreishman-Detrick, M.; Weina, P.J.; Lawrence, K.; McCarthy, W.F.; Adams, R.C.; Scott, C.; et al. Topical paromomycin for New World cutaneous leishmaniasis. PLoS Negl. Trop. Dis. 2019, 13, e0007253. [Google Scholar] [CrossRef] [PubMed]
- Soto, J.; Fuya, P.; Herrera, R.; Berman, J. Topical paromomycin/methylbenzethonium chloride plus parenteral meglumine antimoniate as treatment for American cutaneous leishmaniasis: Controlled study. Clin. Infect. Dis. 1998, 26, 56–58. [Google Scholar] [CrossRef]
- Carneiro, G.; Santos, D.C.; Oliveira, M.C.; Fernandes, A.P.; Ferreira, L.S.; Ramaldes, G.A.; Nunan, E.A.; Ferreira, L.A. Topical delivery and in vivo antileishmanial activity of paromomycin-loaded liposomes for treatment of cutaneous leishmaniasis. J. Liposome Res. 2010, 20, 16–23. [Google Scholar] [CrossRef]
- Brugués, A.P.; Naveros, B.C.; Calpena Campmany, A.C.; Pastor, P.H.; Saladrigas, R.F.; Lizandra, C.R. Developing cutaneous applications of paromomycin entrapped in stimuli-sensitive block copolymer nanogel dispersions. Nanomedicine (Lond.) 2015, 10, 227–240. [Google Scholar] [CrossRef]
- Frankenburg, S.; Glick, D.; Klaus, S.; Barenholz, Y. Efficacious topical treatment for murine cutaneous leishmaniasis with ethanolic formulations of amphoteicin B. Antimicrob. Agents Chemother. 1998, 42, 3092–3096. [Google Scholar] [CrossRef]
- López, L.; Vélez, I.; Asela, C.; Cruz, C.; Alves, F.; Robledo, S.; Arana, B. A phase II study to evaluate the safety and efficacy of topical 3% amphotericin B cream (Anfoleish) for the treatment of uncomplicated cutaneous leishmaniasis in Colombia. PLoS Negl. Trop. Dis. 2018, 12, e0006653. [Google Scholar] [CrossRef]
- Schmidt-Ott, R.; Klenner, T.; Overath, P.; Aebischer, T. Topical treatment with hexadecylphosphocholine (Miltex) efficiently reduces parasite burden in experimental cutaneous leishmaniasis. Trans. R. Soc. Trop. Med. Hyg. 1999, 93, 85–90. [Google Scholar] [CrossRef]
- Dar, M.J.; Din, F.U.; Khan, G.M. Sodium stibogluconate loaded nano-deformable liposomes for topical treatment of leishmaniasis: Macrophage as a target cell. Drug Deliv. 2018, 25, 1595–1606. [Google Scholar] [CrossRef]
- Moosavian Kalat, S.A.; Khamesipour, A.; Bavarsad, N.; Fallah, M.; Khashayarmanesh, Z.; Feizi, E.; Neghabi, K.; Abbasi, A.; Jaafari, M.R. Use of topical liposomes containing meglumine antimoniate (Glucantime) for the treatment of L. major lesion in BALB/c mice. Exp. Parasitol. 2014, 143, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Moosavian, S.A.; Fallah, M.; Jaafari, M.R. The activity of encapsulated meglumine antimoniate in stearylamine-bearing liposomes against cutaneous leishmaniasis in BALB/c mice. Exp. Parasitol. 2019, 200, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Anchisi, C.; Maccioni, A.M.; Sinico, C.; Valenti, D. Stability studies of new cosmetic formulations with vegetable extracts as functional agents. Farmaco 2001, 56, 427–431. [Google Scholar] [CrossRef]
- Bilia, A.R.; Bergonzi, M.C.; Mazzi, G.; Vincieri, F.F. Development and stability of semisolid preparations based on a supercritical CO2 Arnica extract. J. Pharm. Biomed. Anal. 2006, 41, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Risaliti, L.; Piazzini, V.; Di Marzo, M.G.; Brunetti, L.; Cecchi, R.; Lencioni, P.; Bilia, A.R.; Bergonzi, M.C. Topical formulations of delta-aminolevulinic acid for the treatment of actinic keratosis: Characterization and efficacy evaluation. Eur. J. Pharm. Sci. 2018, 115, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Suñer, J.; Calpena, A.C.; Clares, B.; Cañadas, C.; Halbaut, L. Development of Clotrimazole Multiple W/O/W Emulsions as Vehicles for Drug Delivery: Effects of Additives on Emulsion Stability. AAPS Pharm. Sci. Tech. 2017, 18, 539–550. [Google Scholar] [CrossRef]
- Council regulation (EC) no 440/2008 Test guideline for skin absorption: In vitro method (B45). J. Eur. Union 2008, 142, 438–443.
- World medical association declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [CrossRef]
- Du Plessis, J.; Stefaniak, A.; Eloff, F.; John, S.; Agner, T.; Chou, T.C.; Nixon, R.; Steiner, M.; Franken, A.; Kudla, I.; et al. International guidelines for the in vivo assessment of skin properties in non-clinical settings: Part 2. Transepidermal water loss and skin hydration. Skin. Res. Technol. 2013, 19, 265–278. [Google Scholar] [CrossRef]
- Pujol, A.; Urbán, P.; Riera, C.; Fisa, R.; Molina, I.; Salvador, F.; Estelrich, J.; Fernández-Busquets, X. Application of Quantum Dots to the Study of Liposome Targeting in Leishmaniasis and Malaria. Int. J. Theoret. Appiel. Nanotech. 2014, 2, 1–8. [Google Scholar] [CrossRef]
- Carrió, J.; de Colmenares, M.; Riera, C.; Gállego, M.; Arboix, M.; Portús, M. Leishmania infantum: Stage-specific activity of pentavalent antimony related with the assay conditions. Exp. Parasitol. 2000, 95, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Carrió, J.; Riera, C.; Gállego, M.; Portús, M. In vitro activity of pentavalent antimony derivates on promastigotes and intracellular amastigotes of Leishmania infantum strains from humans and dogs in Spain. Acta Trop. 2001, 79, 179–183. [Google Scholar] [CrossRef]
- Handler, M.Z.; Patel, P.A.; Kapila, R.; Al-Qubati, Y.; Schwarts, R.A. Cutaneous and mucocutaneous leishmaniasis: Differential diagnosis, diagnosis, histopathology, and management. J. Am. Acad Dermatol. 2015, 73, 911–926. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Liu, C.; Cun, D.; Fang, L. The effect of rheological behavior and microstructure of the emulgels on the release and permeation profiles of Terpinen-4-ol. Eur. J. Pharm. Sci. 2015, 78, 140–150. [Google Scholar] [CrossRef]
- Sosa, L.; Calpena, A.C.; Silva-Abreu, M.; Espinoza, L.C.; Rincón, M.; Bozal, N.; Domenech, O.; Rodríguez-Lagunas, M.J.; Clares, B. Thermoreversible Gel-Loaded Amphotericin B for the treatment of Dermal and Vaginal Candidiasis. Pharmaceutics 2019, 11, 312. [Google Scholar] [CrossRef] [Green Version]
- Kaur, L.; Jain, S.K.; Singh, K. Vitamin E TPGS based nanogel for the skin targeting of high molecular weight anti-fungal drug: Development and in vitro and in vivo assessment. RSC Adv. 2015, 5, 53671–53686. [Google Scholar] [CrossRef]
- Elias, P.M. Epidermal lipids, barrier function, and desquamation. J. Investig. Dermatol. 1983, 80, 44–49. [Google Scholar] [CrossRef]
- Marzulli, F.N.; Callahan, J.F.; Brown, D.W. Chemical structure and skin penetrating capacity of a short series of organic phosphates and phosphoric acid. J. Investig. Dermatol. 1965, 44, 339–344. [Google Scholar] [CrossRef] [Green Version]
- Anderson, B.D.; Raykar, P.V. Solute structure-permeability relationships in human stratum corneum. J. Investig. Dermatol. 1989, 93, 280–286. [Google Scholar] [CrossRef] [Green Version]
- Rins, M.; Diez, I.; Calpena, A.C.; Obach, R. Skin density in the hairless rat. Evidence of regional differences. Eur. J. Drug Metab. Pharmacokinet. 1991, 3, 456–457. [Google Scholar]




| Formulations | SbV (µg/mL) ± SD | |||
|---|---|---|---|---|
| t0 | t180 RT | t180 37 °C | t180 4 °C | |
| MA solution | 79,659.92 ± 1023.45 | |||
| MA gel | 57,936.62 ± 894.92 | 57,436.62 ± 854.92 | 58,575.93 ± 654.07 | 59,255.83 ± 524.49 |
| Assay | MA Solution | MA Gel | ||
|---|---|---|---|---|
| Non-Damaged Skin | Damaged Skin | Non-Damaged Skin | Damaged Skin | |
| Permeation (µg/cm2) ± SD | 2966.50 ± 562.37 | 121.00 ± 59.45 | 1217.53 ± 279.41 | 774.81 ± 179.63 |
| Retention in skin (µg/g/cm2) ± SD | 51,672.84 ± 8964.28 | 2057.47 ± 381.67 | 71,043.69 ± 10,641.57 | 10,728.23 ± 2254.61 |
| Formulations (µg/mL SbV) | IC50 (µg/mL SbV ± SD) | SI | CC50 (µg/mL SbV ± SD) | |||
|---|---|---|---|---|---|---|
| Promastigotes | Amastigotes | SIRAW | SIJ774 | RAW 264.7 | J774A.1 | |
| MA solution | >750 (* na) | 57.35 ± 2.76 | 6.66 | 6.37 | 381.76 ± 94.74 | 365.14 ± 165.26 |
| MA gel | 633.15 ± 43.26 (* na) | 15.76 ± 4.81 | 14.19 | 14.03 | 223.66 ± 46.82 | 221.05 ± 65.41 |
| Excipients | IC50 (µg/mL ± SD) | SI | CC50 (µg/mL ± SD) | |||
|---|---|---|---|---|---|---|
| Promastigotes | Amastigotes | SIRAW | SIJ774 | RAW 264.7 | J774A.1 | |
| Gelling agents (375–0.37 µg/mL) | >375 | 20.39 ± 5.43 | 6.57 | 6.13 | 134.00 ± 42.57 | 125.00 ± 20.80 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berenguer, D.; Sosa, L.; Alcover, M.; Sessa, M.; Halbaut, L.; Guillén, C.; Fisa, R.; Calpena-Campmany, A.C.; Riera, C. Development and Characterization of a Semi-Solid Dosage Form of Meglumine Antimoniate for Topical Treatment of Cutaneous Leishmaniasis. Pharmaceutics 2019, 11, 613. https://doi.org/10.3390/pharmaceutics11110613
Berenguer D, Sosa L, Alcover M, Sessa M, Halbaut L, Guillén C, Fisa R, Calpena-Campmany AC, Riera C. Development and Characterization of a Semi-Solid Dosage Form of Meglumine Antimoniate for Topical Treatment of Cutaneous Leishmaniasis. Pharmaceutics. 2019; 11(11):613. https://doi.org/10.3390/pharmaceutics11110613
Chicago/Turabian StyleBerenguer, Diana, Lilian Sosa, Magdalena Alcover, Marcella Sessa, Lyda Halbaut, Carme Guillén, Roser Fisa, Ana Cristina Calpena-Campmany, and Cristina Riera. 2019. "Development and Characterization of a Semi-Solid Dosage Form of Meglumine Antimoniate for Topical Treatment of Cutaneous Leishmaniasis" Pharmaceutics 11, no. 11: 613. https://doi.org/10.3390/pharmaceutics11110613






