Experimental Inoculation of Egyptian Rousette Bats (Rousettus aegyptiacus) with Viruses of the Ebolavirus and Marburgvirus Genera
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Biosafety
2.3. Animals and Husbandry
2.4. Viruses
2.5. Ebolavirus Pilot Study
2.6. Sudan Virus (Variant Gulu) Serial Euthanasia Study
2.7. Hematology and Clinical Chemistry
2.8. Necropsy
2.9. RNA Extraction and Q-RT-PCR
2.10. Histology and Immunohistochemistry
2.11. Serology
2.12. Statistical Analyses
3. Results
3.1. Ebolavirus Pilot Study
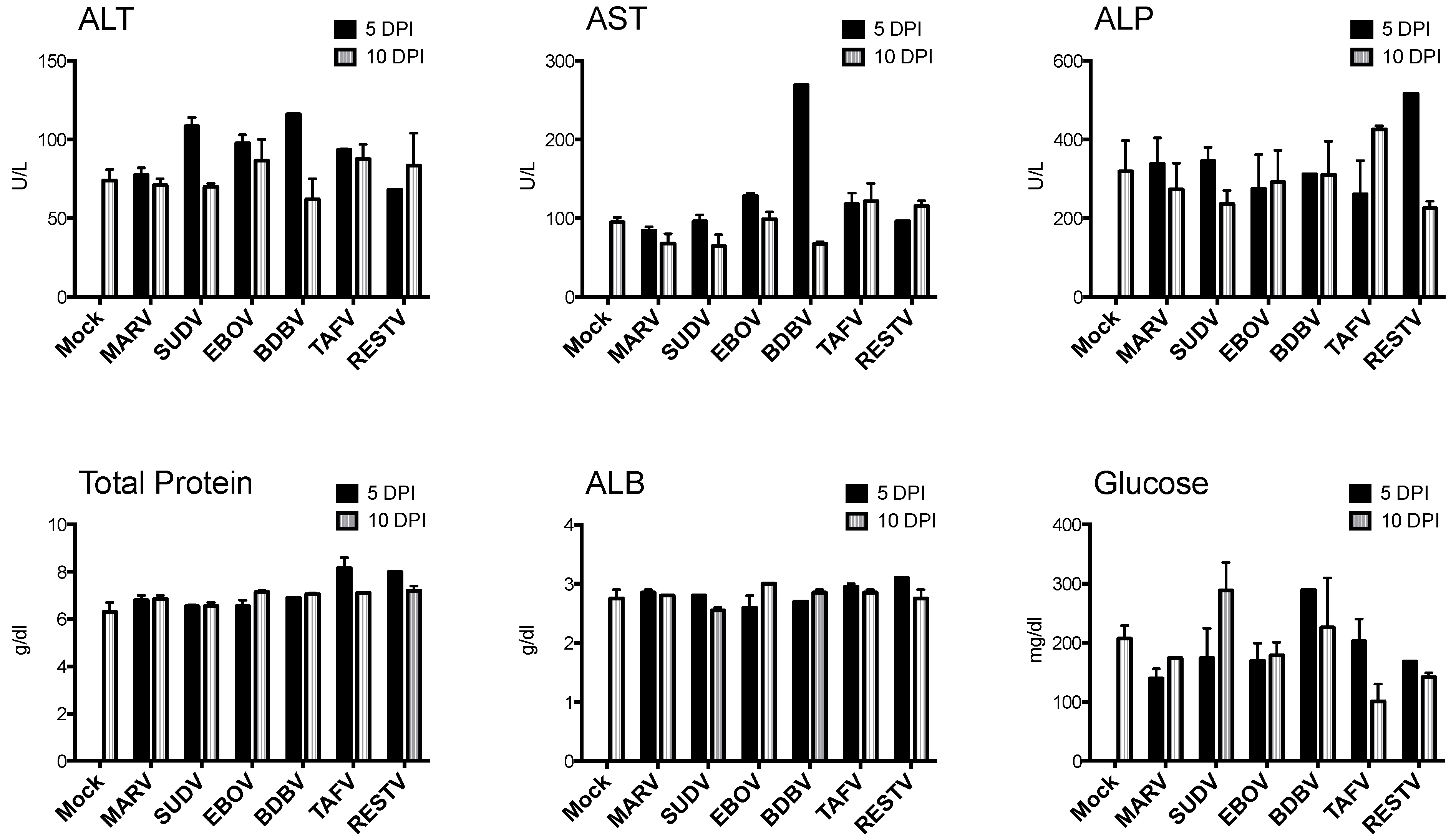
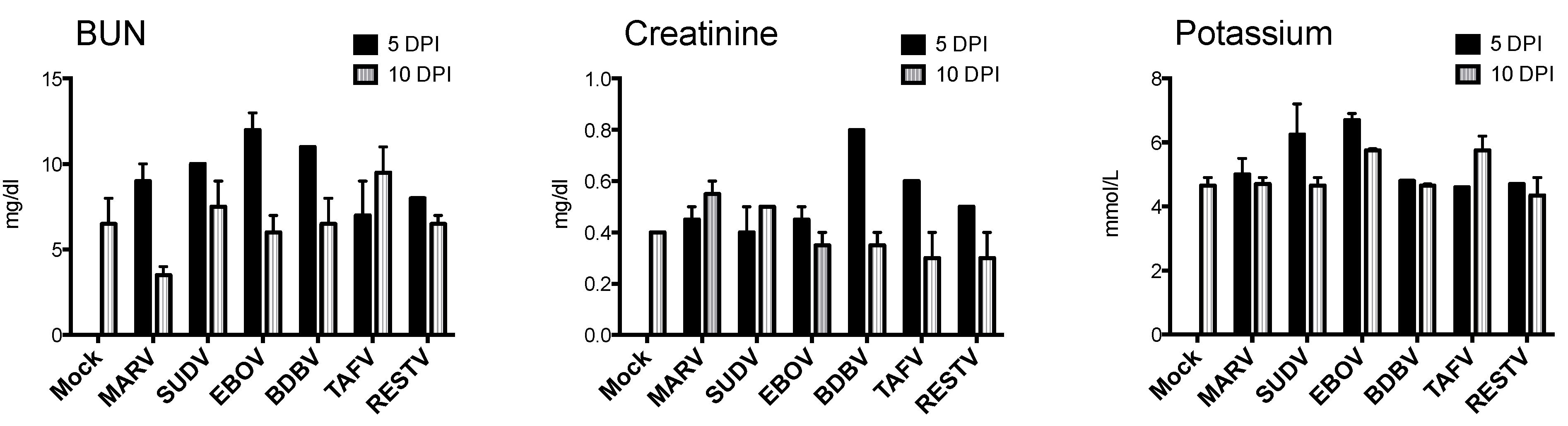
3.1.1. Clinical and Hematologic Findings
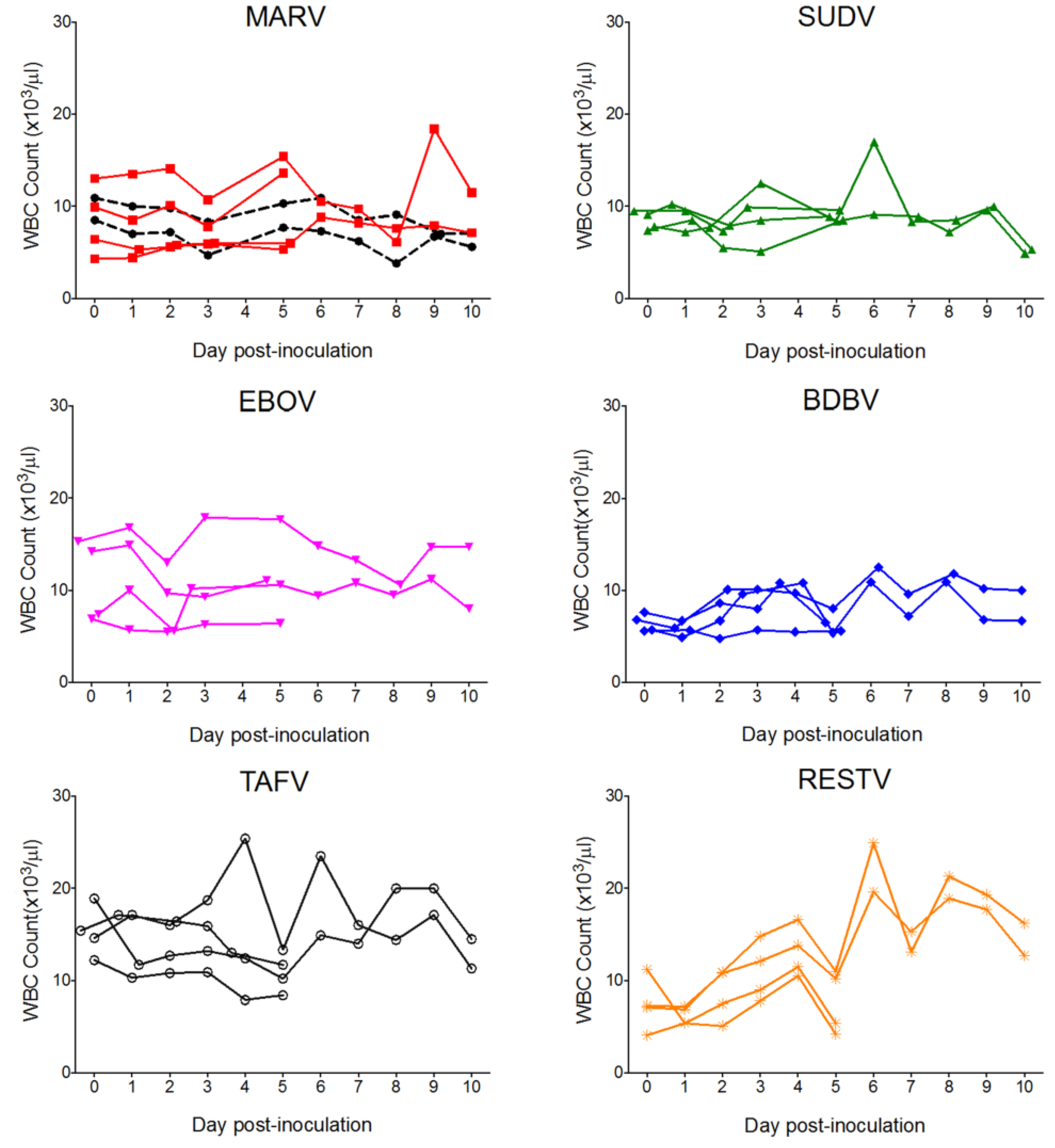
3.1.2. Q-RT-PCR
| Virus | DPI | Bat ID | Sex | Skin (Inoc) | Liv | Spl | Ax LN | Saliv G | UrBl | S Int | Mes LN | G | Hrt | Kid | Bld |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mock | 10 | 85334 | f | − | − | − | − | − | − | − | − | − | − | − | − |
| 91271 | m | − | − | − | − | − | − | − | − | − | − | − | − | ||
| MARV | 5 | 86433 | f | ++++ * | +++ * | +++ * | ++ | ++ | ++ | − | − | − | − | − | ++ |
| 50542 | m | ++++ * | ++++ * | +++ * | − | − | ++ | − | − | ++ | ++ | − | ++ | ||
| 10 | 91482 | f | ++++ * | ++ | − | − | ++ | − | ++ | − | − | − | +++ | - | |
| 91547 | m | +++ * | +++ | +++ | − | +++ | − | ++ | ++ | ++ | − | − | − | ||
| SUDV | 5 | 56380 | f | ++ * | + | + | + | − | − | − | − | − | − | − | − |
| 16107 | m | ++ | + | + | − | − | − | − | − | − | − | − | − | ||
| 10 | 43612 | f | + | − | − | + | − | + | − | − | − | − | − | − | |
| 20778 | m | − | − | − | + | − | − | − | − | − | − | − | − | ||
| EBOV | 5 | 85933 | f | ++ * | − | − | − | − | − | − | − | − | − | − | − |
| 52392 | m | − | − | − | − | − | − | − | − | − | − | − | − | ||
| 10 | 41902 | f | ++ | − | − | ++ | − | − | − | − | − | − | − | − | |
| 26060 | m | + | − | − | − | − | − | − | − | − | − | − | − | ||
| BDBV | 5 | 41354 | f | ++ | − | − | − | − | − | − | − | − | − | − | − |
| 91128 | m | ++ | − | − | − | − | − | − | − | − | − | − | − | ||
| 10 | 23796 | f | − | − | − | − | − | − | − | − | − | − | − | − | |
| 25844 | m | − | − | − | ++ | − | − | − | − | − | − | − | − | ||
| TAFV | 5 | 42084 | f | ++ | − | − | − | − | − | − | − | − | − | − | − |
| 35825 | m | +++ | − | − | − | − | − | − | − | − | − | − | − | ||
| 10 | 42348 | f | − | − | − | − | − | − | − | − | − | − | − | − | |
| 26015 | m | + | − | − | − | − | − | − | − | − | − | − | − | ||
| RESTV | 5 | 86551 | f | +++ * | − | − | − | − | − | − | − | − | − | − | − |
| 38558 | m | ++ | − | − | − | − | − | − | − | − | − | − | − | ||
| 10 | 50188 | f | ++ | − | − | − | − | − | − | − | − | − | − | − | |
| 45164 | m | − | − | − | ++ | − | − | − | − | − | − | − | − |
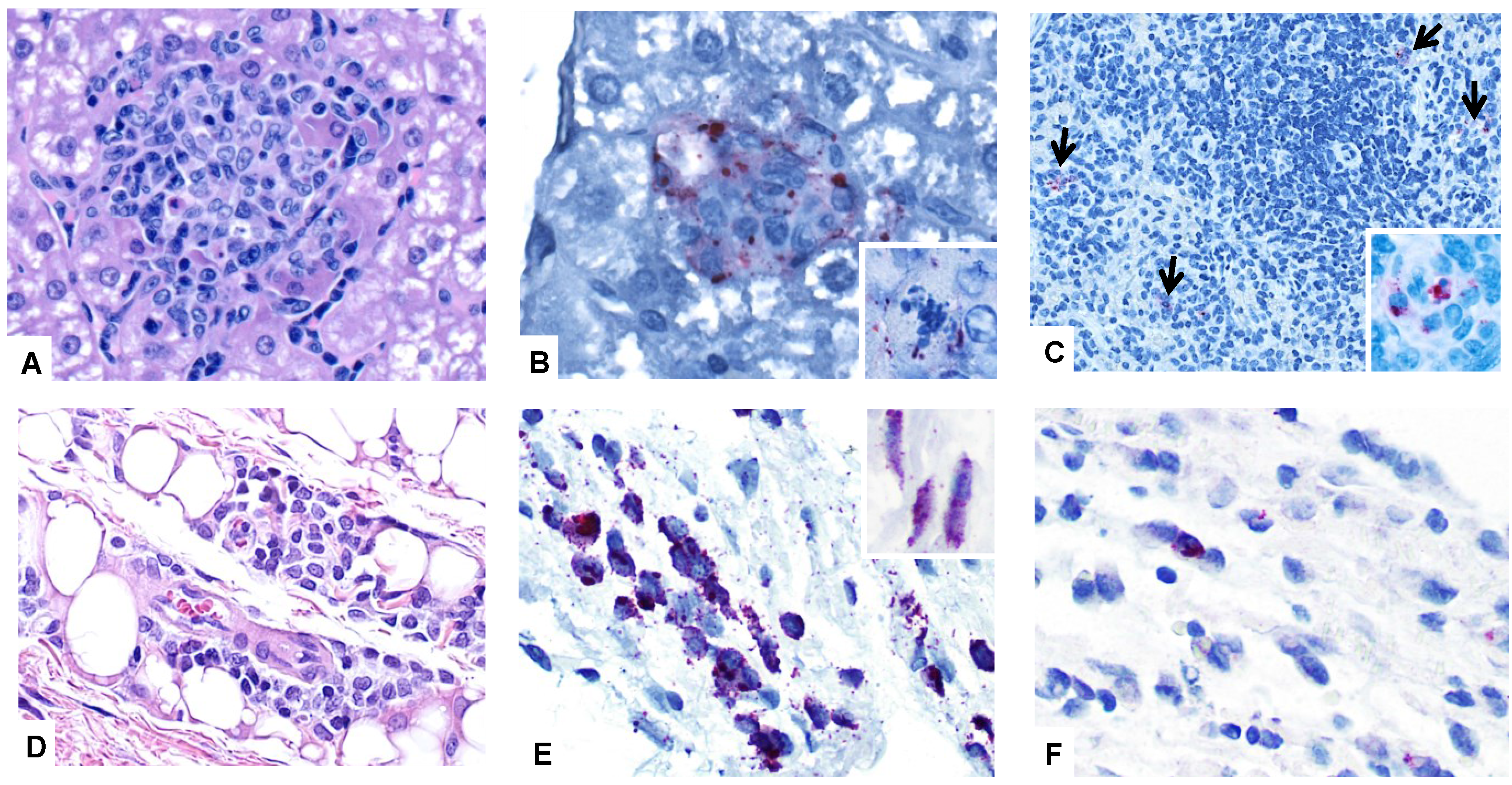
3.1.3. Necropsy, Histopathology, and Immunohistochemistry
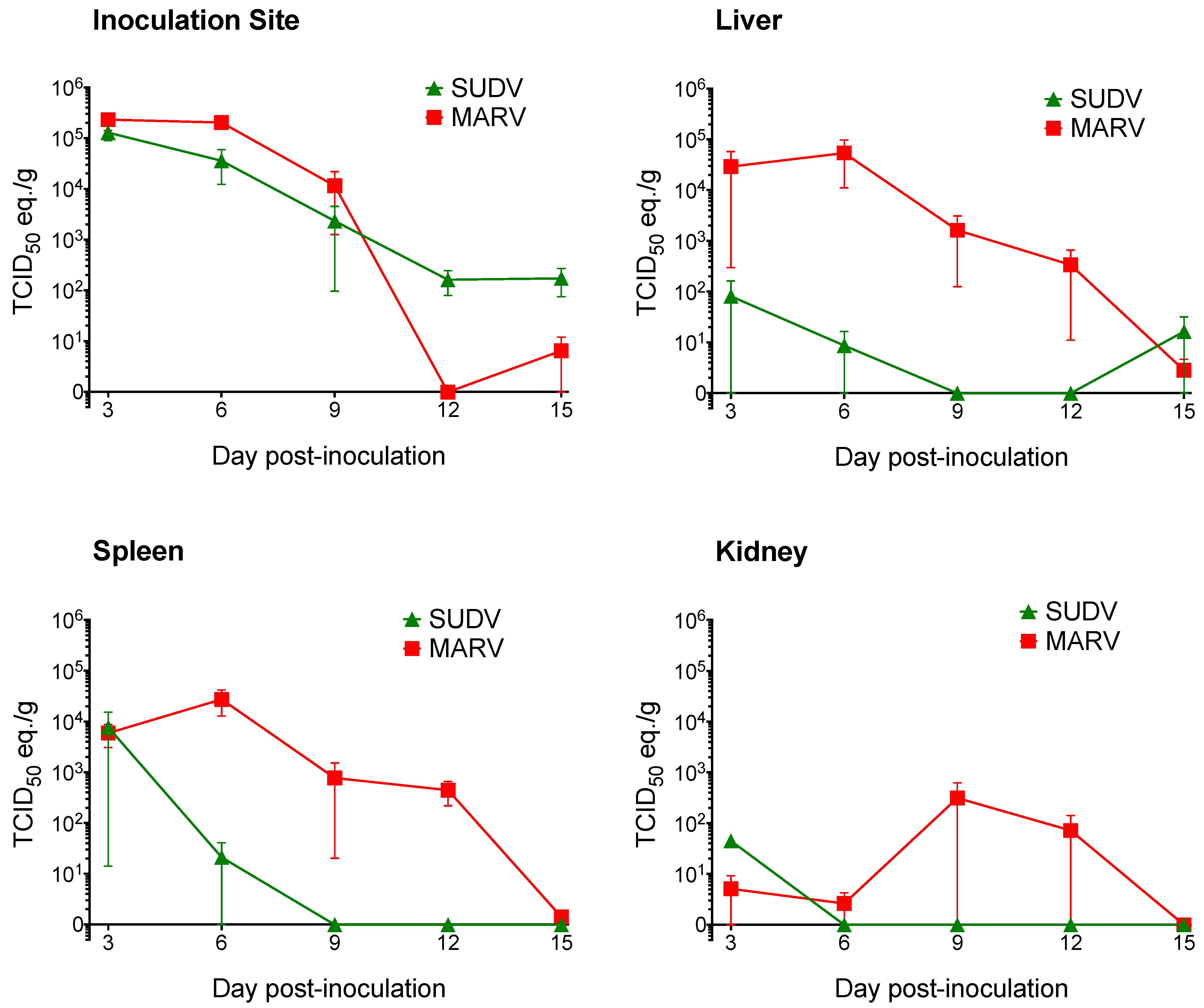
3.2. Sudan Virus Serial Euthanasia Study
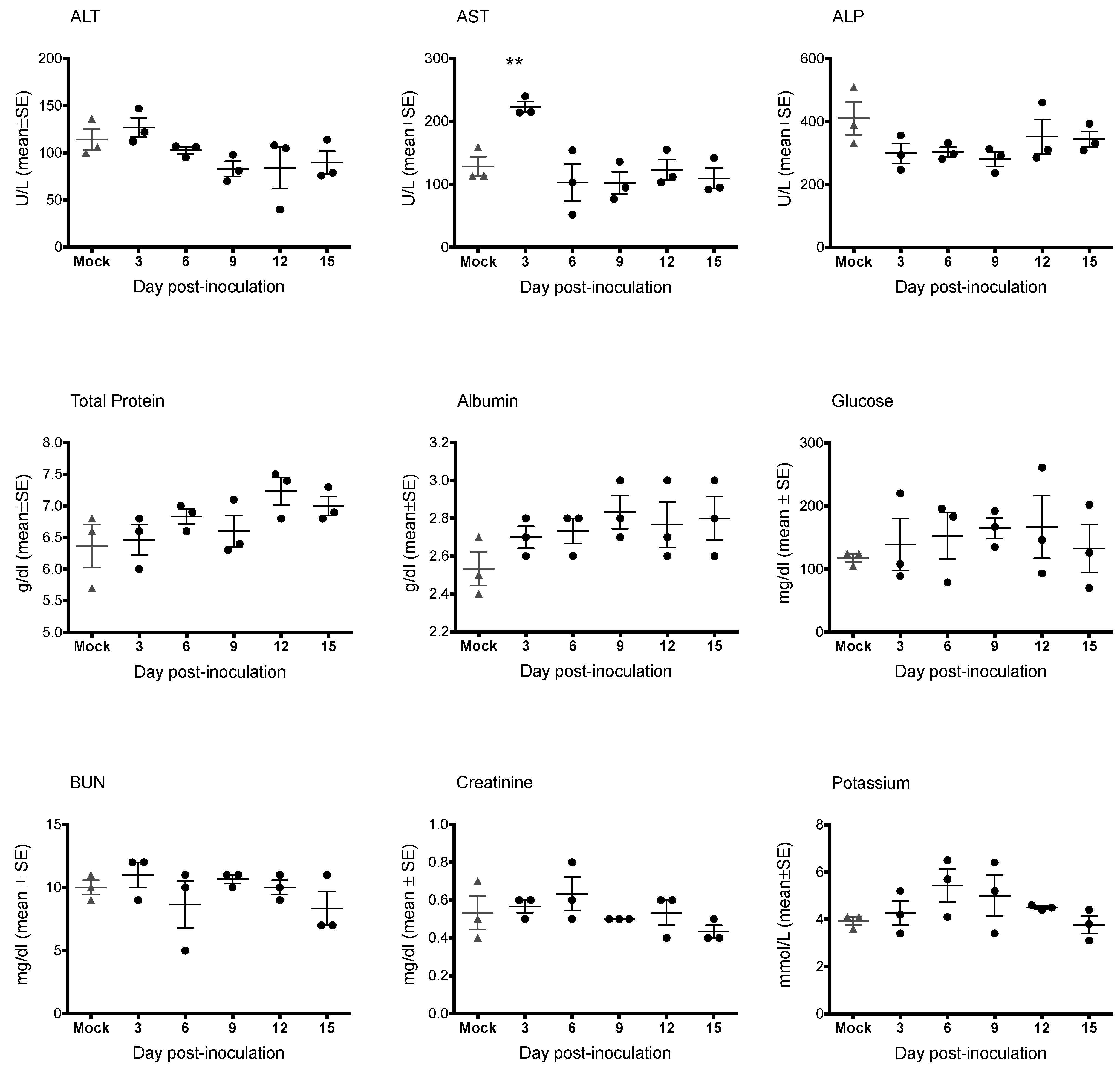
3.2.1. Clinical and Hematologic Findings

3.2.2. Q-RT-PCR
| Group | DPI | Bat ID | Skin (Inoc) | Liv | Spl | Ax LN | Ur Bl | S Int | Lg Int | G | Hrt | Kid |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SUDV | 3 | 546948 | ++++ * | − | + | ++ | + | + | ++ | ++ | − | − |
| 684640 | +++++ * | − | − | +++ | + | − | + | + | − | − | ||
| 720747 | ++++ * | ++ | ++++ | +++ * | − | − | + | + | − | − | ||
| 6 | 550595 | +++ | − | + | +++ | − | − | − | − | − | − | |
| 556705 | ++++ | − | − | ++ | + | + | ++ | − | − | − | ||
| 690641 | ++++ * | + | − | − | ++ | - | + | − | − | − | ||
| 9 | 725908 | +++ | − | − | − | − | − | − | − | − | − | |
| 845660 | ++ | − | − | − | − | − | − | − | − | − | ||
| 546543 | + | − | − | − | − | − | − | − | − | − | ||
| 12 | 721126 | ++ | − | − | +++ | − | − | − | − | − | − | |
| 724099 | + | − | − | − | − | − | − | − | − | − | ||
| 684978 | − | − | − | + | − | − | − | − | − | − | ||
| 15 | 642832 | ++ | − | − | − | − | − | − | − | − | − | |
| 721018 | ++ | − | − | − | − | − | − | − | − | − | ||
| 723995 | − | + | − | − | − | − | − | − | − | − | ||
| Mock | 15 | 214528 | − | − | − | − | − | − | − | − | − | − |
| 550277 | − | − | − | − | − | − | − | − | − | − | ||
| 684727 | − | − | − | − | − | − | − | − | − | − |
3.2.3. Necropsy, Histology, and Immunohistochemistry
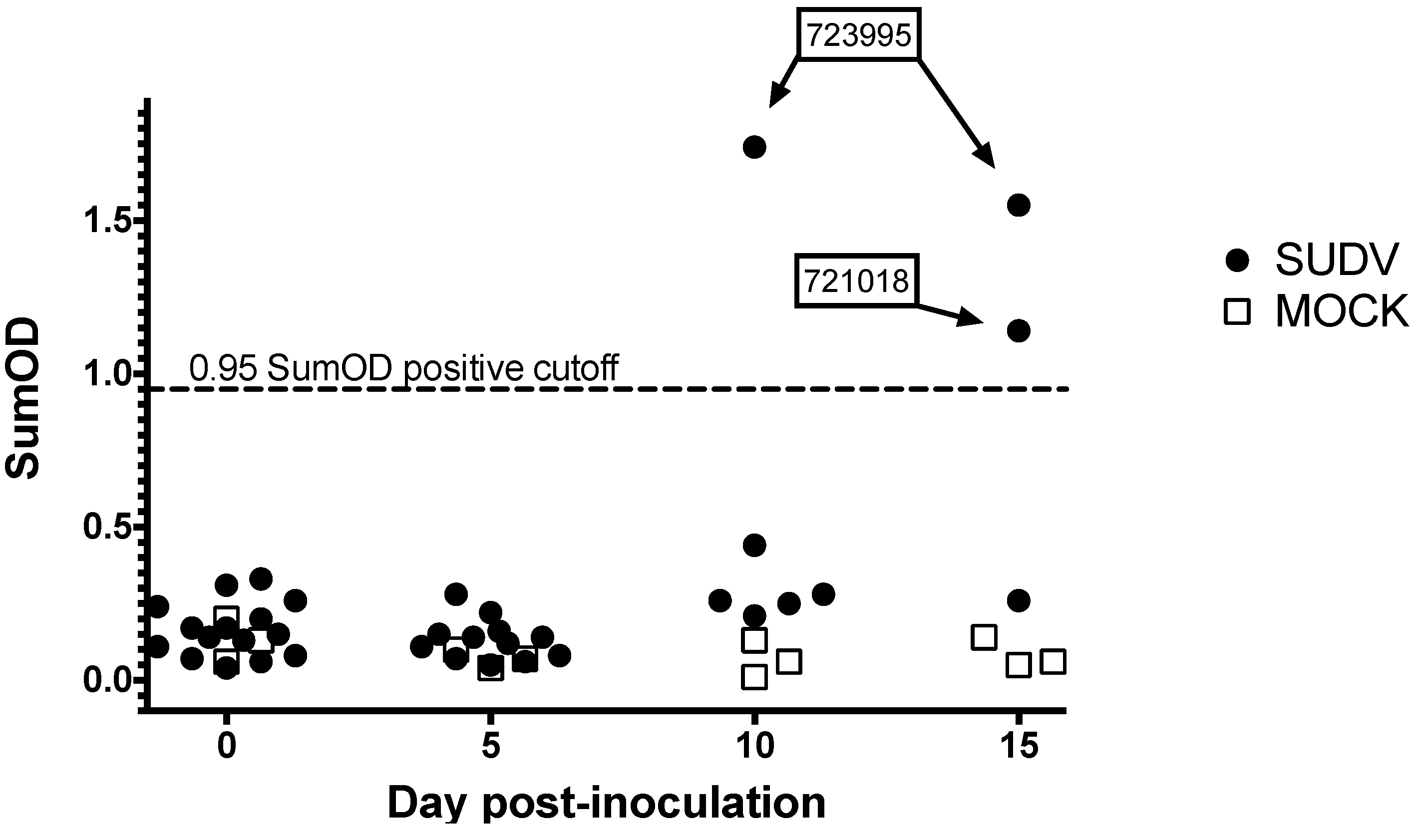
3.2.4. Serology
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Kuhn, J.H.; Becker, S.; Ebihara, H.; Geisbert, T.W.; Johnson, K.M.; Kawaoka, Y.; Lipkin, W.I.; Negredo, A.I.; Netesov, S.V.; Nichol, S.T.; et al. Proposal for a revised taxonomy of the family Filoviridae: Classification, names of taxa and viruses, and virus abbreviations. Arch. Virol. 2010, 155, 2083–2103. [Google Scholar] [CrossRef] [PubMed]
- Negredo, A.; Palacios, G.; Vázquez-Morón, S.; González, F.; Dopazo, H.; Molero, F.; Juste, J.; Quetglas, J.; Savji, N.; de la Cruz Martínez, M.; et al. Discovery of an ebolavirus-like filovirus in europe. PLoS Pathog. 2011, 7, e1002304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Towner, J.S.; Khristova, M.L.; Sealy, T.K.; Vincent, M.J.; Erickson, B.R.; Bawiec, D.A.; Hartman, A.L.; Comer, J.A.; Zaki, S.R.; Ströher, U.; et al. Marburgvirus genomics and association with a large hemorrhagic fever outbreak in Angola. J. Virol. 2006, 80, 6497–6516. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ebola haemorrhagic fever in Sudan, 1976. Bull. World Health Organ. 1978, 56, 247–270. [Google Scholar]
- Baron, R.C.; McCormick, J.B.; Zubeir, O.A. Ebola virus disease in southern Sudan: Hospital dissemination and intrafamilial spread. Bull. World Health Organ. 1983, 61, 997–1003. [Google Scholar] [PubMed]
- Towner, J.S.; Rollin, P.E.; Bausch, D.G.; Sanchez, A.; Crary, S.M.; Vincent, M.; Lee, F.; Spiropoulou, C.F.; Ksiazek, T.G.; Lukwiya, M.; et al. Rapid diagnosis of ebola hemorrhagic fever by reverse transcription-PCR in an outbreak setting and assessment of patient viral load as a predictor of outcome. J. Virol. 2004, 78, 4330–4341. [Google Scholar] [CrossRef] [PubMed]
- Towner, J.S.; Sealy, T.K.; Khristova, M.L.; Albariño, C.G.; Conlan, S.; Reeder, S.A.; Quan, P.-L.; Lipkin, W.I.; Downing, R.; Tappero, J.W.; et al. Newly discovered ebola virus associated with hemorrhagic fever outbreak in Uganda. PLoS Pathog. 2008, 4, e1000212. [Google Scholar] [CrossRef] [PubMed]
- MacNeil, A.; Farnon, E.C.; Wamala, J.; Okware, S.; Cannon, D.L.; Reed, Z.; Towner, J.S.; Tappero, J.W.; Lutwama, J.; Downing, R.; et al. Proportion of deaths and clinical features in Bundibugyo Ebola virus infection, Uganda. Emerg. Infect. Dis. 2010, 16, 1969–1972. [Google Scholar] [CrossRef] [PubMed]
- Albariño, C.G.; Shoemaker, T.; Khristova, M.L.; Wamala, J.F.; Muyembe, J.J.; Balinandi, S.; Tumusiime, A.; Campbell, S.; Cannon, D.; Gibbons, A.; et al. Genomic analysis of filoviruses associated with four viral hemorrhagic fever outbreaks in Uganda and the Democratic Republic of the Congo in 2012. Virology 2013, 442, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Siegert, R.; Shu, H.L.; Slenczka, H.L.; Peters, D.; Muller, G. The aetiology of an unknown human infection transmitted by monkeys (preliminary communication). Ger. Med. Mon. 1968, 13, 1–2. [Google Scholar] [PubMed]
- Pattyn, S.; Jacob, W.; ven der Groen, G.; Piot, P.; Courteille, G. Isolation of Marburg-like virus from a case of hemorrhagic fever in Zaire. Lancet 1977, 309, 573–574. [Google Scholar] [CrossRef]
- Johnson, K.M.; Lange, J.V.; Webb, P.A.; Murphy, F.A. Isolation and partial characterisation of a new virus causing acute haemorrhagic fever in Zaire. Lancet 1977, 1, 569–571. [Google Scholar] [CrossRef]
- Okware, S.I.; Omaswa, F.G.; Zaramba, S.; Opio, A.; Lutwama, J.J.; Kamugisha, J.; Rwaguma, E.B.; Kagwa, P.; Lamunu, M. An outbreak of Ebola in Uganda. Trop. Med. Int. Health 2002, 7, 1068–1075. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention 2014 Ebola Outbreak in West Africa—Case Counts. Available online: http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/case-counts.html (accessed on 4 April 2015).
- Formenty, P.; Boesch, C.; Wyers, M.; Steiner, C.; Donati, F.; Walker, F.; Guenno, B. Le ebola virus outbreak among wild chimpanzees living in a rain forest of Cote d’Ivoire. J. Infect. Dis. 1999, 179, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Formenty, P.; Hatz, C.; Le Guenno, B.; Stoll, A.; Rogenmoser, P.; Widmer, A. Human infection due to Ebola virus, subtype Côte d’Ivoire: Clinical and biologic presentation. J. Infect. Dis. 1999, 179, S48–S53. [Google Scholar] [CrossRef] [PubMed]
- Jahrling, P.B.; Geisbert, T.W.; Dalgard, D.W.; Johnson, E.D.; Ksiazek, T.G.; Hall, W.C.; Peters, C.J. Preliminary report: Isolation of Ebola virus from monkeys imported to USA. Lancet 1990, 335, 502–505. [Google Scholar] [CrossRef]
- Rollin, P.E.; Williams, R.J.; Bressler, D.S.; Pearson, S.; Cottingham, M.; Pucak, G.; Sanchez, A.; Trappier, S.G.; Peters, R.L.; Greer, P.W.; et al. Ebola (subtype Reston) virus among quarantined nonhuman primates recently imported from the Philippines to the United States. J. Infect. Dis. 1999, 179, S108–S114. [Google Scholar] [CrossRef] [PubMed]
- Miranda, M.E.G.; Yoshikawa, Y.; Manalo, D.L.; Calaor, A.B.; Miranda, N.L.J.; Cho, F.; Ikegami, T.; Ksiazek, T.G. Chronological and spatial analysis of the 1996 Ebola Reston virus outbreak in a monkey breeding facility in the Philippines. Exp. Anim. 2002, 51, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Miranda, M.E.; Ksiazek, T.G.; Retuya, T.J.; Khan, S.A.; Sanchez, A.; Fulhorst, C.F.; Rollin, P.E.; Calaor, A.B.; Manalo, D.L.; Roces, M.C.; et al. Epidemiology of Ebola (subtype Reston) virus in the Philippines, 1996. J. Infect. Dis. 1999, 179, S115–S119. [Google Scholar] [CrossRef] [PubMed]
- Barrette, R.W.; Metwally, S.A.; Rowland, J.M.; Xu, L.; Zaki, S.R.; Nichol, S.T.; Rollin, P.E.; Towner, J.S.; Shieh, W.-J.; Batten, B.; et al. Discovery of swine as a host for the Reston ebolavirus. Science 2009, 325, 204–206. [Google Scholar] [CrossRef] [PubMed]
- Towner, J.S.; Amman, B.R.; Sealy, T.K.; Carroll, S.A.R.; Comer, J.A.; Kemp, A.; Swanepoel, R.; Paddock, C.D.; Balinandi, S.; Khristova, M.L.; et al. Isolation of genetically diverse Marburg viruses from Egyptian fruit bats. PLoS Pathog. 2009, 5, e1000536. [Google Scholar] [CrossRef] [PubMed]
- Amman, B.R.; Carroll, S.A.; Reed, Z.D.; Sealy, T.K.; Balinandi, S.; Swanepoel, R.; Kemp, A.; Erickson, B.R.; Comer, J.A.; Campbell, S.; et al. Seasonal pulses of Marburg virus circulation in juvenile Rousettus aegyptiacus bats coincide with periods of increased risk of human infection. PLoS Pathog. 2012, 8, e1002877. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, R.; Smit, S.B.; Rollin, P.E.; Formenty, P.; Leman, P.A.; Kemp, A.; Burt, F.J.; Grobbelaar, A.A.; Croft, J.; Bausch, D.G.; et al. Studies of reservoir hosts for Marburg virus. Emerg. Infect. Dis. 2007, 13, 1847–1851. [Google Scholar] [CrossRef] [PubMed]
- Towner, J.S.; Pourrut, X.; Albariño, C.G.; Nkogue, C.N.; Bird, B.H.; Grard, G.; Ksiazek, T.G.; Gonzalez, J.P.; Nichol, S.T.; Leroy, E.M. Marburg virus infection detected in a common African bat. PLoS ONE 2007, 2, e764. [Google Scholar] [CrossRef] [PubMed]
- Amman, B.R.; Nyakarahuka, L.; McElroy, A.K.; Dodd, K.A.; Sealy, T.K.; Schuh, A.J.; Shoemaker, T.R.; Balinandi, S.; Atimnedi, P.; Kaboyo, W.; et al. Marburgvirus resurgence in Kitaka Mine bat population after extermination attempts, Uganda. Emerg. Infect. Dis. 2014, 20, 1761–1764. [Google Scholar] [CrossRef] [PubMed]
- Arata, A.; Johnson, B. Approaches towards studies on potential reservoirs of viral haemorrhagic fever in southern Sudan (1977). In Ebola Virus Haemorrhagic Fever; Pattyn, S., Ed.; Elsevier: New York, NY, USA, 1978; pp. 191–200. [Google Scholar]
- Leroy, E.M.; Kumulungui, B.; Pourrut, X.; Rouquet, P.; Hassanin, A.; Yaba, P.; Délicat, A.; Paweska, J.T.; Gonzalez, J.-P.; Swanepoel, R. Fruit bats as reservoirs of Ebola virus. Nature 2005, 438, 575–576. [Google Scholar] [CrossRef] [PubMed]
- Pourrut, X.; Souris, M.; Towner, J.S.; Rollin, P.E.; Nichol, S.T.; Gonzalez, J.-P.; Leroy, E. Large serological survey showing cocirculation of Ebola and Marburg viruses in Gabonese bat populations, and a high seroprevalence of both viruses in Rousettus aegyptiacus. BMC Infect. Dis. 2009, 9. [Google Scholar] [CrossRef] [PubMed]
- Pourrut, X.; Délicat, A.; Rollin, P.E.; Ksiazek, T.G.; Gonzalez, J.-P.; Leroy, E.M. Spatial and temporal patterns of Zaire ebolavirus antibody prevalence in the possible reservoir bat species. J. Infect. Dis. 2007, 196, S176–S183. [Google Scholar] [CrossRef] [PubMed]
- Hayman, D.T.S.; Emmerich, P.; Yu, M.; Wang, L.-F.; Suu-Ire, R.; Fooks, A.R.; Cunningham, A.A.; Wood, J.L.N. Long-term survival of an urban fruit bat seropositive for Ebola and Lagos bat viruses. PLoS ONE 2010, 5, e11978. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi, S.; Watanabe, S.; Masangkay, J.S.; Omatsu, T.; Ikegami, T.; Alviola, P.; Ueda, N.; Iha, K.; Fujii, H.; Ishii, Y.; et al. Reston Ebolavirus antibodies in bats, the Philippines. Emerg. Infect. Dis. 2011, 17, 1559–1560. [Google Scholar] [CrossRef] [PubMed]
- Olival, K.J.; Islam, A.; Yu, M.; Anthony, S.J.; Epstein, J.H.; Khan, S.A.; Khan, S.U.; Crameri, G.; Wang, L.; Lipkin, W.I.; et al. Ebola virus antibodies in fruit bats, Bangladesh. Emerg. Infect. Dis. 2013, 19, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.; Zhang, Y.; Li, J.; Zhang, Y.; Wang, L.-F.; Shi, Z. Serological evidence of ebolavirus infection in bats, China. Virol. J. 2012, 9, e236. [Google Scholar] [CrossRef] [PubMed]
- Paweska, J.T.; van Vuren, P.J.; Masumu, J.; Leman, P.A.; Grobbelaar, A.A.; Birkhead, M.; Clift, S.; Swanepoel, R.; Kemp, A. Virological and serological findings in Rousettus aegyptiacus experimentally inoculated with vero cells-adapted hogan strain of Marburg virus. PLoS ONE 2012, 7, e45479. [Google Scholar] [CrossRef] [PubMed]
- Amman, B.R.; Jones, M.E.B.; Sealy, T.K.; Uebelhoer, L.S.; Schuh, A.J.; Bird, B.H.; Coleman-Mccray, J.D.; Martin, B.E.; Nichol, S.T.; Towner, J.S. Oral shedding of marburg virus in experimentally infected egyptian fruit bats (Rousettus aegyptiacus). J. Wildl. Dis. 2015, 51, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, R.; Leman, P.A.; Burt, F.J.; Zachariades, N.A.; Braack, L.E.; Ksiazek, T.G.; Rollin, P.E.; Zaki, S.R.; Peters, C.J. Experimental inoculation of plants and animals with Ebola virus. Emerg. Infect. Dis. 1996, 2, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Saéz, A.M.; Weiss, S.; Nowak, K.; Lapeyre, V.; Kaba, M.; Regnaut, S.; Zimmermann, F.; Düx, A.; Ku, H.S.; Merkel, K.; et al. Investigating the zoonotic origin of the West African Ebola epidemic. EMBO Mol. Med. 2015, 7, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Krähling, V.; Dolnik, O.; Kolesnikova, L.; Schmidt-Chanasit, J.; Jordan, I.; Sandig, V.; Günther, S.; Becker, S. Establishment of fruit bat cells (Rousettus aegyptiacus) as a model system for the investigation of filoviral infection. PLoS Negl. Trop. Dis. 2010, 4, e802. [Google Scholar] [CrossRef] [PubMed]
- National Research Council. Guide for the Care and Use of Laboratory Animals, 8th ed.; National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Ksiazek, T.G.; Rollin, P.E.; Williams, A.J.; Bressler, D.S.; Martin, M.L.; Swanepoel, R.; Burt, F.J.; Leman, P.A.; Khan, A.S.; Rowe, A.K.; et al. Clinical virology of Ebola hemorrhagic fever (EHF): Virus, virus antigen, and IgG and IgM antibody findings among EHF patients in Kikwit, Democratic Republic of the Congo, 1995. J. Infect. Dis. 1999, 179, S177–S187. [Google Scholar] [CrossRef] [PubMed]
- Ksiazek, T.G.; West, C.P.; Rollin, P.E.; Jahrling, P.B.; Peters, C.J. ELISA for the detection of antibodies to Ebola viruses. J. Infect. Dis. 1999, 179, S192–S198. [Google Scholar] [CrossRef] [PubMed]
- Latimer, K.S.; Duncan, J.R. Duncan and Prasse’s Veterinary Laboratory Medicine: Clinical Pathology, 5th ed.; Wiley-Blackwell: Chichester, West Sussex, UK, 2011. [Google Scholar]
- Heard, D.J.; Huft, V.J. The effects of short-term physical restraint and isoflurane anesthesia on hematology and plasma biochemistry in the island flying fox (Pteropus hypomelanus). J. Zoo Wildl. Med. 1998, 29, 14–17. [Google Scholar] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jones, M.E.B.; Schuh, A.J.; Amman, B.R.; Sealy, T.K.; Zaki, S.R.; Nichol, S.T.; Towner, J.S. Experimental Inoculation of Egyptian Rousette Bats (Rousettus aegyptiacus) with Viruses of the Ebolavirus and Marburgvirus Genera. Viruses 2015, 7, 3420-3442. https://doi.org/10.3390/v7072779
Jones MEB, Schuh AJ, Amman BR, Sealy TK, Zaki SR, Nichol ST, Towner JS. Experimental Inoculation of Egyptian Rousette Bats (Rousettus aegyptiacus) with Viruses of the Ebolavirus and Marburgvirus Genera. Viruses. 2015; 7(7):3420-3442. https://doi.org/10.3390/v7072779
Chicago/Turabian StyleJones, Megan E.B., Amy J. Schuh, Brian R. Amman, Tara K. Sealy, Sherif R. Zaki, Stuart T. Nichol, and Jonathan S. Towner. 2015. "Experimental Inoculation of Egyptian Rousette Bats (Rousettus aegyptiacus) with Viruses of the Ebolavirus and Marburgvirus Genera" Viruses 7, no. 7: 3420-3442. https://doi.org/10.3390/v7072779






