What Are the Relationships between Psychosocial Community Characteristics and Dietary Behaviors in a Racially/Ethnically Diverse Urban Population in Los Angeles County?
Abstract
:1. Introduction
2. Materials and Methods
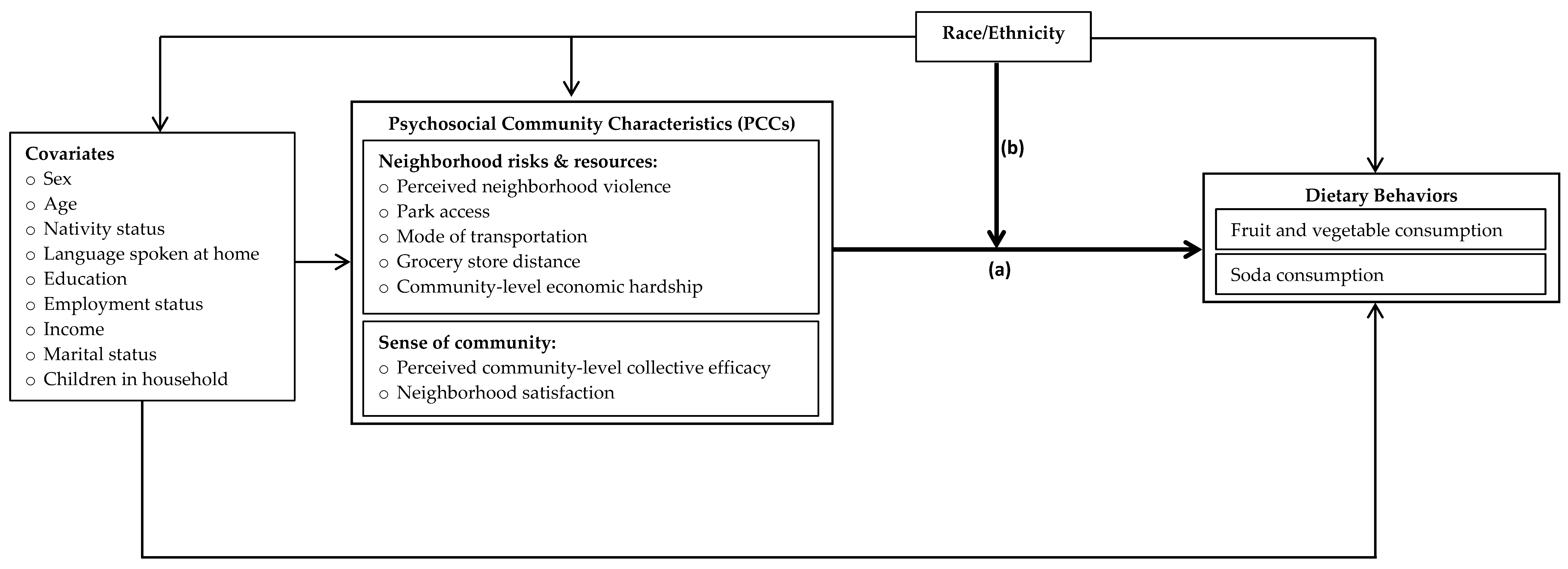
2.1. Conceptual Framework
2.2. Internet Panel Survey
2.3. Dependent Variables
2.3.1. F+V Consumption
2.3.2. Soda Consumption
2.4. Independent Variables
2.4.1. Neighborhood Risks and Resources
2.4.2. Sense of Community
2.5. Covariates
2.6. Statistical Analyses
3. Results
3.1. Descriptive Analyses
3.2. Negative Binomial Regression Analyses
3.2.1. F+V Consumption
3.2.2. Soda Consumption
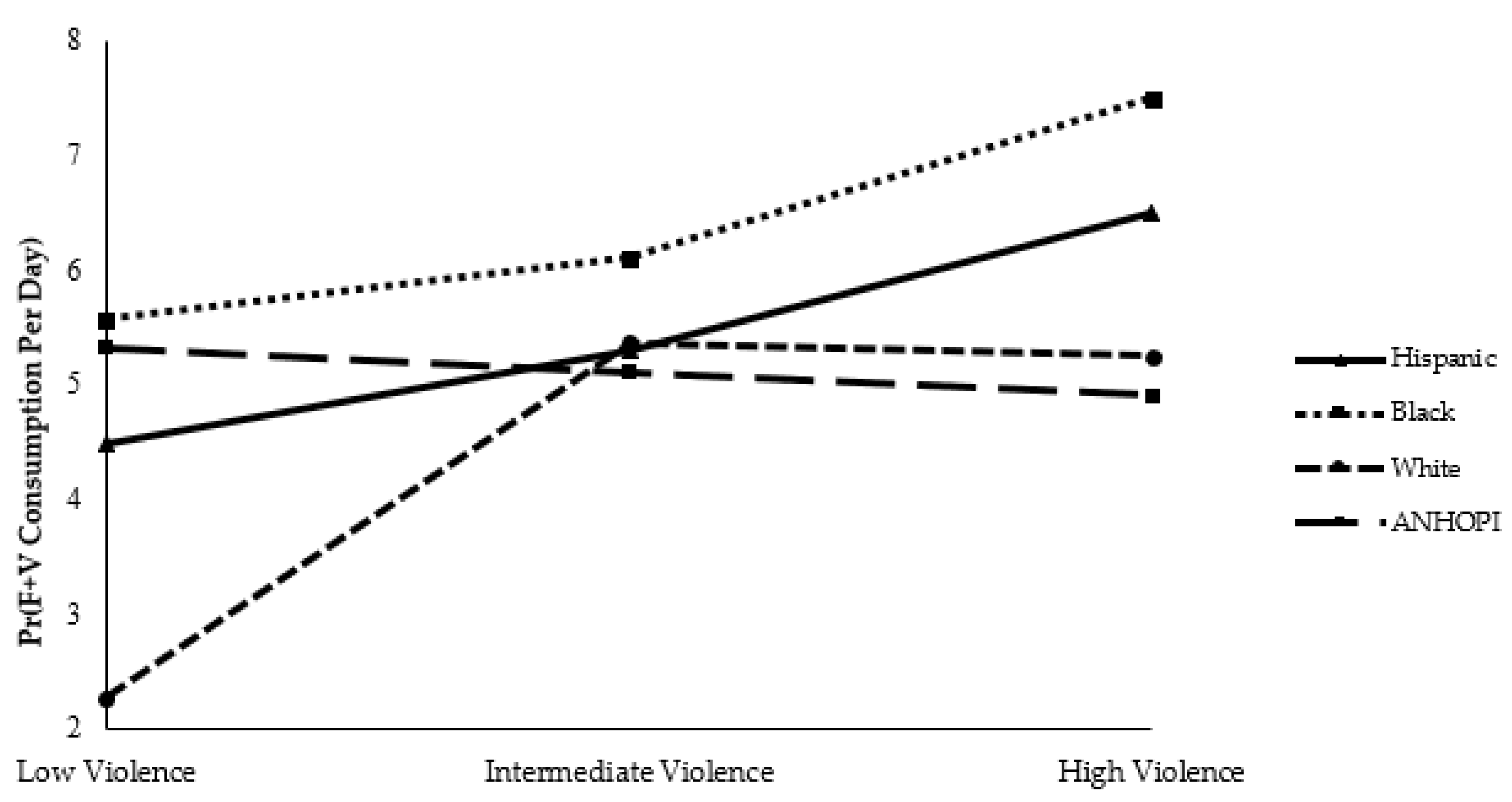
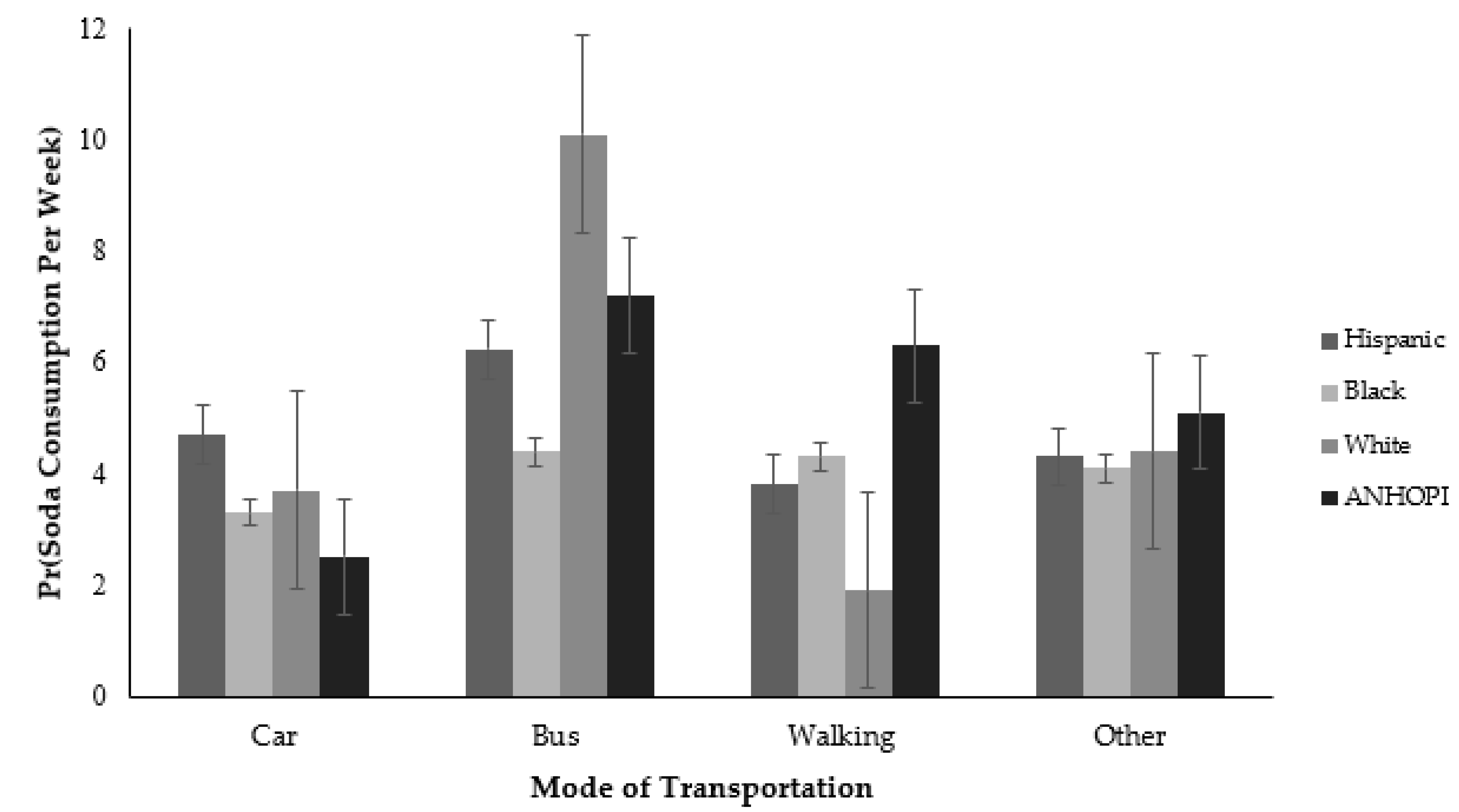
3.3. Moderation Analysis
4. Discussion
4.1. F+V Consumption
4.2. Soda Consumption
4.3. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pitt, E.; Gallegos, D.; Comans, T.; Cameron, C.; Thornton, L. Exploring the influence of local food environments on food behaviours: A systematic review of qualitative literature. Public Health Nutr. 2017, 20, 2393–2405. [Google Scholar] [CrossRef] [Green Version]
- Caspi, C.E.; Sorensen, G.; Subramanian, S.V.; Kawachi, I. The local food environment and diet: A systematic review. Health Place 2012, 18, 1172–1187. [Google Scholar] [CrossRef] [Green Version]
- Micha, R.; Shulkin, M.L.; Peñalvo, J.L.; Khatibzadeh, S.; Singh, G.M.; Rao, M.; Fahimi, S.; Powles, J.; Mozaffarian, D. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: Systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS ONE 2017, 12, e0175149. [Google Scholar]
- Bunnell, R.; O’Neil, D.; Soler, R.; Payne, R.; Giles, W.H.; Collins, J.; Bauer, U.; Communities Putting Prevention to Work Program Group. Fifty communities putting prevention to work: Accelerating chronic disease prevention through policy, systems and environmental change. J. Community Health 2012, 37, 1081–1090. [Google Scholar] [CrossRef] [PubMed]
- Savoie-Roskos, M.R.; DeWitt, K.; Coombs, C. Changes in nutrition education: A policy, systems, and environmental approach. J. Nutr. Educ. Behav. 2018, 50, 431. [Google Scholar] [CrossRef]
- Roof, K.; Oleru, N. Public health: Seattle and King County’s push for the built environment. J. Environ. Health 2008, 71, 24–27. [Google Scholar]
- Swinburn, B.; Vandevijvere, S.; Kraak, V.; Sacks, G.; Snowdon, W.; Hawkes, C.; Barquera, S.; Friel, S.; Kelly, B.; Kumanyika, S.; et al. Monitoring and benchmarking government policies and actions to improve the healthiness of food environments: A proposed government healthy food environment policy index. Obes Rev. 2013, 14 (Suppl. S1), 24–37. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Story, M.T.; Duffy, E. Supporting healthy eating: Synergistic effects of nutrition education paired with policy, systems, and environmental changes. Nestle Nutr. Inst. Workshop Ser. 2019, 92, 69–82. [Google Scholar]
- Lieberman, L.; Golden, S.D.; Earp, J.A. Structural approaches to health promotion: What do we need to know about policy and environmental change? Health Educ. Behav. 2013, 40, 520–525. [Google Scholar] [CrossRef]
- Forrest, R.; Kearns, A. Social cohesion, social capital and the neighbourhood. Urban Stud. 2001, 38, 2125–2143. [Google Scholar] [CrossRef]
- Robles, B.; Jewell, M.P.; Thomas Tobin, C.S.; Smith, L.V.; Kuo, T. Varying levels of depressive symptoms and lifestyle health behaviors in a low income, urban population. J. Behav. Med. 2021, 44, 212–221. [Google Scholar] [CrossRef]
- Schweren, L.J.S.; Larsson, H.; Vinke, P.C.; Li, L.; Kvalvik, L.G.; Arias-Vasquez, A.; Haavik, J.; Hartman, C.A. Diet quality, stress and common mental health problems: A cohort study of 121,008 adults. Clin. Nutr. 2021, 40, 901–906. [Google Scholar] [CrossRef]
- Arcaya, M.C.; Tucker-Seeley, R.D.; Kim, R.; Schnake-Mahl, A.; So, M.; Subramanian, S.V. Research on neighborhood effects on health in the United States: A systematic review of study characteristics. Soc. Sci. Med. 2016, 168, 16–29. [Google Scholar] [CrossRef] [Green Version]
- Black, J.L.; Macinko, J. Neighborhoods and obesity. Nutr. Rev. 2008, 66, 2–20. [Google Scholar] [CrossRef]
- Carroll-Scott, A.; Gilstad-Hayden, K.; Rosenthal, L.; Peters, S.M.; McCaslin, C.; Joyce, R.; Ickovics, J.R. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: The role of built, socioeconomic, and social environments. Soc. Sci. Med. 2013, 95, 106–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haynes-Maslow, L.; Auvergne, L.; Mark, B.; Ammerman, A.; Weiner, B.J. Low-income individuals’ perceptions about fruit and vegetable access programs: A qualitative study. J. Nutr. Educ. Behav. 2015, 47, 317–324.e1. [Google Scholar] [CrossRef] [Green Version]
- Ghosh-Dastidar, B.; Cohen, D.; Hunter, G.; Zenk, S.N.; Huang, C.; Beckman, R.; Dubowitz, T. Distance to store, food prices, and obesity in urban food deserts. Am. J. Prev. Med. 2014, 47, 587–595. [Google Scholar] [CrossRef] [Green Version]
- Suglia, S.F.; Shelton, R.C.; Hsiao, A.; Wang, Y.C.; Rundle, A.; Link, B.G. Why the neighborhood social environment is critical in obesity prevention. J. Urban Health 2016, 93, 206–212. [Google Scholar] [CrossRef] [Green Version]
- Diez Roux, A.V.; Mujahid, M.S.; Hirsch, J.A.; Moore, K.; Moore, L.V. The impact of neighborhoods on CV risk. Glob. Heart 2016, 11, 353–363. [Google Scholar] [CrossRef] [Green Version]
- Cohen, D.A.; Finch, B.K.; Bower, A.; Sastry, N. Collective efficacy and obesity: The potential influence of social factors on health. Soc. Sci. Med. 2006, 62, 769–778. [Google Scholar] [CrossRef]
- Shih, M.; Dumke, K.A.; Goran, M.I.; Simon, P.A. The association between community-level economic hardship and childhood obesity prevalence in Los Angeles. Pediatric Obes. 2013, 8, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.A.; Farley, T.A.; Mason, K. Why is poverty unhealthy? Social and physical mediators. Soc. Sci. Med. 2003, 57, 1631–1641. [Google Scholar] [CrossRef] [Green Version]
- Skrabski, A.; Kopp, M.; Kawachi, I. Social capital and collective efficacy in Hungary: Cross sectional associations with middle aged female and male mortality rates. J. Epidemiol. Community Health 2004, 58, 340–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joiner, J.; Jordan, M.; Reid, K.; Kintziger, K.; Duclos, C. Economic hardship and life expectancy in Nassau County, Florida. Prev. Chronic Dis. 2019, 16, E27. [Google Scholar] [CrossRef] [Green Version]
- Mouratidis, K. Neighborhood characteristics, neighborhood satisfaction, and well-being: The links with neighborhood deprivation. Land Use Policy 2020, 129, 104886. [Google Scholar] [CrossRef]
- Phelan, J.C.; Link, B.G. Is racism a fundamental cause of inequalities in health? Annu. Rev. Sociol. 2015, 41, 311–330. [Google Scholar]
- Williams, D.R.; Lawrence, J.A.; Davis, B.A. Racism and health: Evidence and needed research. Ann. Rev. Public Health 2019, 40, 105–125. [Google Scholar] [CrossRef] [Green Version]
- Mujahid, M.S.; Diez Roux, A.V.; Cooper, R.C.; Shea, S.; Williams, D.R. Neighborhood stressors and race/ethnic differences in hypertension prevalence (the Multi-Ethnic Study of Atherosclerosis). Am. J. Hypertens. 2011, 24, 187–193. [Google Scholar] [CrossRef] [Green Version]
- Brondolo, E.; Love, E.E.; Pencille, M.; Schoenthaler, A.; Ogedegbe, G. Racism and hypertension: A review of the empirical evidence and implications for clinical practice. Am. J. Hypertens. 2011, 24, 518–529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beyer, K.M.; Zhou, Y.; Matthews, K.; Bemanian, A.; Laud, P.W.; Nattinger, A.B. New spatially continuous indices of redlining and racial bias in mortgage lending: Links to survival after breast cancer diagnosis and implications for health disparities research. Health Place 2016, 40, 34–43. [Google Scholar] [CrossRef]
- Riley, A.R. Neighborhood disadvantage, residential segregation, and beyond-lessons for studying structural racism and health. J. Racial Ethn. Health Disparit. 2018, 5, 357–365. [Google Scholar] [CrossRef]
- Rigolon, A.; Browning, M.; Jennings, V. Inequities in the quality of urban park systems: An environmental justice investigation of cities in the United States. Landsc. Urban Plan. 2018, 178, 156–169. [Google Scholar] [CrossRef]
- Hughey, S.M.; Walsemann, K.M.; Child, S.; Powers, A.; Reed, J.A.; Kaczynski, A.T. Using an environmental justice approach to examine the relationships between park availability and quality indicators, neighborhood disadvantage, and racial/ethnic composition. Landsc. Urban Plan. 2016, 148, 159–169. [Google Scholar] [CrossRef]
- 2020–2025 Dietary Guidelines for Americans. Available online: https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf (accessed on 22 August 2021).
- Bolton, D.; Gillett, G. The Biopsychosocial Model of Health and Disease: New philosophical and scientific developments; Palgrave Pivot: Cham, Switzerland, 2019. [Google Scholar]
- Mezuk, B.; Abdou, C.M.; Hudson, D.; Kershaw, K.N.; Rafferty, J.A.; Lee, H.; Jackson, J.S. “White Box” epidemiology and the social neuroscience of health behaviors: The Environmental Affordances Model. Soc. Ment. Health 2013, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robles, B.; Thomas, C.S.; Lai, E.S.; Kuo, T. A geospatial analysis of health, mental health, and stressful community contexts in Los Angeles County. Prev. Chronic Dis. 2019, 16, E150. [Google Scholar] [CrossRef]
- Robles, B. Evaluating Community and Individual-Level Psychosocial Factors to Improve Chronic Disease-Related Dietary Behaviors: A Case Study of Los Angeles County. California Digital Library 2018. Ph.D. Thesis, University of California, Los Angeles, CA, USA, 2018. [Google Scholar]
- National Institutes of Health Eating at America’s Table Study: Quick Food Scan. Available online: https://epi.grants.cancer.gov/diet/shortreg/instruments/eats_all-day.pdf (accessed on 21 July 2021).
- Moore, L.V.; Thompson, F.E. Adults meeting fruit and vegetable intake recommendations–United States, 2013. MMWR Morb. Mortal Wkly. Rep. 2015, 64, 709–713. [Google Scholar] [PubMed]
- Guenther, P.M.; Dodd, K.W.; Reedy, J.; Krebs-Smith, S.M. Most Americans eat much less than recommended amounts of fruits and vegetables. J. Am. Diet. Assoc 2006, 106, 1371–1379. [Google Scholar] [CrossRef]
- 5 A Day Works! Available online: https://www.cdc.gov/nccdphp/dnpa/nutrition/health_professionals/programs/5aday_works.pdf (accessed on 21 July 2021).
- Havas, S.; Heimendinger, J.; Damron, D.; Nicklas, T.A.; Cowan, A.; Beresford, S.A.; Sorensen, G.; Buller, D.; Bishop, D.; Baranowski, T.; et al. 5 A Day for better health--nine community research projects to increase fruit and vegetable consumption. Public Health Rep. 1995, 110, 68–79. [Google Scholar] [CrossRef]
- Robles, B.; Kuo, T. Predictors of public support for nutrition-focused policy, systems and environmental change strategies in Los Angeles County, 2013. BMJ Open 2017, 7, e012654. [Google Scholar] [CrossRef] [Green Version]
- Cutting the Fat: The effect of New York City’s artificial trans fat ban on obesity. Available online: https://www.researchgate.net/profile/Lisa_Stolzenberg/publication/261992289_CUTTING_THE_FAT_The_Effect_of_New_York_City%27s_Artificial_Trans_Fat_Ban_on_Obesity/links/5523d6b70cf2c815e0732e3f/CUTTING-THE-FAT-The-Effect-of-New-York-Citys-Artificial-Trans-Fa (accessed on 21 July 2021).
- Robles, B.; Blitstein, J.L.; Lieberman, A.J.; Barragan, N.C.; Gase, L.N.; Kuo, T. The relationship between amount of soda consumed and intention to reduce soda consumption among adults exposed to the Choose Health LA ‘Sugar Pack’ health marketing campaign. Public Health Nutr. 2015, 18, 2582–2591. [Google Scholar] [CrossRef] [Green Version]
- Project on Human Development in Chicago Neighborhoods: Community Survey, 1994–1995 (ICPSR 2766). Available online: http://www.icpsr.umich.edu/icpsrweb/NACJD/studies/2766 (accessed on 21 July 2021).
- California Health Interview Survey (CHIS) 2009 Child Questionnaire. Available online: https://healthpolicy.ucla.edu/chis/design/Documents/CHIS2009childquestionnaire.pdf (accessed on 21 July 2021).
- Gase, L.N.; DeFosset, A.R.; Smith, L.V.; Kuo, T. The association between self-reported grocery store access, fruit and vegetable intake, sugar-sweetened beverage consumption, and obesity in a racially diverse, low-income population. Front. Public Health 2014, 2, 229. [Google Scholar] [CrossRef] [Green Version]
- Robles, B.; Montes, C.E.; Nobari, T.Z.; Wang, M.C.; Kuo, T. Dietary behaviors among public health center clients with electronic benefit transfer access at farmers’ markets. J. Acad. Nutr. Diet. 2017, 117, 58–68. [Google Scholar] [CrossRef] [PubMed]
- Sampson, R.J.; Raudenbush, S.W.; Earls, F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science 1997, 277, 918–924. [Google Scholar] [CrossRef]
- Sampson, R.J. The neighborhood context of well-being. Perspect. Biol. Med. 2003, 46 (Suppl. S3), S53–S64. [Google Scholar] [CrossRef]
- Los Angeles Family and Neighborhood Survey, Wave 2 (L.A.FANS-2). Available online: http://lasurvey.rand.org/documentation/questionnaires/wave2/LAFANS-2_Adult.pdf (accessed on 21 July 2021).
- Halbert, C.H.; Bellamy, S.; Briggs, V.; Bowman, M.; Delmoor, E.; Kumanyika, S.; Rogers, R.; Purnell, J.; Weathers, B.; Johnson, J.C. Collective efficacy and obesity-related health behaviors in a community sample of African Americans. J. Community Health 2014, 39, 124–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Theall, K.P.; Chaparro, M.P.; Denstel, K.; Bilfield, A.; Drury, S.S. Childhood obesity and the associated roles of neighborhood and biologic stress. Prev. Med. Rep. 2019, 14, 100849. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G.; Kalle-Uhlmann, T.; Arregui, M.; Buijsse, B.; Boeing, H. Fruit and vegetable consumption and changes in anthropometric variables in adult populations: A systematic review and meta-analysis of prospective cohort studies. PLoS ONE 2015, 10, e0140846. [Google Scholar] [CrossRef]
- Michimi, A.; Wimberly, M.C. Associations of supermarket accessibility with obesity and fruit and vegetable consumption in the conterminous United States. Int. J. Health Geogr. 2010, 9, 49. [Google Scholar] [CrossRef] [Green Version]
- Dunn, R.A.; Wesley, W.R.; Johnson, C.M.; Leidner, A.; Sharkey, J.R. The effect of distance and cost on fruit and vegetable consumption in rural Texas. J. Appl. Econ. 2012, 44, 491–500. [Google Scholar] [CrossRef] [Green Version]
- Leung, C.W.; Tester, J.M. The association between food insecurity and diet quality varies by race/ethnicity: An analysis of national health and nutrition examination survey 2011–2014 results. J. Acad. Nutr. Diet. 2019, 119, 1676–1686. [Google Scholar] [CrossRef]
- Dellmelle, E.C. Differentiating pathways of neighborhood change in 50 U.S. metropolitan areas. Environ. Plan. A 2017, 49, 2402–2424. [Google Scholar] [CrossRef]
- Intrator, J.; Tannen, J.; Massey, D.S. Segregation by race and income in the United States 1970–2010. Soc. Sci. Res. 2016, 60, 45–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reardon, S.F.; Fox, L.; Townsend, J. Neighborhood income composition by race and income, 1990–2009. Ann. AAPSS 2015, 660, 78–97. [Google Scholar] [CrossRef]
- Kern, D.M.; Auchincloss, A.H.; Robinson, L.F.; Stehr, M.F.; Pham-Kanter, G. Healthy and unhealthy food prices across neighborhoods and their association with neighborhood socioeconomic status and proportion Black/Hispanic. J. Urban Health 2017, 94, 494–505. [Google Scholar] [CrossRef] [PubMed]
- Robles, B.; Barragan, N.; Smith, B.; Caldwell, J.; Shah, D.; Kuo, T. Lessons learned from implementing the Supplemental Nutrition Assistance Program Education Small Corner Store Project in Los Angeles County. Prev. Med. Rep. 2019, 16, 100997. [Google Scholar] [CrossRef] [PubMed]
- DeFosset, A.R.; Kwan, A.; Rizik-Baer, D.; Gutierrez, L.; Gase, L.N.; Kuo, T. Implementing a healthy food distribution program: A supply chain strategy to increase fruit and vegetable access in underserved areas. Prev. Chronic Dis. 2018, 15, E61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robles, B.; Wright, T.G.; Caldwell, J.; Kuo, T. Promoting congregant health in faith-based organizations across Los Angeles County, 2013–2016. Prev. Med. Rep. 2019, 16, 100963. [Google Scholar] [CrossRef] [PubMed]
- Robles, B.; Wood, M.; Kimmons, J.; Kuo, T. Comparison of nutrition standards and other recommended procurement practices for improving institutional food offerings in Los Angeles County, 2010–2012. Adv. Nutr. 2013, 4, 191–202. [Google Scholar] [CrossRef] [Green Version]
- Groesz, L.M.; McCoy, S.; Carl, J.; Saslow, L.; Stewart, J.; Adler, N.; Laraia, B.; Epel, E. What is eating you? Stress and the drive to eat. Appetite 2012, 58, 717–721. [Google Scholar] [CrossRef] [Green Version]
- Harrington, E.F.; Crowther, J.H.; Shipherd, J.C. Trauma, binge eating, and the “strong Black woman”. J. Consult. Clin. Psychol. 2010, 78, 469–479. [Google Scholar] [CrossRef] [PubMed]
- Goode, R.W.; Cowell, M.M.; Mazzeo, S.E.; Cooper-Lewter, C.; Forte, A.; Olayia, O.I.; Bulik, C.M. Binge eating and binge-eating disorder in Black women: A systematic review. Int. J. Eat. Disord. 2020, 53, 491–507. [Google Scholar] [CrossRef] [PubMed]
- Ellis, K.R.; Griffith, D.M.; Allen, J.O.; Thorpe, R.J.; Bruce, M.A. “If you do nothing about stress, the next thing you know, you’re shattered”: Perspectives on African American men’s stress, coping and health from African American men and key women in their lives. Soc. Sci. Med. 2015, 139, 107–114. [Google Scholar] [CrossRef] [Green Version]
- Fisher, J.O.; Arreola, A.; Birch, L.L.; Rolls, B.J. Portion size effects on daily energy intake in low-income Hispanic and African American children and their mothers. Am. J. Clin. Nutr. 2007, 86, 1709–1716. [Google Scholar] [CrossRef] [PubMed]
- Beccia, A.L.; Jesdale, W.M.; Lapane, K.L. Associations between perceived everyday discrimination, discrimination attributions, and binge eating among Latinas: Results from the National Latino and Asian American Study. Ann. Epidemiol. 2020, 45, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, K.D. Food, culture, and diabetes in the United States. Clin. Diabetes 2004, 22, 190–192. [Google Scholar] [CrossRef] [Green Version]
- Grigsby-Toussaint, D.S.; Zenk, S.N.; Odoms-Young, A.; Ruggiero, L.; Moise, I. Availability of commonly consumed and culturally specific fruits and vegetables in African-American and Latino neighborhoods. J. Am. Diet. Assoc. 2010, 110, 746–752. [Google Scholar] [CrossRef] [Green Version]
- Bekelman, T.A.; Johnson, S.L.; Taylor, C.A. Differences in diet quality and snack intakes among Non-Hispanic White and Mexican American adolescents from different acculturation groups. J. Racial Ethn. Health Disparit. 2020, 7, 1090–1099. [Google Scholar] [CrossRef]
- Lee-Kwan, S.H.; Moore, L.V.; Blanck, H.M.; Harris, D.M.; Galuska, D. Disparities in state-specific adult fruit and vegetable consumption–United States, 2015. Morb. Mortal. Wkly. Rep. 2017, 66, 1241–1247. [Google Scholar] [CrossRef]
- Basu, S.; Akers, M.; Berkowitz, S.A.; Josey, K.; Schillinger, D.; Seligman, H. Comparison of fruit and vegetable intake among urban low-income US adults receiving a produce voucher in 2 cities. JAMA Netw. Open 2021, 4, e211757. [Google Scholar] [CrossRef]
- Los Angeles County Department of Public Health Key Indicators of Health. Available online: http://publichealth.lacounty.gov/ha/docs/2015LACHS/KeyIndicator/Correction/KIH_020617-sec.pdf (accessed on 21 July 2021).
- Barragan, N.C.; Noller, A.J.; Robles, B.; Gase, L.N.; Leighs, M.S.; Bogert, S.; Simon, P.A.; Kuo, T. The “Sugar Pack” health marketing campaign in Los Angeles County, 2011–2012. Health Promot. Pract. 2014, 15, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Aburto, N.J.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F.P.; Meerpohl, J.J. Effect of lower sodium intake on health: Systematic review and meta-analyses. BMJ 2013, 346, f1326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simon, P.A.; Wold, C.M.; Cousineau, M.R.; Fielding, J.E. Meeting the data needs of a local health department: The Los Angeles County Health Survey. Am. J. Public Health 2001, 91, 1950–1952. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Wang, B.; Yuan, T.; Chen, X.; Ao, Y.; Fitzpatrick, T.; Li, P.; Zhou, Y.; Lin, Y.F.; Duan, Q.; et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J. Infect. 2020, 80, 656–665. [Google Scholar] [CrossRef]
- Shah, H.; Khan, M.S.H.; Dhurandhar, N.V.; Hegde, V. The triumvirate: Why hypertension, obesity, and diabetes are risk factors for adverse effects in patients with COVID-19. Acta Diabetol. 2021, 58, 831–843. [Google Scholar] [CrossRef]

| Characteristics | Number (%) or Mean [SD] |
|---|---|
| Dietary Behaviors | |
| Fruit and vegetable consumption | |
| Optimal consumption (≥5 servings per day) | 472 (49.5) |
| Intermediate consumption (3–4 servings per day) | 278 (29.1) |
| Worse consumption (0–2 servings per day) | 204 (21.4) |
| Mean fruit and vegetable consumption | 5.6 [4.3] |
| Soda consumption | |
| Optimal consumption (0 sodas per week) | 233 (24.4) |
| Intermediate consumption (1–6 sodas per week) | 532 (55.8) |
| Worse consumption (≥7 sodas per week) | 189 (19.8) |
| Mean soda consumption | 4.4 [5.9] |
| Psychosocial Community Characteristics | |
| Neighborhood risks and resources | |
| Perceived neighborhood violence | |
| Low violence | 364 (38.2) |
| Intermediate violence | 283 (29.7) |
| High violence | 307 (32.2) |
| Park access | |
| Has park access | 774 (81.1) |
| Does not have park access | 180 (18.9) |
| Mode of transportation to the nearest grocery store | |
| Car | 775 (81.2) |
| Bus | 38 (4.0) |
| Walking | 123 (12.9) |
| Other | 18 (1.9) |
| Mean average number of miles traveled to the nearest grocery store | 4.1 [6.1] |
| Mean community-level economic hardship | 50.4 [17.5] |
| Sense of community | |
| Mean perceived community-level collective efficacy | 33.8 [7.9] |
| Neighborhood satisfaction | |
| Very satisfied/satisfied | 852 (89.3) |
| Very dissatisfied/dissatisfied | 102 (10.7) |
| Sociodemographic Characteristics | |
| Sex | |
| Female | 472 (49.5) |
| Male | 482 (50.5) |
| Age (years) | |
| 18–30 | 401 (42.0) |
| 31–40 | 245 (25.7) |
| 41–50 | 127 (13.3) |
| Older than 50 | 181 (19.0) |
| Race/ethnicity | |
| Hispanic | 468 (49.1) |
| Black | 88 (9.2) |
| White | 251 (26.3) |
| ANHOPI | 147 (15.4) |
| Nativity Status | |
| Born in Los Angeles County | 637 (66.8) |
| Native born but outside of Los Angeles County | 203 (21.3) |
| Foreign born | 114 (12.0) |
| Language spoken at home | |
| English | 728 (76.3) |
| Not English | 226 (23.7) |
| Education | |
| High school or less | 184 (19.3) |
| Technical/vocational school or some college | 343 (36.0) |
| College graduate/postgraduate | 427 (44.8) |
| Employment Status | |
| Employed–full time | 531 (55.7) |
| Employed–part time | 114 (12.0) |
| Unemployed | 104 (10.9) |
| Other employment status | 205 (21.5) |
| Income | |
| Under $50,000 | 436 (45.7) |
| $50,000–$99,000 | 297 (31.1) |
| $100,000 or more | 221 (23.2) |
| Marital Status | |
| Married | 367 (38.5) |
| Single | 511 (53.6) |
| Divorced/Separated/Widowed | 76 (8.0) |
| Mean number of children in the household | 0.8 [1.1] |
| Fruit and Vegetable Consumption | Soda Consumption | |||
|---|---|---|---|---|
| PCCs Only | Full Model a | PCCs Only | Full Modela | |
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Psychosocial Community Characteristics | ||||
| Perceived neighborhood violence (ref: low violence) | ||||
| Intermediate violence | 1.09 (0.98–1.23) | 1.08 (0.97–1.20) | 1.07 (0.87–1.33) | 1.02 (0.82–1.25) |
| High violence | 1.27 (1.13–1.43) *** | 1.24 (1.11–1.40) *** | 1.42 (1.14–1.77) ** | 1.24 (0.99–1.54) |
| Park access (ref: has park access) | ||||
| Does not have park access | 0.95 (0.84–1.07) | 0.94 (0.83–1.06) | 0.89 (0.71–1.10) | 0.88 (0.70–1.10) |
| Mode of transportation (ref: Car) | ||||
| Bus | 1.18 (0.92–1.53) | 1.25 (0.97–1.61) | 1.47 (0.98–2.22) | 1.53 (0.98–2.38) |
| Walking | 1.03 (0.89–1.19) | 1.08 (0.94–1.24) | 0.99 (0.76–1.28) | 0.89 (0.69–1.15) |
| Other | 1.45 (1.02–2.06) * | 1.38 (0.99–1.93) | 1.24 (0.85–1.80) | 1.20 (0.78–1.85) |
| Grocery store distance | 1.01 (1.00–1.02) b ** | 1.01 (1.00–1.02) b * | 1.02 (1.01–1.03) ** | 1.01 (1.00–1.02) |
| Community-level economic hardship | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.01) | 1.00 (0.99–1.00) |
| Perceived community-level collective efficacy | 1.02 (1.01–1.02) *** | 1.02 (1.01–1.02) *** | 1.01 (1.00–1.02) | 1.01 (0.99–1.02) |
| Neighborhood satisfaction (ref: very satisfied/satisfied) | ||||
| Very dissatisfied/dissatisfied | 0.86 (0.74–1.01) | 0.88 (0.76–1.03) | 0.94 (0.69–1.29) | 0.97 (0.71–1.33) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robles, B.; Kuo, T.; Thomas Tobin, C.S. What Are the Relationships between Psychosocial Community Characteristics and Dietary Behaviors in a Racially/Ethnically Diverse Urban Population in Los Angeles County? Int. J. Environ. Res. Public Health 2021, 18, 9868. https://doi.org/10.3390/ijerph18189868
Robles B, Kuo T, Thomas Tobin CS. What Are the Relationships between Psychosocial Community Characteristics and Dietary Behaviors in a Racially/Ethnically Diverse Urban Population in Los Angeles County? International Journal of Environmental Research and Public Health. 2021; 18(18):9868. https://doi.org/10.3390/ijerph18189868
Chicago/Turabian StyleRobles, Brenda, Tony Kuo, and Courtney S. Thomas Tobin. 2021. "What Are the Relationships between Psychosocial Community Characteristics and Dietary Behaviors in a Racially/Ethnically Diverse Urban Population in Los Angeles County?" International Journal of Environmental Research and Public Health 18, no. 18: 9868. https://doi.org/10.3390/ijerph18189868






