From Burden to Depressive Symptoms in Informal Caregivers during the COVID-19 Pandemic: A Path Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. SF-12
2.2. Fatigue Severity Scale (FSS)
2.3. ADL and IADL
2.4. Zarit Caregiver Burden Scale
2.5. Beck Depression Inventory
2.6. COVID-19 Related Questions
2.7. Statistical Analysis
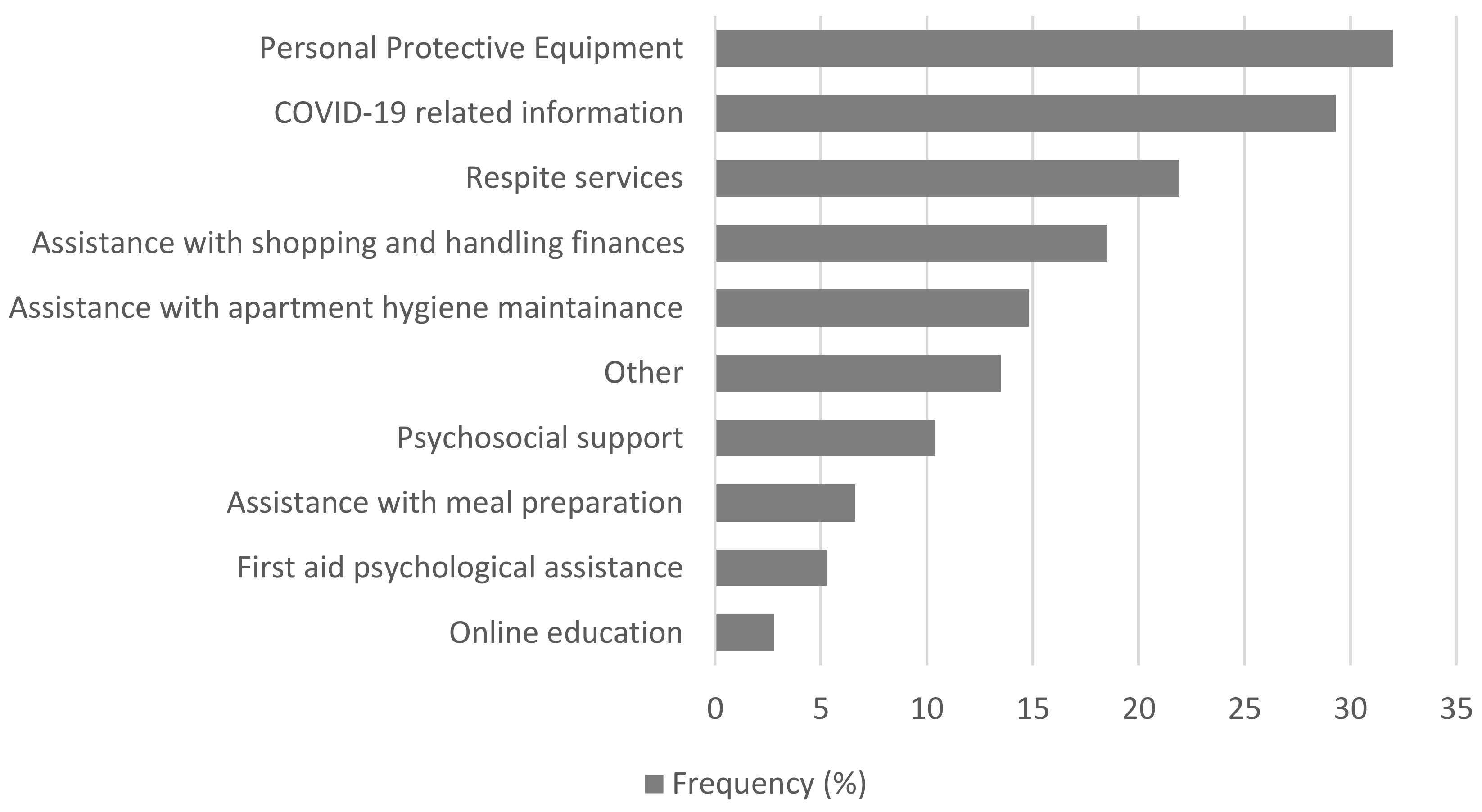
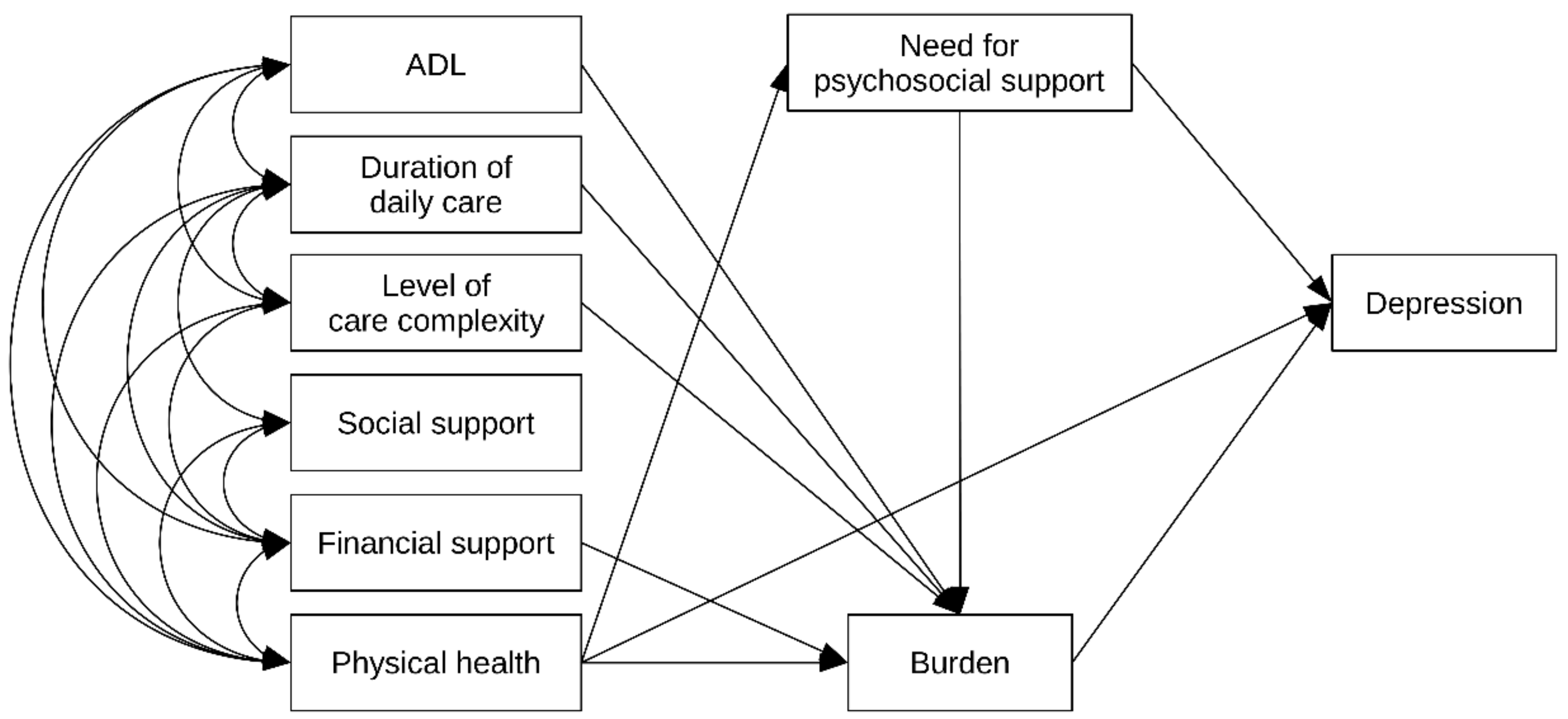
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eurocarer’s Analysis of the European Semester: Informal Carers, Left Aside Again?; Eurocarer’s Position Paper. Available online: https://eurocarers.org/publications/eurocarers-analysis-of-the-european-semester-informal-carers-left-aside-again-2/ (accessed on 31 August 2021).
- Impact of the Covid-19 Outbreak on Informal Carers Across Europe; Eurocarer’s Final Report. Available online: https://eurocarers.org/publications/impact-of-the-covid-19-outbreak-on-informal-carers-across-europe/ (accessed on 31 August 2021).
- Lovell, B.; Wetherell, M.A. The cost of caregiving: Endocrine and immune implications in elderly and non elderly caregivers. Neurosci. Biobehav. Rev. 2011, 35, 1342–1352. [Google Scholar] [CrossRef]
- George, L.K.; Gwyther, L.P. Caregiver well-being: A multidimensional examination of family caregivers of demented adults. Gerontologist 1986, 26, 253–259. [Google Scholar] [CrossRef]
- Adelman, R.; Tmanova, L.; Delgado, D.; Dion, S.; Lachs, M. Caregiver burden: A clinical review. JAMA 2014, 311, 1052–1060. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M.; Sörensen, S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci 2003, 58, 112–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, L.; Onwumere, J.; Craig, T.; McManus, S.; Bebbington, P.; Kuipers, E. Mental and physical illness in caregivers: Results from an English national survey sample. Br. J. Psychiatry 2014, 205, 197–203. [Google Scholar] [CrossRef]
- Pottie, C.G.; Burch, K.A.; Montross Thomas, L.P.; Irwin, S.A. Informal caregiving of hospice patients. J. Palliat. Med. 2015, 17, 845–856. [Google Scholar] [CrossRef]
- Sallim, A.B.; Sayampanathan, A.A.; Cuttilan, A.; Chun-Man Ho, R. Prevalence of mental health disorders among caregivers of patients with alzheimer disease. J. Am. Med. Dir. Assoc. 2015, 16, 1034–1041. [Google Scholar] [CrossRef] [PubMed]
- Kiecolt-Glaser, J.K.; Preacher, K.J.; Mac Callum, R.C.; Atkinson, C.; Malarkey, W.B.; Glaser, R. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proc. Natl. Acad. Sci. USA 2003, 100, 9090–9095. [Google Scholar] [CrossRef] [Green Version]
- Von Känel, R.; Dimsdale, J.E.; Ancoli-Israel, S.; Mills, P.J.; Patterson, T.L.; McKibbin, C.L.; Archuleta, C.; Grant, I. Poor sleep is associated with higher plasma Proinflammatory cytokine Interleukin-6 and Procoagulant marker fibrin D-dimer in older caregivers of people with Alzheimer’s disease. J. Am. Geriatr. Soc. 2006, 54, 431–437. [Google Scholar] [CrossRef]
- Capistrant, B.D.; Moon, J.R.; Glymour, M.M. Spousal caregiving and incident hypertension. Am. J. Hypertens. 2012, 25, 437–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schreiner, A.S.; Morimoto, T.; Arai, Y.; Zarit, S. Assessing family caregiver’s mental health using a statistically derived cut-off score for the Zarit Burden Interview. Aging Ment. Health 2006, 10, 107–111. [Google Scholar] [CrossRef]
- The Impact of Caregiving on Informal Carers’ Mental and Physical Health. Available online: https://eurocarers.org/publications/the-impact-of-caregiving-on-informal-carers-mental-and-physical-health/ (accessed on 31 August 2021).
- Pearlin, L.I.; Mullan, J.T.; Semple, S.J.; Skaff, M.M. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist 1990, 30, 583–594. [Google Scholar] [CrossRef]
- Lawton, M.P.; Moss, M.; Kleban, M.H.; Glicksman, A.; Rovine, M. A two-factor model of caregiving appraisal and psychological well-being. J. Gerontol. 1991, 46, 181–189. [Google Scholar] [CrossRef]
- Sörensen, S.; Duberstein, P.; Gill, D.; Pinquart, M. Dementia care: Mental health effects, intervention strategies, and clinical implications. Lancet Neurol. 2006, 5, 961–973. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 6, 547–560. [Google Scholar] [CrossRef]
- Gallagher, S.; Wetherell, M.A. Risk of depression in family caregivers: Unintended consequence of COVID-19. BJPsych Open 2020, 6, e119. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Keller, S.D. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales, 2nd ed.; Health Institute, New England Medical Centre: Boston, UK, 1995. [Google Scholar]
- Krupp, L.B.; LaRocca, N.G.; Muir-Nash, J.; Steinberg, A.D. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef] [PubMed]
- Staff of the Benjamin Rose Hospital. Multidisciplinary studies of illness in aged persons: II. A new classification of functional status in activities of daily living. J. Chronic Dis. 1959, 9, 55–62. [Google Scholar] [CrossRef]
- Zarit, S.H.; Reever, K.E.; Back-Peterson, J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist 1980, 20, 649–655. [Google Scholar] [CrossRef] [Green Version]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sethabouppha, H.; Kane, C. Caring for the seriously mentally ill in Thailand: Buddhist family caregiving. Arch. Psychiatr. Nurs. 2005, 19, 44–57. [Google Scholar] [CrossRef]
- Gater, A.; Rofail, D.; Tolley, C.; Marshall, C.; Abetz-Webb, L.; Zarit, S.H.; Berardo, C.G. “Sometimes It’s Difficult to Have a Normal Life”: Results from a Qualitative Study Exploring Caregiver Burden in Schizophrenia. Schizophr. Res. Treat. 2014, 2014, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Yu, Y.; Liu, Z.W.; Tang, B.W.; Zhao, M.; Liu, X.G.; Xiao, S.Y. Reported family burden of schizophrenia patients in rural China. PLoS ONE 2017, 12, e0179425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del-Pino-Casado, R.; Frías-Osuna, A.; Palomino-Moral, P.A.; Ruzafa-Martínez, M.; Ramos-Morcillo, A.J. Social support and subjective burden in caregivers of adults and older adults: A meta-analysis. PLoS ONE 2018, 13, e0189874. [Google Scholar] [CrossRef] [Green Version]
- Del-Pino-Casado, R.; Rodríguez Cardosa, M.; López-Martínez, C.; Orgeta, V. The association between subjective caregiver burden and depressive symptoms in carers of older relatives: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0217648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Todorovic, N.; Vracevic, M.; Rajovic, N.; Pavlovic, V.; Madzarevic, P.; Cumic, J.; Mostic, T.; Milic, N.; Rajovic, T.; Sapic, R.; et al. Quality of Life of Informal Caregivers behind the Scene of the COVID-19 Epidemic in Serbia. Medicina 2020, 56, 647. [Google Scholar] [CrossRef] [PubMed]
- Netherlands Ministry of Foreign Affairs. Amsterdam Conference Declaration. 2019. Available online: https://www.government.nl/documents/diplomatic-statements/2019/10/08/amsterdam-conference-declaration (accessed on 22 August 2021).
- Inter-Agency Standing Committee (IASC). IASC Guidelines on Mental Health and Psychosocial Support in Emergency Settings; Inter-Agency Standing Committee (IASC): Geneva, Switzerland, 2007. [Google Scholar]
- Pan American Health Organization. Minimum Package of Recommended MHPSS Interventions for COVID-19. Available online: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=15786:paquete-minimo-de-intervenciones-smaps-recomendadas-para-covid-19&Itemid=1426&lang=en (accessed on 22 August 2021).
- Wiegelmann, H.; Speller, S.; Verhaert, L.M.; Schirra-Weirich, L.; Wolf-Ostermann, K. Psychosocial interventions to support the mental health of informal caregivers of persons living with dementia—A systematic literature review. BMC Geriatr. 2021, 21, 94. [Google Scholar] [CrossRef]
- Treanor, C.J.; Santin, O.; Prue, G.; Coleman, H.; Cardwell, C.R.; O’Halloran, P.; Donnelly, M. Psychosocial interventions for informal caregivers of people living with cancer. Cochrane Database Syst. Rev. 2019, 6, CD009912. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic Characteristics of Informal Caregivers | n (%) * |
|---|---|
| Female gender | 560 (70.8) |
| Age | |
| 18–34 | 47 (6.0) |
| 35–64 | 574 (72.8) |
| 65+ | 167 (21.2) |
| Marital status | |
| Married | 472 (59.4) |
| Single | 101 (12.7) |
| Divorced | 98 (12.3) |
| Widowed | 95 (11.9) |
| Domestic partnership | 31 (3.9) |
| Level of education | |
| Primary education or below | 107 (13.4) |
| Secondary education | 444 (55.8) |
| Tertiary education or above | 245 (30.8) |
| Employment status | |
| Employed | 376 (47.2) |
| Unemployed | 154 (19.3) |
| Retired | 192 (24.1) |
| Housewife | 60 (7.5) |
| Other | 15 (1.9) |
| Caring alone | 537 (67.5) |
| Number of persons cared for | |
| One | 667 (84.9) |
| More than one | 119 (15.1) |
| SF-12, mean ± sd, range | |
| Physical health score | 45.6 ± 11.1 (19–64) |
| Mental health score | 41.0 ± 6.3 (22–57) |
| Fatigue severity scale (FSS), mean ± sd, range | 3.5 ± 1.8 (1–7) |
| Characteristics of Care and Care Recipients | n (%) * |
|---|---|
| Age (years) | |
| <18 | 19 (2.4) |
| 18–65 | 136 (17.0) |
| ≥65 | 637 (80.4) |
| Female gender | 467 (60.2) |
| Duration of caregiving (years) | |
| ≤1 | 188 (24.3) |
| 2–9 | 437 (56.4) |
| ≥10 | 149 (19.3) |
| Caregiving frequency | |
| Everyday | 619 (78.5) |
| Several times a week | 122 (15.5) |
| At least once a week | 33 (4.2) |
| At least once a month | 15 (1.9) |
| Daily duration of caregiving (hours) | |
| <6 | 295 (38.0) |
| 6–12 | 122 (15.7) |
| >12 | 360 (46.3) |
| Living with caregiver in joint household | 531 (66.6) |
| Related to caregiver | 712 (90.6) |
| Relationship with care recipient | |
| Father/mother | 326 (45.8) |
| Husband/wife | 95 (13.4) |
| Son/daughter | 61 (8.6) |
| Other blood relative | 229 (32.2) |
| Sufficient financial means | 251 (31.6) |
| Regular financial aid | 145 (18.3) |
| Zarit Caregiver Burden Scale | n (%) |
|---|---|
| Little or no burden | 230 (28.8) |
| Mild to moderate burden | 309 (38.7) |
| Moderate to severe burden | 211 (26.4) |
| Severe burden | 48 (6.0) |
| Beck Depression Inventory | |
| No depression | 577 (72.9) |
| Mild depression | 89 (11.2) |
| Moderate depression | 69 (8.7) |
| Severe depression | 57 (7.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rajovic, T.; Todorovic, N.; Vracevic, M.; Rajovic, N.; Pavlovic, A.; Pavlovic, V.; Grbic, I.; Sapic, R.; Krsmanovic, S.; Vukmirovic, M.; et al. From Burden to Depressive Symptoms in Informal Caregivers during the COVID-19 Pandemic: A Path Analysis. Int. J. Environ. Res. Public Health 2021, 18, 9577. https://doi.org/10.3390/ijerph18189577
Rajovic T, Todorovic N, Vracevic M, Rajovic N, Pavlovic A, Pavlovic V, Grbic I, Sapic R, Krsmanovic S, Vukmirovic M, et al. From Burden to Depressive Symptoms in Informal Caregivers during the COVID-19 Pandemic: A Path Analysis. International Journal of Environmental Research and Public Health. 2021; 18(18):9577. https://doi.org/10.3390/ijerph18189577
Chicago/Turabian StyleRajovic, Tatjana, Natasa Todorovic, Milutin Vracevic, Nina Rajovic, Andrija Pavlovic, Vedrana Pavlovic, Igor Grbic, Rosa Sapic, Slavica Krsmanovic, Marijana Vukmirovic, and et al. 2021. "From Burden to Depressive Symptoms in Informal Caregivers during the COVID-19 Pandemic: A Path Analysis" International Journal of Environmental Research and Public Health 18, no. 18: 9577. https://doi.org/10.3390/ijerph18189577









