The Influence of Examiner Experience on Inter- and Intra-Rater Agreement in Dental Restorations Identification on Three-Dimensional Digital Models
Abstract
1. Introduction
- Seven Surfaces for six upper Molars.
- Five Surfaces for
- ◾
- Six upper Canines and Premolars;
- ◾
- Six lower Canines and Premolars;
- ◾
- Four upper Incisors.
- Four surfaces for four lower Incisors.
- Six surfaces for six lower Molars.
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
2.3. Diagnostic Methods
2.3.1. Visual Examination (ICDAS)
2.3.2. Intraoral Scanners
2.4. Missing Data
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Bias Avoidance Strategy
- -
- intra-rater agreement for different examination methods amongst the 3 methods used, on the same patients;
- -
- inter-rater agreement for the same examination method for different experience levels examiners, tested on the same patient.
- -
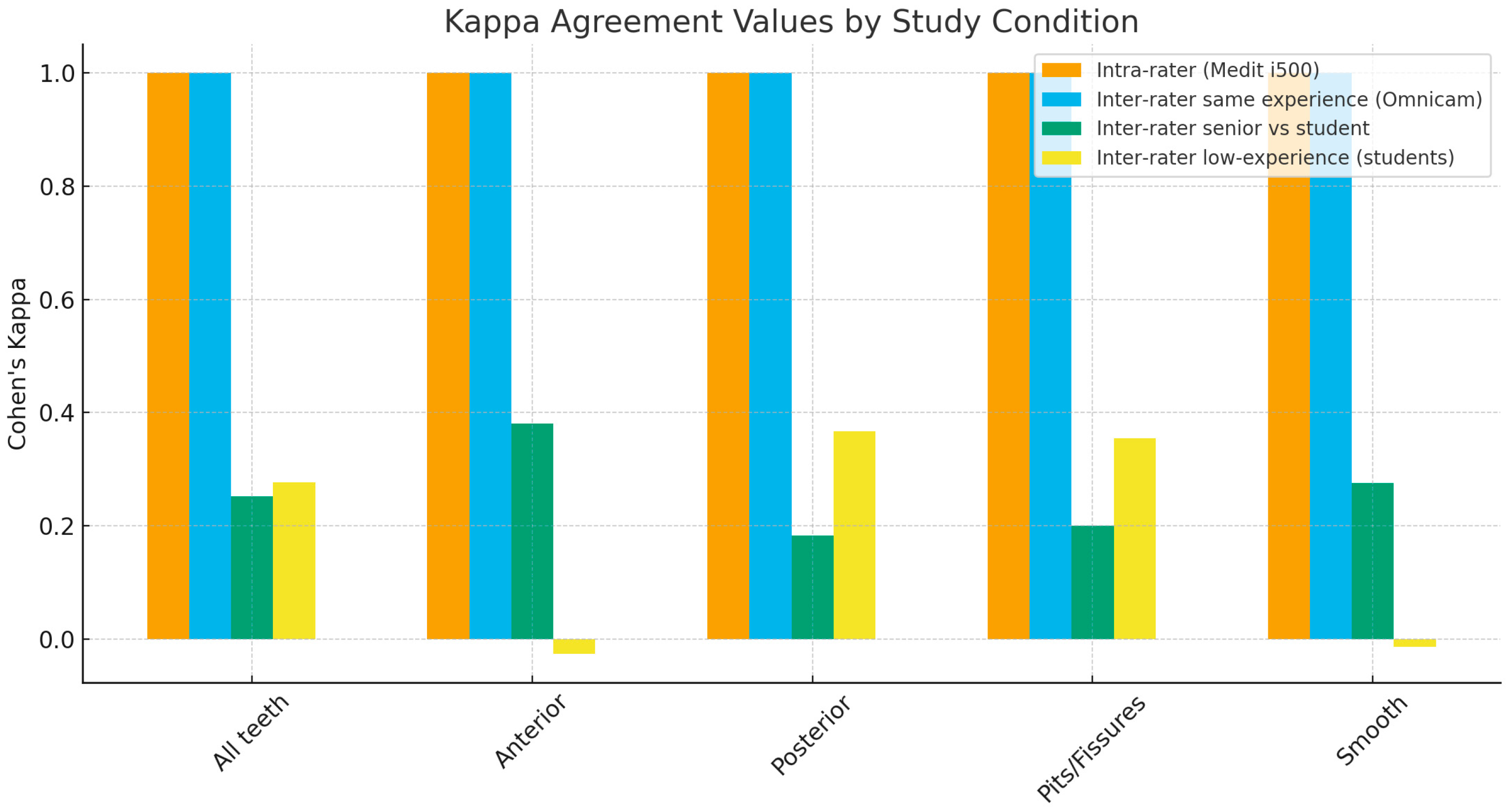
- for Medit 500-Clinical, the agreement was 1 probably because there were only nine tooth-colored restorations (code 3 ICDAS), meaning 3.12% out of the total number of surfaces;
- -
- For Omnicam, rater 3 with rater 31, the agreement of experienced raters was also 1, meaning that all nine existing tooth-colored restorations (3.12% of the total number of surfaces) were correctly rated and the surfaces without restorations were identically rated as well.
- -
- We addressed the memory or learning bias as follows: since the ICDAS pre-calibration, the examiners used the ICDAS daily (in total each examiner filled in up to 90 ICDAS files for this study only). The 3-month interval was between the examinations of the same patient in order for the intra-rater agreement not to be biased by seeing the same patient too soon through different methods. For each patient, the clinical examination and the two intraoral scans were performed on the same day, and then the digital 3D models were examined at 3 months interval to avoid bias due to the same examiner memorizing the ICDAS codes which she/he assigned. Each rater filled in ICDAS paper files without consulting previous scoring of the same patient. Professional cleaning and 5 s of air-drying of all surfaces should have minimized, but not completely eliminated, other possible sources of bias, such as examiner familiarity with ICDAS, scanning artifacts, or differences between scanner types. This 3-month interval between examinations also minimized another possible limitation of the study, the lack of examiner blinding.
- -
- Another possible source of bias could be the experience of the examiner, but one of the aims was to evaluate if despite ICDAS training, the inter and intra-rater agreement depends on the examiner’s experience. This objective was chosen as a groundwork procedure for students and early career dentists’ participation in the validation steps for training AI models for automatic ICDAS-based DMF-S calculation.
- -
- The single-center design provided uniform conditions for examination and access to identical equipment for all raters. Also, in order to minimize ICDAS training variability as a potential source of bias, the training was provided hands-on by the same team of two university lecturers, both of whom are ICDAS-validated trainers.
- -
- The Agency for Healthcare Research and Quality highlights that recall bias is a function of time, and the likelihood of forgetting previous diagnostic experiences increases as the interval between events and evaluation lengthens, especially for less memorable or less impactful findings. While no specific optimal interval is universally established for intraoral scan studies, intervals of several weeks to months are supported by the general principles of minimizing recall bias in diagnostic research [48].
- -
- The low number of tooth-colored dental restorations led to k = 1. We consider that it is realistic for experienced dentists to identify restorations on 3D virtual models, but the fact that early career dental professionals incorrectly rated some of the tooth-colored dental fillings means it can still be an important challenge, for example, to train AI models for automatic dental examination and caries susceptibility assessment. At least the preliminary validation has to be performed by experienced dentists.
- -
- DIAGNOdent exhibits limited reliability in detecting secondary caries due to moderate sensitivity, low accuracy for posterior teeth, and a high risk of false positives, making it suitable only as a supplementary diagnostic aid [49].
- -
- A possible limitation of ICDAS, resulting from systematic reviews and meta-analyses, is that ICDAS is more accurate for secondary caries detection adjacent to composite restorations than amalgam [50]. However, we addressed this possible issue, including only patients without amalgam restorations.
4.2. Future Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 3D | Three-Dimensional |
| AI | Artificial Intelligence |
| CBCT | Cone-Beam Computed Tomography |
| DMFs | Decayed, Missing, and Filled Surfaces |
| EQUATOR | Enhancing the QUAlity and Transparency Of health Research |
| ICDAS | International Caries Detection and Assessment System |
| IOS | Intraoral scanning |
| LF | Laser Fluorescence technique (DIAGNODent 2095 (LF), KaVo, Biberach, Germany) |
| PABAK | Prevalence and biased adjusted kappa |
| STROBE | STrengthening the Reporting of OBservational studies in Epidemiology |
| VR | Virtual Reality |
| WHO | World Health Organization |
References
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet. 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Al Saffan, A. Current Approaches to Diagnosis of Early Proximal Carious Lesion: A Literature Review. Cureus 2023, 15, e43489. [Google Scholar] [CrossRef]
- Abrams, T.; Abrams, S.; Sivagurunathan, K.; Moravan, V.; Hellen, W.; Elman, G.; Amaechi, B.; Mandelis, A. Detection of Caries Around Resin-Modified Glass Ionomer and Compomer Restorations Using Four Different Modalities In Vitro. Dent. J. 2018, 6, 47. [Google Scholar] [CrossRef]
- Fatiny, F.I.; Alyahya, F.; Alfuways, F. Secondary caries formation in aged restorations: A clinical review. Int. J. Community Med. Public Health 2025, 12, 4242–4246. [Google Scholar] [CrossRef]
- Magalhães, C.; Freitas, A.; Moreira, A.; Ferreira, E. Validity of staining and marginal ditching as criteria for diagnosis of secondary caries around occlusal amalgam restorations: An in vitro study. Braz. Dent. J. 2009, 20, 307–313. [Google Scholar] [CrossRef]
- Ismail, A.I.; Sohn, W.; Tellez, M.; Amaya, A.; Sen, A.; Hasson, H.; Pitts, N.B. The International Caries Detection and Assessment System (ICDAS): An integrated system for measuring dental caries. Community Dent. Oral Epidemiol. 2007, 35, 170–178. [Google Scholar] [CrossRef]
- Pitts, N.B.; Banerjee, A.; Mazevet, M.E.; Goffin, G.; Martignon, S. From ‘ICDAS’ to ‘CariesCare International’: The 20-year journey building international consensus to take caries evidence into clinical practice. Br. Dent. J. 2021, 231, 769–774. [Google Scholar] [CrossRef]
- Parolia, A.; Toh, C.G.; Seow, L.; Bhatia, S.; Smales, F. Evaluating Interfaculty Agreement in ICDAS Coding Between Restorative and Nonrestorative Dentists Using Photographic and Extracted Carious Samples: A Pilot Study. Eur. J. Dent. Educ. 2025; ahead of print. [Google Scholar]
- Nokhbatolfoghahaei, H.; Khasi, M.; Chiniforush, N.; Khoei, F.; Safavi, N.; Zadeh, B. Evaluation of Accuracy of DIAGNOdent in Diagnosis of Primary and Secondary Caries in Comparison to Conven-tional Methods. J. Lasers Med. Sci. 2013, 4, 159–167. [Google Scholar]
- Abrams, S.; Sivagurunathan, K.; Silvertown, J.; Wong, B.; Hellen, A.; Mandelis, A.; Hellen, W.M.; Elman, G.I.; Mathew, S.; Mensinkai, P.K.; et al. Correlation with Caries Lesion Depth of The Canary System, DIAGNOdent and ICDAS II. Open Dent. J. 2017, 11, 679–689. [Google Scholar] [CrossRef] [PubMed]
- Abrams, T.; Abrams, S.; Sivagurunathan, K.; Silvertown, J.; Hellen, W.M.P.; Elman, G.; Amaechi, B.T. In Vitro Detection of Caries Around Amalgam Restorations Using Four Different Modalities. Open Dent. J. 2017, 11, 609–620. [Google Scholar] [CrossRef] [PubMed]
- Galuscan, A.; Doris Fratila, A.; Jumanca, D. Caries Management Aided by Fluorescence-Based Devices. In Dental Caries—The Selection of Restoration Methods and Restorative Materials; Rusu, L.C., Ardelean, L.C., Eds.; IntechOpen: London, UK, 2022. [Google Scholar] [CrossRef]
- Slimani, A.; Terrer, E.; Manton, D.J.; Tassery, H. Detection and Diagnosis of Carious Lesions: Factual Clinical Approaches. In Evidence-Based Caries Prevention; Eden, E., Ed.; Springer Nature: Cham, Switzerland, 2025; pp. 23–46. [Google Scholar] [CrossRef]
- Michou, S.; Lambach, M.S.; Ntovas, P.; Benetti, A.R.; Bakhshandeh, A.; Rahiotis, C.; Ekstrand, K.R.; Vannahme, C. Automated caries detection in vivo using a 3D intraoral scanner. Sci. Rep. 2021, 11, 21276. [Google Scholar] [CrossRef]
- Michou, S.; Vannahme, C.; Bakhshandeh, A.; Ekstrand, K.R.; Benetti, A.R. Intraoral scanner featuring transillumination for proximal caries detection. An in vitro validation study on permanent posterior teeth. J. Dent. 2022, 116, 103841. [Google Scholar] [CrossRef]
- Zhang, J.; Huang, Z.; Cai, Y.; Luan, Q. Digital assessment of gingiva morphological changes and related factors after initial periodontal therapy. J. Oral Sci. 2021, 63, 59–64. [Google Scholar] [CrossRef]
- O’Toole, S.; Bartlett, D.; Keeling, A.; McBride, J.; Bernabé, E.; Crins, L.; Loomans, B. The influence of scanner precision and analysis software on quantifying 3D intraoral changes: Two-factor factorial experimental design. J. Med. Internet Res. 2020, 22, e17150. [Google Scholar] [CrossRef] [PubMed]
- İlisulu, S.C.; Birant, S.; Kasimoglu, Y.; Koruyucu, M.; Tuna İnce, E.B.; Seymen, F. Clinical assessment of deleterious oral habits and dental caries–periodontal parameters among Turkish twins. J. Dent. Sci. 2023, 18, 1859–1866. [Google Scholar] [CrossRef]
- Ataol, A.; Ergun, G. Prevalence and awareness levels of color blindness among students of faculty of dentistry and dental prosthesis technology program. Eur. Oral Res. 2022, 56, 149–157. [Google Scholar] [CrossRef]
- Chou, R.; Bougatsos, C.; Griffin, J.; Selph, S.S.; Ahmed, A.; Fu, R.; Nix, C.; Schwarz, E. Screening, Referral, Behavioral Counseling, and Preventive Interventions for Oral Health in Children and Adolescents Aged 5 to 17 Years: A Systematic Review for the US Preventive Services Task Force. JAMA 2023, 330, 1674–1686. [Google Scholar] [CrossRef]
- US Preventive Services Task Force; Davidson, K.W.; Barry, M.J.; Mangione, C.M.; Cabana, M.; Caughey, A.B.; Davis, E.M.; Donahue, K.E.; Doubeni, C.A.; Kubik, M.; et al. Screening and Interventions to Prevent Dental Caries in Children Younger Than 5 Years: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2021, 326, 2179–2192. [Google Scholar]
- Çelik, B.; Çelik, M.E. Automated detection of dental restorations using deep learning on panoramic radiographs. Dentomaxillofac. Radiol. 2022, 51, 20220244. [Google Scholar] [CrossRef]
- Abdalla-Aslan, R.; Yeshua, T.; Kabla, D.; Leichter, I.; Nadler, C. An artificial intelligence system using machine-learning for automatic detection and classification of dental restorations in panoramic radiography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 130, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Bonfanti-Gris, M.; Garcia-Cañas, A.; Alonso-Calvo, R.; Salido Rodriguez-Manzaneque, M.P.; Pradies Ramiro, G. Evaluation of an Artificial Intelligence web-based software to detect and classify dental structures and treatments in panoramic radiographs. J. Dent. 2022, 126, 104301. [Google Scholar] [CrossRef]
- Yüksel, A.E.; Gültekin, S.; Simsar, E.; Özdemir, Ş.D.; Gündoğar, M.; Tokgöz, S.B.; Hamamcı, İ.E. Dental enumeration and multiple treatment detection on panoramic X-rays using deep learning. Sci. Rep. 2021, 11, 12342. [Google Scholar] [CrossRef] [PubMed]
- Bumann, E.E.; Al-Qarni, S.; Chandrashekar, G.; Sabzian, R.; Bohaty, B.; Lee, Y. A novel collaborative learning model for mixed dentition and fillings segmentation in panoramic radiographs. J. Dent. 2024, 140, 104779. [Google Scholar] [CrossRef]
- De Angelis, F.; Pranno, N.; Franchina, A.; Di Carlo, S.; Brauner, E.; Ferri, A.; Pellegrino, G.; Grecchi, E.; Goker, F.; Stefanelli, L.V. Artificial Intelligence: A New Diagnostic Software in Dentistry: A Preliminary Performance Diagnostic Study. Int. J. Environ. Res. Public Health 2022, 19, 1728. [Google Scholar] [CrossRef] [PubMed]
- Cao, L.; van Nistelrooij, N.; Chaves, E.T.; Bergé, S.; Cenci, M.S.; Xi, T.; Loomans, B.; Vinayahalingam, S. Automated chart filing on bitewings using deep learning: Enhancing clinical diagnosis in a multi-center study. J. Dent. 2025, 161, 105919. [Google Scholar] [CrossRef]
- Fontenele, R.C.; Gerhardt, M.d.N.; Pinto, J.C.; Van Gerven, A.; Willems, H.; Jacobs, R.; Freitas, D.Q. Influence of dental fillings and tooth type on the performance of a novel artificial intelligence-driven tool for automatic tooth segmentation on CBCT images—A validation study. J. Dent. 2022, 119, 104069. [Google Scholar] [CrossRef]
- Schwendicke, F.; Samek, W.; Krois, J. Artificial Intelligence in Dentistry: Chances and Challenges. J. Dent. Res. 2020, 99, 769–774. [Google Scholar] [CrossRef]
- Shan, T.; Tay, F.R.; Gu, L. Application of Artificial Intelligence in Dentistry. J. Dent. Res. 2021, 100, 232–244. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Nozaki, K.; Gonda, T.; Mameno, T.; Ikebe, K. Deep learning-based detection of dental prostheses and restorations. Sci. Rep. 2021, 11, 1960. [Google Scholar] [CrossRef]
- Li, M.; Gao, Q.; Yu, T. Kappa statistic considerations in evaluating inter-rater reliability between two raters: Which, when and context matters. BMC Cancer 2023, 23, 799. [Google Scholar] [CrossRef]
- ElSalhy, M.; Ali, U.; Lai, H.; Flores-Mir, C.; Amin, M. Caries reporting in studies that used the International Caries Detection and Assessment System: A scoping review. Community Dent. Oral Epidemiol. 2019, 47, 92–102. [Google Scholar] [CrossRef]
- Perkins, S.M. Statistical Inference on Categorical Variables. In Topics in Biostatistics; Ambrosius, W.T., Ed.; Humana Press: Totowa, NJ, USA, 2007; pp. 73–88. [Google Scholar] [CrossRef]
- Vetter, T.R. Fundamentals of Research Data and Variables: The Devil Is in the Details. Anesth. Analg. 2017, 125, 1375–1380. [Google Scholar] [CrossRef]
- The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies|EQUATOR Network. Available online: https://www.equator-network.org/reporting-guidelines/strobe/ (accessed on 9 November 2025).
- Lang, T.A.; Altman, D.G. Basic statistical reporting for articles published in Biomedical Journals: The “Statistical Analyses and Methods in the Published Literature” or the SAMPL Guidelines. Int. J. Nurs. Stud. 2015, 52, 5–9. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023. [Google Scholar]
- Porumb (Chifor), I.; Leucuta, D.C.; Nigoghossian, M.; Culic, B.; Lucaciu, P.O.; Culic, C.; Lucaciu, P.O.; Culic, C.; Badea, I.C.; Leghezeu, A.-N.; et al. Caries Lesion Assessment Using 3D Virtual Models by Examiners with Different Degrees of Clinical Experience. Medicina 2023, 59, 2157. [Google Scholar] [CrossRef]
- Timme, M.; Bender, J.; Steffens, L.; Shay, D.; Schmeling, A. Third Molar Eruption in Dental Panoramic Radiographs as a Feature for Forensic Age Assessment—Presentation of a New Non-Staging Method Based on Measurements. Biology 2023, 12, 1403. [Google Scholar] [CrossRef]
- Byju, M.; Mala, K.; Natarajan, S.; Thomas, M.S.; Parolia, A. Comparing the effectiveness of an e-learning module at different levels of magnification for detecting occlusal caries in permanent teeth, utilizing the international caries detection and assessment system (ICDAS): An ex vivo study. BDJ Open 2025, 11, 43. [Google Scholar] [CrossRef]
- Guo, J.; Lu, Y.; Li, R.; Zhou, K.; Ge, R.; Zhao, D.; Xia, S.; Wang, Y. Influence of repeated cut-off and rescanning on the trueness of the intraoral digital scans. J. Dent. 2024, 150, 105153. [Google Scholar] [CrossRef]
- Revilla-León, M.; Sicilia, E.; Agustín-Panadero, R.; Gómez-Polo, M.; Kois, J.C. Clinical evaluation of the effects of cutting off, overlapping, and rescanning procedures on intraoral scanning accuracy. J. Prosthet. Dent. 2023, 130, 746–754. [Google Scholar] [CrossRef]
- Revilla-León, M.; Quesada-Olmo, N.; Gómez-Polo, M.; Sicilia, E.; Farjas-Abadia, M.; Kois, J.C. Influence of rescanning mesh holes on the accuracy of an intraoral scanner: An in vivo study. J. Dent. 2021, 115, 103851. [Google Scholar] [CrossRef]
- Oh, K.C.; Park, J.M.; Moon, H.S. Effects of Scanning Strategy and Scanner Type on the Accuracy of Intraoral Scans: A New Approach for Assessing the Accuracy of Scanned Data. J. Prosthodont. 2020, 29, 518–523. [Google Scholar] [CrossRef]
- An, H.; Langas, E.E.; Gill, A.S. Effect of scanning speed, scanning pattern, and tip size on the accuracy of intraoral digital scans. J. Prosthet. Dent. 2024, 131, 1160–1167. [Google Scholar] [CrossRef]
- Schlesinger, M.; Grob, R.; Gleason, K.; Yuan, C.; Haskell, H.; Giardina, T.; McDonald, K. Patient Experience as a Source for Understanding the Origins, Impact, and Remediation of Diagnostic Errors. Agency for Healthcare Research and Quality; 2023 July. Report No.: Volume 2, Eliciting Patient Narratives. Available online: https://www.ahrq.gov/sites/default/files/wysiwyg/topics/dxsafety-patient-experience-vol2.pdf (accessed on 14 November 2025).
- Ku, J.C.K.; Lam, W.Y.H.; Li, K.Y.; Hsung, R.T.C.; Chu, C.H.; Yu, O.Y. Accuracy of detection methods for secondary caries around direct restorations: A systematic review and meta-analysis. J. Dent. 2025, 153, 105541. [Google Scholar] [CrossRef]
- Brouwer, F.; Askar, H.; Paris, S.; Schwendicke, F. Detecting Secondary Caries Lesions: A Systematic Review and Meta-analysis. J. Dent. Res. 2016, 95, 143–151. [Google Scholar] [CrossRef]
- Haug, S.R.; Virtej, A.; Sunde, P.T.; Fristad, I. Ethical considerations and legal allegations in endodontic practice. Eur. J. Oral Sci. 2025, e70043. [Google Scholar] [CrossRef]
- Medit i700 Wireless Intraoral Scanner Review + Medit Apps. Available online: https://instituteofdigitaldentistry.com/cad-cam/medit/medit-i700-wireless-intraoral-scanner-review/?srsltid=AfmBOorsgzBbJyhou2x4-Fj-5mbjBpc8ihaGJzFIjoeUOGP9vXURwWh0 (accessed on 10 November 2025).
- Schulz-Weidner, N.; Gruber, M.; Wöstmann, B.; Uebereck, C.F.; Krämer, N.; Schlenz, M.A. Occlusal Caries Detection with Intraoral Scanners in Pediatric Dentistry: A Comparative Clinical Study. J. Clin. Med. 2024, 13, 925. [Google Scholar] [CrossRef]
- Al-Yaseen, W.; Haghi Ashtiani, G.; Pattinson, R.; Pritchard, M.F.; Pickles, T.; Galloway, J.; Innes, N. Picture perfect: Study protocol for assessing the accuracy, feasibility and acceptability of intraoral photographs captured by parents for remote dental screening in children—An observational mixed-methods study. BMJ Open 2025, 15, e104769. [Google Scholar] [CrossRef]
- Grischke, J.; Johannsmeier, L.; Eich, L.; Griga, L.; Haddadin, S. Dentronics: Towards robotics and artificial intelligence in dentistry. Dent. Mater. 2020, 36, 765–778. [Google Scholar] [CrossRef]
- Liang, Y.; Li, D.; Deng, D.; Chu, C.H.; Mei, M.L.; Li, Y.; Yu, N.; He, J.; Cheng, L. AI-Driven Dental Caries Management Strategies: From Clinical Practice to Professional Education and Public Self Care. Int. Dent. J. 2025, 75, 100827. [Google Scholar] [CrossRef]
- Park, J.W.; Lim, Y.J.; Lim, B.S.; Baek, Y.W. Comparison of accuracy of three intraoral scanners for different types of tooth preparations: A laboratory study. Am. J. Dent. 2025, 38, 196–200. [Google Scholar]
- Park, J.M.; Kim, R.J.Y.; Lee, K.W. Comparative reproducibility analysis of 6 intraoral scanners used on complex intracoronal preparations. J. Prosthet. Dent. 2020, 123, 113–120. [Google Scholar] [CrossRef]
- Oh, H.S.; Lim, Y.J.; Kim, B.; Kim, M.J.; Kwon, H.B.; Baek, Y.W. Effect of scanning-aid agents on the scanning accuracy in specially designed metallic models: A laboratory study. PLoS ONE 2022, 17, e0267742. [Google Scholar] [CrossRef]
- Michelinakis, G.; Apostolakis, D.; Tsagarakis, A.; Lampropoulos, P. Influence of different material substrates on the accuracy of 3 intraoral scanners: A single-blinded in vitro study. Int. J. Prosthodont. 2022, 35, 82–93. [Google Scholar] [CrossRef]
- Rotondi, M.A.; Donner, A. A confidence interval approach to sample size estimation for interobserver agreement studies with multiple raters and outcomes. J. Clin. Epidemiol. 2012, 65, 778–784. [Google Scholar] [CrossRef]
- Shan, G.; Wang, W. Exact one-sided confidence limits for Cohen’s kappa as a measurement of agreement. Stat. Methods Med. Res. 2017, 26, 615–632. [Google Scholar] [CrossRef]
- Giraudeau, B.; Mary, J.Y. Planning a reproducibility study: How many subjects and how many replicates per subject for an expected width of the 95 per cent confidence interval of the intraclass correlation coefficient. Stat. Med. 2001, 20, 3205–3214. [Google Scholar] [CrossRef]
- Schober, P.; Mascha, E.J.; Vetter, T.R. Statistics From A (Agreement) to Z (z Score): A Guide to Interpreting Common Measures of Association, Agreement, Diagnostic Accuracy, Effect Size, Heterogeneity, and Reliability in Medical Research. Anesth. Analg. 2021, 133, 1633–1641. [Google Scholar] [CrossRef]
| Observations | Number of Observations | Cohen’s Kappa Weighted | 95% CI | p-Value | PABAK 95% CI |
|---|---|---|---|---|---|
| All teeth | 288 | 1 | (1–1) | <0.001 | 1 (0.975–1) |
| Anterior teeth | 104 | 1 | (1–1) | <0.001 | 1 (0.93–1) |
| Posterior teeth | 184 | 1 | (1–1) | <0.001 | 1 (0.96–1) |
| Pits and fissures | 64 | 1 | (1–1) | <0.001 | 1 (0.888–1) |
| Smooth surface | 224 | 1 | (1–1) | <0.001 | 1 (0.967–1) |
| Observations | Number of Observations | Cohen’s Kappa Weighted | 95% CI | p-Value | PABAK 95% CI |
|---|---|---|---|---|---|
| All teeth | 288 | 1 | (1–1) | <0.001 | 1 (0.975–1) |
| Anterior teeth | 104 | 1 | (1–1) | <0.001 | 1 (0.93–1) |
| Posterior teeth | 184 | 1 | (1–1) | <0.001 | 1 (0.96–1) |
| Pits and fissures | 64 | 1 | (1–1) | <0.001 | 1 (0.888–1) |
| Smooth surface | 224 | 1 | (1–1) | <0.001 | 1 (0.967–1) |
| Observations | Number of Observations | Cohen’s Kappa Weighted | 95% CI | p-Value | PABAK 95% CI |
|---|---|---|---|---|---|
| All teeth | 144 | 0.252 | −0.195–0.699 | 0.269 | 0.861 (0.752–0.932) |
| Anterior teeth | 52 | 0.381 | −0.299–1.061 | 0.272 | 0.885 (0.681–0.976) |
| Posterior teeth | 92 | 0.183 | −0.399–0.765 | 0.538 | 0.848 (0.699–0.938 |
| Pits and fissures | 32 | 0.2 | −0.444–0.844 | 0.543 | 0.688 (0.344–0.894) |
| Smooth surface | 112 | 0.275 | −0.347–0.896 | 0.386 | 0.911 (0.798–0.971) |
| Observations | Number Observations | Cohen’s Kappa Weighted | 95% CI | p-Value | PABAK 95% CI |
|---|---|---|---|---|---|
| All teeth | 144 | 0.277 | −0.181–0.734 | 0.236 | 0.875 (0.769–0.942) |
| Anterior teeth | 52 | −0.026 | −1.154–1.101 | 0.964 | 0.885 (0.681–0.976) |
| Posterior teeth | 92 | 0.367 | −0.123–0.857 | 0.142 | 0.87 (0.727–0.951) |
| Pits and fissures | 32 | 0.355 | −0.165–0.874 | 0.181 | 0.688 (0.344–0.894) |
| Smooth surface | 112 | −0.014 | −0.989–0.962 | 0.978 | 0.929 (95% CI 0.822–0.98) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nigoghossian, M.; Simu, M.-R.; Culic, B.; Sava, S.; Bouteiller, H.; Culic, C.; Badea, I.C.; Lucaciu, O.P.; Ilea, A.; Porumb, I. The Influence of Examiner Experience on Inter- and Intra-Rater Agreement in Dental Restorations Identification on Three-Dimensional Digital Models. Medicina 2025, 61, 2135. https://doi.org/10.3390/medicina61122135
Nigoghossian M, Simu M-R, Culic B, Sava S, Bouteiller H, Culic C, Badea IC, Lucaciu OP, Ilea A, Porumb I. The Influence of Examiner Experience on Inter- and Intra-Rater Agreement in Dental Restorations Identification on Three-Dimensional Digital Models. Medicina. 2025; 61(12):2135. https://doi.org/10.3390/medicina61122135
Chicago/Turabian StyleNigoghossian, Marion, Meda-Romana Simu, Bogdan Culic, Sorina Sava, Henri Bouteiller, Carina Culic, Iulia Clara Badea, Ondine Patricia Lucaciu, Aranka Ilea, and Ioana Porumb. 2025. "The Influence of Examiner Experience on Inter- and Intra-Rater Agreement in Dental Restorations Identification on Three-Dimensional Digital Models" Medicina 61, no. 12: 2135. https://doi.org/10.3390/medicina61122135
APA StyleNigoghossian, M., Simu, M.-R., Culic, B., Sava, S., Bouteiller, H., Culic, C., Badea, I. C., Lucaciu, O. P., Ilea, A., & Porumb, I. (2025). The Influence of Examiner Experience on Inter- and Intra-Rater Agreement in Dental Restorations Identification on Three-Dimensional Digital Models. Medicina, 61(12), 2135. https://doi.org/10.3390/medicina61122135








