1. Introduction
Cystic fibrosis [CF, Online Mendelian Inheritance in Man (OMIM) no. 219700] is a rare autosomal recessive genetic disease characterized by exocrine gland dysfunction and multisystem involvement, primarily affecting the respiratory and digestive tracts [
1,
2,
3]. It results from pathogenic variants in the
CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) gene [
4,
5,
6,
7]. The
CFTR gene encodes an Adenosine Triphosphate (ATP)-dependent ion channel protein that is essential for chloride and bicarbonate transport across epithelial surfaces. Alterations in this protein impair the ionic and water homeostasis of secretions, leading to the production of thick and viscous mucus [
6,
8,
9,
10]. This dysfunction promotes, for instance, airway obstruction, persistent bacterial colonization, and chronic inflammation—key factors in the pathophysiology and progression of CF [
4,
5,
6,
11,
12].
The average incidence of CF in Brazil is estimated at 1 in 10,000 live births, being more prevalent among individuals of European ancestry [
13]. In Latin America, recent studies report prevalence rates ranging from 1 in 8000 to 1 in 10,000, reflecting the region’s genetic diversity [
14]. With the advancement of newborn screening programs, many cases have been diagnosed earlier, enabling prompt clinical interventions [
4,
6,
8,
13,
15]. Pulmonary involvement remains the leading cause of morbidity and mortality in CF, characterized by progressive decline in respiratory function, recurrent infections, and acute exacerbations that often require hospitalization—highlighting the importance of individualized clinical management strategies [
9,
16]. In recent years, however, the introduction of CFTR modulators has revolutionized disease management, leading to significant improvements in pulmonary function, nutritional status, and overall survival [
10,
17]. Nevertheless, clinical variability among individuals carrying identical genotypes continues to represent a major challenge [
18,
19,
20].
Despite therapeutic advances and the significant improvement in the prognosis of CF, pulmonary complications remain the leading cause of morbidity and mortality among patients [
13,
17,
19,
20,
21]. In this context, comprehensive assessment of pulmonary function is essential for early diagnosis, clinical severity stratification, and the development of individualized therapeutic strategies [
6,
9,
10,
21].
Recent studies have demonstrated that the clinical heterogeneity observed in CF cannot be explained solely by
CFTR genotype [
22,
23,
24]. Growing evidence indicates that this variability arises, in part, from the interaction between environmental factors and the action of modifier genes, which can modulate the phenotypic expression of the disease [
25,
26]. These genes do not directly alter the primary
CFTR mutation but influence the clinical course, affecting the severity of pulmonary involvement, the inflammatory response, susceptibility to respiratory infections, and even therapeutic responsiveness [
20,
27]. Understanding this complex genetic landscape is crucial to elucidate the mechanisms underlying disease progression and identify potential targets for personalized therapies [
18,
19,
27,
28,
29,
30,
31,
32,
33]. Among the most extensively studied modifier genes is
ADAM33 (A Disintegrin and Metalloproteinase Domain 33), located on chromosome 20p13. This gene encodes a metalloproteinase expressed in fibroblasts and bronchial smooth muscle cells, involved in airway remodeling, cell proliferation, adhesion, and inflammation, playing a significant role in chronic respiratory diseases [
34,
35].
Variants of the
ADAM33 gene have been widely associated with bronchial hyperresponsiveness, persistent inflammation, and a progressive decline in lung function in respiratory diseases such as asthma [
34,
36]. Among these, the rs2280091 (NC_000020.11:3669586:A>G) variant has received particular attention due to its association with altered pulmonary function, increased airway inflammation, and airflow obstruction in individuals with asthma [
35,
36,
37]. However, its role in CF remains under investigation. Considering that the pathophysiology of CF also involves chronic inflammation and pulmonary remodeling, it is relevant to explore the potential contribution of this variant to the clinical heterogeneity of the disease [
34,
38,
39].
Understanding the influence of ADAM33, particularly the rs2280091 variant, on lung function in patients with CF may provide valuable insights into the genetic mechanisms underlying phenotypic modulation. This analysis opens new perspectives for patient stratification based on genetic profiles, enabling the development of more effective and targeted therapeutic approaches. Thus, the rs2280091 variant emerges as a potential target for personalized interventions in the management of CF.
3. Discussion
This study evaluated the frequency and impact of the rs2280091 variant of the
ADAM33 gene on pulmonary function in 55 patients with CF treated at a Brazilian referral center and compared them with 608 individuals without CF from the Online Archive of Brazilian Mutations (ABraOM) database [
40]. The study population consisted predominantly of young female participants of self-declared Caucasian ethnicity, with low body weight and height, and showed marked heterogeneity in
CFTR genotypes, with F508del/F508del being the most frequent. With respect to
ADAM33 rs2280091 distribution, the AA genotype was the most prevalent in both groups; however, the GG genotype demonstrated the highest statistical relevance by occurring disproportionately more often in CF patients than in the controls. Importantly, the rs2280091 variant deviated from Hardy–Weinberg equilibrium in the CF group, which may reflect recruitment-related factors or a survivor effect, rather than a true disease-association signal. Carriers of the G allele showed higher spirometric values, especially in indices reflecting peripheral airway flow, indicating a possible influence of this allele on airflow dynamics and bronchodilator responsiveness. These findings support the potential role for
ADAM33 rs2280091 as a modifier gene contributing to phenotypic variability in CF while emphasizing the need to interpret allele frequency shifts within the context of Hardy–Weinberg equilibrium deviation.
An important factor contributing to the heterogeneity of pulmonary function in patients with CF is environmental exposure [
43]. Although air pollution was not directly assessed in this study, previous research has demonstrated that external environmental factors can modify airway inflammation and clinical outcomes in CF. For example, in a cohort of 11,484 patients, Goss et al. (2004) reported that a 10 μg/m
3 increase in particulate matter was associated with an 8% higher likelihood (95% CI: 2–15%) of experiencing more than two pulmonary exacerbations per year [
44], underscoring that airway function in CF is influenced not only by genetic background but also by environmental burden. This supports the rationale for considering both intrinsic factors, such as
ADAM33 variation, and external exposures when interpreting pulmonary phenotypes in CF.
Also, among the possible reasons for the differences observed in pulmonary function and clinical severity among patients with CF, the genetic variability of
CFTR mutations stands out [
25,
45,
46,
47]. In some populations, such as the Brazilian one, this variability is remarkably extensive [
12,
45,
48,
49]. Pereira and colleagues (2019) identified 63 variants—classified into seven distinct groups and 77 different genotypes—in a sample of 169 patients with CF [
50]. Some of these variants were not listed in the databases of the CFF or the REBRAFC, highlighting the considerable genotypic heterogeneity of the disease and the potential underreporting of specific genotypes [
50]. In addition to the analysis of pathogenic
CFTR variants, recent studies have emphasized the role of modifier genes in determining the clinical phenotype of CF [
22,
23,
24,
26,
38,
51]. In this context, our findings support that the rs2280091 variant of
ADAM33 may act as one such modifier, helping explain differences in pulmonary function even among individuals with similar
CFTR genotypes.
Among the modifier genes associated with CF, several have been investigated for their potential influence on disease severity [
22,
52,
53,
54,
55,
56,
57,
58,
59]. These include members of the
SLC family (
Solute Carrier family), which encode membrane transport proteins responsible for ion and metabolite transport, thus influencing ionic homeostasis and acid–base balance [
60,
61,
62];
ACE2 (
Angiotensin-Converting Enzyme 2), which regulates blood pressure, modulates inflammation, and provides epithelial protection in the lungs [
63];
GSH (
Glutathione synthetase), a key enzyme in glutathione synthesis, the major intracellular antioxidant [
64,
65];
GCLC (
Glutamate–Cysteine Ligase Catalytic Subunit), the catalytic subunit of the rate-limiting enzyme in glutathione biosynthesis, essential for maintaining redox balance [
64,
65];
ADRB2 (
Adrenoceptor Beta 2), a β
2-adrenergic receptor involved in bronchodilation and airway inflammation control [
66];
ADIPOQ (
Adiponectin, C1Q And Collagen Domain Containing), a protein with anti-inflammatory and metabolic regulatory effects [
67];
STATH (
Statherin), a salivary protein with antimicrobial properties that contributes to epithelial homeostasis [
67];
TNF-α (
Tumor Necrosis Factor Alpha), a pro-inflammatory cytokine central to immune regulation and chronic airway inflammation [
68];
TCF7L2 (
Transcription Factor 7 Like 2), a transcription factor participating in the Wnt/β-catenin signaling pathway and glucose metabolism [
69];
IL8 (
Interleukin 8), a chemokine that mediates neutrophil recruitment and activation in the airways [
70,
71];
MUC4 and
MUC20 (
Mucin 4 and
Mucin 20), mucin glycoproteins that contribute to mucus composition and epithelial protection [
72];
EHF (
ETS Homologous Factor), an epithelial transcription factor involved in cell differentiation and inflammatory regulation [
72]; and
CEP72 (
Centrosomal Protein 72), a centrosomal component critical for microtubule organization and ciliary function [
72]. Although this list illustrates the diversity of modifier pathways described in CF, it is not exhaustive, and several comprehensive reviews have synthesized the expanding landscape of CF modifier genes in recent years.
This context is directly aligned with the subsequent discussion in this study, in which the rs2280091 variant of ADAM33 was evaluated as a potential modifier gene. Pulmonary function in CF reflects a complex interplay between CFTR mutations, secondary modifier loci, and environmental drivers, and the associations observed in our cohort suggest that ADAM33 variation may help explain functional heterogeneity even among patients carrying similar CFTR genotypes. Subsequent paragraphs expand on this relationship and position ADAM33 within the broader mechanistic framework of airway remodeling, inflammation, and differential pulmonary function trajectories in CF.
Pulmonary function in CF is shaped by complex interactions between genetic and environmental factors.
CFTR mutations, such as F508del, drive disease severity by promoting chronic inflammation and mucus accumulation in the airways [
6,
45]. Modifier genes, including
ADAM33, may influence disease progression by regulating tissue remodeling and inflammatory processes, while environmental factors such as recurrent infections and pollutants further modulate these effects [
24,
25,
26,
44,
72].
ADAM33 has emerged as a key modifier gene implicated in airway remodeling, tissue repair, and inflammatory processes [
34]. Variants in
ADAM33 have been associated with altered bronchial reactivity and progressive pulmonary function decline [
34,
73,
74], suggesting a potential role in modulating the respiratory phenotype of patients with CF.
The
ADAM33 gene, a member of the transmembrane glycoprotein family known as A Disintegrin and Metalloproteinases (ADAMs), plays a pivotal role in biological processes such as cell adhesion, proteolysis, and extracellular matrix remodeling, making it relevant in the pathophysiology of various inflammatory and proliferative diseases [
75,
76]. Initially identified as an asthma susceptibility gene [
76,
77,
78,
79],
ADAM33 is expressed in vascular smooth muscle cells and tissues including the lungs, where it contributes to airway remodeling, angiogenesis, and chronic inflammation, for instance, in cases of allergic rhinitis [
80,
81]. Studies on nasal polyposis have shown that its upregulated expression in epithelial and mesenchymal cells suggests a pathogenic role, with potential implications in allergies and drug intolerances [
78,
82].
Beyond its involvement in respiratory conditions [
83],
ADAM33 has been implicated in palmar dermatoglyphic patterns and cutaneous disorders such as psoriasis and atopic dermatitis, where polymorphisms consistently associated with early onset forms suggest roles in cell adhesion and epidermal remodeling [
79,
84,
85,
86,
87,
88]. In oncological contexts,
ADAM33 expression and differential methylation have been linked to several cancers, including breast, thyroid, and gastric malignancies. It may act as a tumor suppressor in certain settings—for instance, via truncated isoforms that inhibit the oncogenic activity of the full-length protein—or alternatively promote tumor progression by enhancing cell migration, potentially through Interleukin 18 (IL-18)–mediated mechanisms [
89,
90,
91,
92,
93]. Moreover, in atherosclerosis,
ADAM33 expression in vascular lesions appears to inhibit smooth muscle cell migration, highlighting a potential protective role in vascular remodeling [
94].
The rs2280091 variant of the
ADAM33 gene, although its significance varies across populations, has been consistently linked to an increased risk of allergic and functional asthma, with the G allele correlating with greater susceptibility and pulmonary function decline [
74,
95]. Similar observations in psoriasis suggest that this variant contributes to disease progression through shared mechanisms of inflammation and tissue remodeling, highlighting its modulatory role in systemic pathological processes [
85,
86,
96]. This evidence supports the potential of
ADAM33, particularly the rs2280091 variant, as a biomarker for pulmonary function progression in respiratory conditions such as asthma and CF.
The genotypic distribution among patients with CF showed a significant deviation from Hardy–Weinberg equilibrium, a phenomenon not observed in the control group. This finding suggests that the rs2280091 variant may be subject to selective pressures within the affected population. In CF, similar deviations have been described for other modifier genes whose variants can influence survival or long-term disease trajectories. For example, polymorphisms in
STAT3 (
Signal Transducer and Activator of Transcription 3),
IL1R (
Interleukin-1 Receptor), and
TNFR1 (
Tumor Necrosis Factor Receptor 1) have previously been associated with protection against chronic airway inflammation, slower functional decline, and improved prognosis, supporting the concept that modifier loci may be enriched among individuals who survive longer or experience milder disease [
97,
98,
99].
In this context, individuals carrying the ADAM33 rs2280091 G allele could theoretically derive functional advantages—such as better preservation of small-airway flow—leading to longer survival or greater likelihood of reaching adulthood with sufficient clinical stability to be recruited into such studies. This could contribute to the deviation from the expected genotype frequencies. Importantly, such selection would operate only within the CF population and would not influence allele distribution in the general population, given the reduced fertility and shortened lifespan typically associated with CF.
Evidence suggests that the G allele of the
ADAM33 rs2280091 variant may be associated with preserved peripheral airway function in CF, potentially through modulation of tissue remodeling, extracellular matrix integrity, and smooth muscle and fibroblast proliferation. This protective effect appears to be context-specific, contrasting with findings in asthma, where the same variant has been associated with greater susceptibility and worse pulmonary function [
35,
100].
This apparent paradox may reflect fundamental physiological differences between the two conditions. In asthma, airway obstruction results primarily from hyperresponsiveness, eosinophilic inflammation, and excessive tissue remodeling, and increased ADAM33 activity may exacerbate these processes, worsening airflow limitation [
101]. In CF, however, lung pathology is heavily driven by neutrophilic inflammation, infection-mediated injury, and chronic structural damage rather than bronchial hyperreactivity [
102,
103]. In this setting, enhanced ADAM33-mediated remodeling or matrix turnover could theoretically support the structural preservation of small airways or aid tissue adaptation under chronic inflammatory stress, resulting in better spirometric performance. The distinct inflammatory microenvironments, immune pathways, and mechanisms of airway injury in asthma and CF therefore offer a plausible biological explanation for how the same
ADAM33 variant could manifest opposite clinical effects. This reinforces the importance of interpreting modifier gene effects within disease-specific context and supports the rationale for further mechanistic studies to elucidate the functional consequences of rs2280091 in CF.
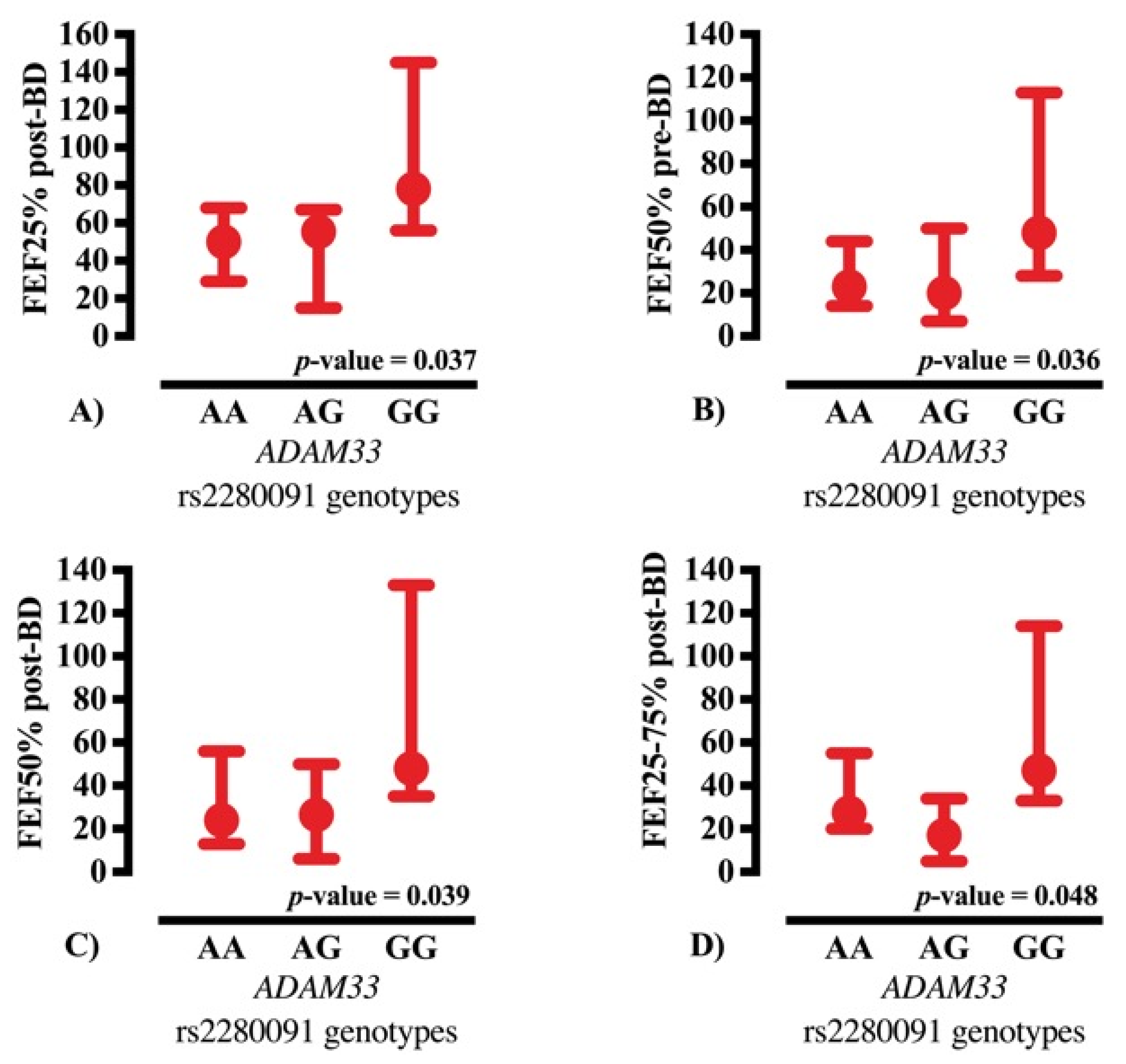
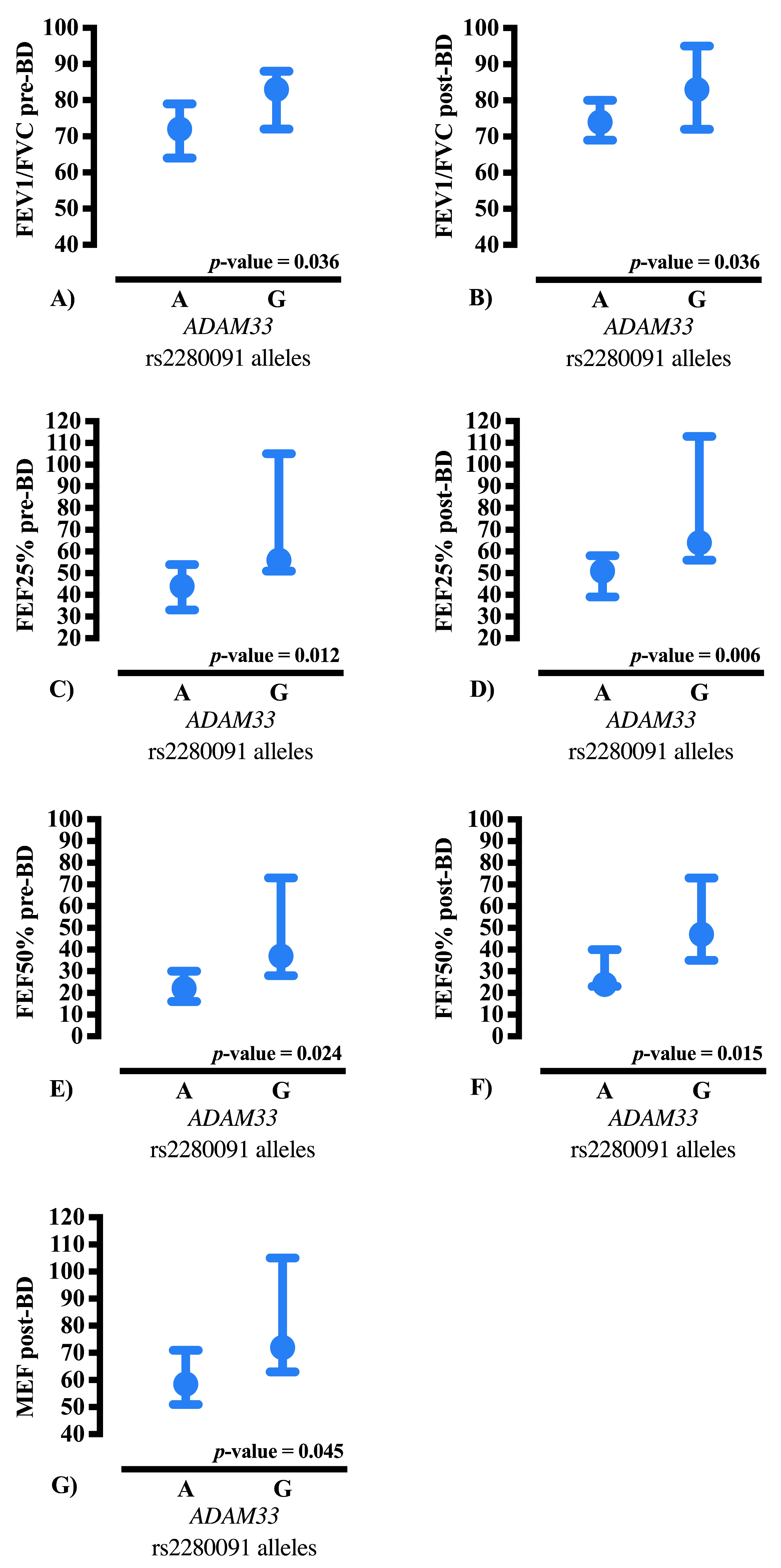
In addition, in CF, chronic activation of inflammatory pathways and viscous mucus accumulation may render G allele carriers more resilient to small airway damage, reflected in superior peripheral expiratory flow parameters, including FEF25–75%, FEF50%, and MEF, without necessarily affecting bronchodilator responsiveness. These observations support ADAM33 as a significant modifier gene in CF, influencing chronic structural and inflammatory mechanisms that contribute to the preservation of peripheral airway function.
The observed protective effect associated with the G allele of the rs2280091 variant in
ADAM33 is biologically plausible within the current understanding of the gene’s functional role in airway biology and chronic respiratory disease [
101]. Although rs2280091 is a synonymous variant and therefore does not alter the amino acid sequence of the encoded protein, its position within a transcribed region may influence post-transcriptional regulatory processes, including messenger ribonucleic acid (mRNA) stability, codon usage efficiency, or RNA secondary structure, which in turn could modulate protein expression. In addition, evidence from population genomic datasets indicates that rs2280091 is in linkage disequilibrium with other
ADAM33 variants harboring recognized functional relevance, including promoter and intronic loci capable of affecting transcription factor affinity, epigenetic remodeling, and enhancer–promoter interactions. These linked variants have previously been associated with altered expression of
ADAM33 in bronchial epithelium and with downstream phenotypes such as airway hyperresponsiveness, extracellular matrix deposition, tissue remodeling, and pro-inflammatory signaling [
101]. In the context of CF, where chronic infection and sustained inflammatory activation drive progressive airway damage, a reduction in ADAM33-mediated remodeling could contribute to attenuated disease severity, aligning with the protective directionality identified in the present analysis. Therefore, rather than representing an isolated synonymous effect, the G allele of rs2280091 may act as a genomic proxy for a wider regulatory haplotype that decreases ADAM33 functional impact in airway pathology. Future expression studies, chromatin accessibility assays, and haplotype-level fine-mapping analyses in CF cohorts are warranted to elucidate the mechanistic link between this variant and the respiratory outcomes observed.
Limitations
This study has several limitations that should be considered when interpreting the results. First, the sample size was relatively small, with a predominance of young female participants, which limits the generalizability of the findings to the broader CF population. Additionally, the cross-sectional design restricts the ability to assess longitudinal progression of pulmonary function, preventing conclusions about the long-term impact of the rs2280091 variant of ADAM33.
The lack of stratification by ethnicity and environmental factors also limits the analysis of potential gene–environment interactions, which may significantly influence disease expression. Another important consideration is that the study focused exclusively on the rs2280091 variant, not addressing potential effects of other ADAM33 variants or interactions with additional modifier genes that could modulate the pulmonary phenotype.
Another limitation of the present study is the limited characterization of asthma or asthma-like disease within the CF population. Because airway remodeling and hyperresponsiveness may overlap between CF and asthma, it is not possible to fully determine whether the observed associations with ADAM33 reflect CF-specific mechanisms or concomitant airway disease resembling asthma.
A major limitation of the study is the marked predominance of female participants in the cohort, which may limit the generalizability of the findings. Although ADAM33 is not located on a sex chromosome, sex-related differences in lung disease presentation and progression cannot be completely excluded. Future studies with more balanced sex distribution are needed to validate whether the associations observed are consistent across sexes.
Although the results indicate that carriers of the G allele, particularly GG homozygotes, exhibit relative preservation of pulmonary function, these findings should be interpreted with caution. Future longitudinal studies with larger and more heterogeneous cohorts are needed to confirm these associations and elucidate the molecular mechanisms underlying the influence of ADAM33 on the phenotypic variability observed in CF.
4. Materials and Methods
4.1. Study Population
This was a cross-sectional observational study conducted at the Hospital das Clínicas of the University of Campinas (Universidade de Campinas—Unicamp, Campinas, São Paulo, Brazil) and at the University of São Francisco (Universidade São Francisco—USF, Bragança Paulista, São Paulo, Brazil). The study protocol was approved by the Research Ethics Committee [Certificate of Presentation for Ethical Consideration (Certificado de Apresentação para Apreciação Ética—CAAE) no. 38162914.3.0000.5404], and all participants—or their legal guardians—provided written informed consent, in accordance with the Declaration of Helsinki.
A total of 55 patients CF were included. The diagnosis was established based on an abnormal sweat test (chloride ion concentration > 60 mEq/L) and confirmation of two pathogenic variants in the CFTR gene. Inclusion criteria comprised age ≥ 6 years, ability to perform reliable spirometry, and clinical stability, defined as the absence of pulmonary exacerbation in the preceding four weeks. Patients with significant comorbidities that could interfere with lung function were excluded.
For clinical characterization, demographic and anthropometric data were collected, including age (years), sex (male or female), ethnicity (White, Black, Mixed-race, or Asian), weight (kg), height (m), and BMI (calculated as kg/m
2). Additional data included history of respiratory exacerbations and spirometric measurements performed before and after bronchodilator administration, following the American Thoracic Society/European Respiratory Society (ATS/ERS) recommendations [
104].
As a control group, allele frequencies were obtained from the ABraOM database, which includes genomic data from 608 elderly (> 60 years), genetically admixed individuals residing in São Paulo, representing the genetic diversity of the Brazilian population, with predominant African, European, and Indigenous ancestry [
40]. ABraOM participants were healthy elderly individuals without a history of severe disease, providing an appropriate reference population for genetic comparison [
40]. The use of ABraOM as a control enables population-based comparison with a non-affected cohort, offering reference values for the rs2280091 variant frequency in the
ADAM33 gene [
40].
4.2. Pulmonary Function
Pulmonary function was assessed by spirometry before and after bronchodilator administration, strictly following the ATS/ERS (2019) standards [
104]. The following clinical markers of pulmonary function were analyzed:
1. FVC: the total volume of air exhaled with maximal effort, starting from full inspiration. It reflects the individual’s pulmonary reserve and is essential for assessing ventilatory function.
2. FEV1: the volume of air exhaled during the one second of the FVC maneuver, serving as a sensitive marker of airway obstruction.
3. FEV1/FVC ratio: expresses the proportion of air exhaled in the first second relative to the total exhaled volume; reduced values indicate airflow obstruction.
4. Forced Expiratory Flow (FEF) at 25%, 50%, and 75% of FVC (FEF25%, FEF50%, and FEF75%): reflects the mean expiratory flow at different points during exhalation, providing information about small and large airways.
5. FEF25–75%: represents the average expiratory flow between 25% and 75% of FVC, a sensitive marker of medium and small airway involvement, frequently compromised in CF.
6. Maximal Expiratory Forced flow (MEF): the highest airflow achieved during the FVC maneuver, reflecting overall airway function and serving as a sensitive marker for early airflow obstruction.
These parameters provide a comprehensive assessment of pulmonary function, enabling accurate characterization of obstruction severity and ventilatory heterogeneity among the patients studied. All spirometric values were expressed as percentages of predicted values, based on the Global Lung Function Initiative (GLI-2012) reference equations [
105].
4.3. Analysis of the rs2280091 Variant in the ADAM33 Gene
Genomic DNA was extracted from peripheral blood samples previously stored in a biorepository, following standardized preservation protocols. The single nucleotide variant (SNV) rs2280091 of the ADAM33 gene was genotyped using the Polymerase Chain Reaction-Restriction Fragment Length Polymorphism (PCR-RFLP) method. The resulting fragments were visualized on 2% agarose gels stained with SYBR® Safe DNA Gel Stain (1X) (ThermoFisher Scientific, Waltham, MA, USA). The technical details of the reaction, including primer sequences and enzyme digestion conditions, are described below.
For DNA amplification, all samples were previously quantified to ensure optimal concentrations between 50 and 500 ng/µL, thereby guaranteeing PCR efficiency. The reaction conditions were optimized for a final volume of 25 µL, containing 1 µL of genomic DNA, 0.5 µL of each primer (5 pmol), 0.75 U of Uniscience DNA Polymerase (5 U/µL), 2 mM MgCl2, 50 µM of each deoxyribonucleotide, and 1X reaction buffer containing KCl (50 mM KCl; 75 mM Tris-HCl, pH 9.0; 20 mM (NH4)2SO4). All reactions were performed in parallel with a negative (blank) control.
The amplification was carried out using a touchdown PCR protocol, as outlined in
Table 6.
Following amplification, the resulting fragments were subjected to enzymatic digestion for approximately 16 h using a PTC-100™ Programmable Thermal Controller (MJ Research Inc., Saint-Bruno-de-Montarville, QC, Canada). For the rs2280091 variant, the digestion reaction had a final volume of 15 µL, consisting of 10 µL of amplified DNA, 5 U of the NcoI restriction enzyme (10 U/µL), and 1X ThermoFisher Scientific Tango Buffer™, (ThermoFisher Scientific, Waltham, MA, USA) incubated at 37 °C.
The primer sequences, the restriction enzyme used for cleavage of the amplified DNA, and the resulting fragment sizes are summarized in
Table 7. For genotyping of the rs2280091 variant in the
ADAM33 gene, the following primers were used: T1 A/G F: 5′-ACTCAAGGTGACTGGGTGCT-3′ and T1 A/G R: 5′-GAGGGCATGAGGCTCACTTG-3′.
Enzymatic digestion with NcoI produced fragments of different lengths depending on the allele present: the A allele generated 140 bases pairs (bp) and 260 bp fragments, whereas the G allele produced a single 400 bp fragment.
The digested products were analyzed by 2% agarose gel electrophoresis, stained with SYBR® Safe DNA Gel Stain (1X), and separated according to molecular size, allowing for unequivocal allele identification. This approach ensured high sensitivity and specificity for detecting the ADAM33 rs2280091 variant, enabling robust association analyses with clinical and spirometric parameters.
4.4. Statistical Analysis
Genotypic frequencies were assessed for Hardy–Weinberg equilibrium using the chi-square (χ2) test implemented in the OEGE. p-values < 0.05 were considered indicative of deviation from equilibrium.
Allelic and genotypic frequencies of patients with CF were compared with those of the reference population from ABraOM using the χ2 test.
Spirometric parameters, including FVC, FEV1, FEF25%, FEF50%, FEF75%, MEF, and FEF25–75%, were analyzed using the Kruskal–Wallis and Mann–Whitney tests for independent samples. Numerical variables were presented as median with interquartile range (25th–75th percentiles), whereas categorical variables were expressed as absolute frequencies and percentages. Additionally, ORs and corresponding 95% CI were calculated using OpenEpi software (version 3.01) [
42].
All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) software (IBM SPSS Statistics for Macintosh, Version 28.0). Graphical representations and figures were generated using GraphPad Prism version 10.2.3 (GraphPad Software, Boston, MA, USA;
www.graphpad.com).
A significance level of 5% (p-values < 0.05) was adopted for all analyses. In this study, the FDR was controlled to reduce the likelihood of type I errors arising from multiple statistical comparisons. When a large number of hypotheses are tested simultaneously, the probability of obtaining statistically significant results by chance alone increases. To address this, we applied the Benjamini–Hochberg procedure, a widely accepted method for FDR correction, as implemented by the FDR calculator platform. This approach ranks the individual p-values from lowest to highest and determines the largest p-value that satisfies the threshold for statistical significance at a predefined FDR level. All values equal to or smaller than this cutoff are then considered significant after correction. Unlike more conservative methods such as Bonferroni adjustment, the Benjamini–Hochberg procedure maintains greater statistical power while still controlling the expected proportion of false positives among the results deemed significant.
In the present dataset, FDR correction was applied over three simultaneous comparisons, corresponding to the analytical groups presented in the title of
Table 4: (i) genotype comparisons (AA vs. AG vs. GG), (ii) grouped genotypes (AA vs. AG + GG), and (iii) allelic comparisons (A vs. G) for the rs2280091 variant of the
ADAM33 gene in individuals with CF. Therefore, the corrected
p-values reflect the adjustment for these three levels of analysis, ensuring that the reported associations remain robust after controlling for multiple testing. The application and rationale of this correction are explicitly described in
Section 4 and indicated in
Section 2 to ensure transparency and reproducibility.
The primary outcome of the study was to evaluate the association between the rs2280091 genotype of the ADAM33 gene and spirometric parameters. The secondary outcome was to compare the allelic and genotypic frequencies observed in CF patients with those reported for the Brazilian reference population from ABraOM.