Biological Mechanisms of Pain Management in Lumbar Disk Herniation: Focus on Cytokine Correlations and Therapeutic Approaches
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
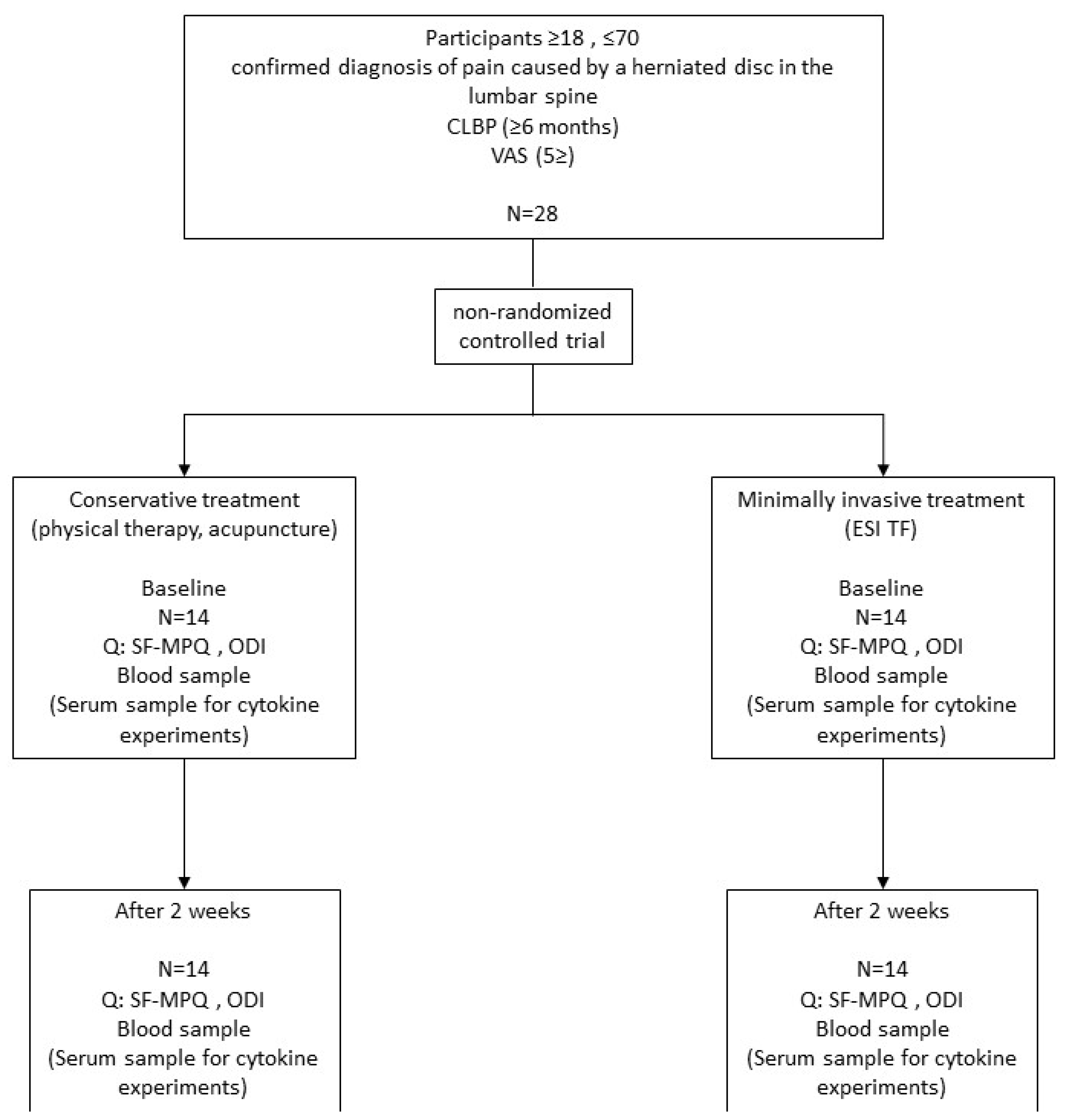
4.1. Study Design
4.2. Patients
4.3. Minimally Invasive Treatment Methods
4.4. Conservative Treatment Methods
4.5. Outcome Measurement
4.5.1. McGill (SF-MPQ)
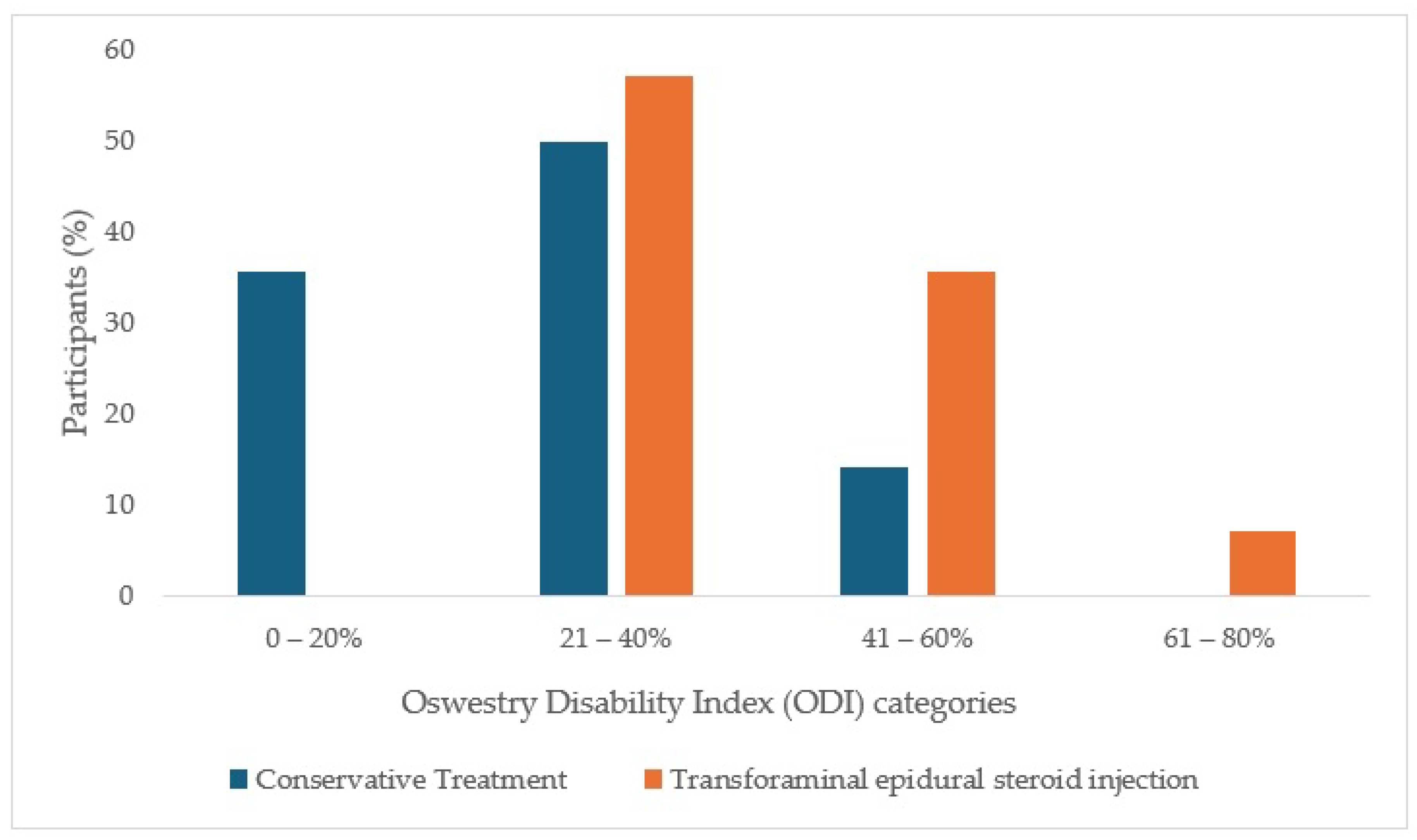
4.5.2. Oswestry Disability Index (ODI)
4.6. Blood Samples
4.7. Luminex
4.8. Statistical Methods
4.9. Ethics Committee
4.10. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LDH | lumbar disk herniation |
| IVD | intervertebral disk |
| IL-1β | interleukin-1 beta |
| TNF-α | tumor necrosis factor-α |
| MMP | matrix metalloproteinase |
| IFN -γ | interferon- gamma |
| IL-8 | interleukin 8 |
| IL-6 | interleukin 6 |
| MCP-1 | monocyte chemoattractant protein-1 |
| ESI TF | transforaminal Epidural Steroid Injection |
| IFC | interferential Current |
| TENS | transcutaneous electrical nerve stimulation |
| SF-MPQ | short form McGill pain questionnaire |
| ODI | Oswestry low back pain questionnaire |
| VAS | visual analog scale |
| SCI | spinal cord injury |
References
- Albert, H.B.; Sayari, A.J.; Barajas, J.N.; Hornung, A.L.; Harada, G.; Nolte, M.T.; Chee, A.V.; Samartzis, D.; Tkachev, A. The impact of novel inflammation-preserving treatment towards lumbar disc herniation resorption in symptomatic patients: A prospective, multi-imaging and clinical outcomes study. Eur. Spine J. 2024, 33, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Wan, S.; Xue, B.; Xiong, Y. Three-Dimensional Biomechanical Finite Element Analysis of Lumbar Disc Herniation in Middle Aged and Elderly. J. Healthc. Eng. 2022, 2022, 7107702. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.; Mao, F.; Chen, J.; Ma, X.; Dai, Y.; Liu, G.; Dai, F.; Liu, J. Characteristics and mechanisms of resorption in lumbar disc herniation. Arthritis Res. Ther. 2022, 24, 205. [Google Scholar] [CrossRef] [PubMed]
- Cunha, C.; Silva, A.J.; Pereira, P.; Vaz, R.; Gonçalves, R.M.; Barbosa, M.A. The inflammatory response in the regression of lumbar disc herniation. Arthritis Res. Ther. 2018, 20, 251. [Google Scholar] [CrossRef]
- Erwin, W.M.; Hood, K.E. The cellular and molecular biology of the intervertebral disc: A clinician’s primer. J. Can. Chiropr. Assoc. 2014, 58, 246–257. [Google Scholar]
- Nijs, J.; De Baets, L.; Hodges, P. Phenotyping nociceptive, neuropathic, and nociplastic pain: Who, how, & why? Braz. J. Phys. Ther. 2023, 27, 100537. [Google Scholar] [CrossRef]
- Cohen, S.P.; Mao, J. Neuropathic pain: Mechanisms and their clinical implications. BMJ 2014, 348, f7656, Erratum in BMJ 2014, 348, g2323. [Google Scholar] [CrossRef]
- Cohen, S.P.; Vase, L.; Hooten, W.M. Chronic pain: An update on burden, best practices, and new advances. Lancet 2021, 397, 2082–2097. [Google Scholar] [CrossRef]
- Wang, L.; He, T.; Liu, J.; Tai, J.; Wang, B.; Zhang, L.; Quan, Z. Revealing the Immune Infiltration Landscape and Identifying Diagnostic Biomarkers for Lumbar Disc Herniation. Front. Immunol. 2021, 12, 666355. [Google Scholar] [CrossRef]
- Sun, Z.; Liu, B.; Luo, Z.J. The Immune Privilege of the Intervertebral Disc: Implications for Intervertebral Disc Degeneration Treatment. Int. J. Med. Sci. 2020, 17, 685–692. [Google Scholar] [CrossRef]
- Rashed, S.; Vassiliou, A.; Starup-Hansen, J.; Tsang, K. Systematic review and meta-analysis of predictive factors for spontaneous regression in lumbar disc herniation. J. Neurosurg. Spine 2023, 39, 471–478. [Google Scholar] [CrossRef]
- Bermudez-Lekerika, P.; Crump, K.B.; Tseranidou, S.; Nüesch, A.; Kanelis, E.; Alminnawi, A.; Baumgartner, L.; Muñoz-Moya, E.; Compte, R.; Gualdi, F.; et al. Immuno-Modulatory Effects of Intervertebral Disc Cells. Front. Cell Dev. Biol. 2022, 10, 924692. [Google Scholar] [CrossRef]
- Martirosyan, N.L.; Patel, A.A.; Carotenuto, A.; Kalani, M.Y.; Belykh, E.; Walker, C.T.; Preul, M.C.; Theodore, N. Genetic alterations in intervertebral disc disease. Front. Surg. 2016, 3, 59. [Google Scholar] [CrossRef] [PubMed]
- Benzakour, T.; Igoumenou, V.; Mavrogenis, A.F.; Benzakour, A. Current concepts for lumbar disc herniation. Int. Orthop. 2019, 43, 841–851. [Google Scholar] [CrossRef] [PubMed]
- Wuertz, K.; Haglund, L. Inflammatory mediators in intervertebral disk degeneration and discogenic pain. Glob. Spine J. 2013, 3, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Thavarajasingam, S.G.; Salih, A.; Arif, A.; Varadpande, M.; Sabeshan, P.; Ponniah, H.S.; Kanakala, S.; Namireddy, S.R.; Ramsay, D.S.C.; Thavarajasingam, A.; et al. Indications for surgery versus conservative treatment in the management of lumbar disc herniations: A systematic review. Brain Spine 2025, 5, 105619. [Google Scholar] [CrossRef]
- Amin, R.M.; Andrade, N.S.; Neuman, B.J. Lumbar Disc Herniation. Curr. Rev. Musculoskelet. Med. 2017, 10, 507–516. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, R.; Wang, Y.; Dang, X. Efficacy of epidural steroid injection in the treatment of sciatica secondary to lumbar disc herniation: A systematic review and meta-analysis. Front. Neurol. 2024, 15, 1406504. [Google Scholar] [CrossRef]
- Zhou, T.; Salman, D.; McGregor, A.H. Recent clinical practice guidelines for the management of low back pain: A global comparison. BMC Musculoskelet. Disord. 2024, 25, 344. [Google Scholar] [CrossRef]
- GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- Kögl, N.; Petr, O.; Löscher, W.; Liljenqvist, U.; Thomé, C. Lumbar Disc Herniation—The Significance of Symptom Duration for the Indication for Surgery. Dtsch. Arztebl. Int. 2024, 121, 440–448. [Google Scholar] [PubMed]
- Budrovac, D.; Radoš, I.; Hnatešen, D.; Haršanji-Drenjančević, I.; Tot, O.K.; Katić, F.; Lukić, I.; Škiljić, S.; Nešković, N.; Dimitrijević, I. Effectiveness of Epidural Steroid Injection Depending on Discoradicular Contact: A Prospective Randomized Trial. Int. J. Environ. Res. Public Health 2023, 20, 3672. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Bigdon, S.; Riether, C.; Ma, X.; Niu, X.; Häckel, S.; Li, Z.; Gantenbein, B. The Role of the Bone Morphogenetic Protein Antagonist Noggin in Nucleus Pulposus Intervertebral Disc Cells. Int. J. Mol. Sci. 2024, 25, 11803. [Google Scholar] [CrossRef] [PubMed]
- Yan, L.; Zhang, J.; Wang, X.; Zhou, Q.; Wen, J.; Zhao, H.; Guo, K.; Zeng, J. Efficacy of acupuncture for lumbar disc herniation: Changes in paravertebral muscle and fat infiltration—A multicenter retrospective cohort study. Front. Endocrinol. 2024, 15, 1467769. [Google Scholar] [CrossRef]
- Yang, L.; Li, J.; Cui, Z.; Huang, L.; Chen, T.; Liu, X.; Lu, H. Integrating Bulk RNA and Single-Cell Sequencing Data Reveals Genes Related to Energy Metabolism and Efferocytosis in Lumbar Disc Herniation. Biomedicines 2025, 13, 1536. [Google Scholar] [CrossRef]
- Satpute, K.; Hall, T.; Bisen, R.; Lokhande, P. The Effect of Spinal Mobilization with Leg Movement in Patients with Lumbar Radiculopathy-A Double-Blind Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2019, 100, 828–836. [Google Scholar] [CrossRef]
- Joswig, H.; Neff, A.; Ruppert, C.; Hildebrandt, G.; Stienen, M.N. The Value of Short-Term Pain Relief in Predicting the Long-Term Outcome of Lumbar Transforaminal Epidural Steroid Injections. World Neurosurg. 2017, 107, 764–771. [Google Scholar] [CrossRef]
- Hammerich, A.; Whitman, J.; Mintken, P.; Denninger, T.; Akuthota, V.; Sawyer, E.E.; Hofmann, M.; Childs, J.D.; Cleland, J. Effectiveness of Physical Therapy Combined with Epidural Steroid Injection for Individuals with Lumbar Spinal Stenosis: A Randomized Parallel-Group Trial. Arch. Phys. Med. Rehabil. 2019, 100, 797–810. [Google Scholar] [CrossRef]
- Tarcău, E.; Ianc, D.; Sirbu, E.; Ciobanu, D.; Boca, I.C.; Marcu, F. Effects of Complex Rehabilitation Program on Reducing Pain and Disability in Patients with Lumbar Disc Protrusion-Is Early Intervention the Best Recommendation? J. Pers. Med. 2022, 12, 741. [Google Scholar] [CrossRef]
- Pedersen, L.M.; Schistad, E.; Jacobsen, L.M.; Røe, C.; Gjerstad, J. Serum levels of the pro-inflammatory interleukins 6 (IL-6) and -8 (IL-8) in patients with lumbar radicular pain due to disc herniation: A 12-month prospective study. Brain Behav. Immun. 2015, 46, 132–136. [Google Scholar] [CrossRef]
- Krock, E.; Millecamps, M.; Anderson, K.M.; Srivastava, A.; Reihsen, T.E.; Hari, P.; Sun, Y.R.; Jang, S.H.; Wilcox, G.L.; Belani, K.G.; et al. Interleukin-8 as a therapeutic target for chronic low back pain: Upregulation in human cerebrospinal fluid and pre-clinical validation with chronic reparixin in the SPARC-null mouse model. EBioMedicine 2019, 43, 487–500. [Google Scholar] [CrossRef]
- Brisby, H.; Olmarker, K.; Larsson, K.; Nutu, M.; Rydevik, B. Proinflammatory cytokines in cerebrospinal fluid and serum in patients with disc herniation and sciatica. Eur. Spine J. 2002, 11, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Das, B.; Conroy, M.; Moore, D.; Lysaght, J.; McCrory, C. Human dorsal root ganglion pulsed radiofrequency treatment modulates cerebrospinal fluid lymphocytes and neuroinflammatory markers in chronic radicular pain. Brain Behav. Immun. 2018, 70, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Moen, G.H.; Moen, A.; Schistad, E.I.; Gjerstad, J. Local up-regulation of interferon-γ (IFN-γ) following disc herniation is involved in the inflammatory response underlying acute lumbar radicular pain. Cytokine 2017, 97, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Nerlich, A.G.; Weiler, C.; Zipperer, J.; Narozny, M.; Boos, N. Immunolocalization of phagocytic cells in normal and degenerated intervertebral discs. Spine 2002, 27, 2484–2490. [Google Scholar] [CrossRef]
- Kamieniak, P.; Bielewicz, J.M.; Grochowski, C.; Litak, J.; Bojarska-Junak, A.; Janczarek, M.; Daniluk, B.; Trojanowski, T. IFN-γ Correlations with Pain Assessment, Radiological Findings, and Clinical Intercourse in Patient after Lumbar Microdiscectomy: Preliminary Study. Dis. Markers 2020, 2020, 1318930. [Google Scholar] [CrossRef]
- Sabirov, D.; Ogurcov, S.; Shulman, I.; Kabdesh, I.; Garanina, E.; Sufianov, A.; Rizvanov, A.; Mukhamedshina, Y. Comparative Analysis of Cytokine Profiles in Cerebrospinal Fluid and Blood Serum in Patients with Acute and Subacute Spinal Cord Injury. Biomedicines 2023, 11, 2641. [Google Scholar] [CrossRef]
- Gorth, D.J.; Shapiro, I.M.; Risbud, M.V. Transgenic mice overexpressing human TNF-α experience early onset spontaneous intervertebral disc herniation in the absence of overt degeneration. Cell Death Dis. 2018, 10, 7. [Google Scholar] [CrossRef]
- Nilsson, E.; Nakamae, T.; Olmarker, K. Pain behavior changes following disc puncture relate to nucleus pulposus rather than to the disc injury per se: An experimental study in rats. Open Orthop. J. 2011, 5, 72–77. [Google Scholar] [CrossRef]
- Lai, A.; Moon, A.; Purmessur, D.; Skovrlj, B.; Laudier, D.M.; Winkelstein, B.A.; Cho, S.K.; Hecht, A.C.; Iatridis, J.C. Annular puncture with tumor necrosis factor-alpha injection enhances painful behavior with disc degeneration in vivo. Spine J. 2016, 16, 420–431. [Google Scholar] [CrossRef]
- Zu, B.; Pan, H.; Zhang, X.J.; Yin, Z.S. Serum Levels of the Inflammatory Cytokines in Patients with Lumbar Radicular Pain Due to Disc Herniation. Asian Spine J. 2016, 10, 843–849. [Google Scholar] [CrossRef]
- Zhang, J.; Bellow, E.; Bae, J.; Johnson, D.; Bajrami, S.; Torpey, A.; Caldwell, W. Modic Changes as Biomarkers for Treatment of Chronic Low Back Pain. Biomedicines 2025, 13, 1697. [Google Scholar] [CrossRef] [PubMed]
- Chalermkitpanit, P.; Singhatanadgige, W.; Yingsakmongkol, W.; Tanasansomboon, T.; Jitjumnong, M.; Honsawek, S. A reduction in serum IFN-γ, IL-1β, IL-6, and GM-CSF serves as potential markers for a positive outcome to lumbar epidural steroid injections. PLoS ONE 2025, 20, e0329552. [Google Scholar] [CrossRef] [PubMed]
- Sadowska, A.; Touli, E.; Hitzl, W.; Greutert, H.; Ferguson, S.J.; Wuertz-Kozak, K.; Hausmann, O.N. Inflammaging in cervical and lumbar degenerated intervertebral discs: Analysis of proinflammatory cytokine and TRP channel expression. Eur. Spine J. 2018, 27, 564–577. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, L.M.R.; Oliveira, L.Z.; Silva, M.B.R.D.; Accardo, C.M.; Giglio, A.B.D.; Pinhal, M.A.D.S. Inflammatory biomarkers in sera of patients with intervertebral disc degeneration. Einstein 2019, 17, eAO4637. [Google Scholar] [CrossRef]
- Pravdyuk, N.G.; Novikova, A.V.; Shostak, N.A.; Buianova, A.A.; Tairova, R.T.; Patsap, O.I.; Raksha, A.P.; Timofeyev, V.T.; Feniksov, V.M.; Nikolayev, D.A.; et al. Immunomorphogenesis in Degenerative Disc Disease: The Role of Proinflammatory Cytokines and Angiogenesis Factors. Biomedicines 2023, 11, 2184. [Google Scholar] [CrossRef]
- Kabdesh, I.; Tutova, O.; Akhmetzyanova, E.; Timofeeva, A.; Bilalova, A.; Mukhamedshina, Y.; Chelyshev, Y. Thoracic Spinal Cord Contusion Impacts on Lumbar Enlargement: Molecular Insights. Mol. Neurobiol. 2025, 62, 8551–8567. [Google Scholar] [CrossRef]
- Bruce, B.; Fries, J.F. The Stanford Health Assessment Questionnaire: Dimensions and Practical Applications. Health Qual. Life Outcomes 2003, 1, 20. [Google Scholar] [CrossRef]
| Number (%) of Participants | p * | |||
|---|---|---|---|---|
| Conservative Treatment (n = 14) | ESI TF (n = 14) | Total (n = 28) | ||
| Gender | ||||
| Male | 3 (21) | 4 (29) | 7 (25) | >0.99 |
| Female | 11 (79) | 10 (71) | 21 (75) | |
| Marital status | ||||
| Married | 10 (71) | 10 (71) | 20 (71) | >0.99 |
| Divorced | 2 (14) | 1 (7) | 3 (11) | |
| Single | 1 (7) | 1 (7) | 2 (7) | |
| Widower | 1 (7) | 1 (7) | 2 (7) | |
| Education | ||||
| Primary school | 0 | 3 (21) | 3 (11) | 0.40 |
| High school | 12 (86) | 9 (64) | 21 (75) | |
| Bachelor’s degree | 1 (7) | 1 (7) | 2 (7) | |
| Master’s degree | 1 (7) | 1 (7) | 2 (7) | |
| Working status | ||||
| Employed | 7 (50) | 4 (29) | 11 (39) | 0.09 |
| Employed, but currently on sick leave | 1 (7) | 1 (7.1) | 2 (7) | |
| Employed, but on long-term sick leave | 0 | 3 (21) | 3 (11) | |
| Unemployed | 0 | 3 (21) | 3 (11) | |
| Retired | 6 (43) | 3 (21) | 9 (32,1) | |
| Median (Interquartile Range) | p * | ||||
|---|---|---|---|---|---|
| Conservative Treatment (n = 14) | p † | ESI TF (n = 14) | p † | ||
| Sensory domain | |||||
| Baseline | 16.5 (6.8–18.8) | 0.41 | 16 (8.75–25.5) | 0.10 | 0.27 |
| After 2 weeks | 10.5 (5.75–16.5) | 12 (8–22.75) | 0.38 | ||
| Affective domain | |||||
| Baseline | 4 (2–6) | 0.65 | 9 (1.75–11.25) | 0.33 | 0.09 |
| After 2 weeks | 3 (0–5.25) | 4.5 (2.75–10) | 0.12 | ||
| Pain in the past week | |||||
| Baseline | 60 (48.25–68.25) | 0.02 | 70 (67.75–79.25) | 0.02 | 0.04 |
| After 2 weeks | 47.5 (30–58.5) | 50 (37.5–60) | 0.75 | ||
| Current pain intensity [1(none)–5 (severe)] | |||||
| Baseline | 2 (2–3) | 0.01 | 3 (2–3) | 0.13 | 0.49 |
| After 2 weeks | 2 (1.75–2.25) | 2 (1.75–3) | 0.67 | ||
| ODI Total | Median (Interquartile Range) | p * | |||
|---|---|---|---|---|---|
| Conservative Treatment (n = 14) | p † | ESI TF (n = 14) | p † | ||
| ODI total | |||||
| Baseline | 30 (15–37) | 0.06 | 40 (35.5–53) | 0.008 | 0.006 |
| After 2 weeks | 34 (21–41.5) | 36 (27–45.5) | 0.46 | ||
| Spearman’s Correlation Coefficient Rho (p Value) | |||||
|---|---|---|---|---|---|
| IFN-γ (pg/mL) | IL-1β (pg/mL) | IL-6 (pg/mL) | Il-8 (pg/mL) | TNF-α (pg/mL) | |
| Conservative Treatment | |||||
| Baseline | |||||
| IFN-γ (pg/mL) | - | ||||
| IL-1β (pg/mL) | −0.204 (0.50) | - | |||
| IL-6 (pg/mL) | 0.515 (0.07) | 0.060 (0.85) | - | ||
| IL-8 (pg/mL) | −0.120 (0.70) | 0.280 (0.35) | 0.274 (0.36) | - | |
| TNF-α (pg/mL) | −0.528 (0,06) | −0.047 (0.88) | −0.712 (0.006) | −0.104 (0.74) | - |
| After 2 weeks | |||||
| IFN-γ (pg/mL) | - | ||||
| IL-1β (pg/mL) | 0.587 (0.03) | - | |||
| IL-6 (pg/mL) | 0.337 (0.26) | 0.198 (0.52) | - | ||
| IL-8 (pg/mL) | 0.127 (0.68) | −0.234 (0.44) | 0.260 (0.39) | - | |
| TNF-α (pg/mL) | −0.146 (0.63) | 0.063 (0.84) | −0.025 (0.94) | −0.158 (0.61) | - |
| ESI TF | |||||
| Baseline | |||||
| IFN-γ (pg/mL) | - | ||||
| IL-1β (pg/mL) | 0.772 (0.001) | - | |||
| IL-6 (pg/mL) | 0.159 (0.59) | 0.273 (0.35) | - | ||
| IL-8 (pg/mL) | 0.210 (0.47) | 0.263 (0.36) | 0.505 (0.07) | - | |
| TNF-α (pg/mL) | 0.265 (0.36) | 0.464 (0.09) | 0.108 (0.71) | 0.153 (0.60) | - |
| After 2 weeks | |||||
| IFN-γ (pg/mL) | - | ||||
| IL-1β (pg/mL) | 0.425 (0.13) | - | |||
| IL-6 (pg/mL) | 0.432 (0.12) | 0.183 (0.53) | - | ||
| IL-8 (pg/mL) | −0.024 (0.93) | −0.135 (0.65) | −0.305 (0.29) | - | |
| TNF-α (pg/mL) | 0.326 (0.26) | 0.501 (0.07) | −0.016 (0.96) | 0.040 (0.89) | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rožac, K.; Matić, A.; Budrovac, D.; Hnatešen, D.; Radoš, I.; Kralik, K.; Smolić, M.; Kovač Lukić, T. Biological Mechanisms of Pain Management in Lumbar Disk Herniation: Focus on Cytokine Correlations and Therapeutic Approaches. Int. J. Mol. Sci. 2025, 26, 10830. https://doi.org/10.3390/ijms262210830
Rožac K, Matić A, Budrovac D, Hnatešen D, Radoš I, Kralik K, Smolić M, Kovač Lukić T. Biological Mechanisms of Pain Management in Lumbar Disk Herniation: Focus on Cytokine Correlations and Therapeutic Approaches. International Journal of Molecular Sciences. 2025; 26(22):10830. https://doi.org/10.3390/ijms262210830
Chicago/Turabian StyleRožac, Karla, Anita Matić, Dino Budrovac, Dijana Hnatešen, Ivan Radoš, Kristina Kralik, Martina Smolić, and Tanja Kovač Lukić. 2025. "Biological Mechanisms of Pain Management in Lumbar Disk Herniation: Focus on Cytokine Correlations and Therapeutic Approaches" International Journal of Molecular Sciences 26, no. 22: 10830. https://doi.org/10.3390/ijms262210830
APA StyleRožac, K., Matić, A., Budrovac, D., Hnatešen, D., Radoš, I., Kralik, K., Smolić, M., & Kovač Lukić, T. (2025). Biological Mechanisms of Pain Management in Lumbar Disk Herniation: Focus on Cytokine Correlations and Therapeutic Approaches. International Journal of Molecular Sciences, 26(22), 10830. https://doi.org/10.3390/ijms262210830





